Methods for implanting intraocular shunts
a technology of intraocular shunt and shunt, which is applied in the field of surgical methods, implantation devices, and shunts, can solve the problems of trabecular meshwork, open angle glaucoma, retinal damage and blindness, etc., and achieve the effect of reducing or eliminating the risk of hypotony and related side effects, and protecting the integrity of the conjunctiva
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
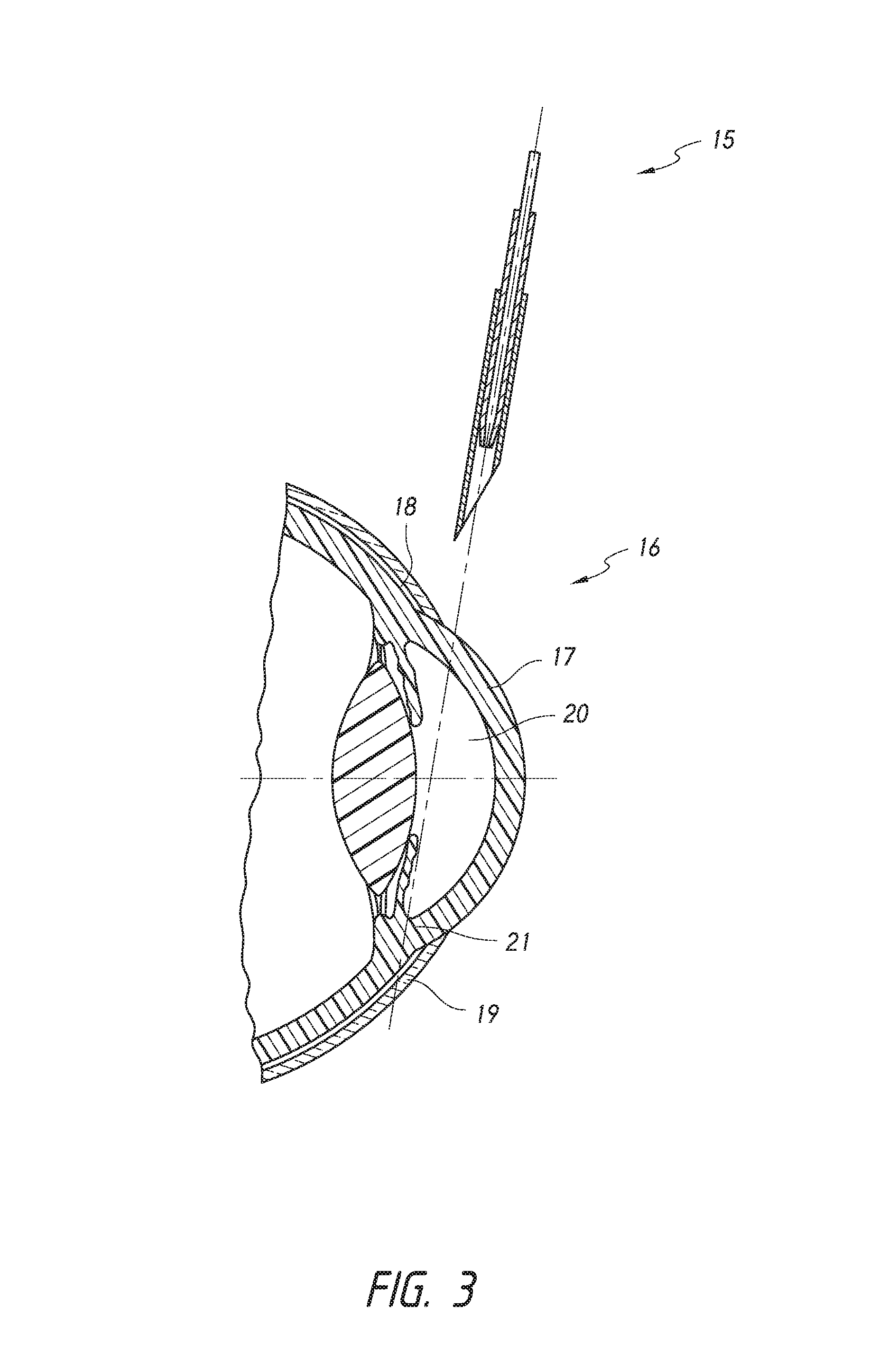
[0136]The present inventions generally relate to methods for treating closed angle glaucoma that involve using a deployment device that is configured to both re-open a partially or completely closed anterior chamber angle and deploy an intraocular shunt. In certain aspects, some methods involve inserting into an eye a deployment device configured to hold an intraocular shunt, using the device to re-open an at least partially closed anterior chamber angle of an eye, and deploying the shunt from the device.
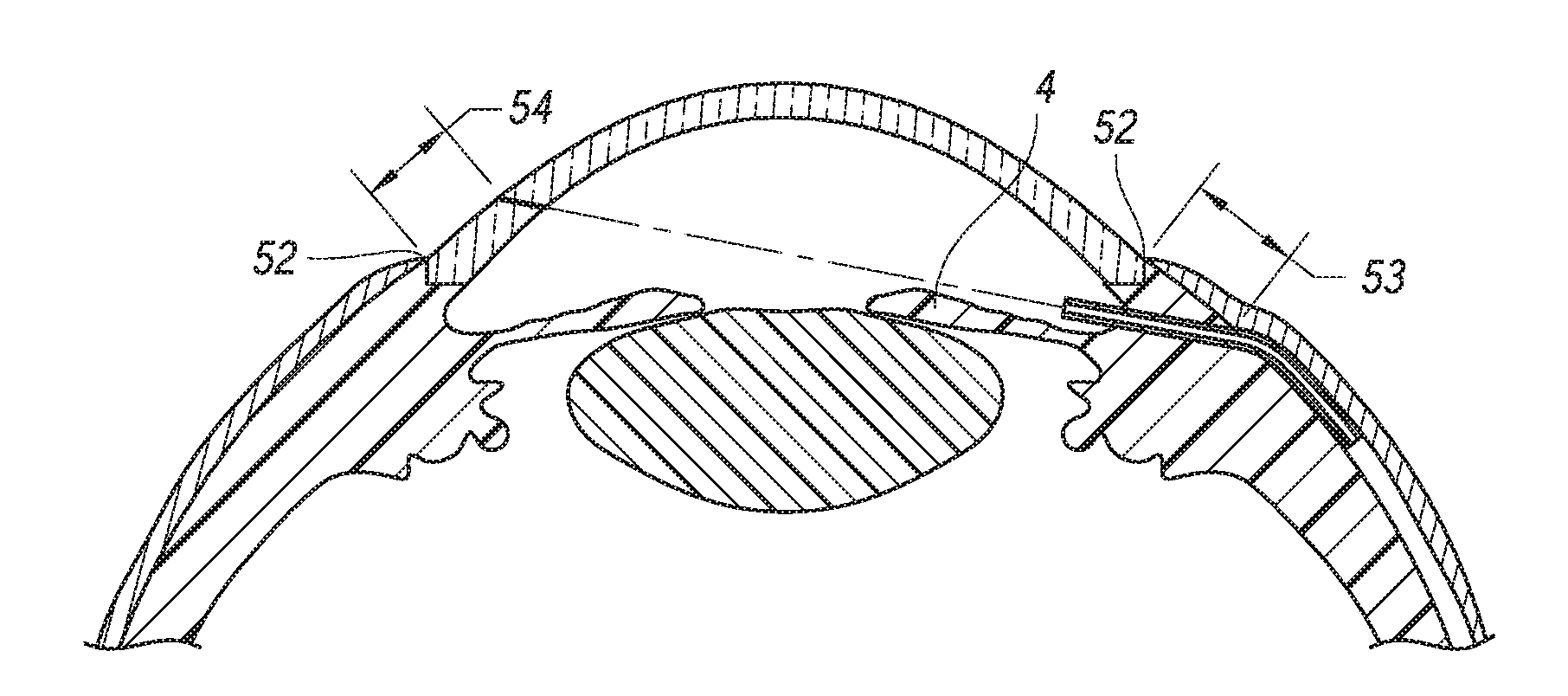
[0137]FIG. 1 provides a schematic diagram of the general anatomy of the eye. An anterior aspect of the anterior chamber 1 of the eye is the cornea 2, and a posterior aspect of the anterior chamber 1 of the eye is the iris 4. Beneath the iris 4 is the lens 5. The anterior chamber 1 is filled with aqueous humor 3. The aqueous humor 3 drains into a space(s) 6 below the conjunctiva 7 through the trabecular meshwork (not shown in detail) of the sclera 8. The aqueous humor is drained from...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com