Devices, systems and methods for tissue repair
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example a
[0192] Arthroscopic repair of Bankart lesion with arthroscopic suture plication of associated anterior capsular laxity.
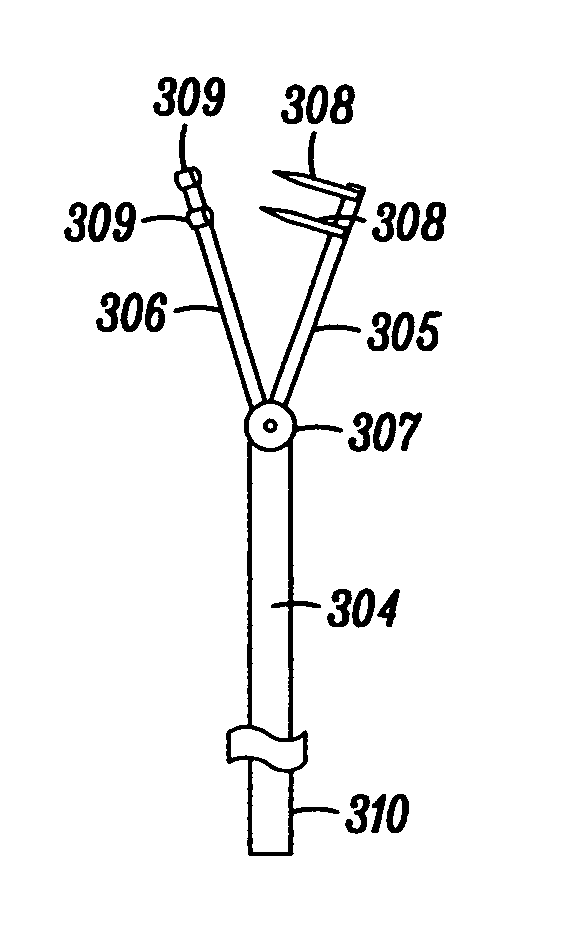
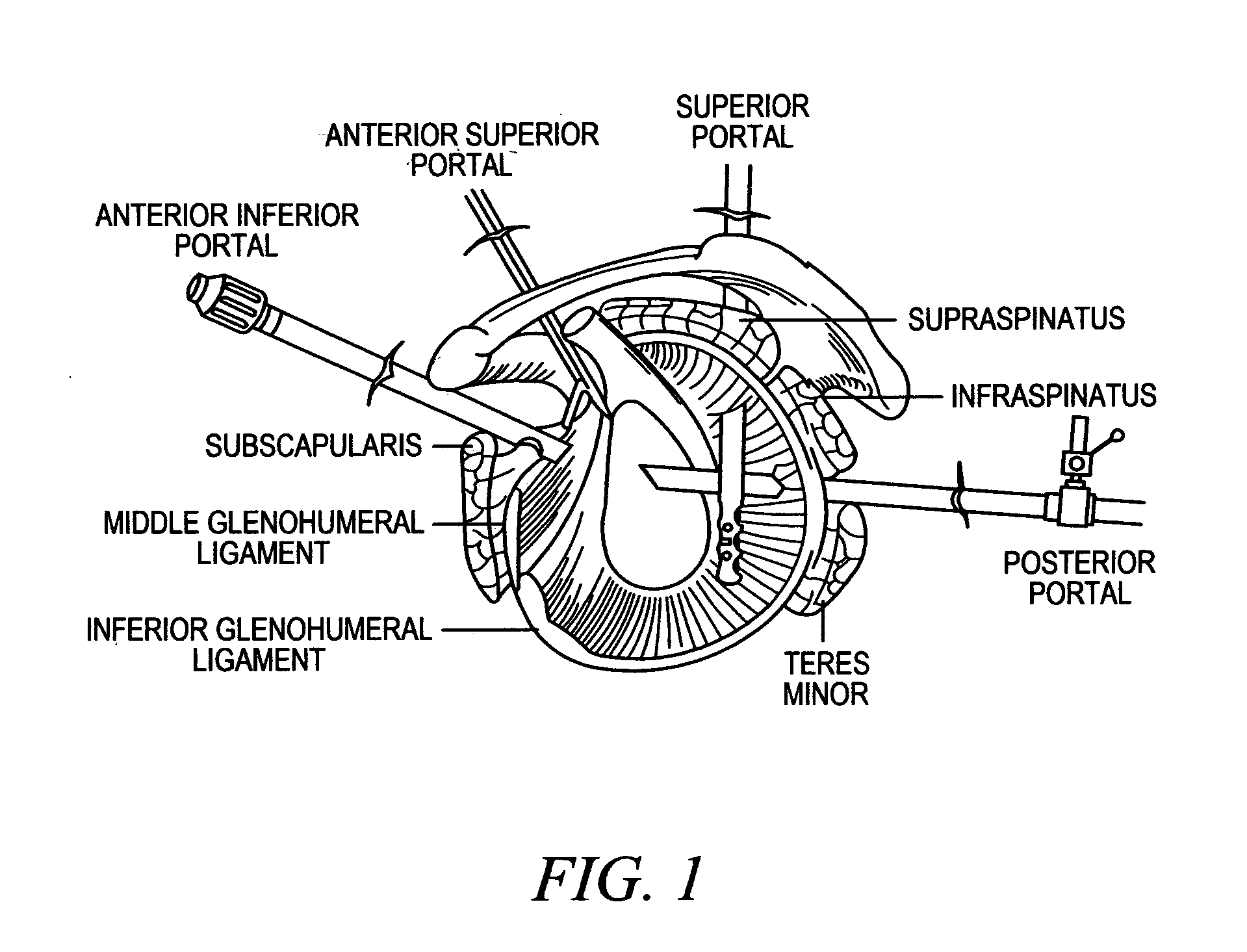
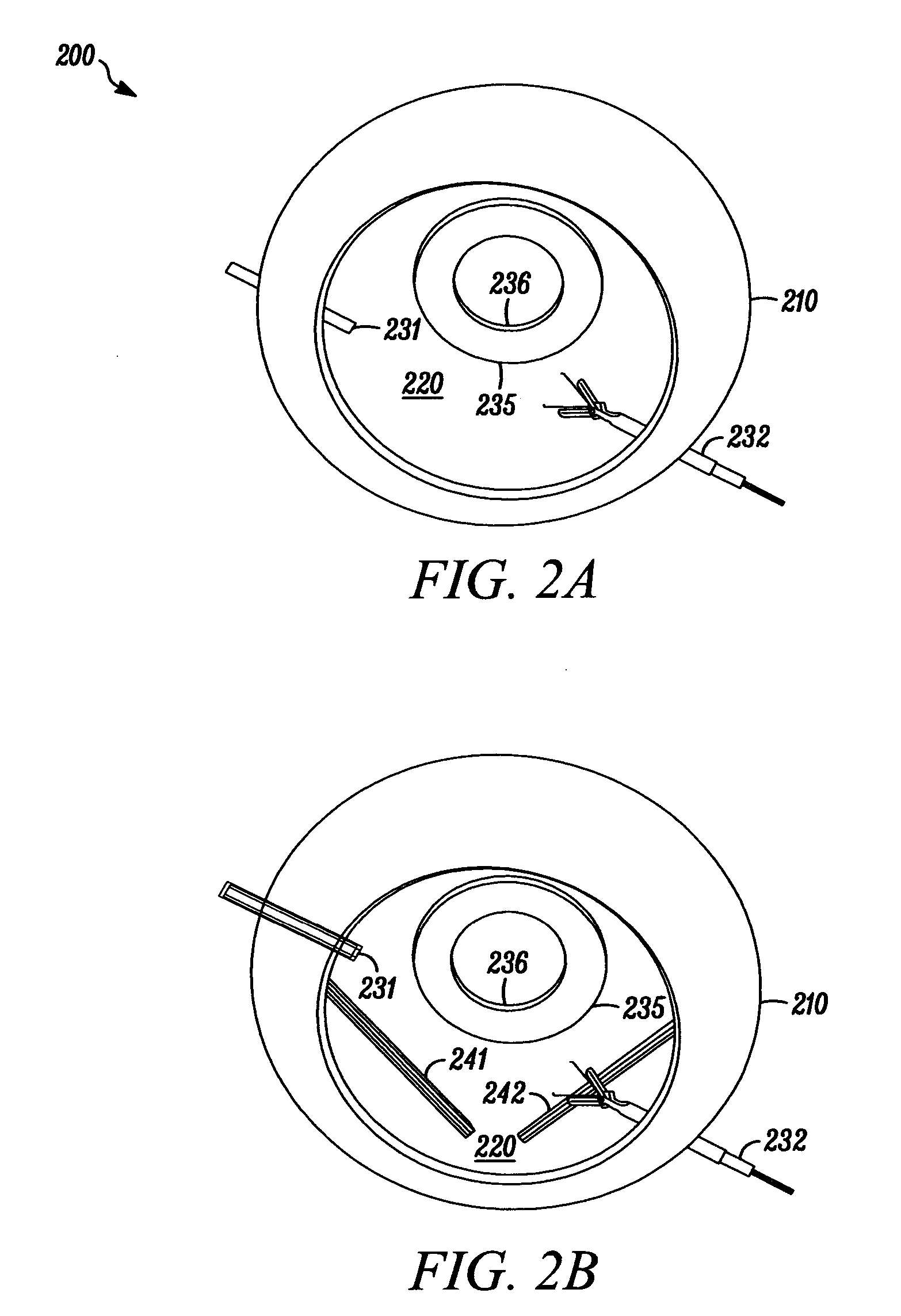
[0193] Following examination under anesthesia and standard surgical prepping and draping, standard anterior and posterior glenohumeral arthroscopy portal are established. The patient may be positioned either in the lateral decubitus position or in a beach chair position. Following completion of diagnostic arthroscopy, attention is first focused on repair of the Bankart lesion. After the Bankart repair has been performed, residual anterior capsular laxity is assessed. The surgeon subsequently places the humerus in the desired position (in terms of external rotation and abduction; this will vary according to patient demand and individual surgeon preference). With the shoulder placed in the desired position, capsular redundancy is addressed via performing a suture plication. The capsular plication deployment device is introduced through a standard anterosuperior porta...
example b
[0194] Capsular laxity without an associated Bankart lesion (e.g., anterior unidirectional atraumatic instability).
[0195] Following examination under anesthesia, standard anterior and posterior glenohumeral arthroscopic portals are established. A thorough diagnostic glenohumeral arthroscopy is performed with specific attention to determining the extent and distribution of capsular laxity. With the shoulder positioned in the desired amount of abduction and external rotation, the anterior capsule is tensioned via placement of anterior capsular plications in a posteroinferior to anterosuperior sequence via the anterosuperior portal. The sequence of placement of successive plication devices in a posteroinferior to anterosuperior direction is determined by virtue of the fact that if the anterosuperior capsule is tensioned first then placement of the capsular plication deployment device more inferiorly and posteriorly will be more difficult. However, tensioning the axillary pouch (poster...
example c
[0196] Multidirectional Instability (MDI).
[0197] Following examination under anesthesia, standard anterosuperior and posterior glenohumeral arthroscopic portals are established and a through diagnostic arthroscopy is performed. The redundant posterior capsule and posteroinferior capsule is tightened first. This is accomplished via visualization through an accessory anterior portal. The capsular plication deployment device is introduced through the standard anterosuperior portal. The posterior capsule is visualized via placement of the arthroscope through the accessory anterior portal. Posterior capsular redundancy is reduced via placement of successive capsular plications posteriorly (in an inferior to superior sequence). The arthroscope is subsequently reintroduced through the standard posterior glenohumeral viewing portal and the standard anterosuperior portal is utilized to perform the capsular plications. The inferior and anterior glenohumeral capsule is tensioned via placement...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com