Patents
Literature
682 results about "Sclera" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
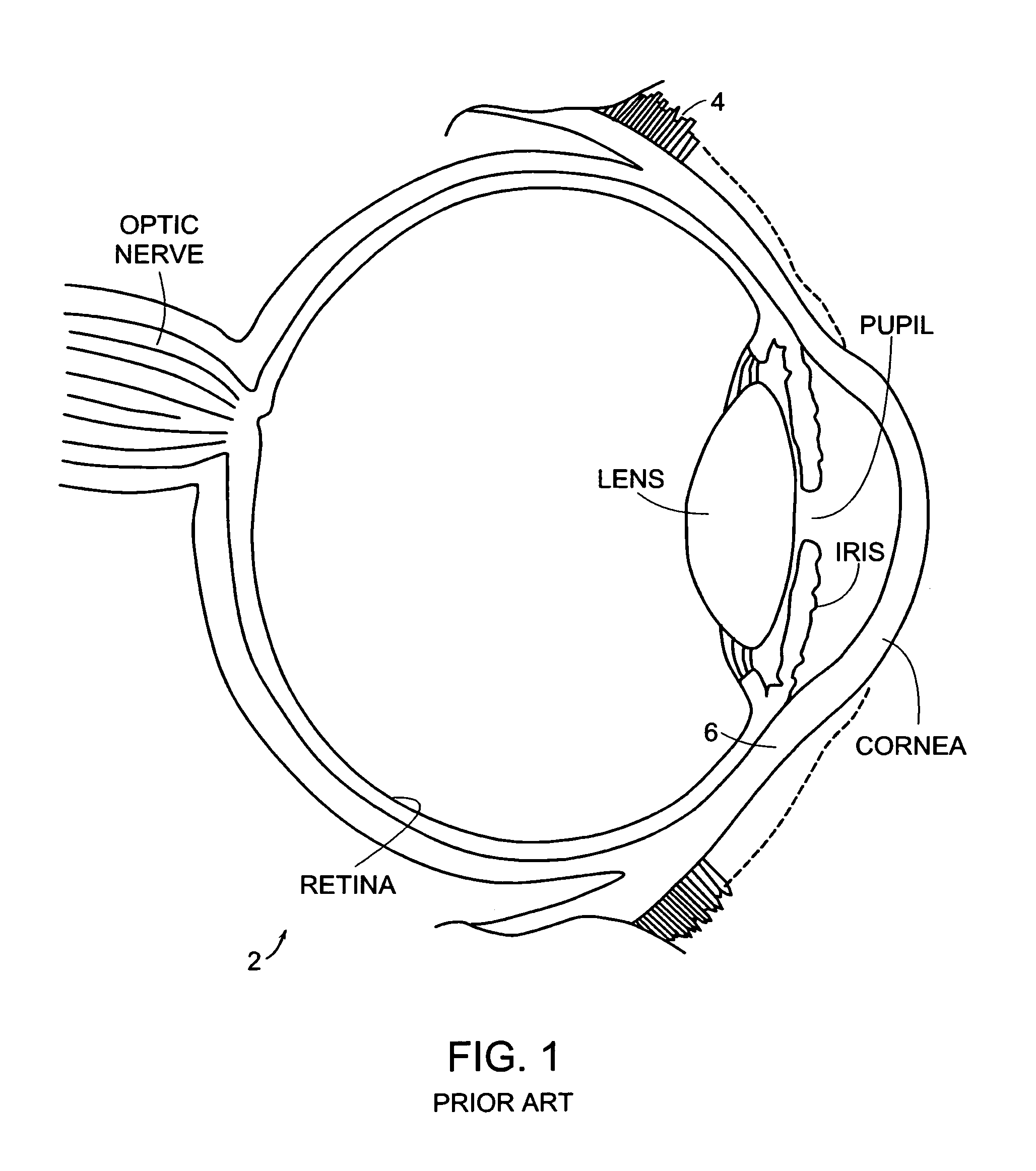
The sclera, also known as the white of the eye, is the opaque, fibrous, protective, outer layer of the human eye containing mainly collagen and some elastic fiber. In humans, the whole sclera is white, contrasting with the coloured iris, but in other mammals the visible part of the sclera matches the colour of the iris, so the white part does not normally show. In the development of the embryo, the sclera is derived from the neural crest. In children, it is thinner and shows some of the underlying pigment, appearing slightly blue. In the elderly, fatty deposits on the sclera can make it appear slightly yellow. Many people with dark skin have naturally darkened sclerae, the result of melanin pigmentation.
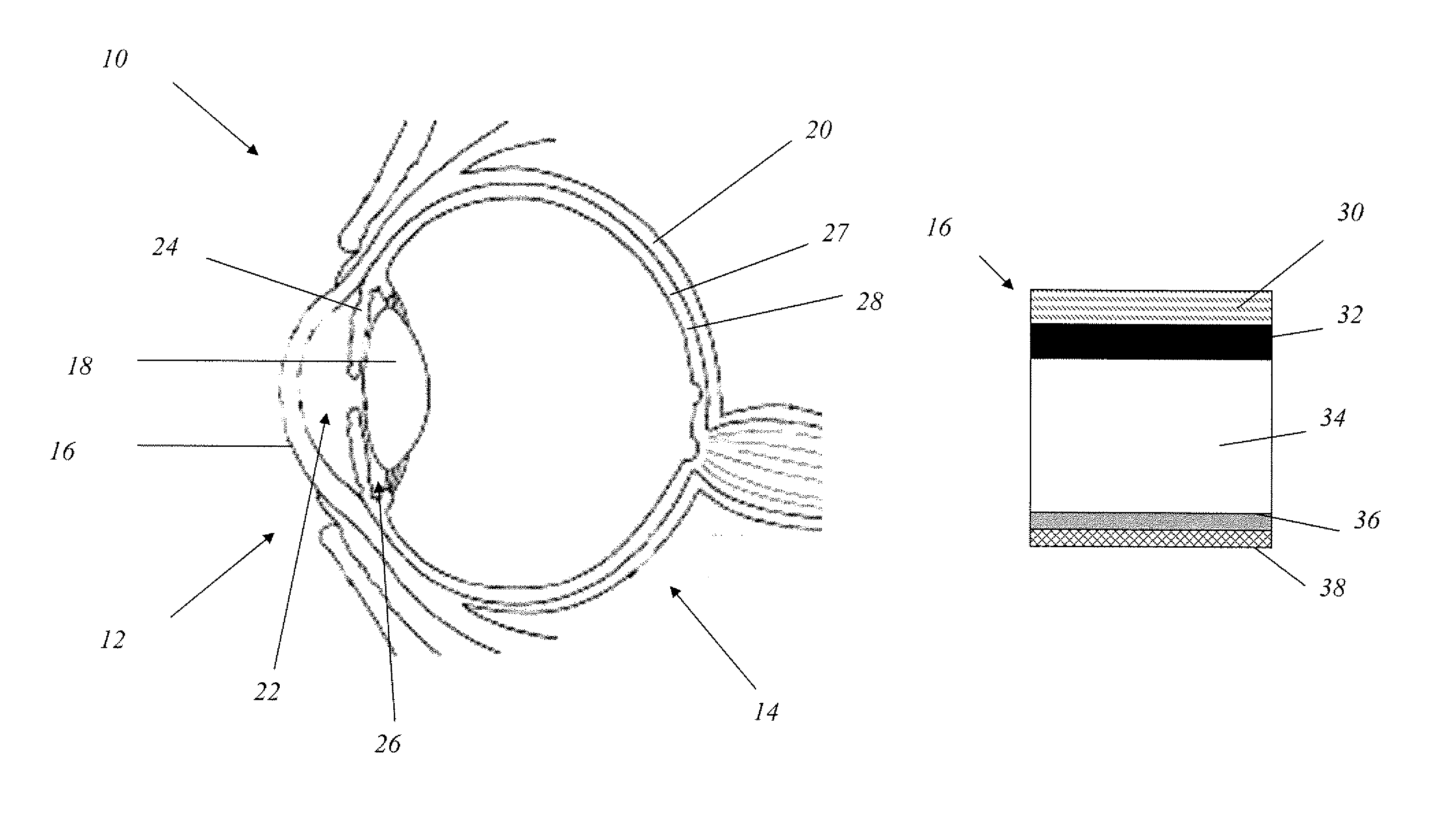
Uveoscleral shunt and methods for implanting same
ActiveUS20080228127A1Small sectionAvoid passingSenses disorderEar treatmentCiliary bodySuprachoroidal space
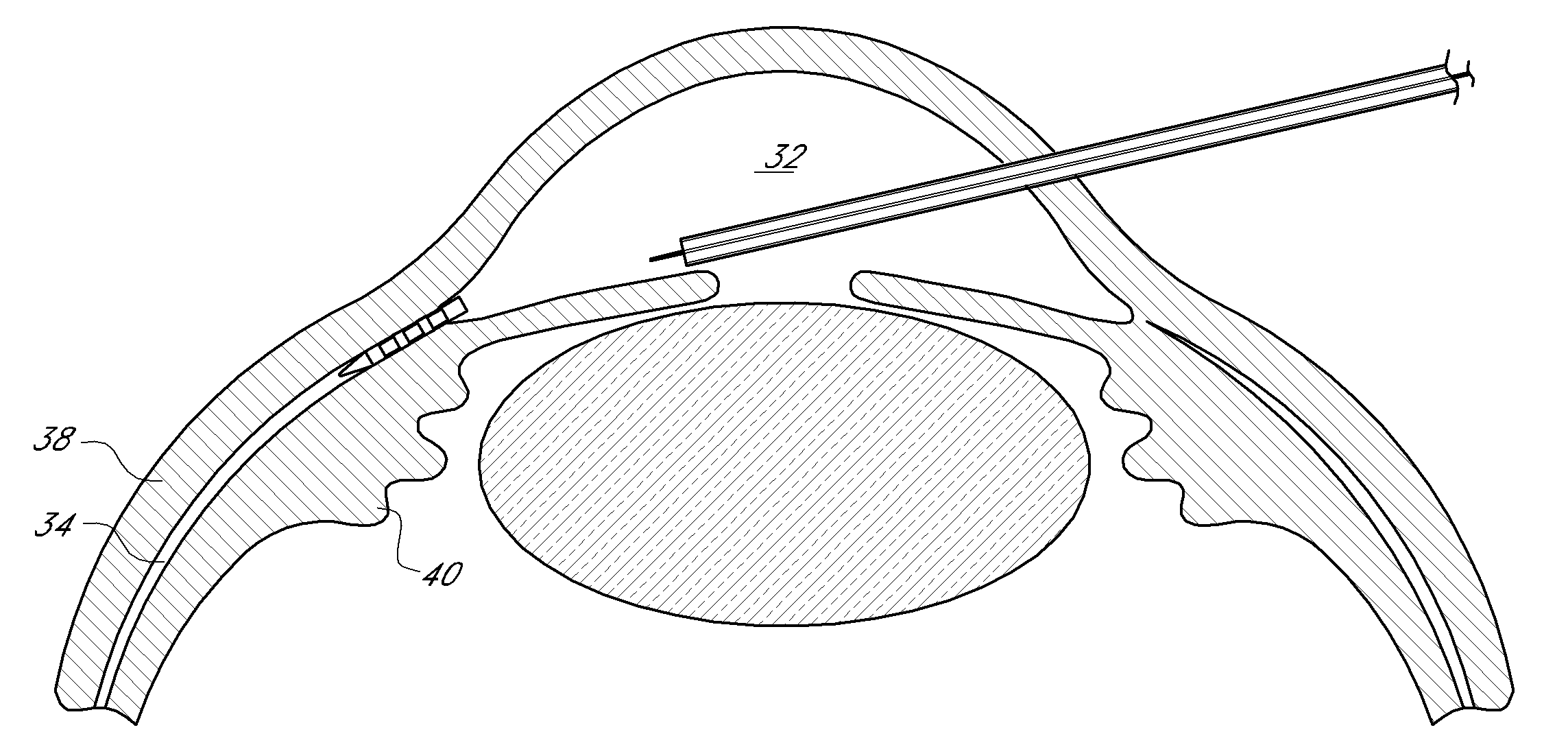
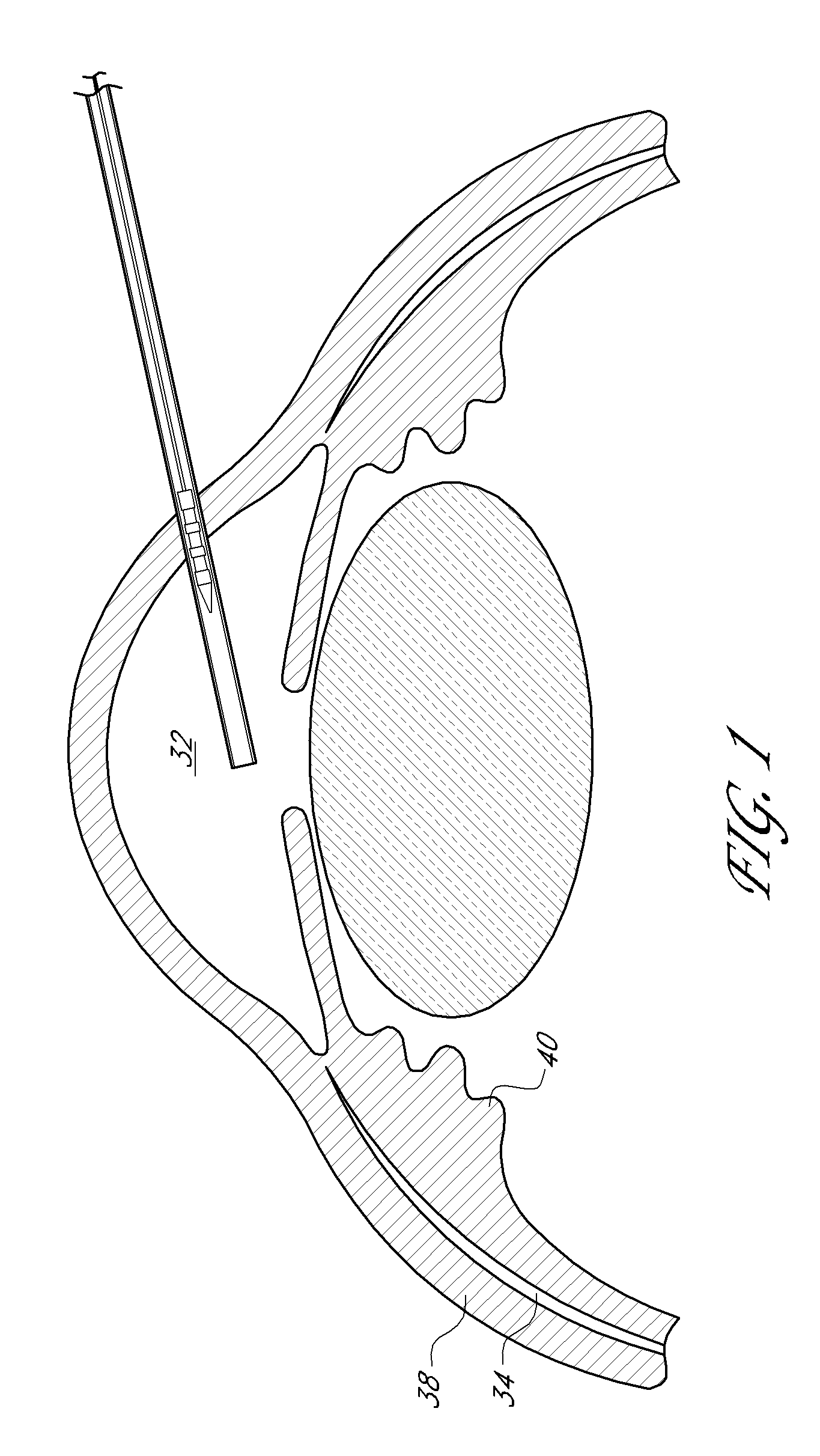
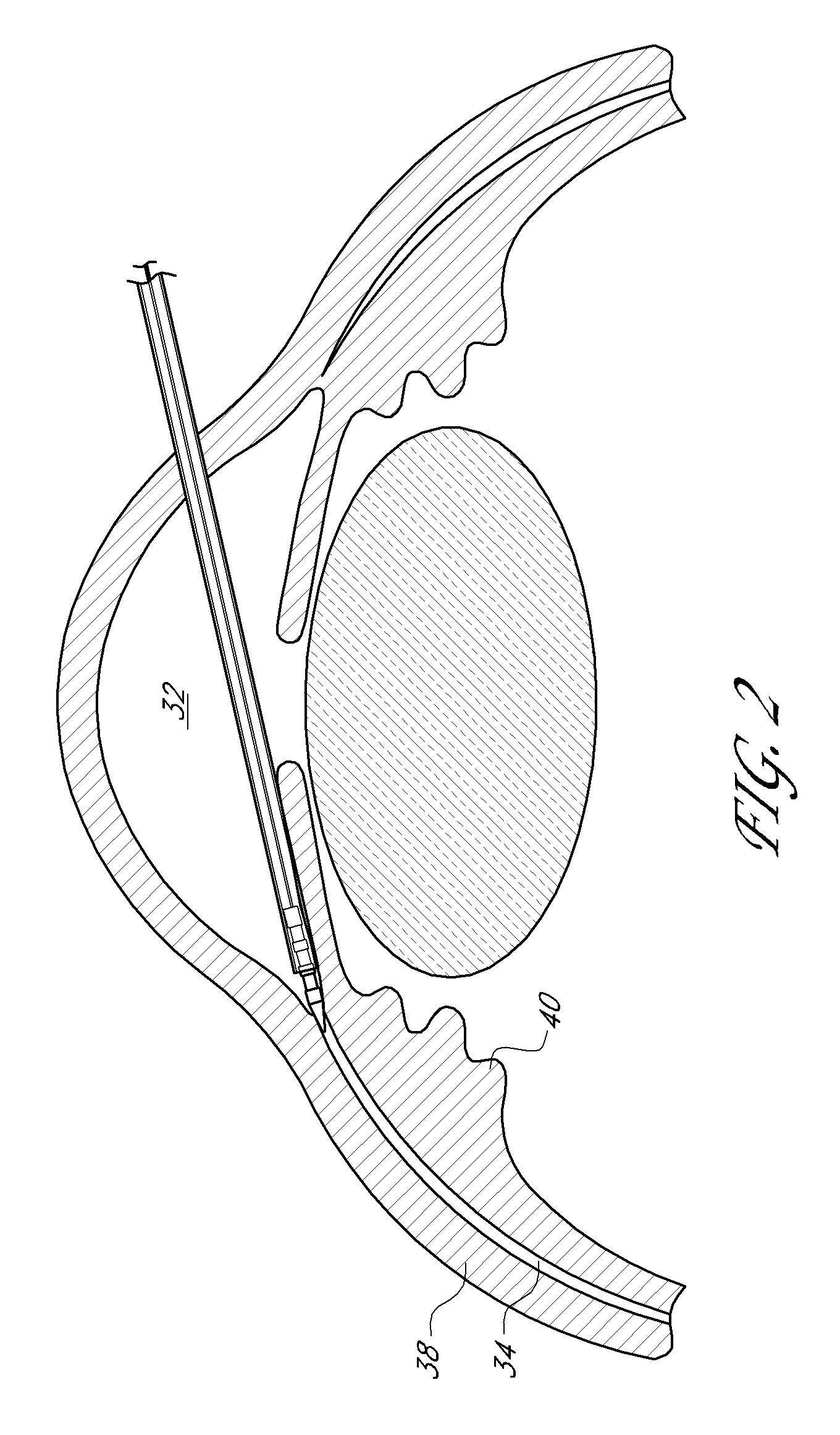
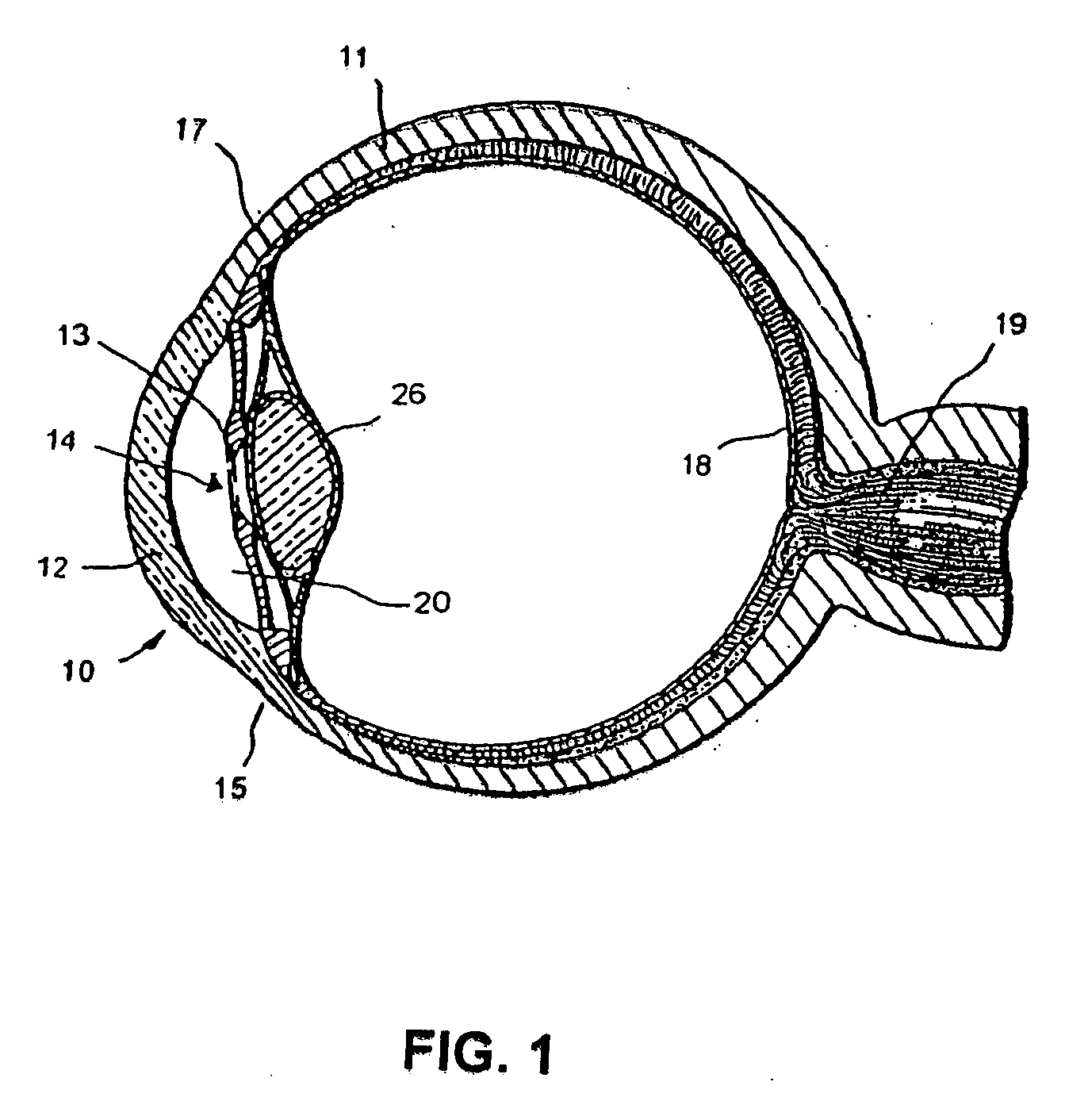
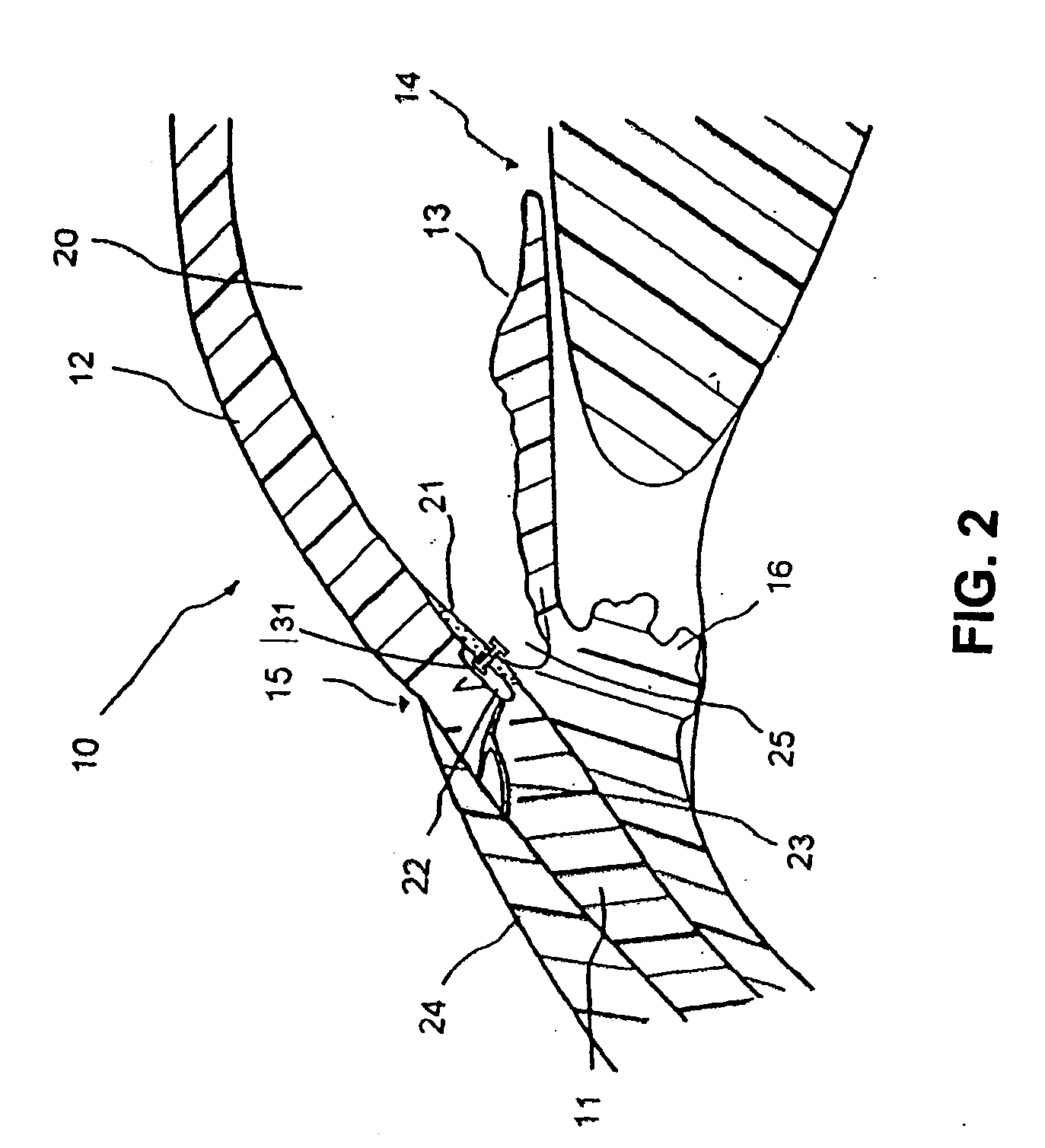
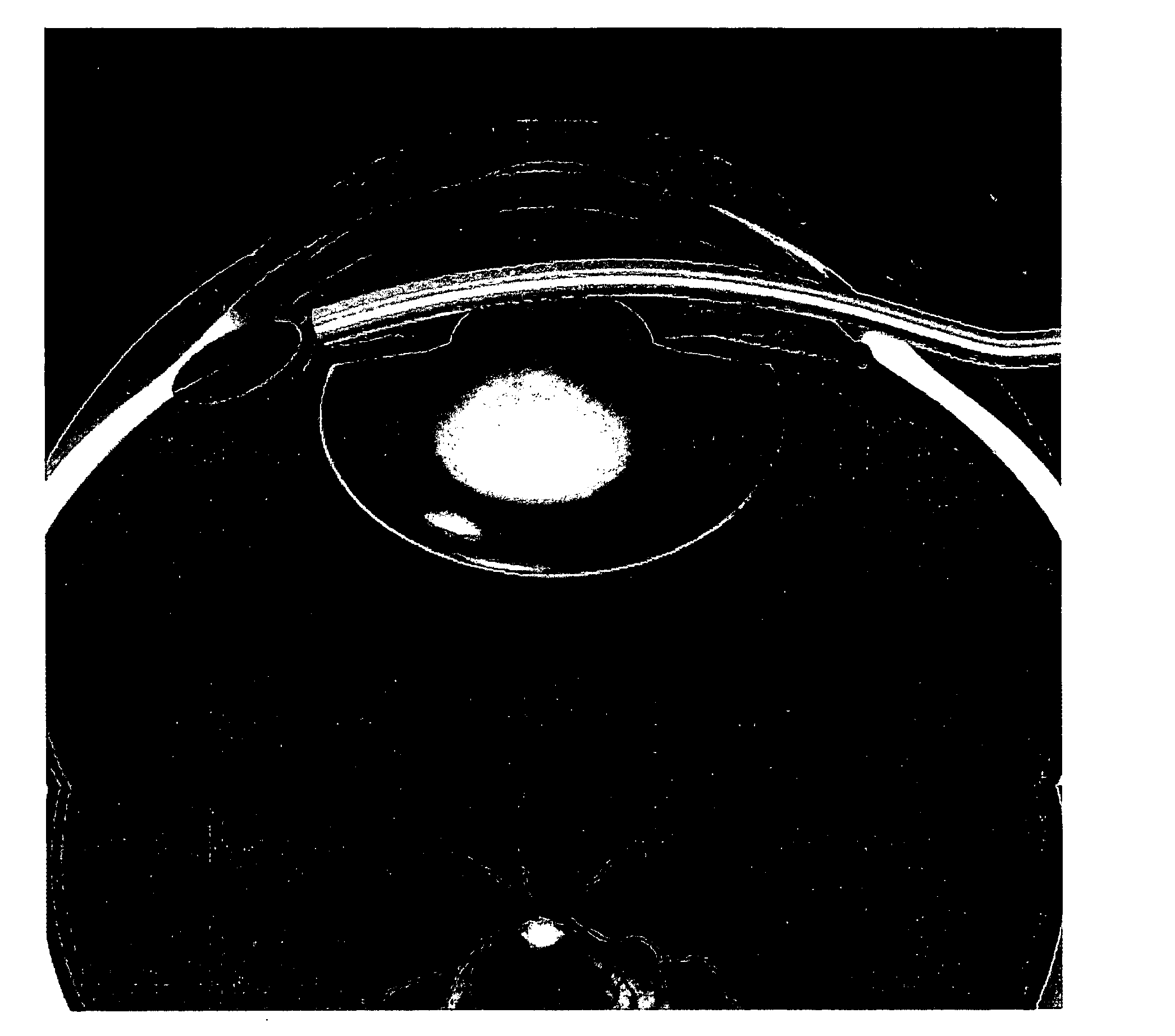
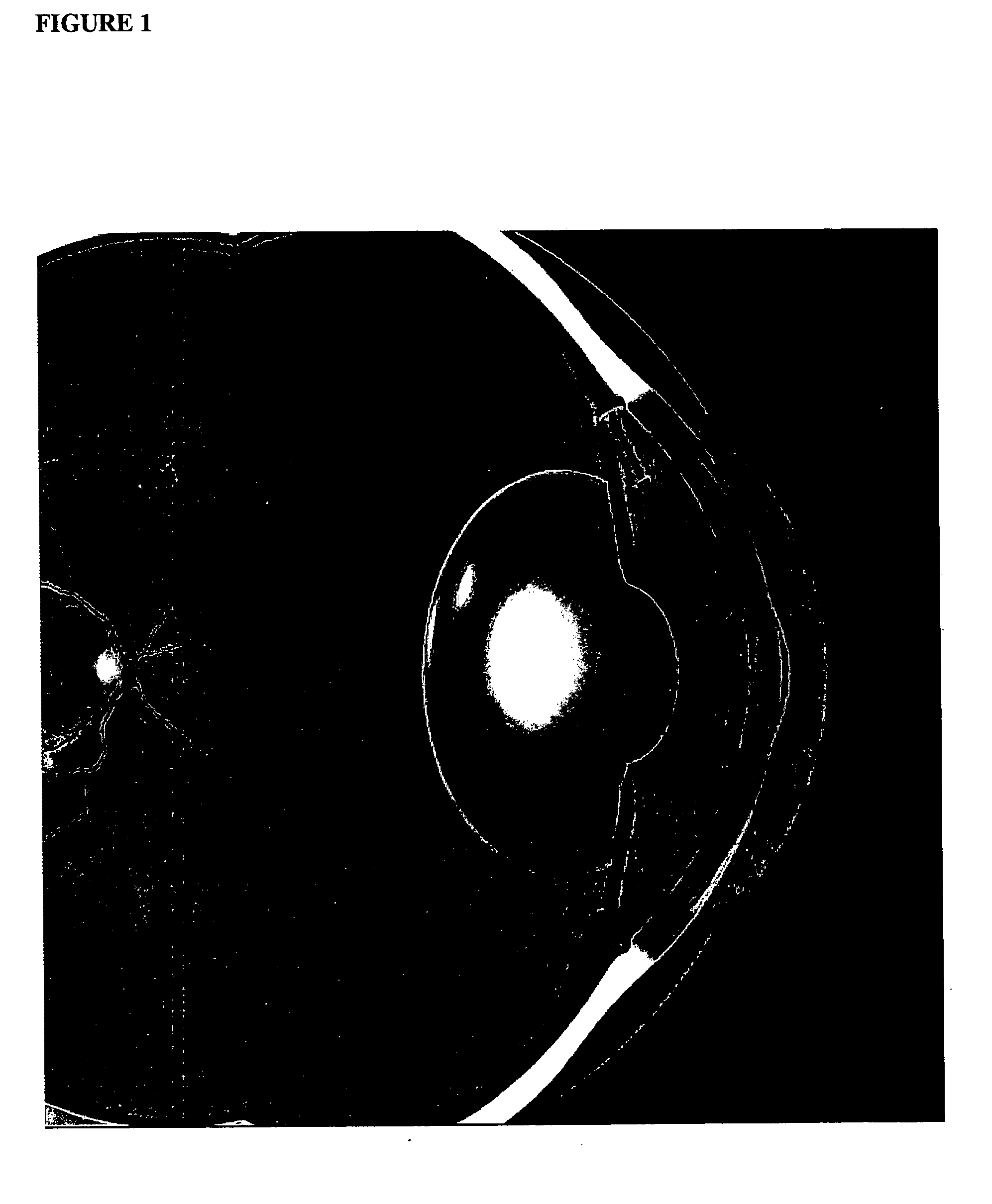
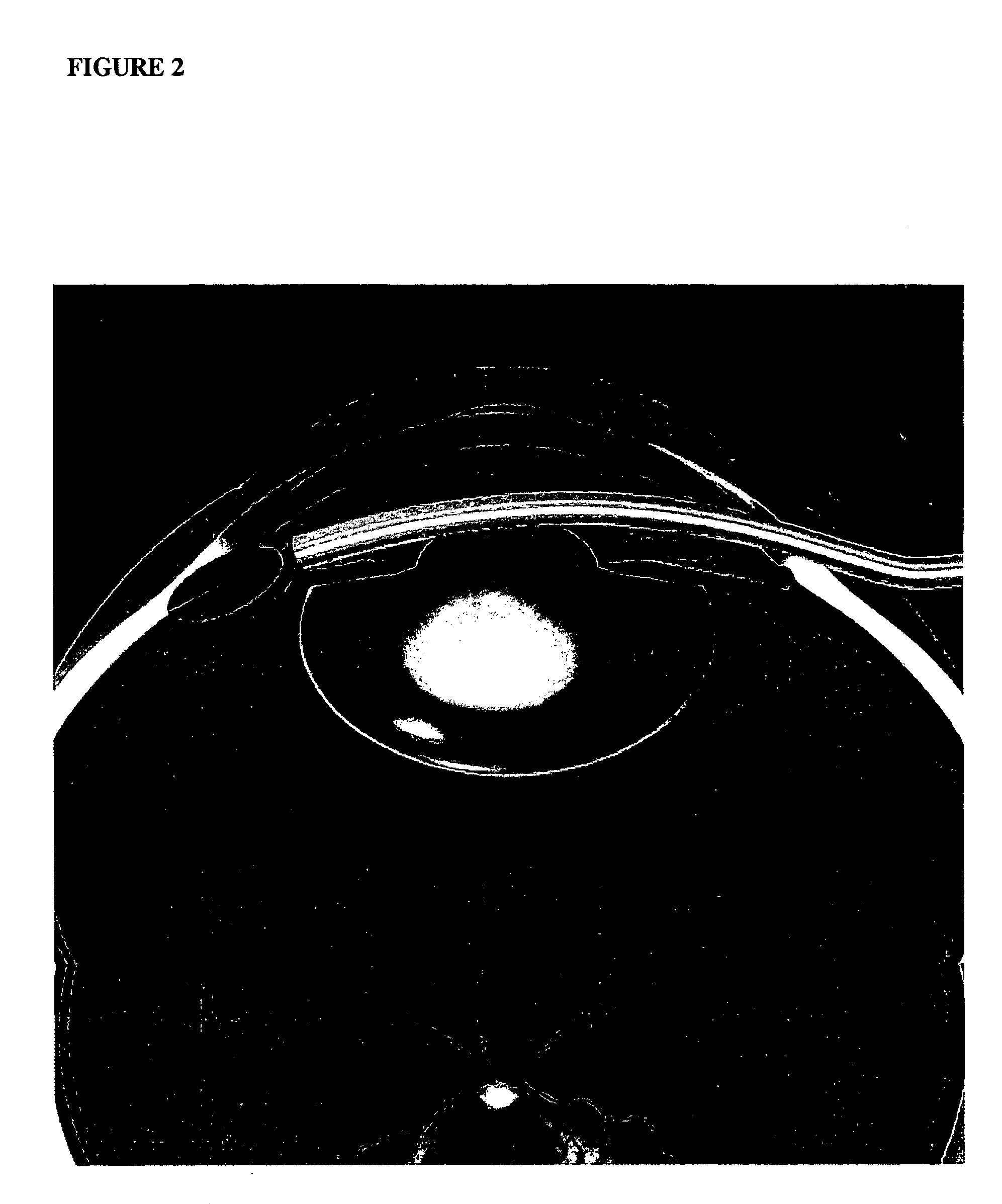
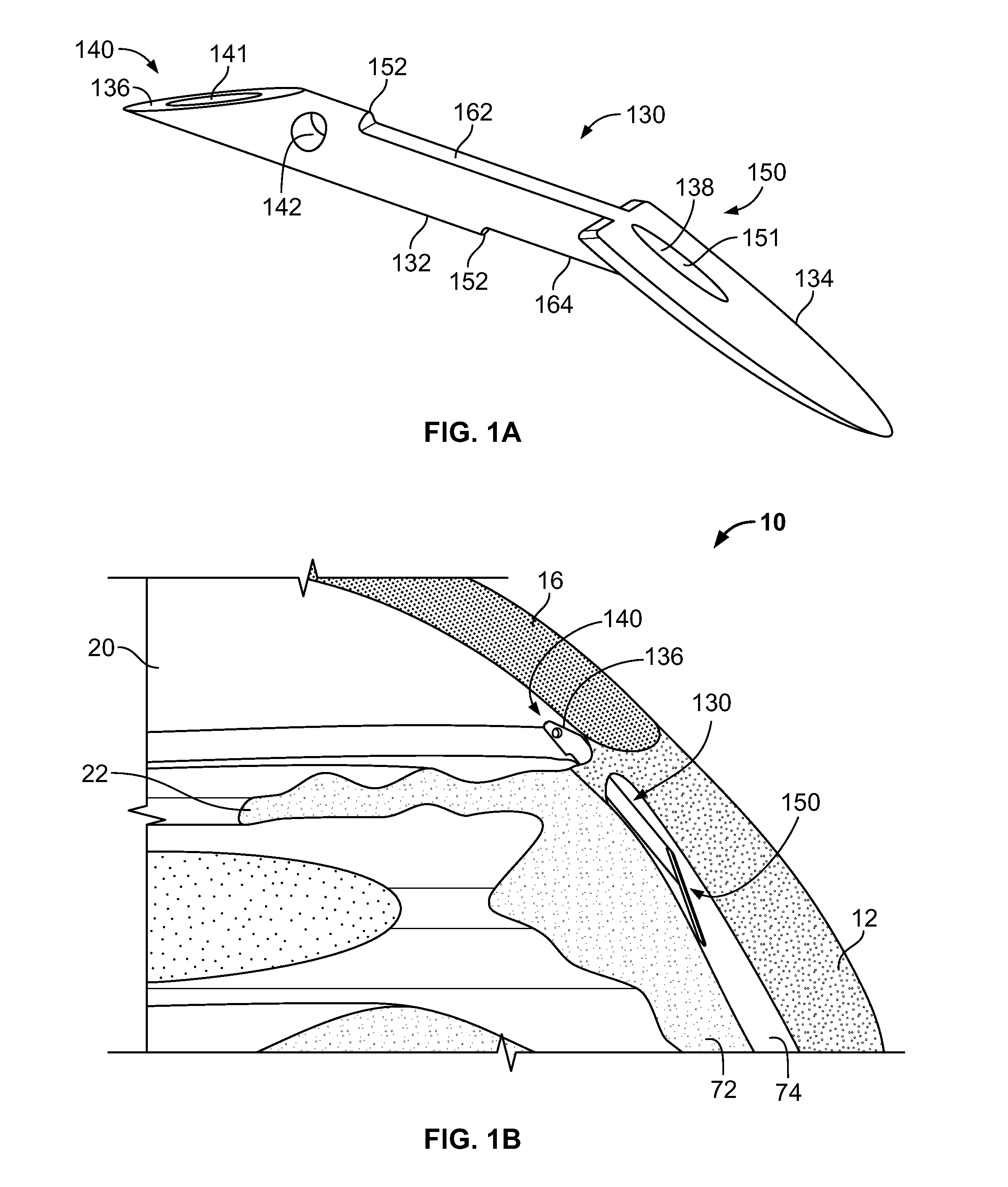
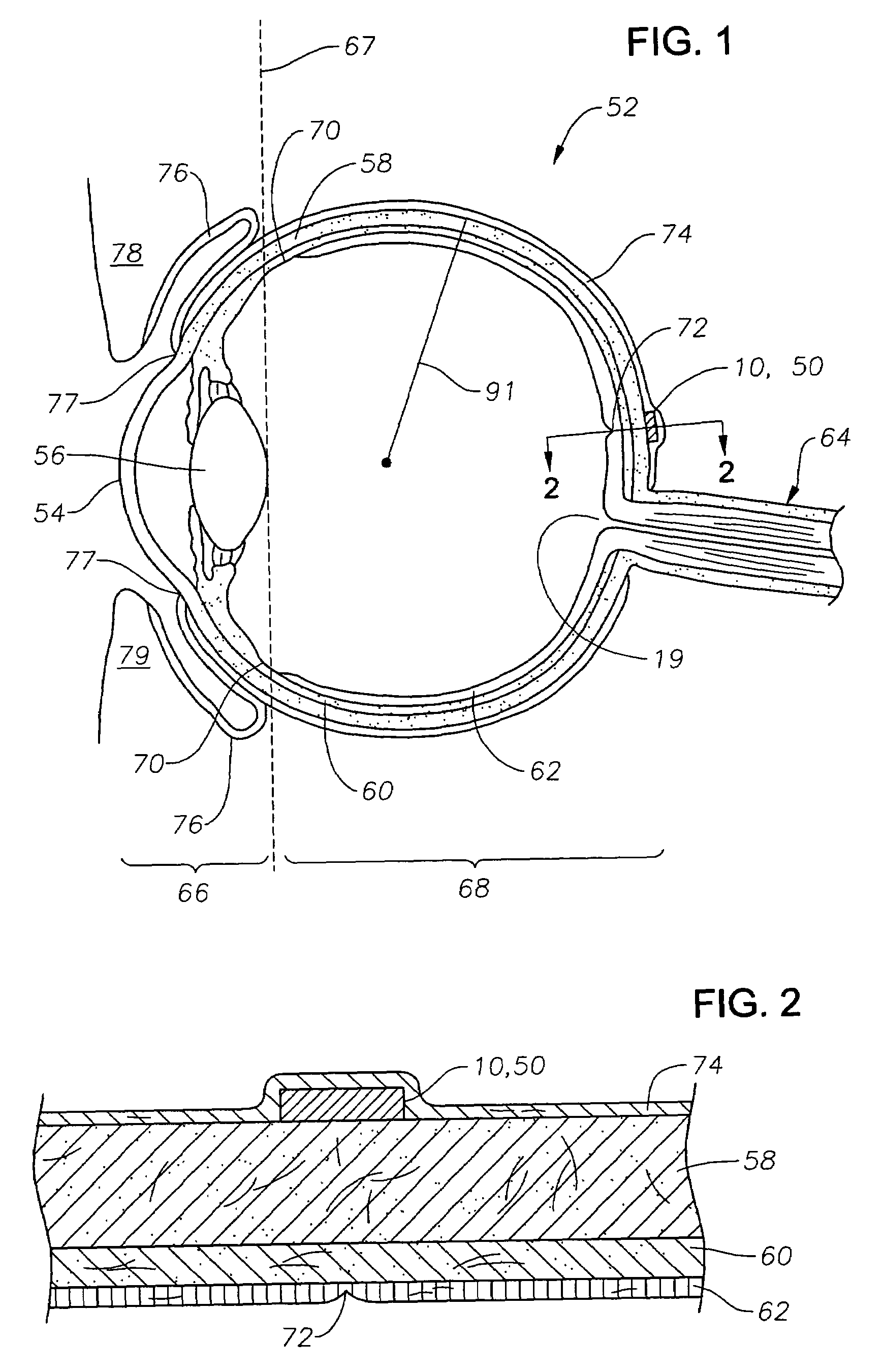
Devices and methods for treating intraocular pressure are disclosed. The devices include shunts for draining aqueous humor from the anterior chamber to the uveoscleral outflow pathway, including the supraciliary space and the suprachoroidal space. The shunts are preferably implanted by ab interno procedures.
Owner:GLAUKOS CORP
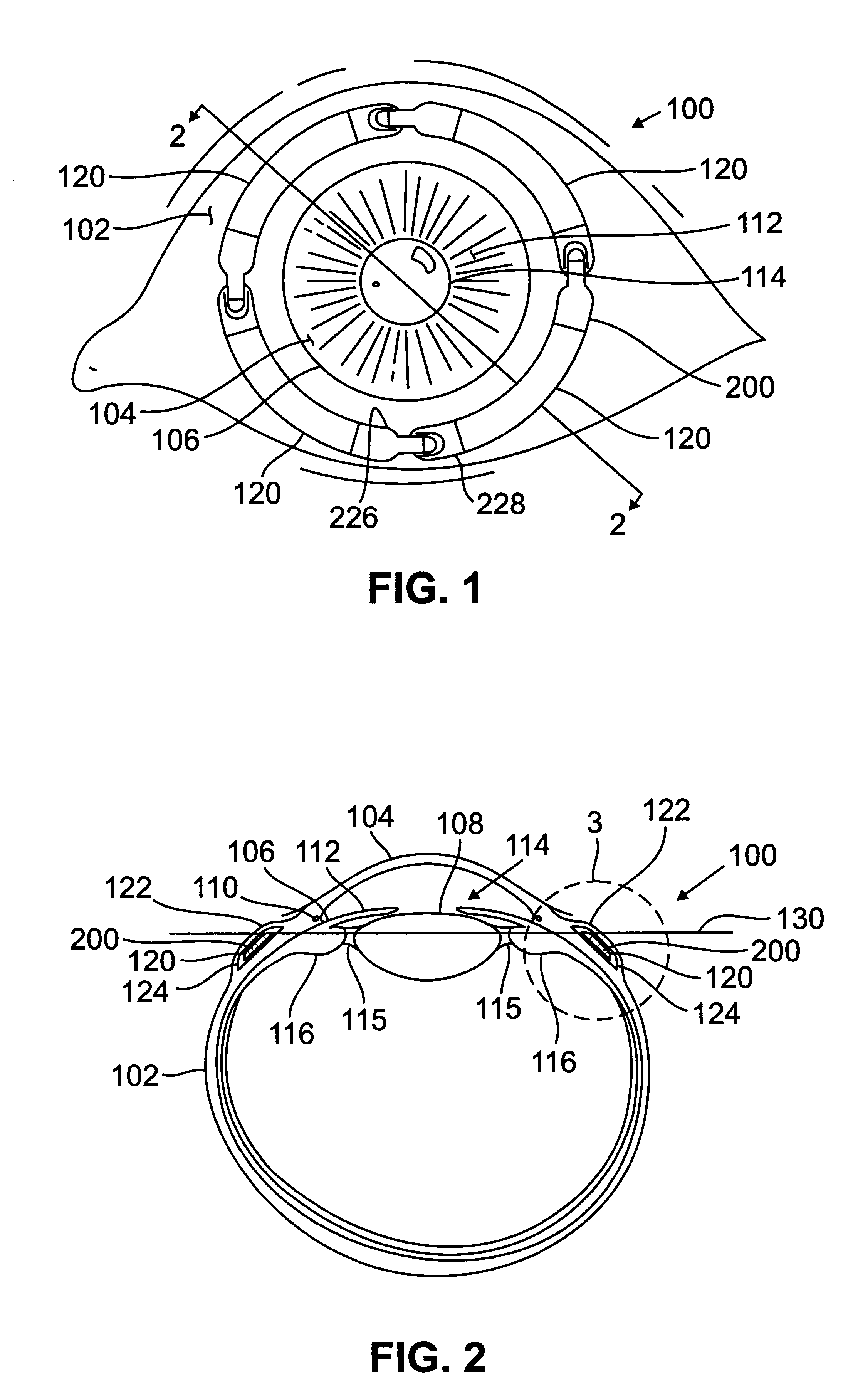
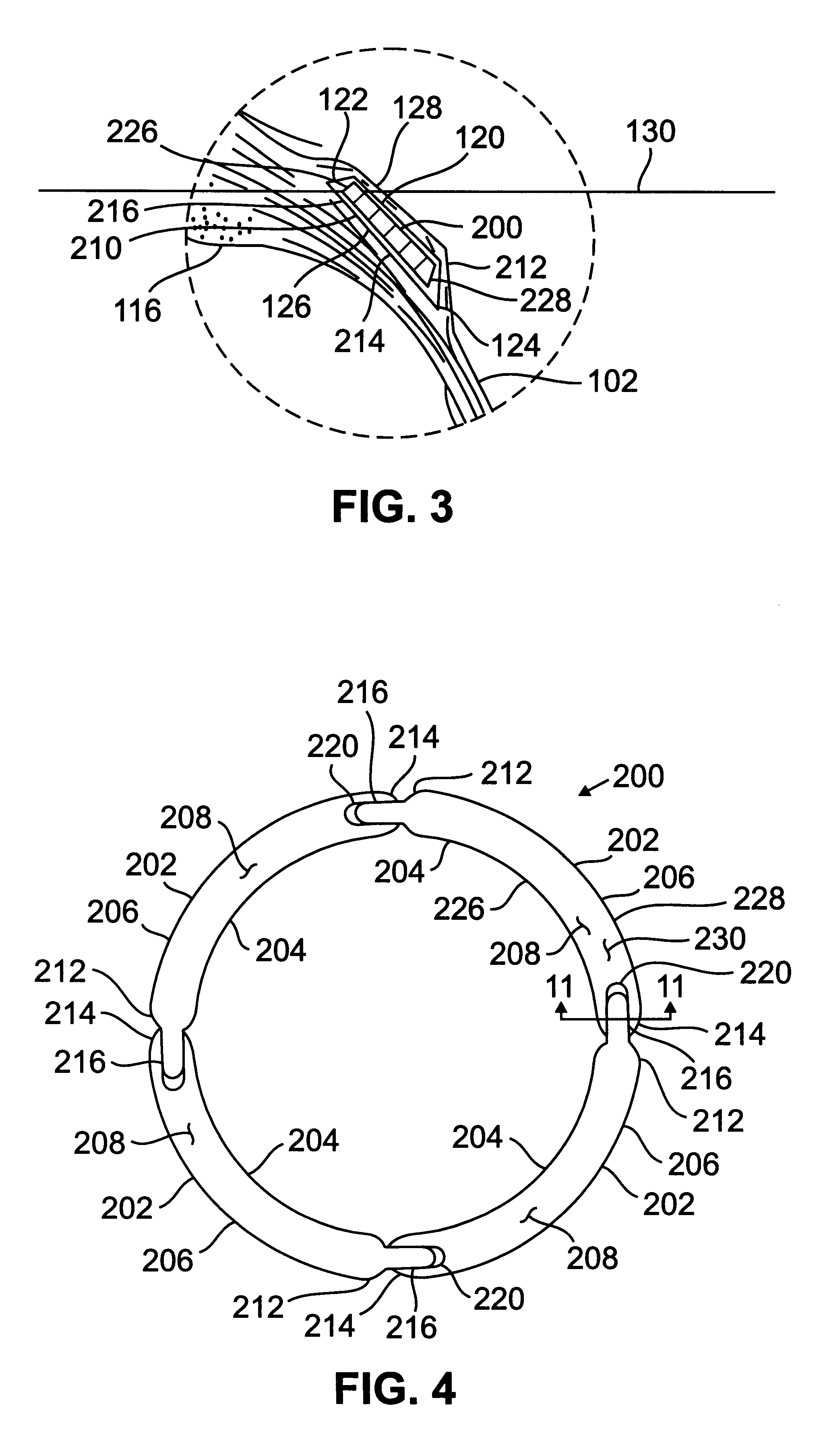
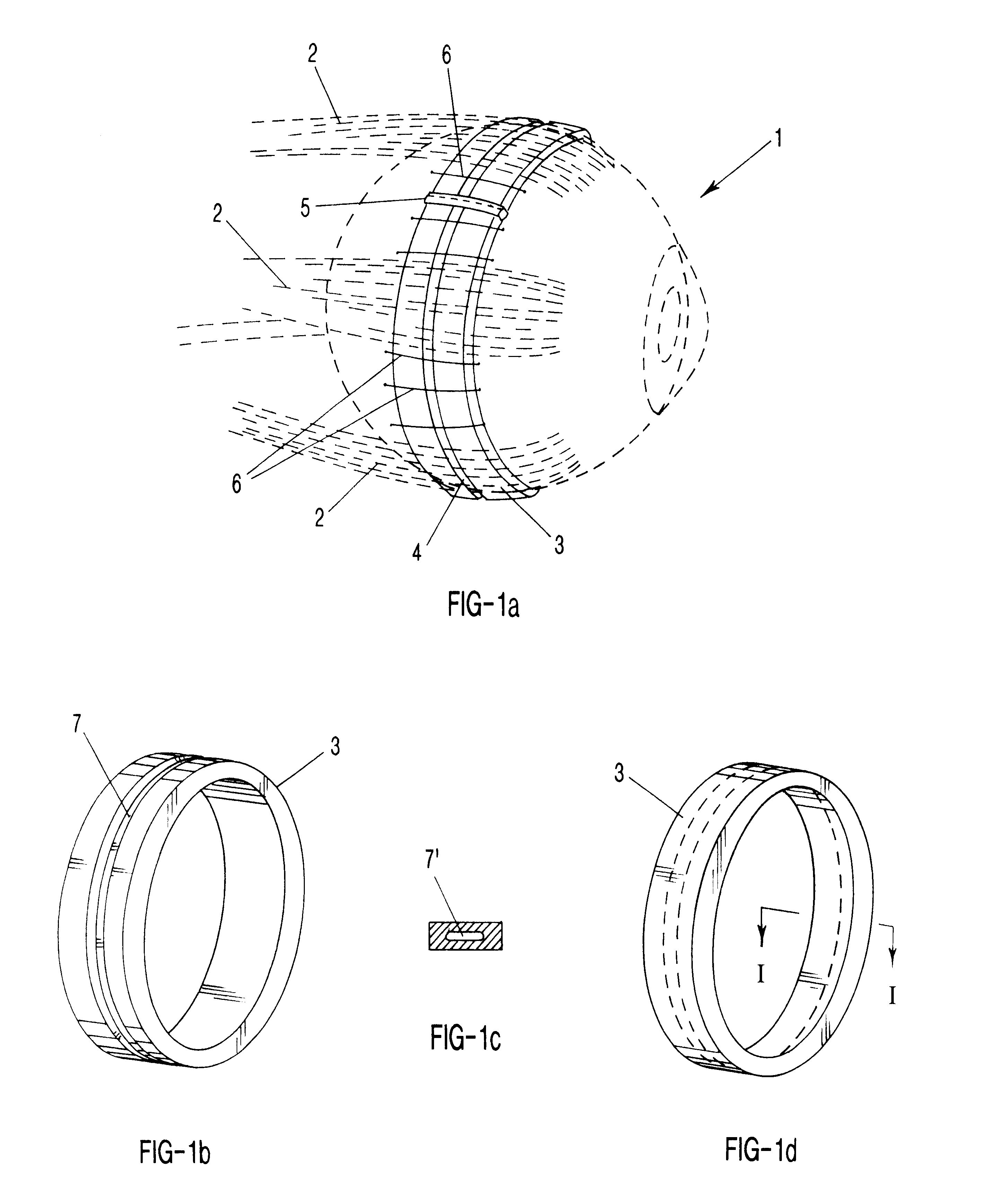
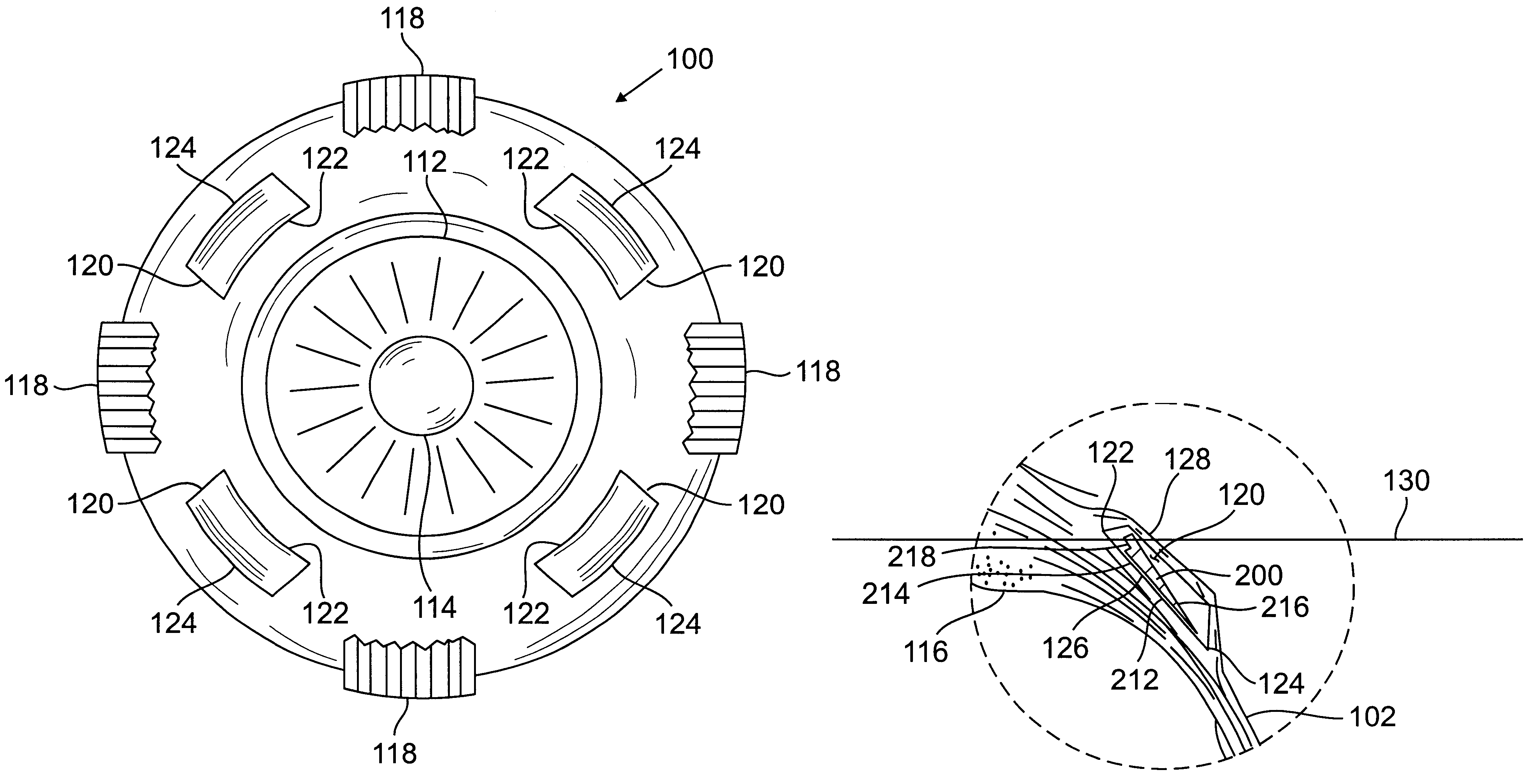
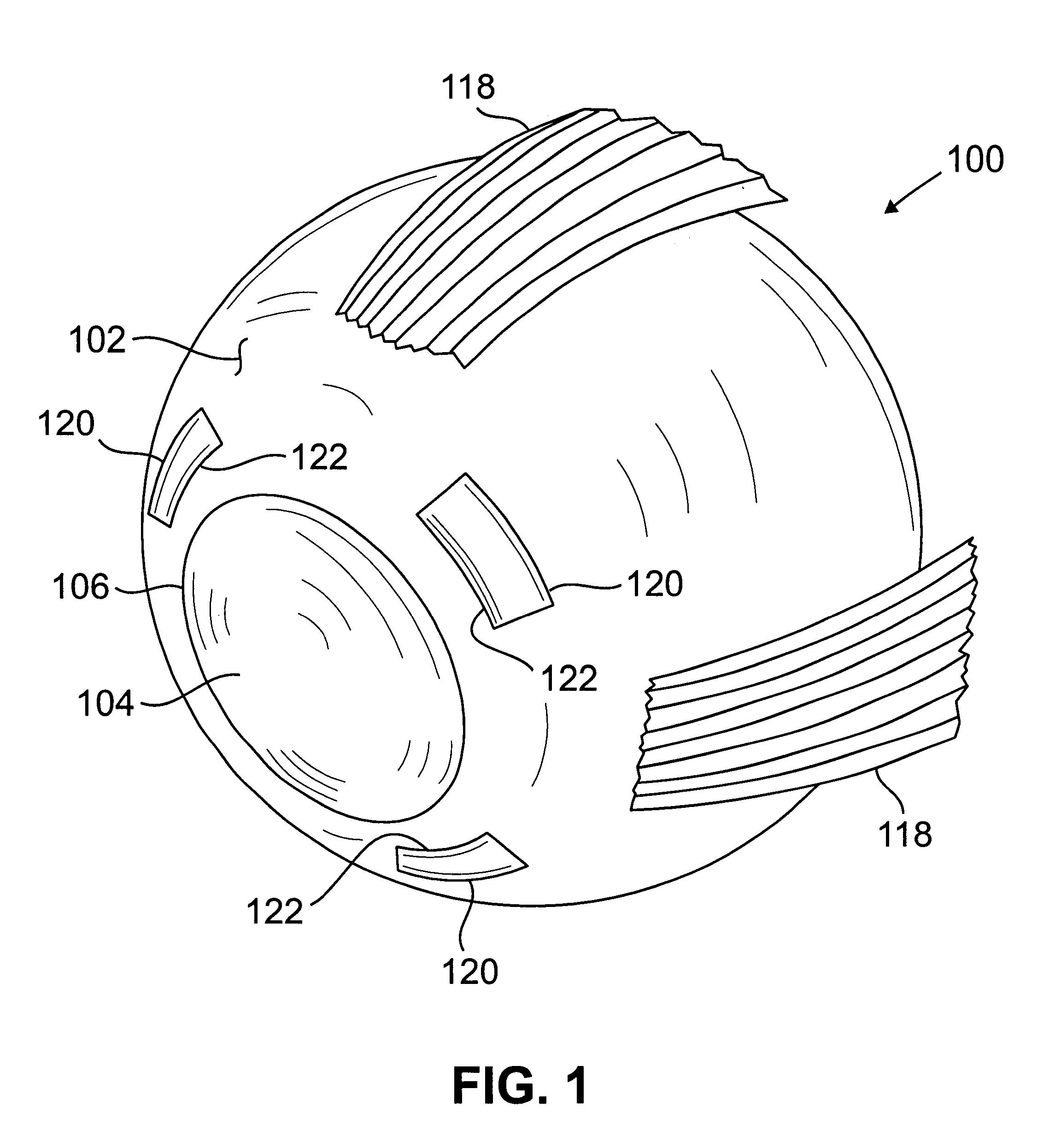
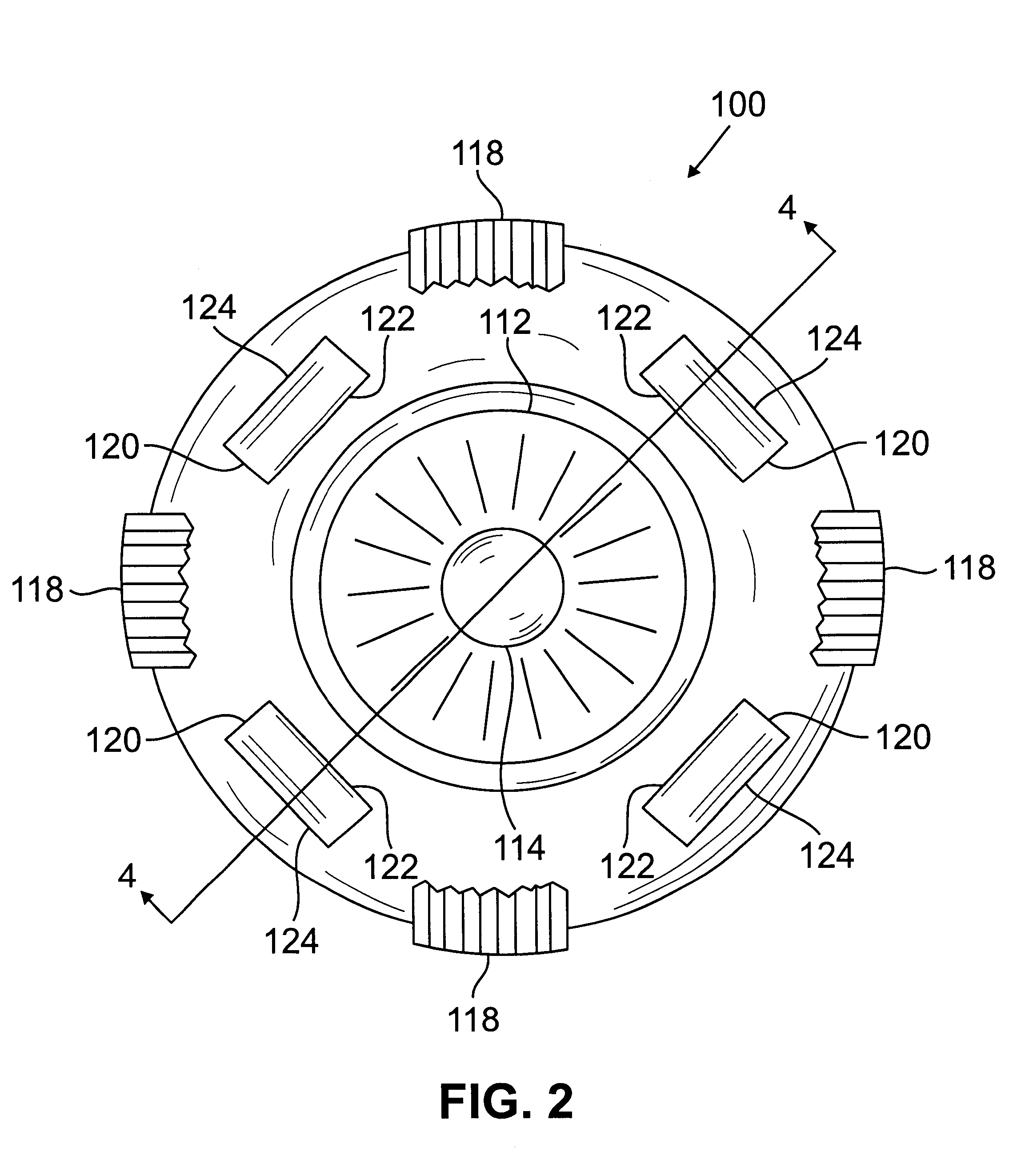
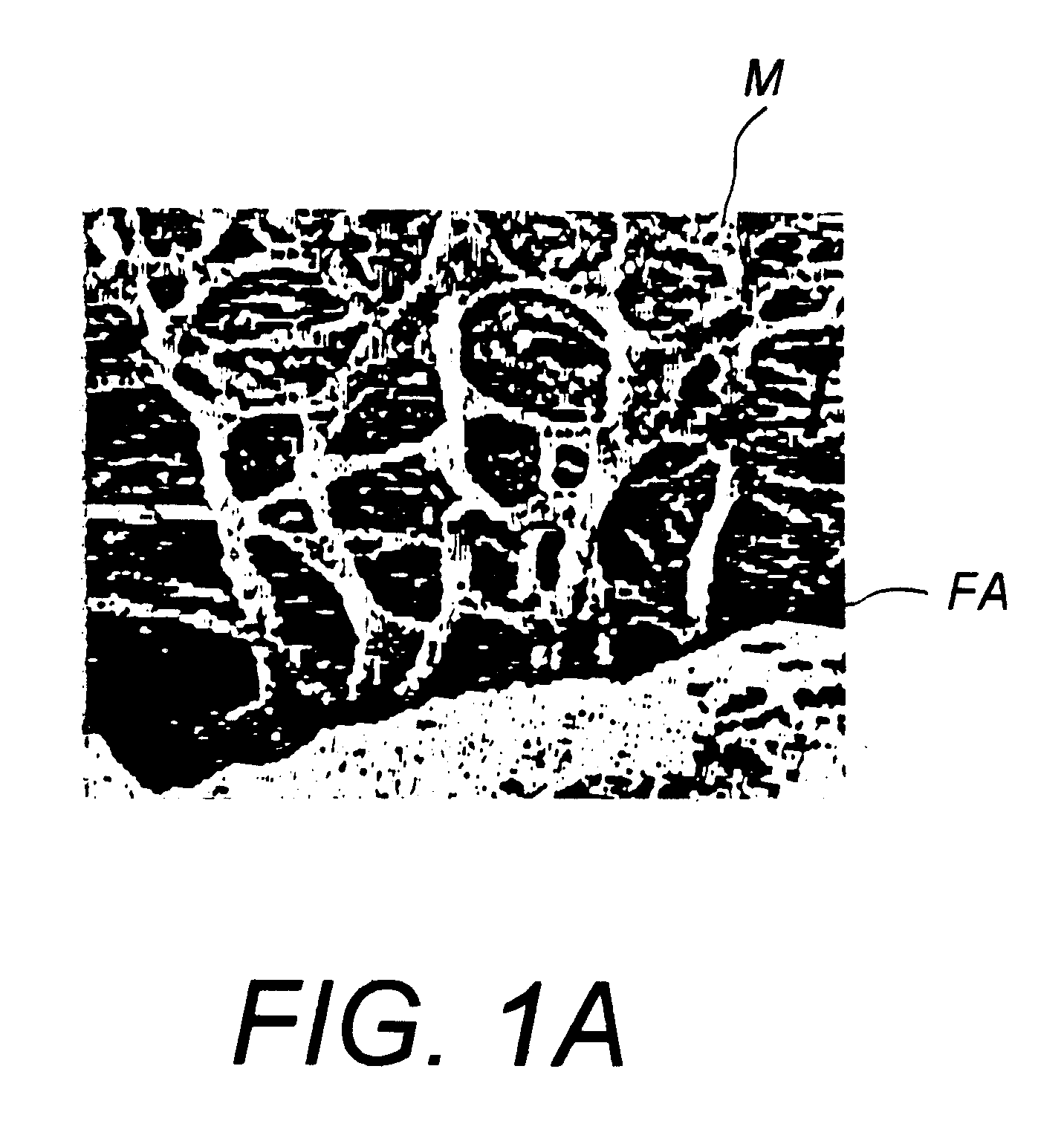
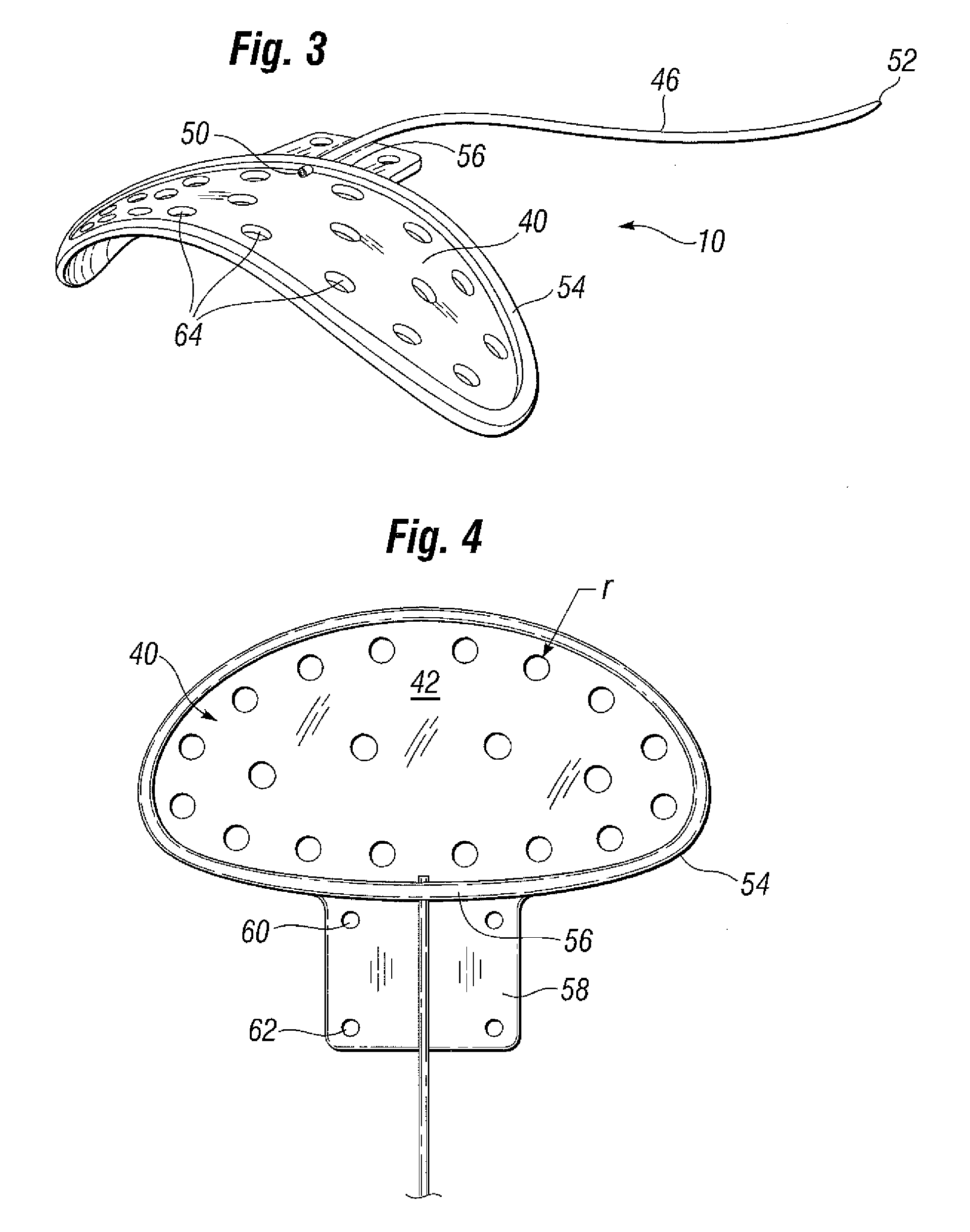
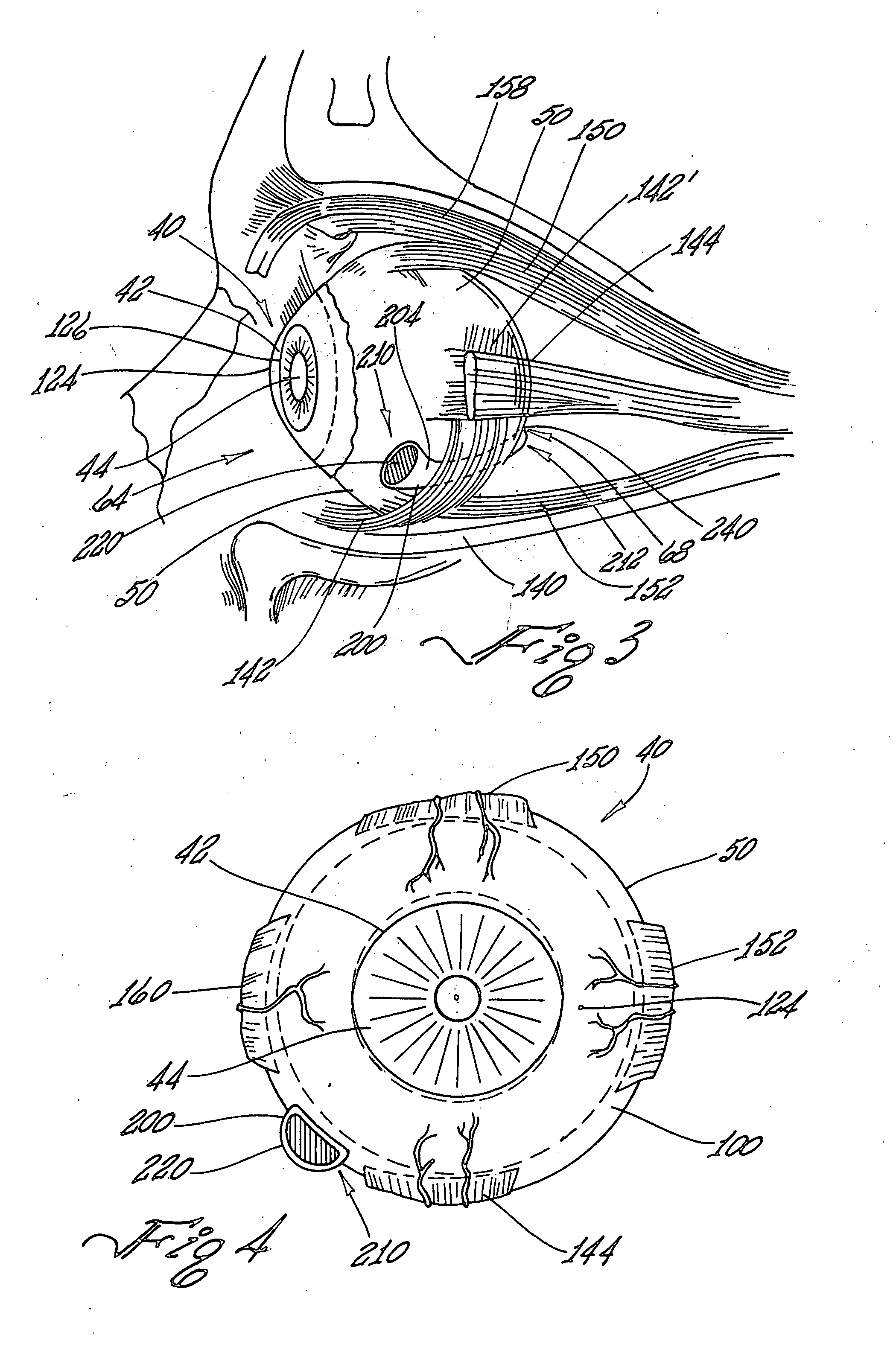
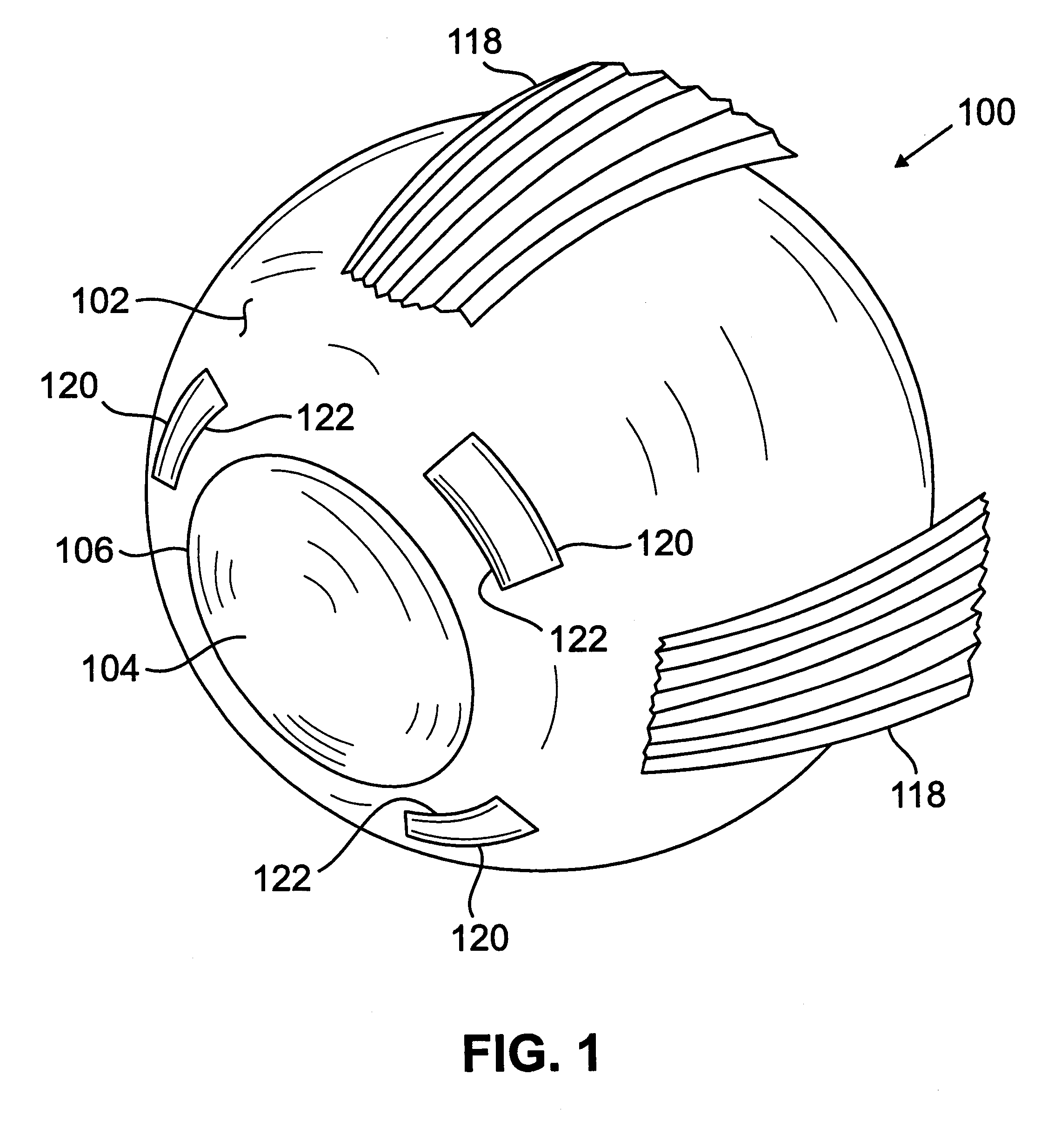
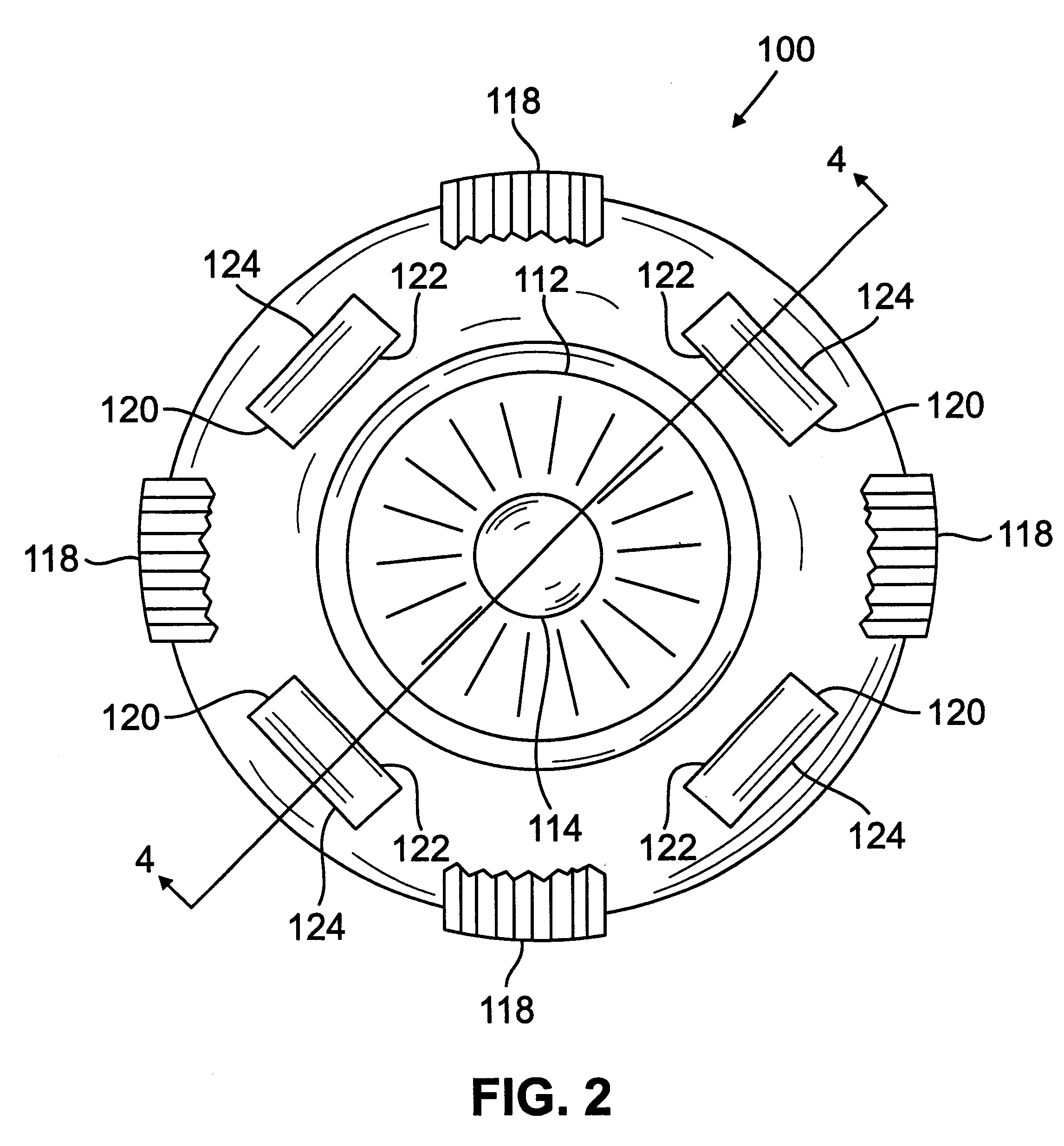
Segmented scleral band for treatment of presbyopia and other eye disorders
InactiveUS6197056B1Increase the effective working distanceLaser surgeryEye implantsDiseaseCiliary body
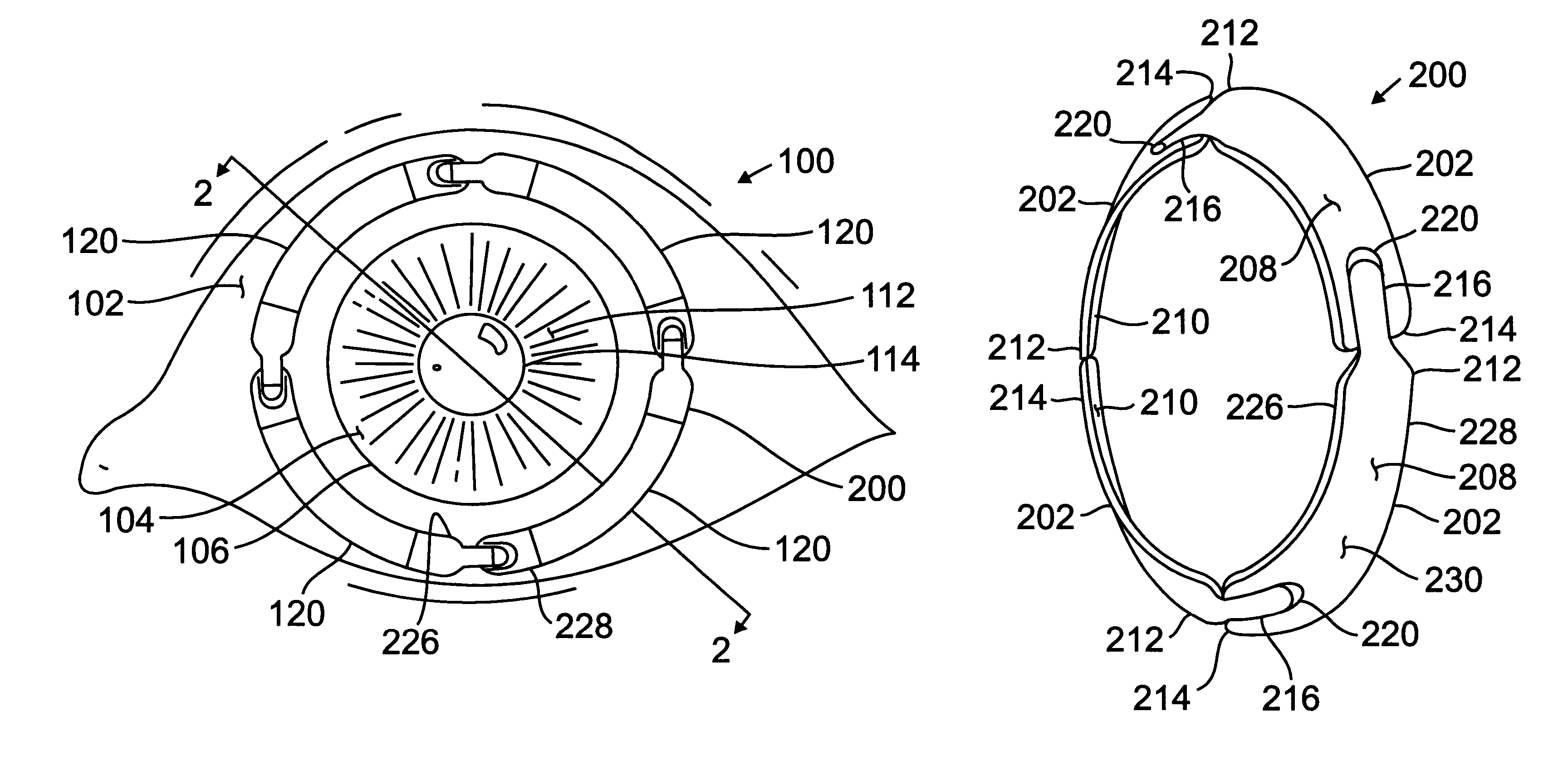
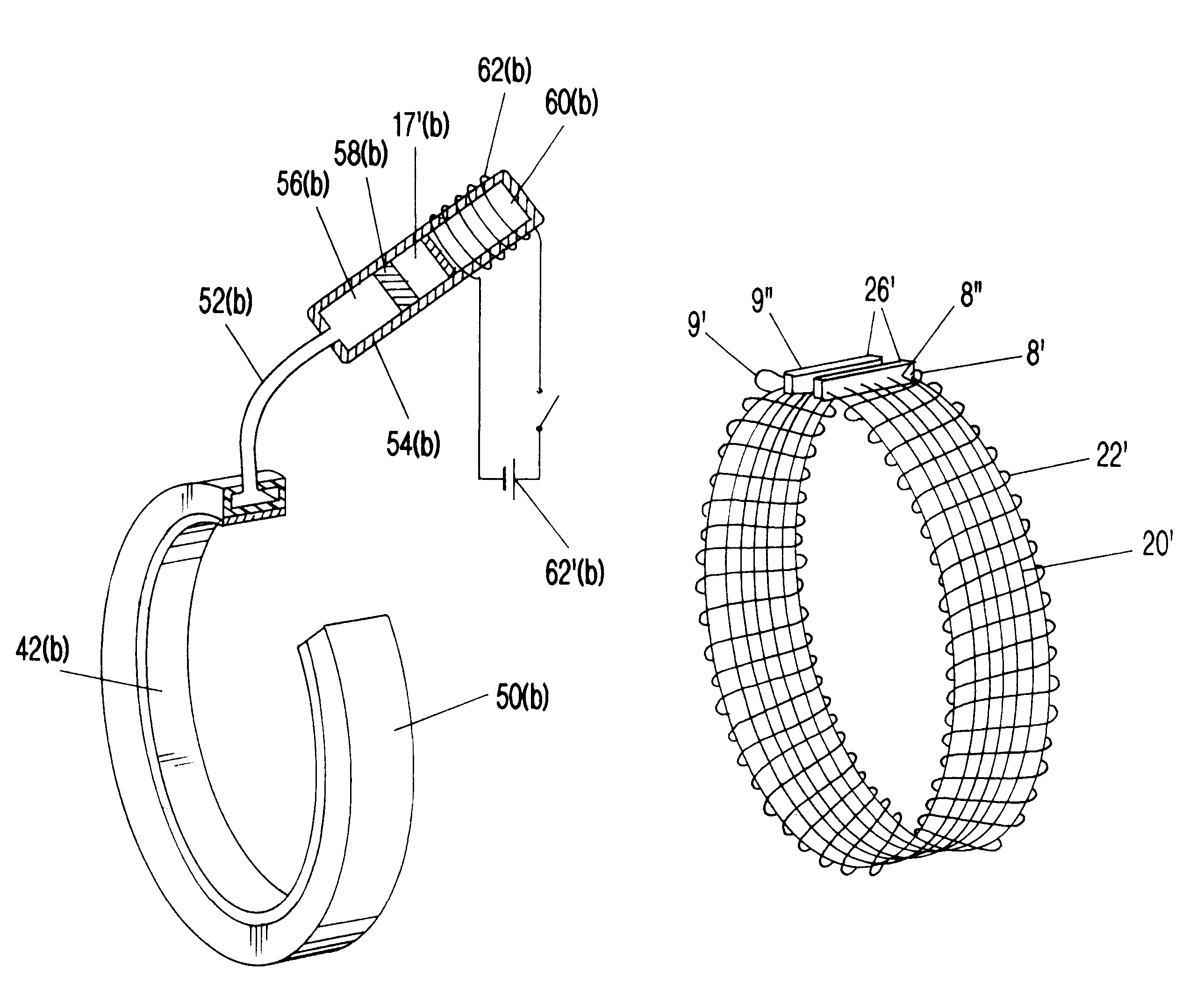
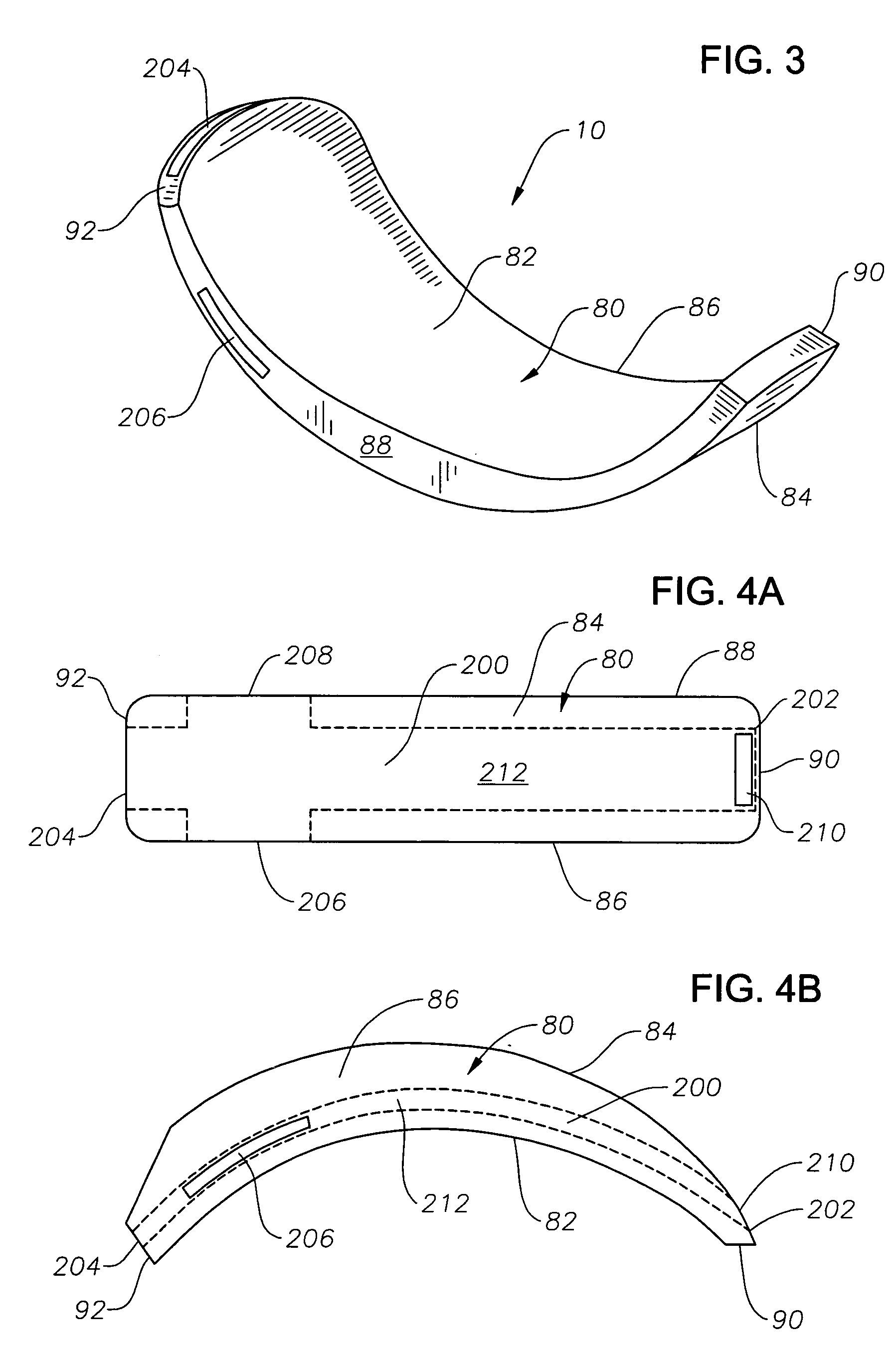
A segmented scleral expansion band adapted for implantation within or fastening to a segment of the sclera of an eye lying outside of and adjacent to the ciliary body of the eye, is formed from a number of arcuate segments, curved to match the curvature of the globe of the eye, and joined together at each end to form a complete scleral expansion band. The band is implanted in the sclera of the eye by forming circumferential tunnels, inserting the band segments through the tunnels, and joining the ends of the segments to form a complete scleral expansion band. The scleral expansion band is useful in treating presbyopia and other ocular disorders.
Owner:REFOCUS OCULAR INC
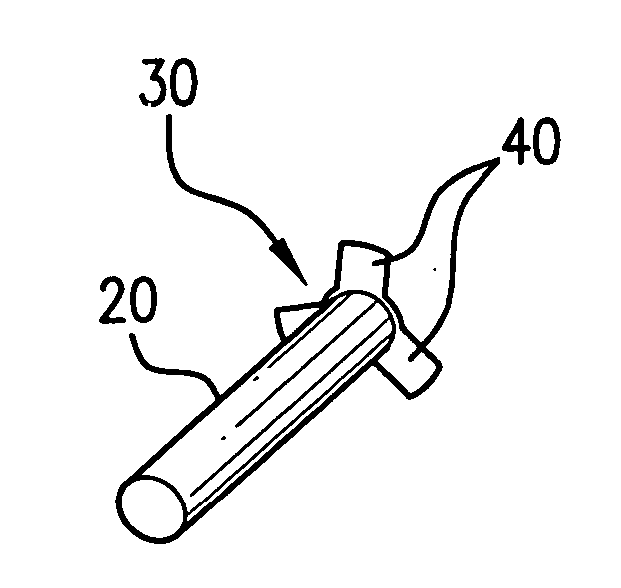
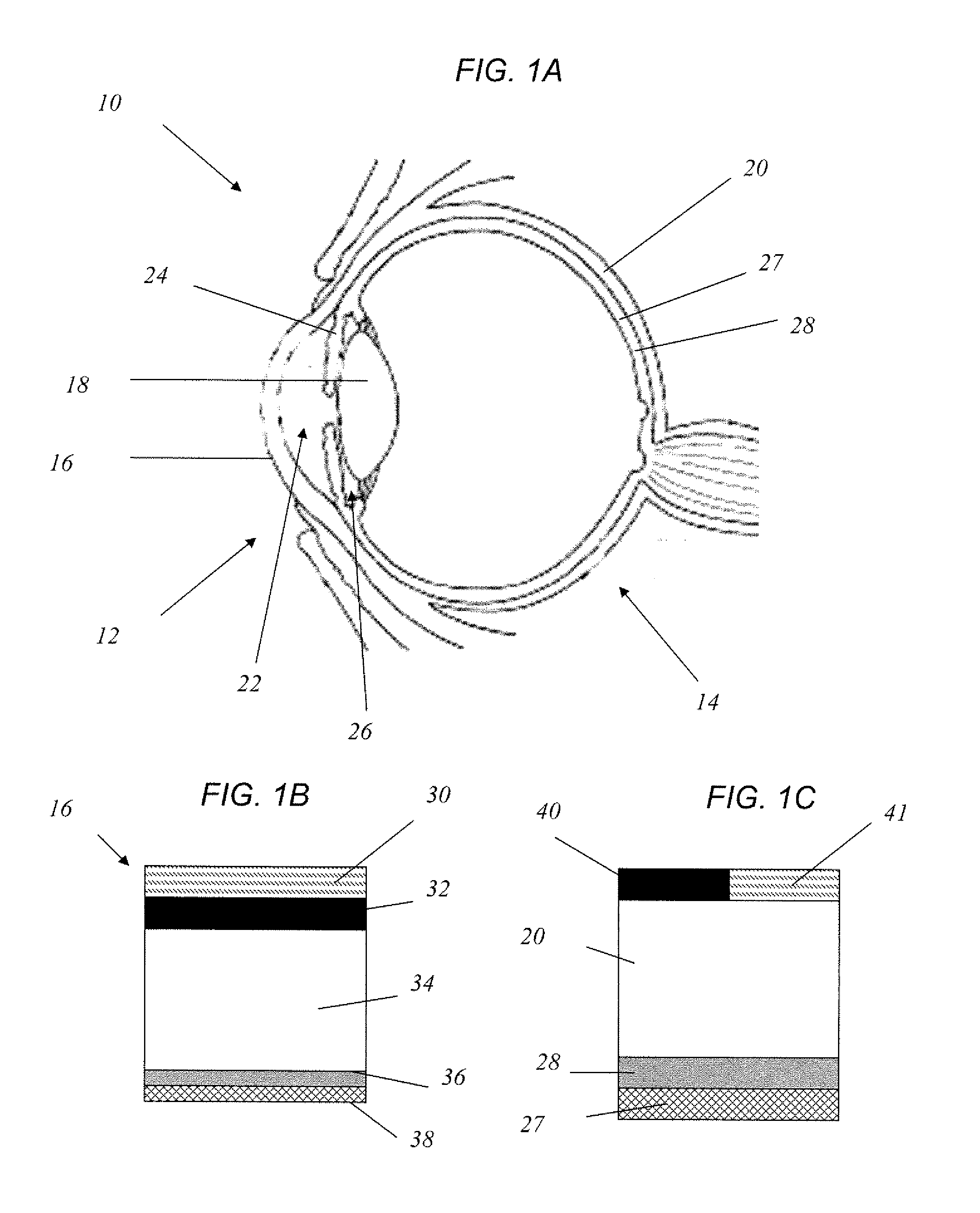
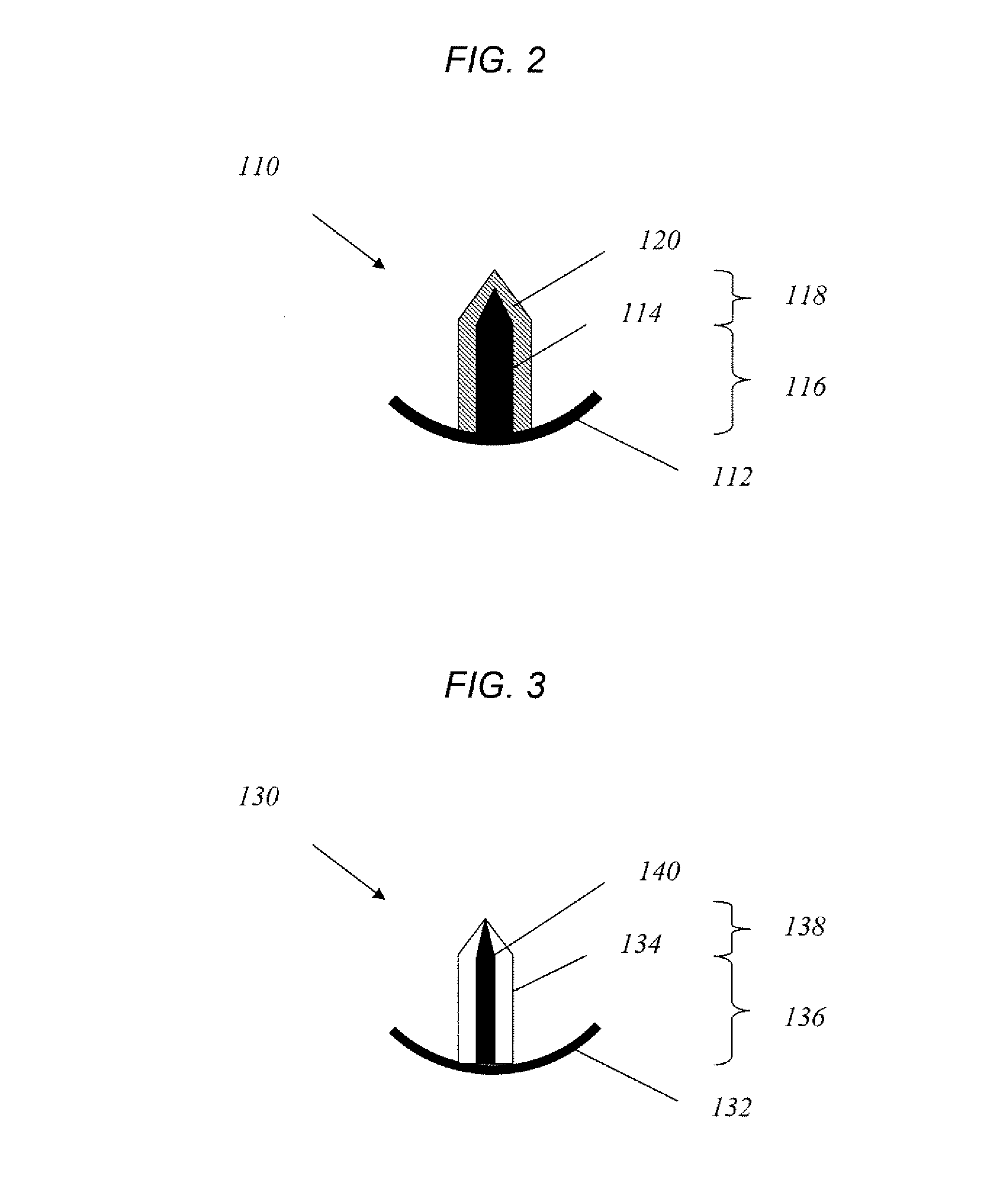
Ocular plug formed from placenta derived collagen biofabric
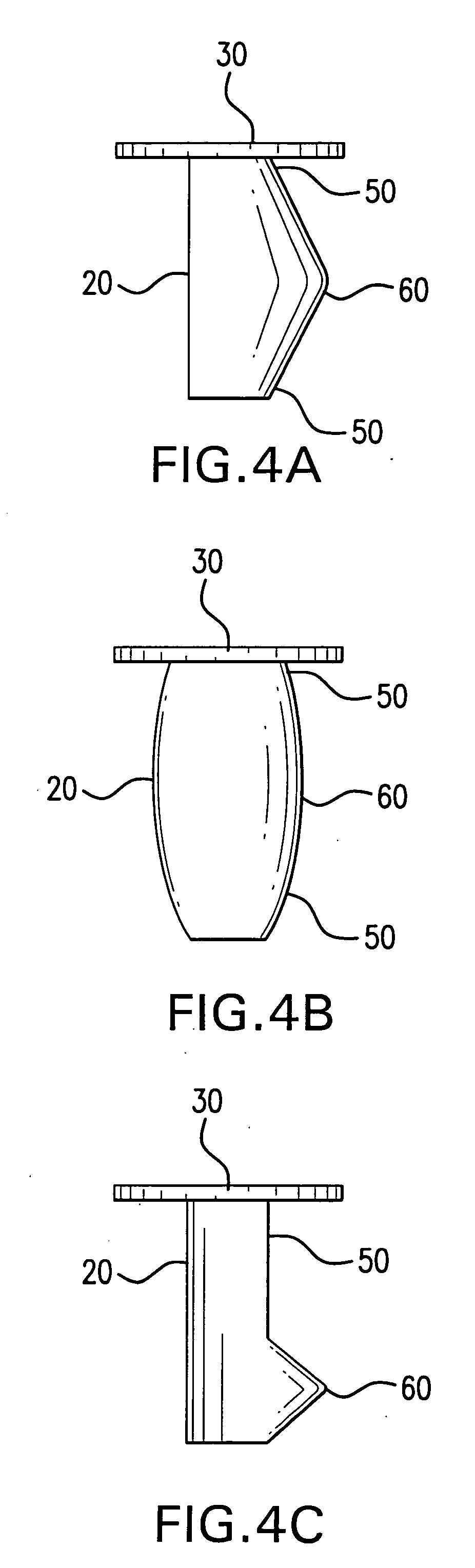
The present invention relates to ocular plugs formed from a biodegradable material. The plugs comprises a shaft and, optionally, a cap. The ocular plugs are intended to occlude, and to repair, discontinuities in the sclera, whether formed deliberately during injection or surgical foray into the eye, or accidentally. The method further provides methods of making the ocular plug. the invention also provides methods of using the ocular plugs to occlude and repair discontinuities in the sclera, or to deliver biologically active compounds to the sclera or the eye. Finally, the invention provides kits comprising one or more ocular plugs in a container.
Owner:LIU QING +1
Contrast-enhanced ocular imaging
The invention relates generally to medical devices and methods for ocular imaging and, more particularly, to devices and methods for increasing contrast in an eye in which an imaging contrast agent is introduced into an aqueous humor outflow channel. For example, in one embodiment, the outflow channel may be Schlemm's Canal, or in another embodiment, the outflow channel may be an episcleral vein. Also disclosed are methods for implanting a trabecular stent via an ab extemo procedure with assistance of enhanced magnetic resonance imaging to restore a part or all of the normal physiological function of directing aqueous outflow for maintaining a normal intraocular pressure in an eye.
Owner:GLAUKOS CORP
Ocular pressure regulation
This invention comprises a flexible ocular device for implantation into the eye formed of a biocompatible elastomeric material, foldable to a diameter of 1.5 mm or less, comprising a fluid drainage tube having at one end a foldable plate adapted to locate the device on the inner surface of the sclera in a suprachoroidal space formed by cyclodialysis, said drainage tube opening onto the disc at one end and opening to the anterior chamber when implanted into the eye at its other end, so as to provide aqueous pressure regulation. Also provided are methods for the treatment of glaucoma utilising the flexible ocular device, and an ocular pressure spike shunt.
Owner:ALCON INC
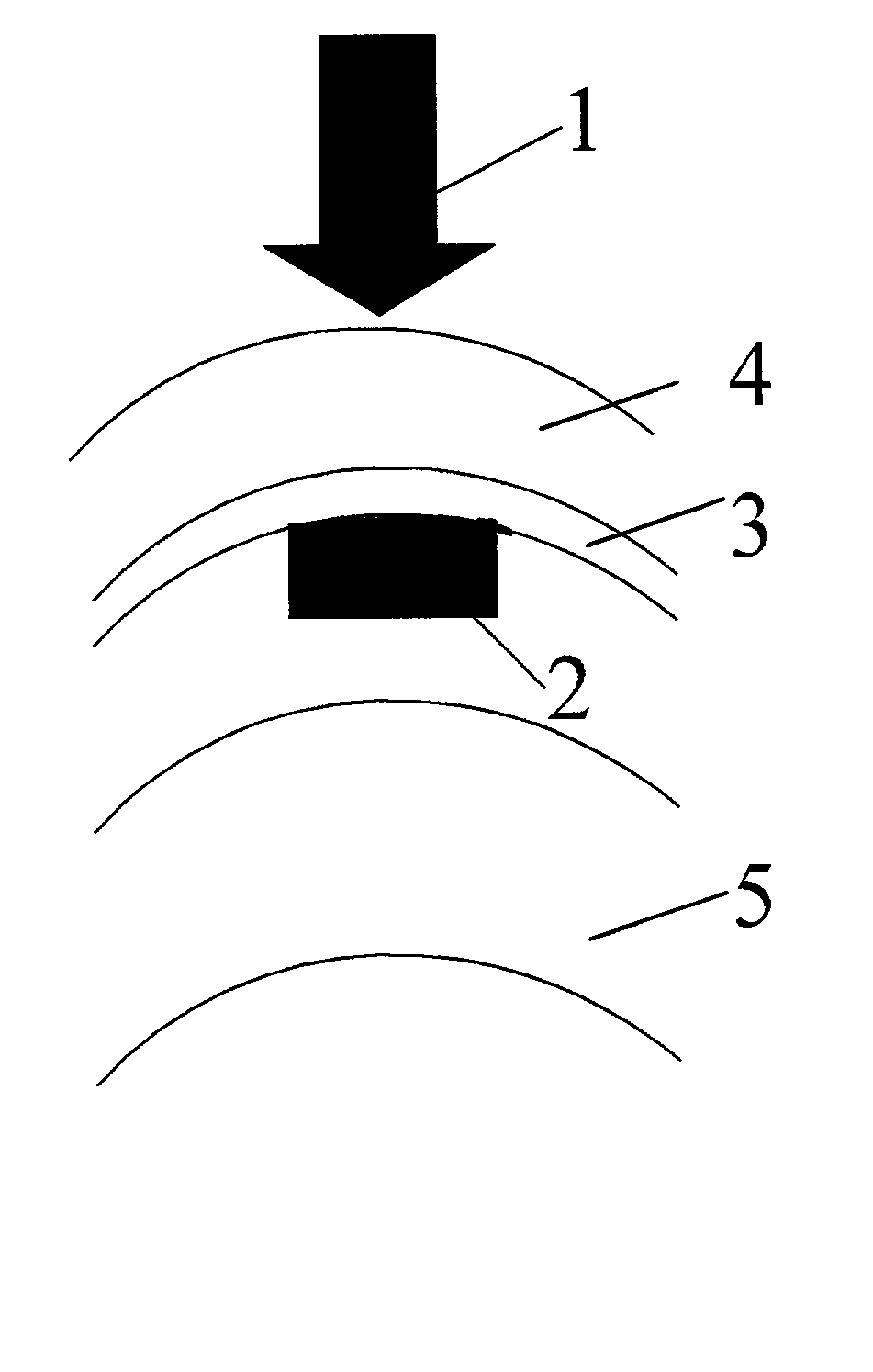
Surgical correction of human eye refractive errors by active composite artificial muscle implants
Surgical correction of human eye refractive errors such as presbyopia, hyperopia, myopia, and stigmatism by using transcutaneously inductively energized artificial muscle implants to either actively change the axial length and the anterior curvatures of the eye globe. This brings the retina / macula region to coincide with the focal point. The implants use transcutaneously inductively energized scleral constrictor bands equipped with composite artificial muscle structures. The implants can induce enough accommodation of a few diopters, to correct presbyopia, hyperopia, and myopia on demand. In the preferred embodiment, the implant comprises an active sphinctering smart band to encircle the sclera, preferably implanted under the conjunctiva and under the extraocular muscles to uniformly constrict the eye globe, similar to a scleral buckle band for surgical correction of retinal detachment, to induce active temporary myopia (hyperopia) by increasing (decreasing) the active length of the globe. In another embodiment, multiple and specially designed constrictor bands can be used to enable surgeons to correct stigmatism. The composite artificial muscles are either resilient composite shaped memory alloy-silicone rubber implants in the form of endless active scleral bands, electroactive ionic polymeric artificial muscle structures, electrochemically contractile endless bands of ionic polymers such as polyacrylonitrile (PAN), thermally contractile liquid crystal elastomer artificial muscle structures, magnetically deployable structures or solenoids or other deployable structures equipped with smart materials such as preferably piezocerams, piezopolymers, electroactive and eletrostrictive polymers, magnetostrictive materials, and electro or magnetorheological materials.
Owner:ENVIRONMENTAL ROBOTS
Apparatus and formulations for suprachoroidal drug delivery
InactiveUS20070202186A1Avoid traumaMinimally-invasive deliveryBiocidePowder deliveryPosterior regionPharmaceutical formulation
Drug formulations, devices and methods are provided to deliver biologically active substances to the eye. The formulations are delivered into scleral tissues adjacent to or into the suprachoroidal space without damage to the underlying choroid. One class of formulations is provided wherein the formulation is localized in the suprachoroidal space near the region into which it is administered. Another class of formulations is provided wherein the formulation can migrate to another region of the suprachoroidal space, thus allowing an injection in the anterior region of the eye in order to treat the posterior region.
Owner:CLEARSIDE BIOMEDICAL
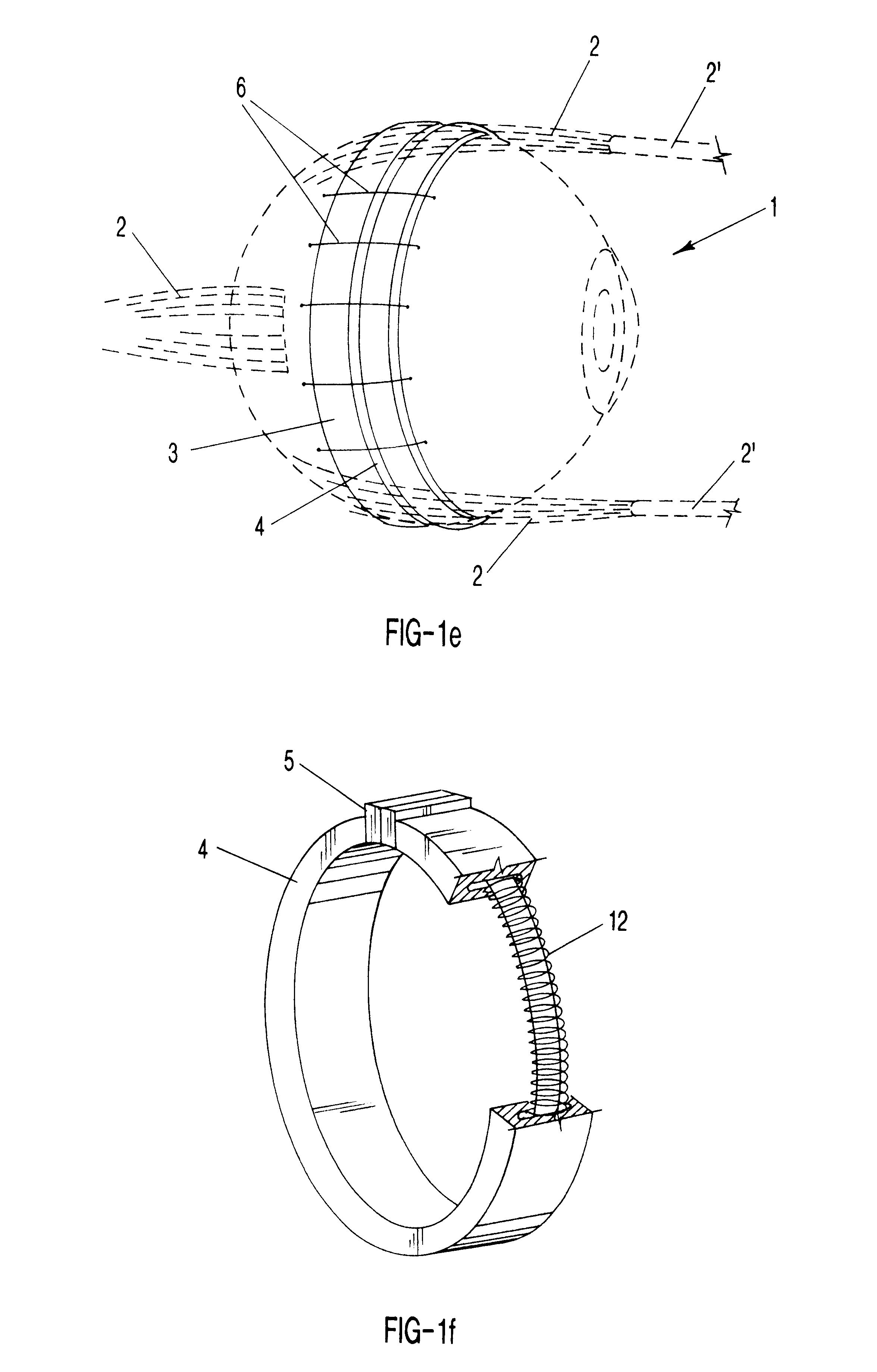
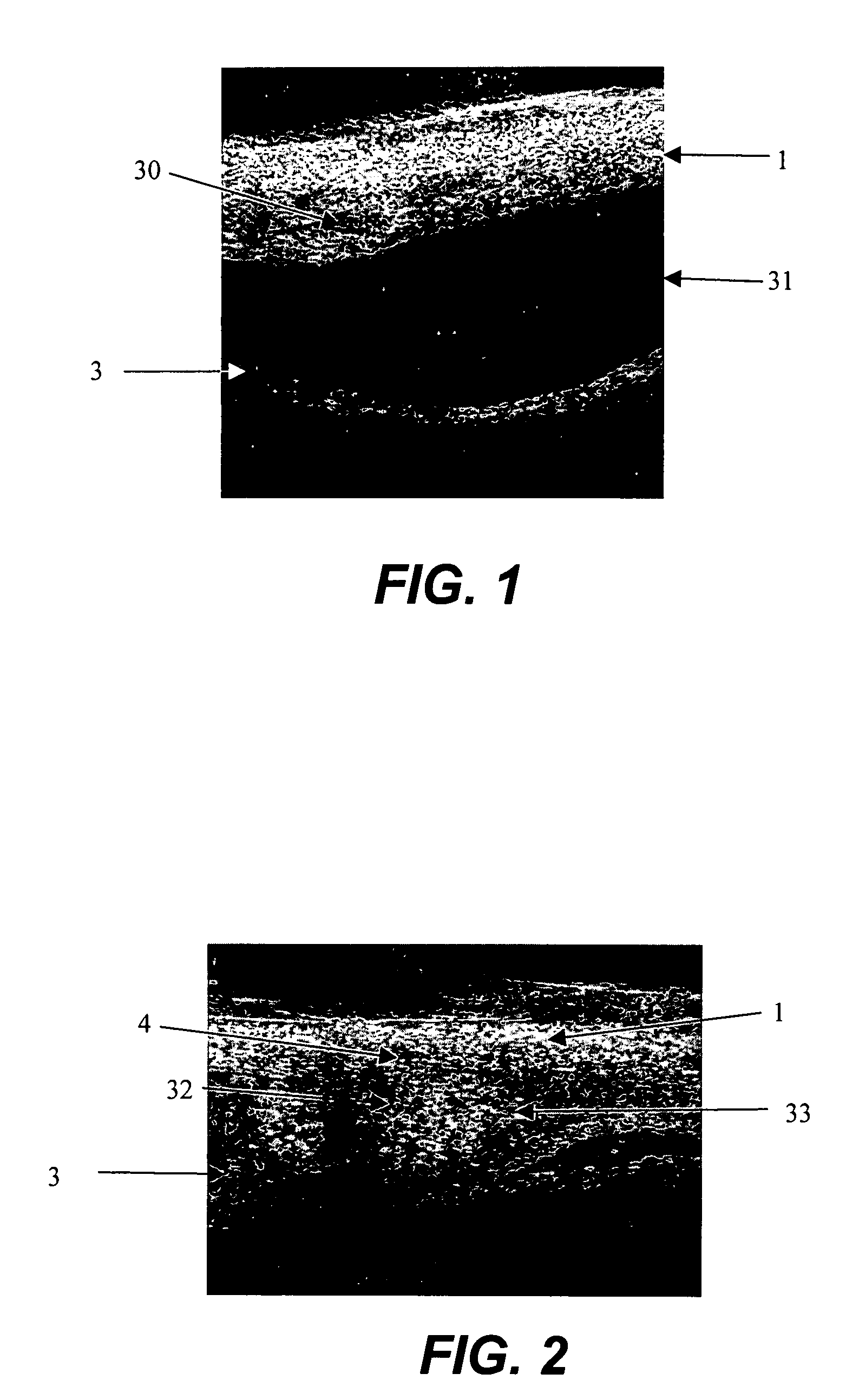
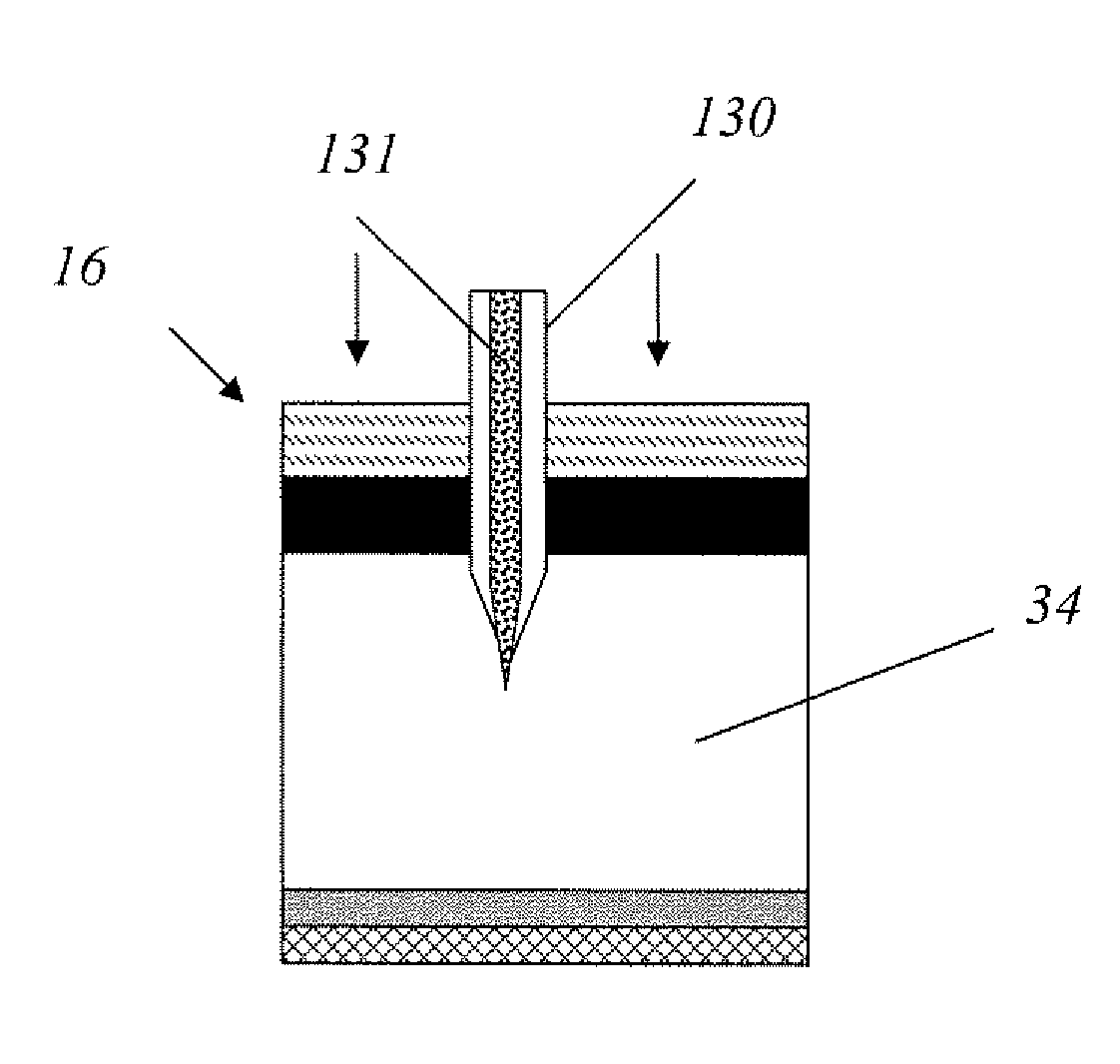
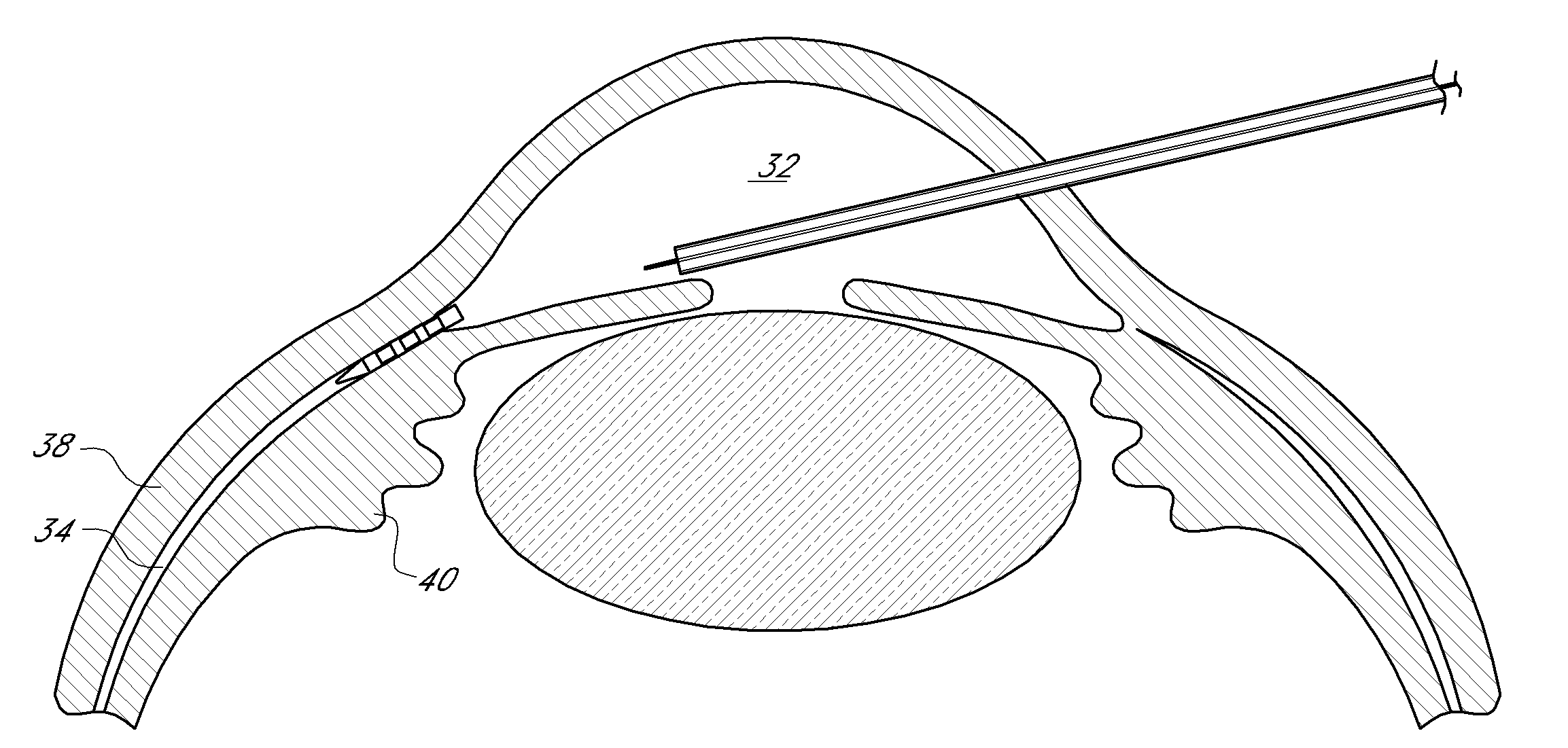
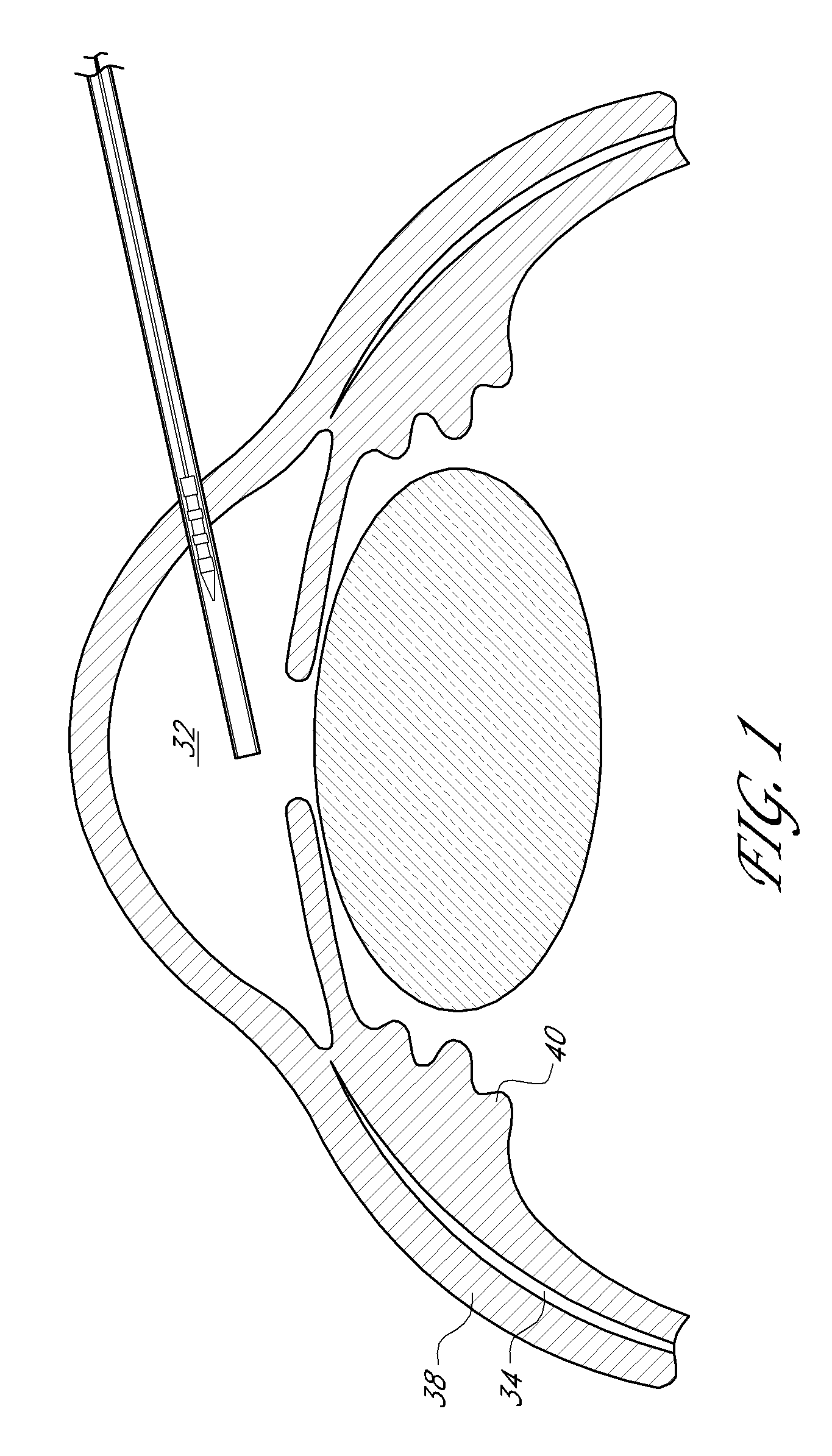
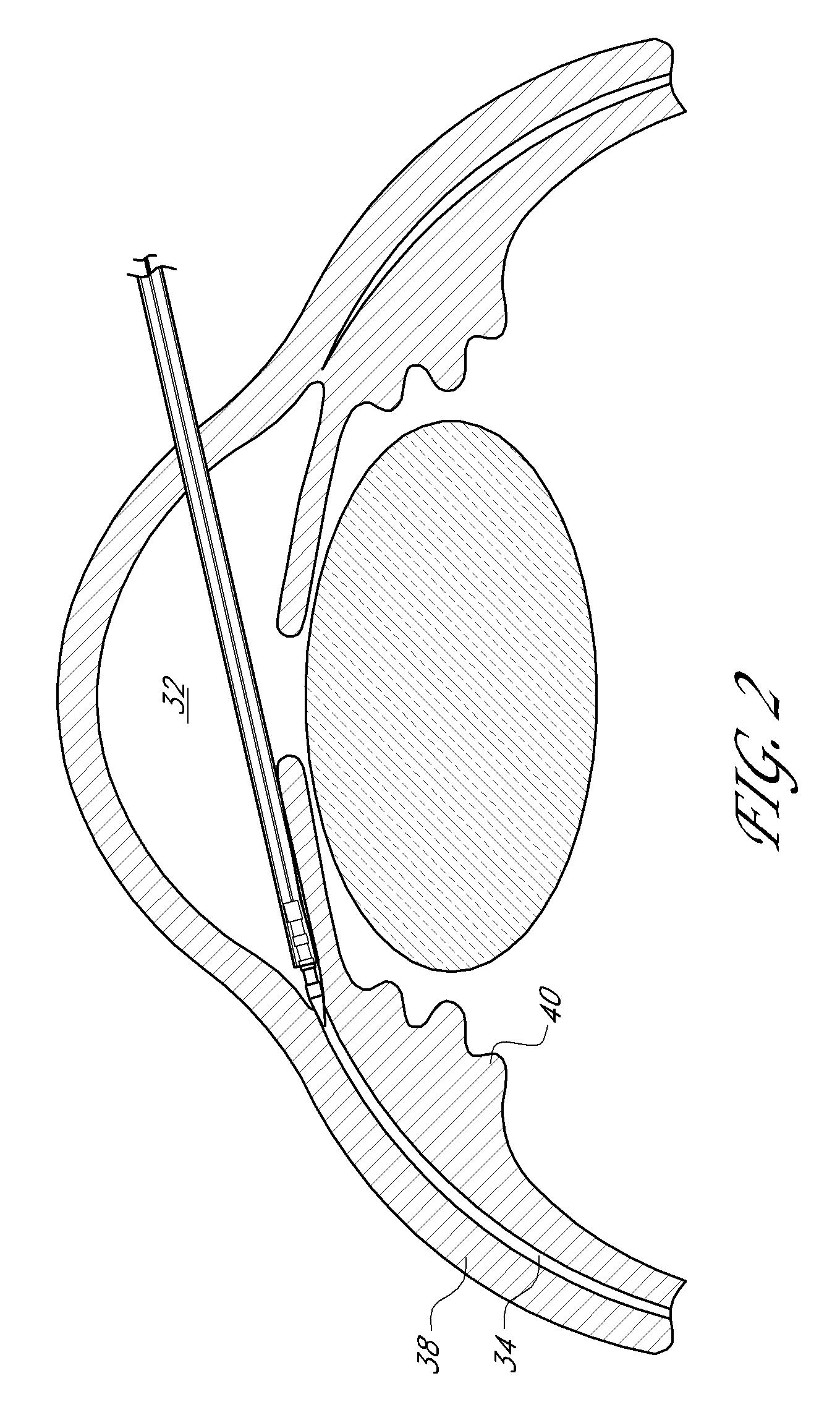
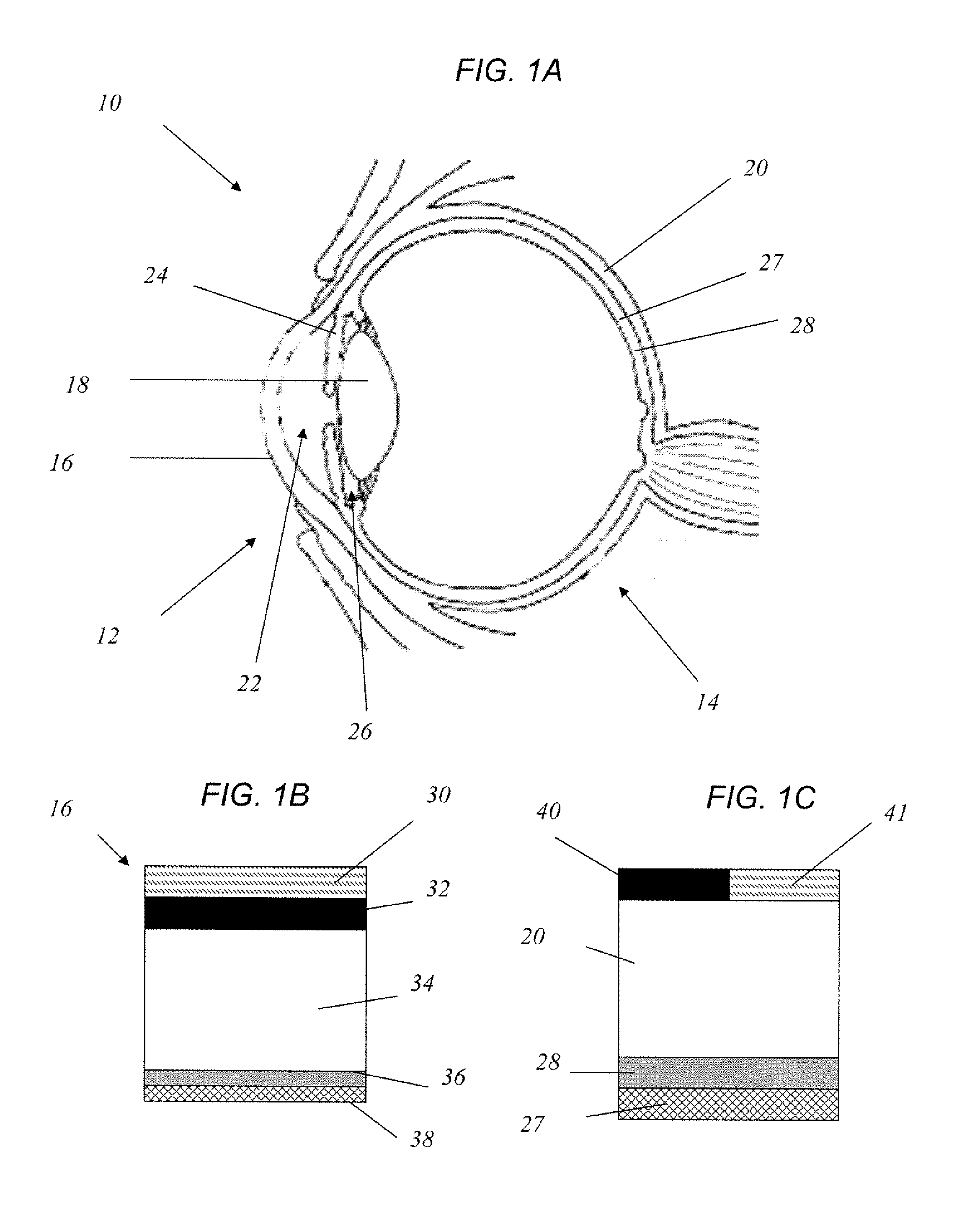
Method for drug delivery to ocular tissue using microneedle
Methods and devices are provided for administering a drug to a patient's eye. The methods include (a) inserting a hollow microneedle into the sclera or corneal stroma without penetrating across the sclera or corneal stroma; and (b) infusing a fluid drug formulation through the microneedle and into the sclera or cornea. It further may include partially retracting the microneedle before infusion to enhance delivery. Alternatively, the methods may include (a) inserting a solid microneedle into the sclera or corneal stroma without penetrating across the sclera or corneal stroma, wherein the solid microneedle comprises a first quantity of a drug formulation and inserting causes the solid microneedle to form a pocket in the sclera or corneal stroma; and (b) releasing the drug formulation into the pocket to form a drug depot, whereby a drug is released from the depot. The methods and devices may include an array of multiple microneedles.
Owner:GEORGIA TECH RES CORP +1
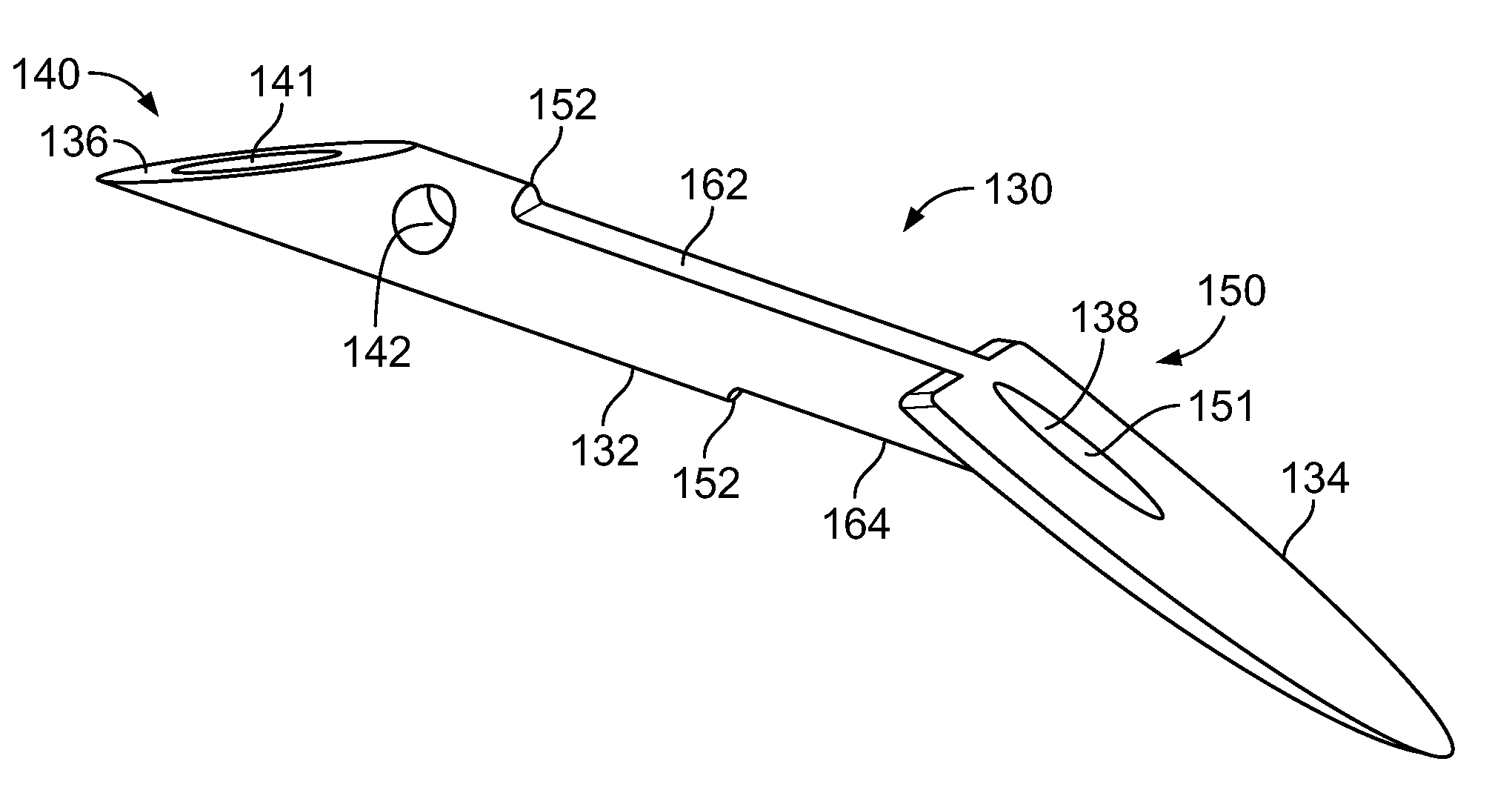
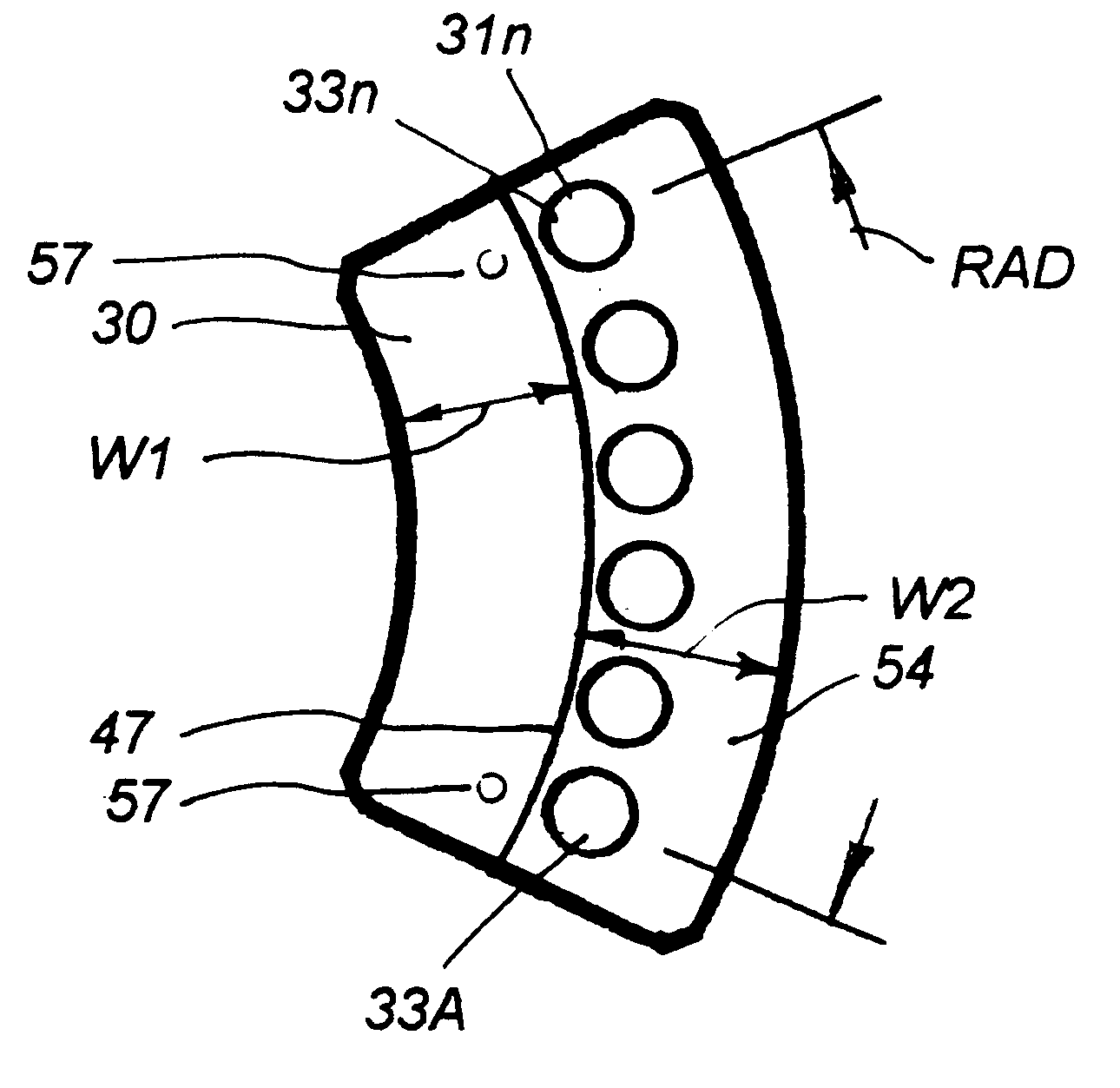
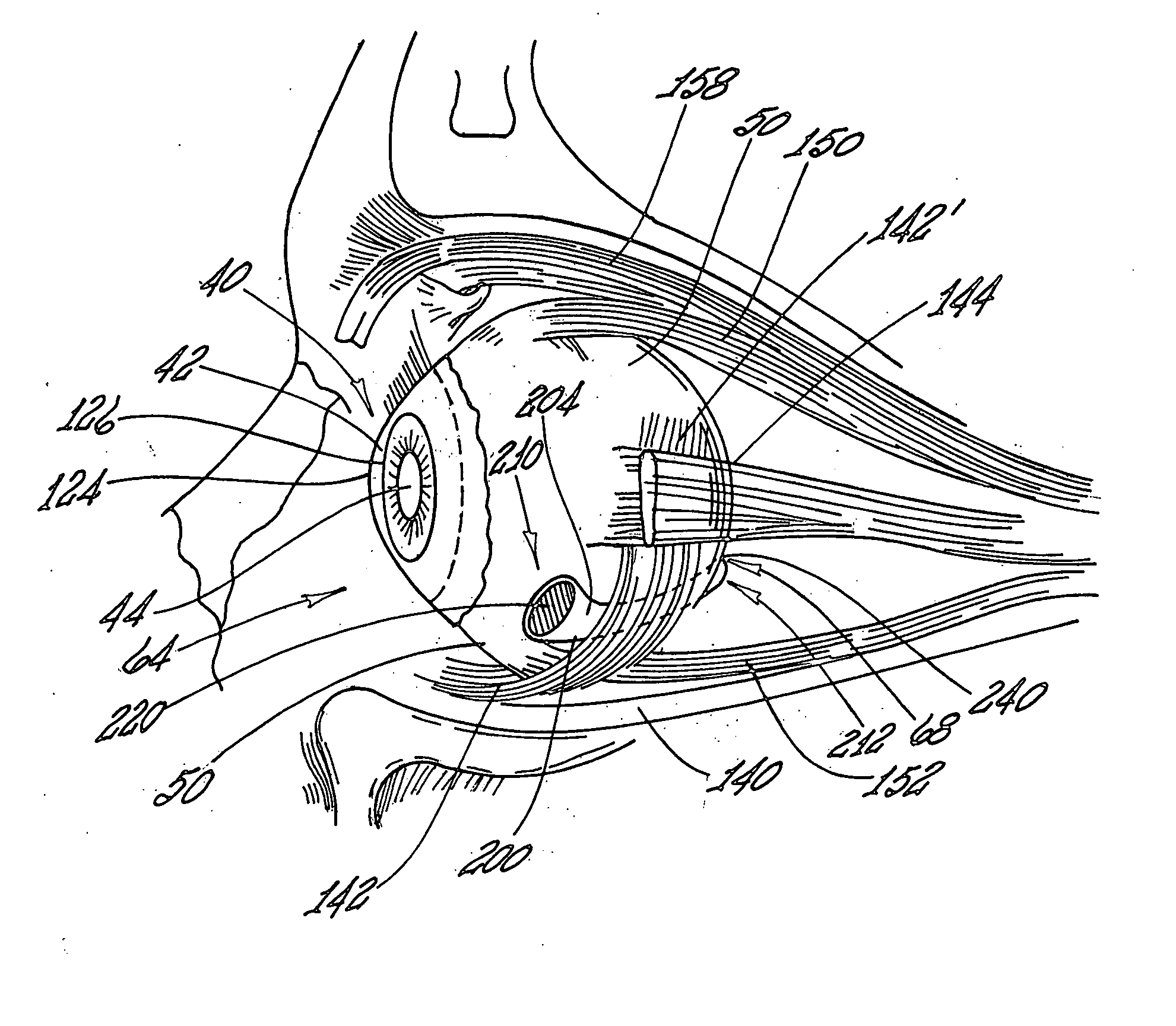
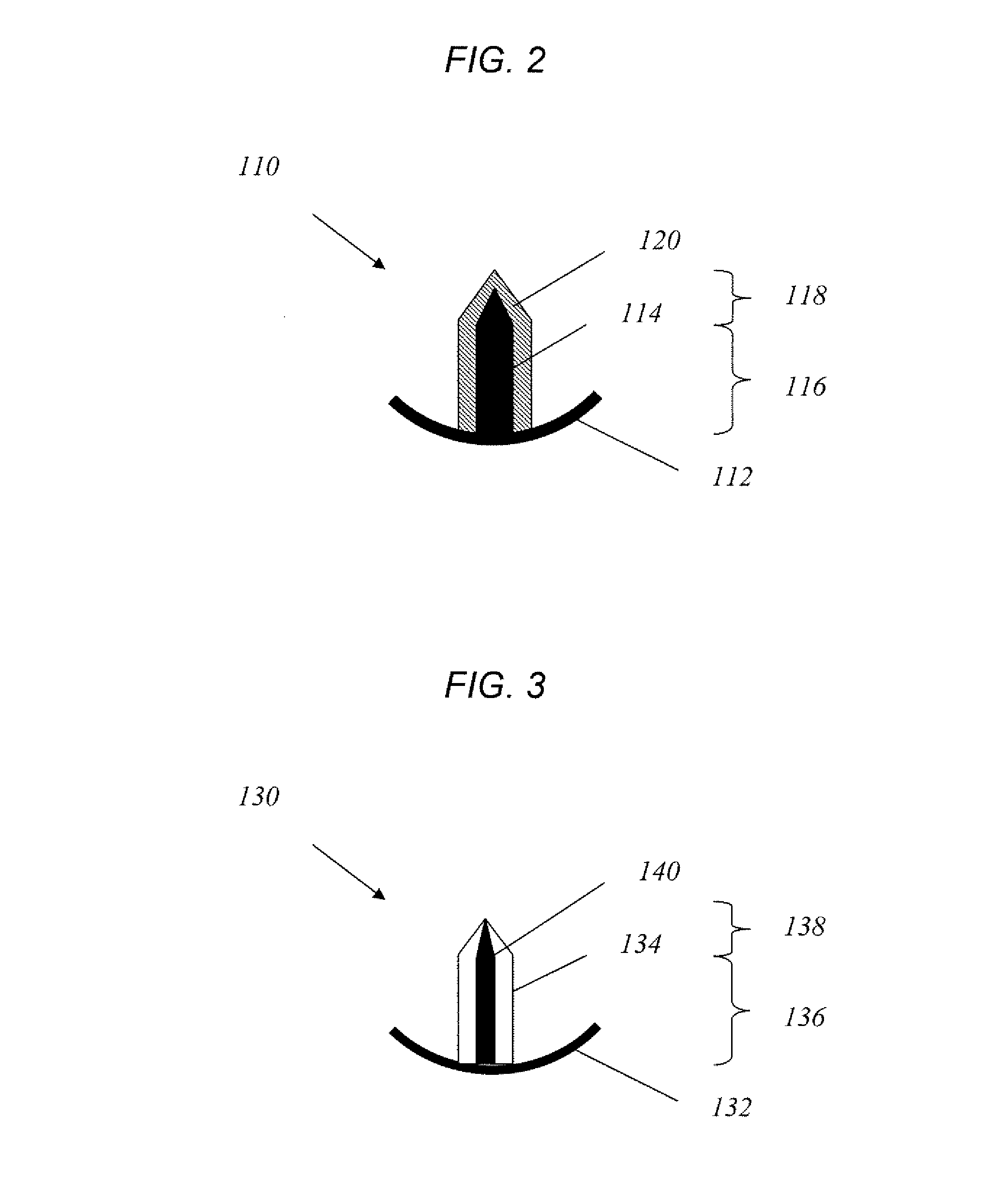
Scleral prosthesis for treatment of presbyopia and other eye disorders
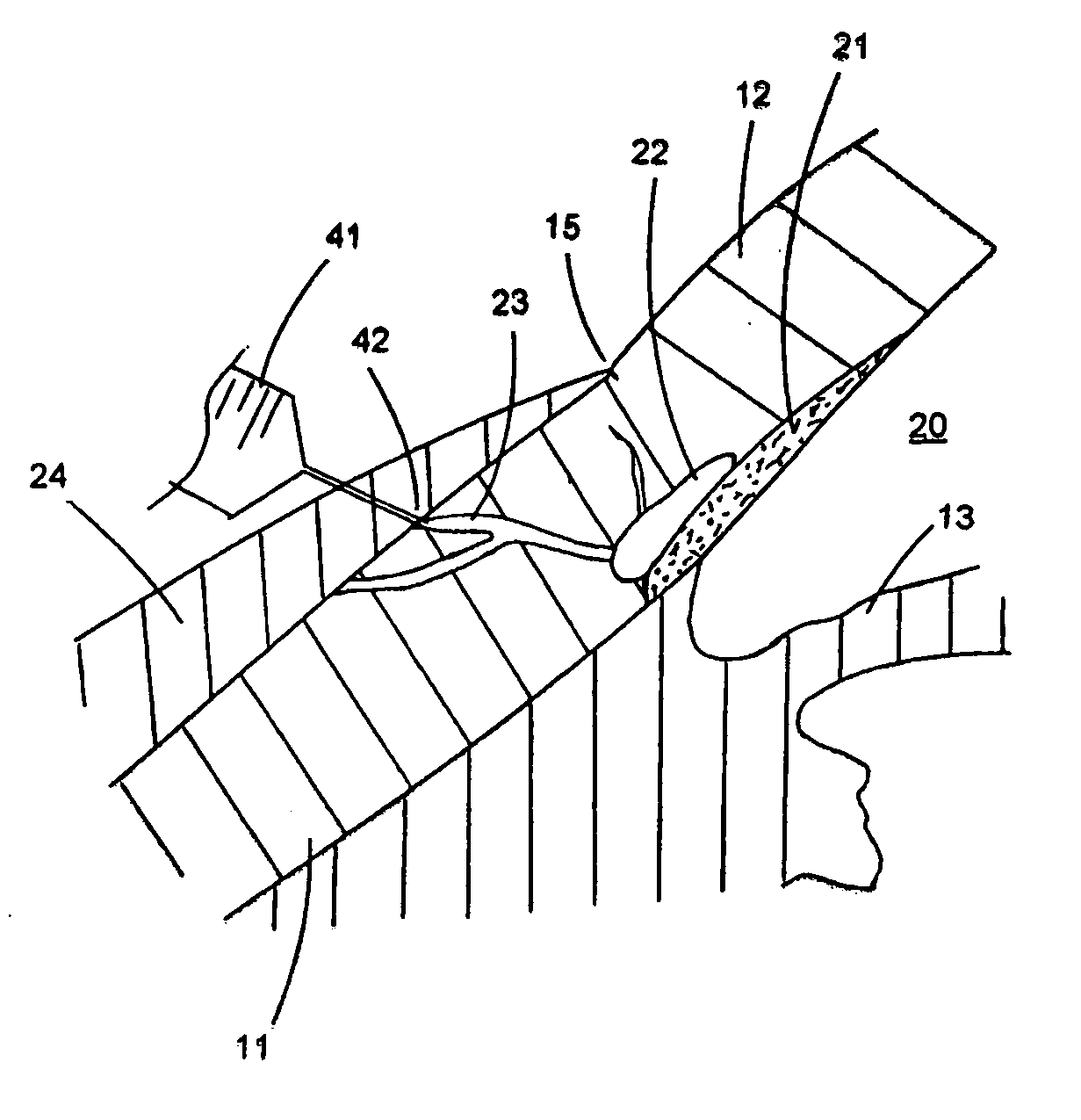
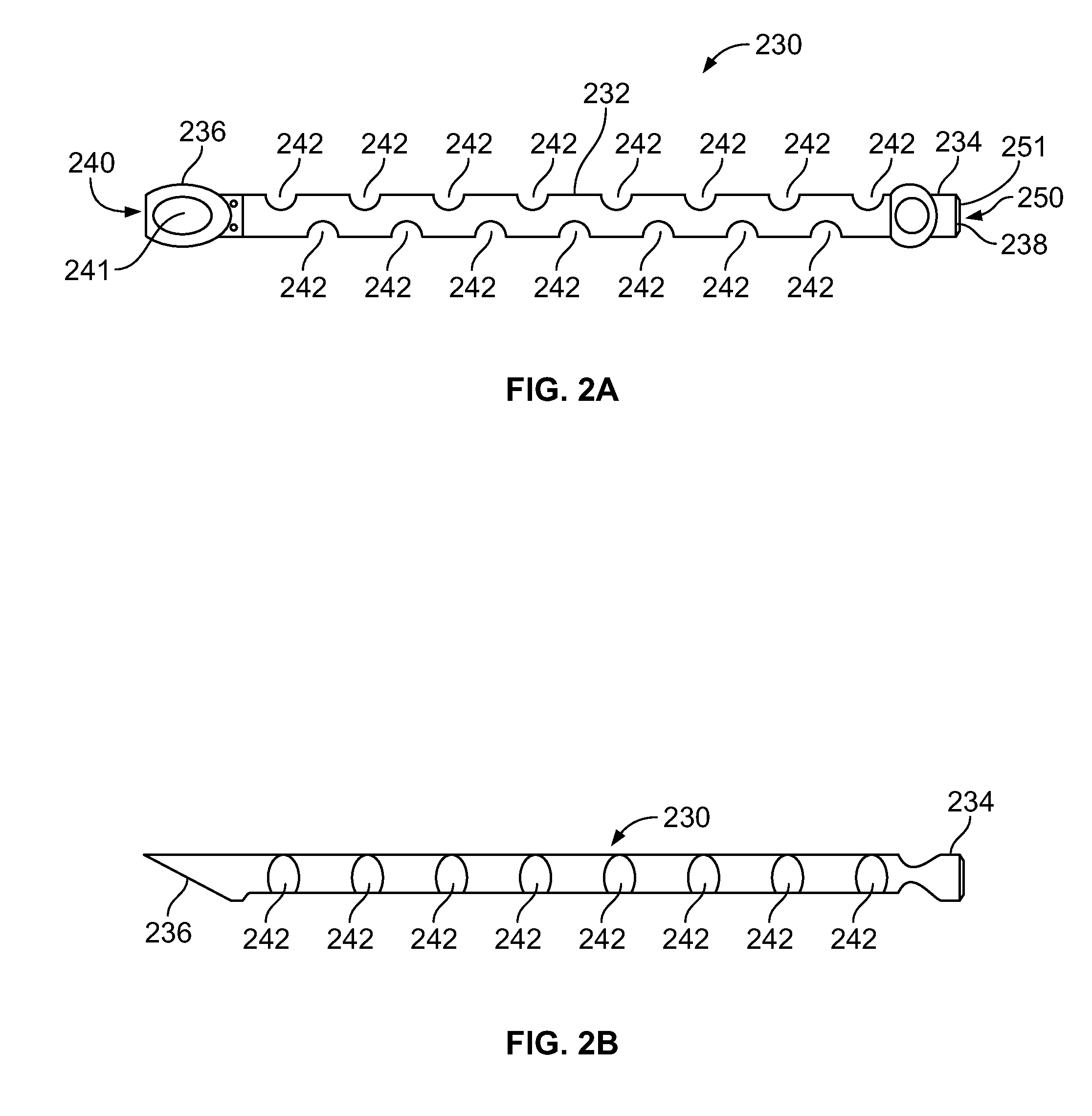
InactiveUS6280468B1Increase the effective working distanceIncrease the working distanceLaser surgeryEye implantsDiseaseOpen angle glaucoma
Presbyopia is treated by implanting within a plurality of elongated pockets formed in the tissue of the sclera of the eye transverse to a meridian of the eye, a prosthesis having an elongated body having a first surface and a second surface opposite the first surface to contact the base and flap of the scleral pocket. The first and second surfaces are spaced apart a distance so that the implanted prosthesis exerts an outward force on the flap of the scleral pocket which results in an outward traction on at least the anterior margin of the scleral pocket. The combined effect of the implanted prostheses is to exert a radially outward traction on the sclera in the region overlying the ciliary body which expands the sclera in the affected region together with the underlying ciliary body. The expansion of the ciliary body restores the effective working distance of the ciliary muscle in the presbyopic eye and thereby increases the amplitude of accommodation. Hyperopia, primary open angle glaucoma and / or ocular hypertension can be treated by increasing the effective working distance of the ciliary muscle according to the invention. A preferred embodiment of the scleral prosthesis has a major surface adapted to contact the base or flap of the pocket and an opposite surface or ridge spaced from the major surface.
Owner:REFOCUS GROUP
Fluid drainage device, delivery device, and associated methods of use and manufacture
The disclosure provides an intraocular implant for allowing fluid flow from the anterior chamber of an eye, the implant comprising a tube having an inlet end, an outlet end, and a tube passage, wherein the inlet end is adapted to extend into the anterior chamber of the eye, and wherein the outlet end is adapted to be implanted adjacent scleral tissue of the eye. The implant may be adapted to drain aqueous humor into a suprachoroidal space or a juxta-uveal space. The disclosure also provides associated delivery devices, methods of use, and methods of manufacture.
Owner:OPTONOL LTD
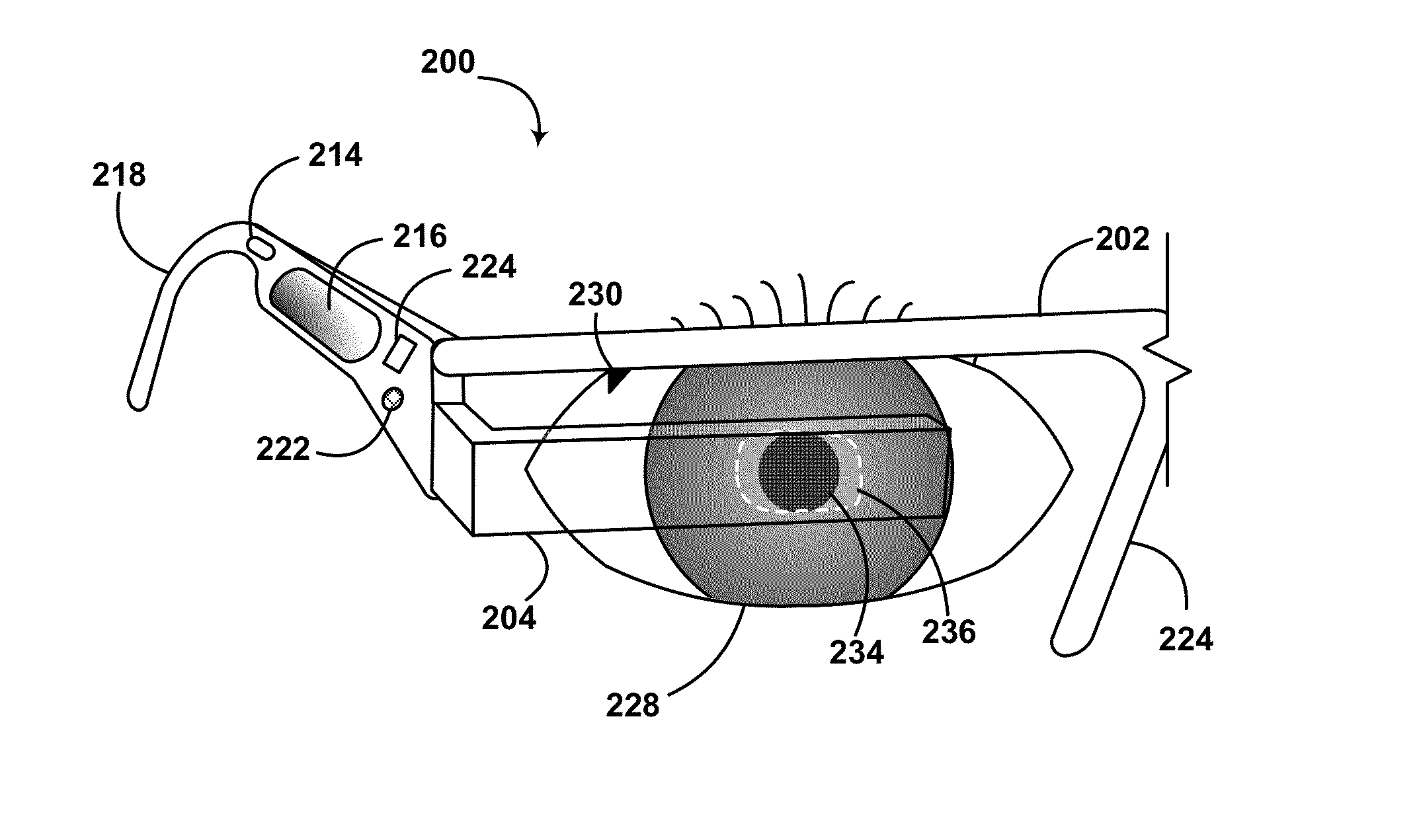
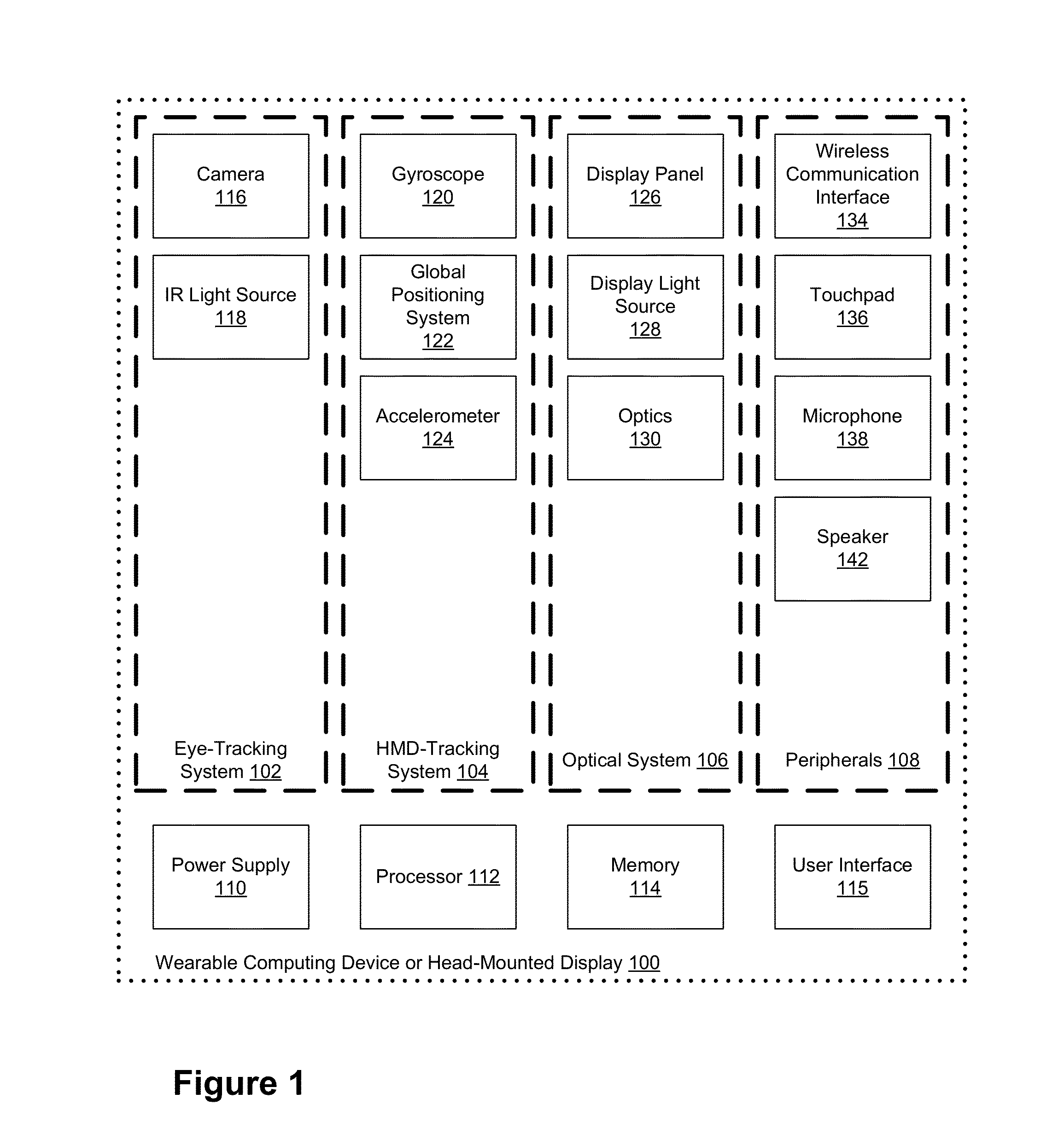
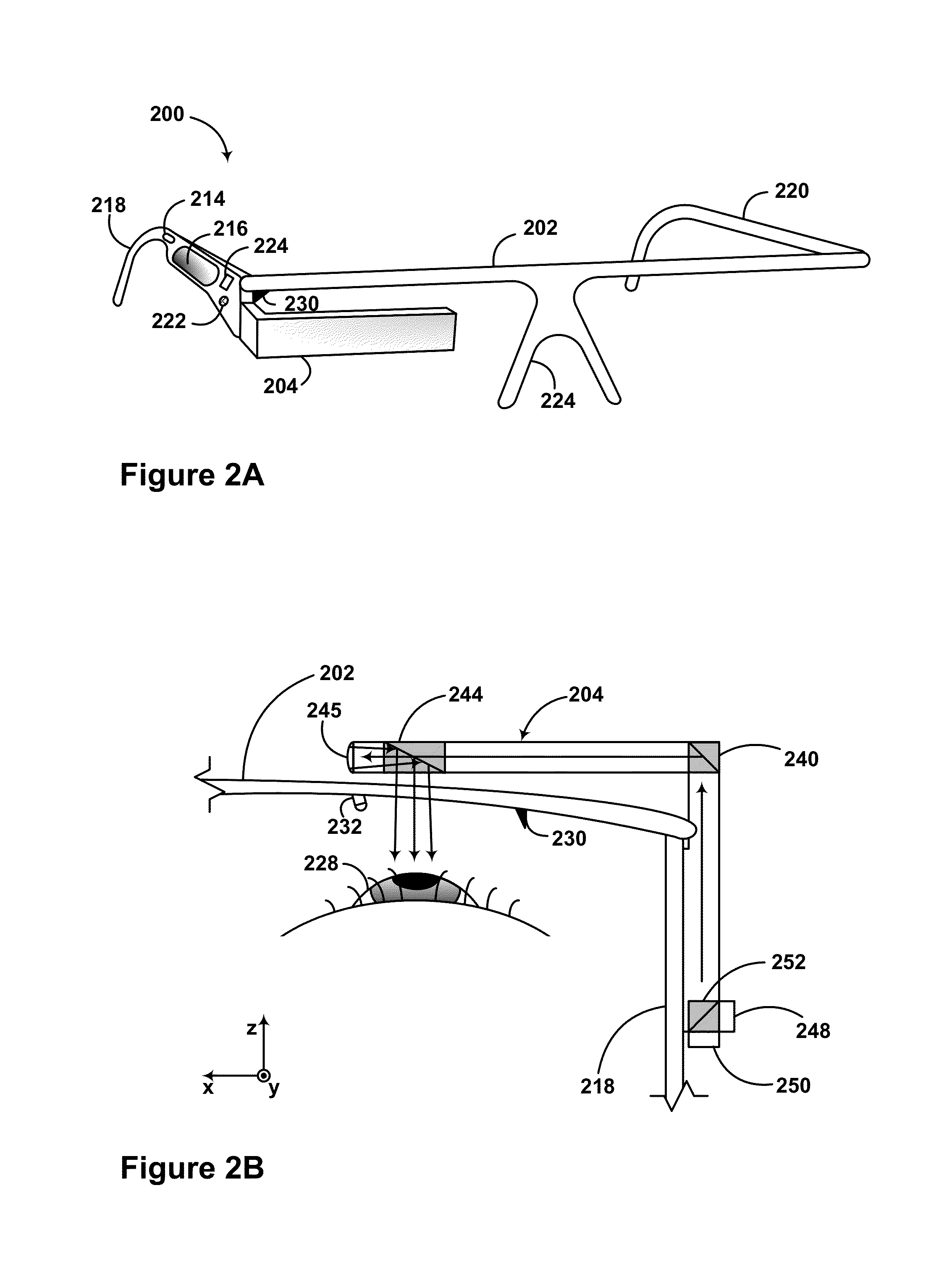
Method and system for input detection using structured light projection
Exemplary methods and systems help provide for tracking an eye. An exemplary method may involve: causing the projection of a pattern onto an eye, wherein the pattern comprises at least one line, and receiving data regarding deformation of the at least one line of the pattern. The method further includes correlating the data to iris, sclera, and pupil orientation to determine a position of the eye, and causing an item on a display to move in correlation with the eye position.
Owner:GOOGLE LLC
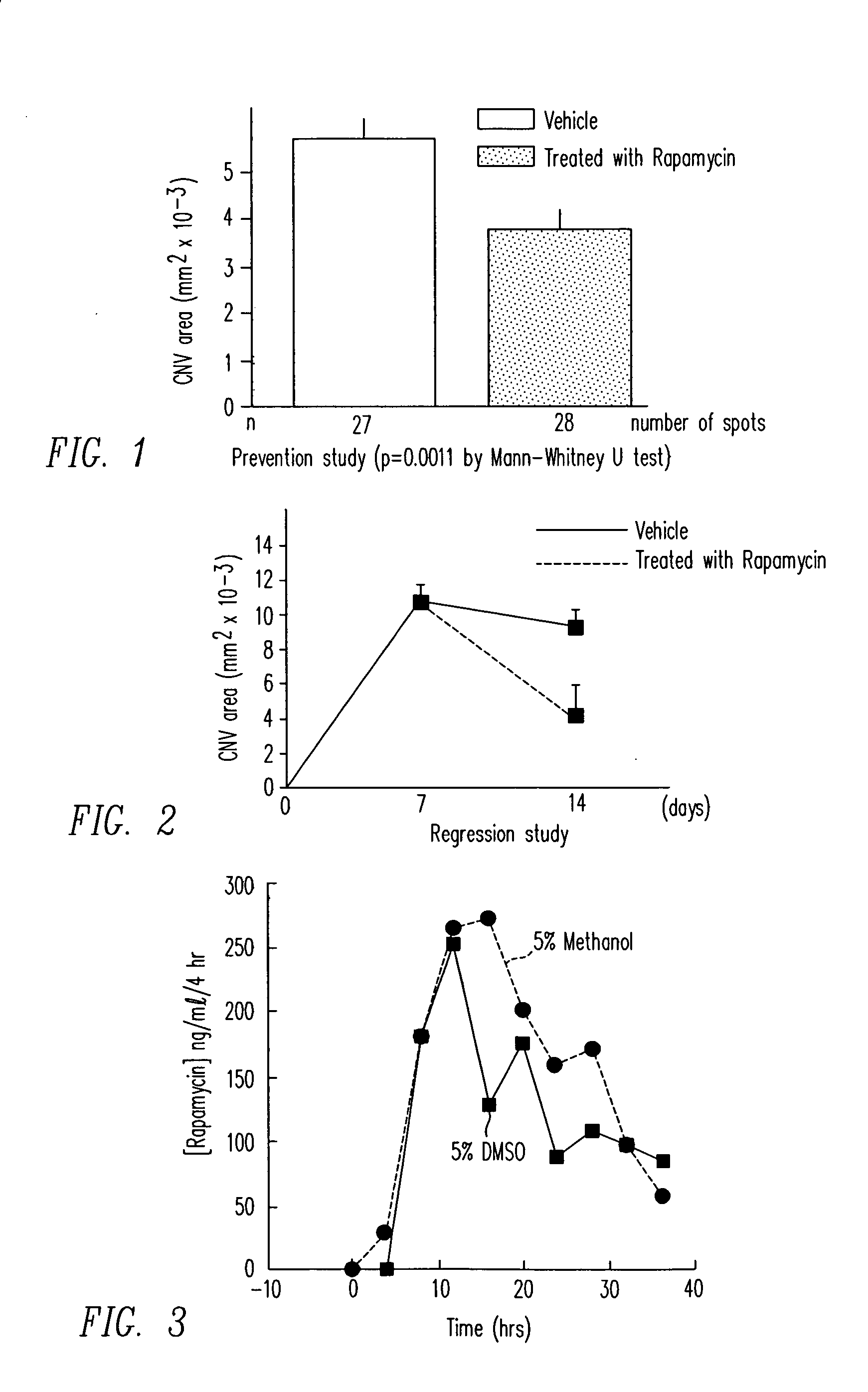
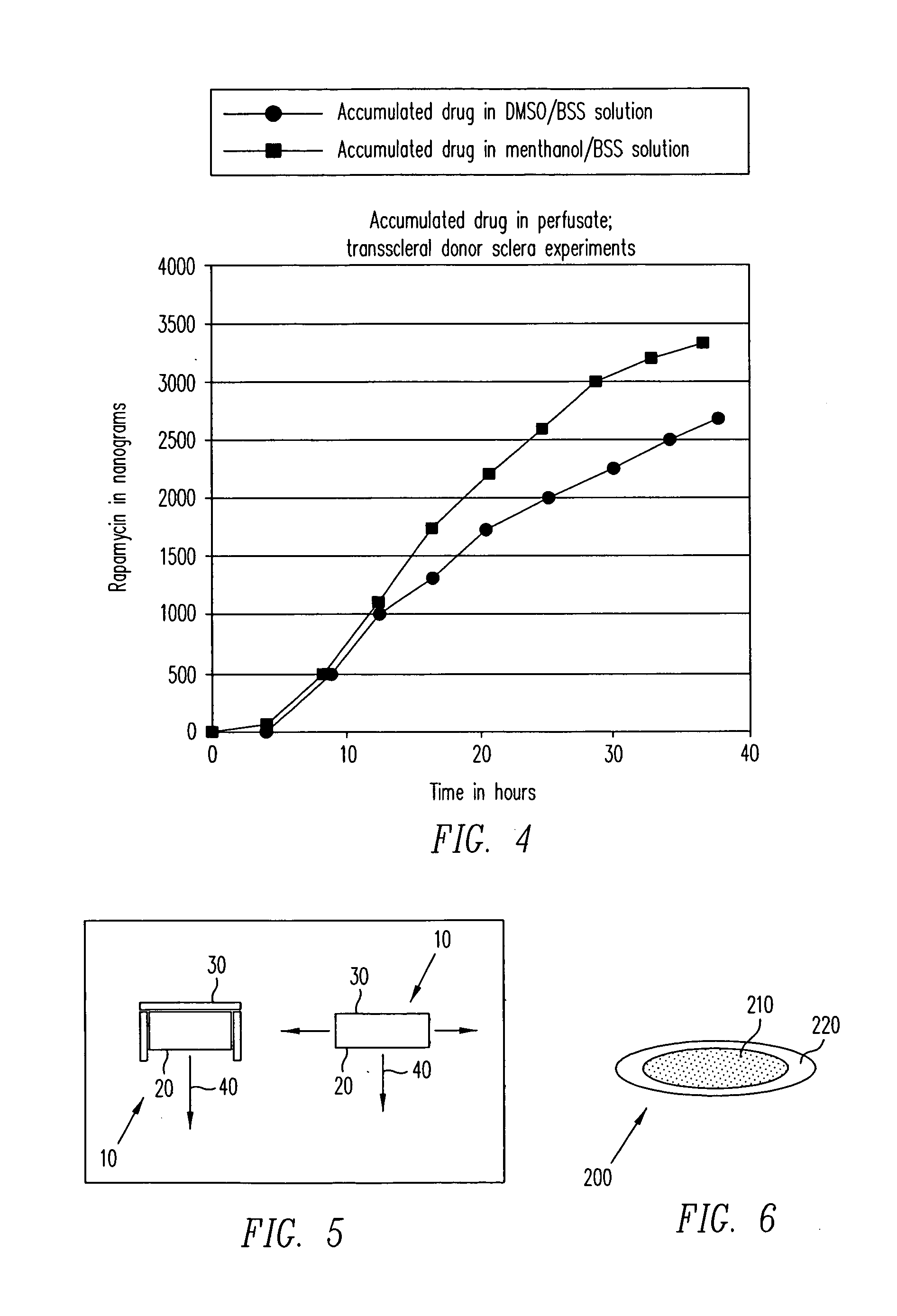
Transscleral delivery
Diseases associated with the tissues in the posterior segment of the eye can be effectively treated by administering therapeutic agents transsclerally to those tissues. Compositions, devices, and methods for delivering therapeutic agents so that they cross the sclera and reach these tissues include injecting solutions or suspensions adjacent to or within the sclera and implanting solid structures containing the therapeutic agent adjacent to or within the sclera. These methods may be used for administering rapamycin or related compounds to treat choroidal neovascularization associated with age-related macular degeneration.
Owner:SANTEN PHARMA CO LTD
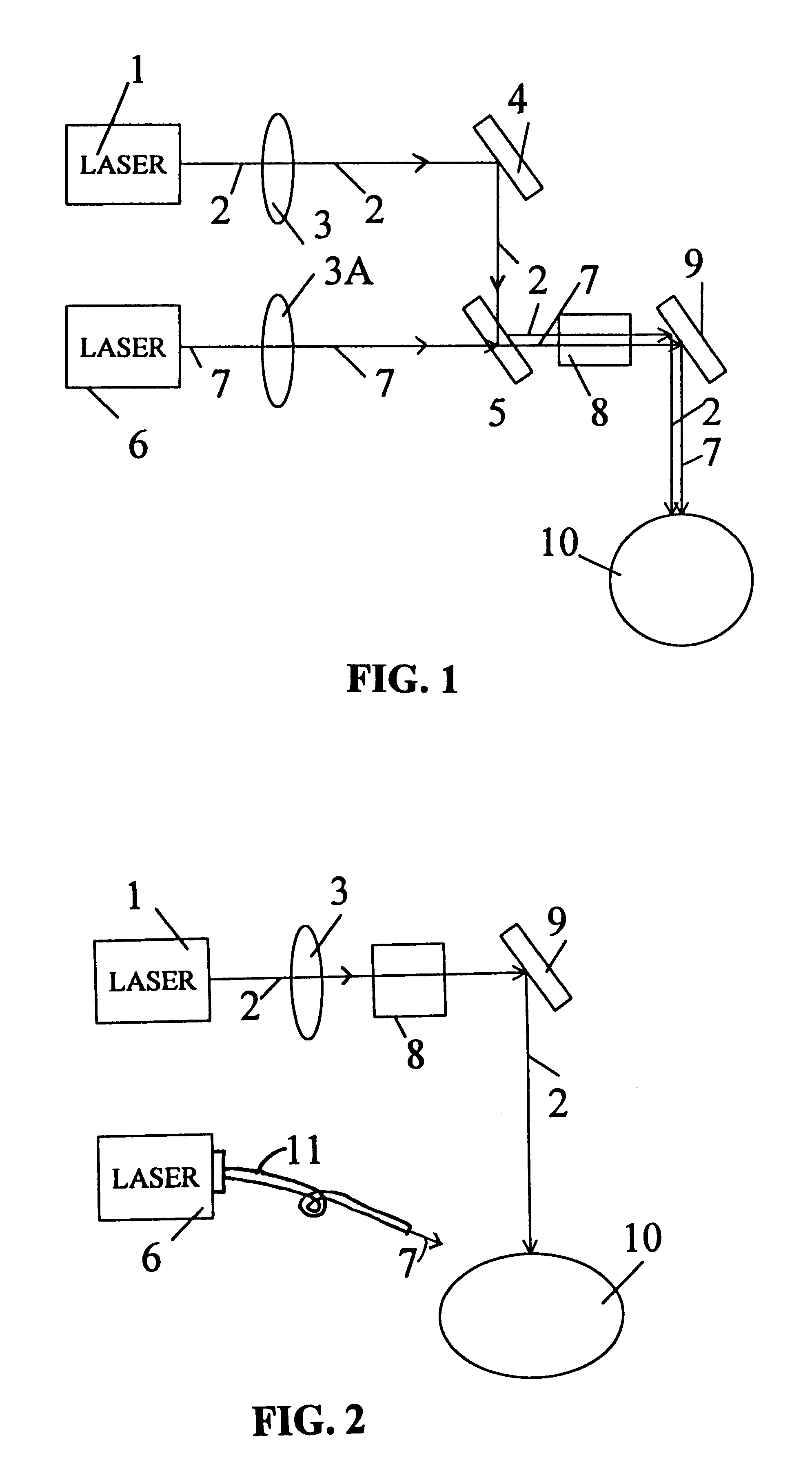
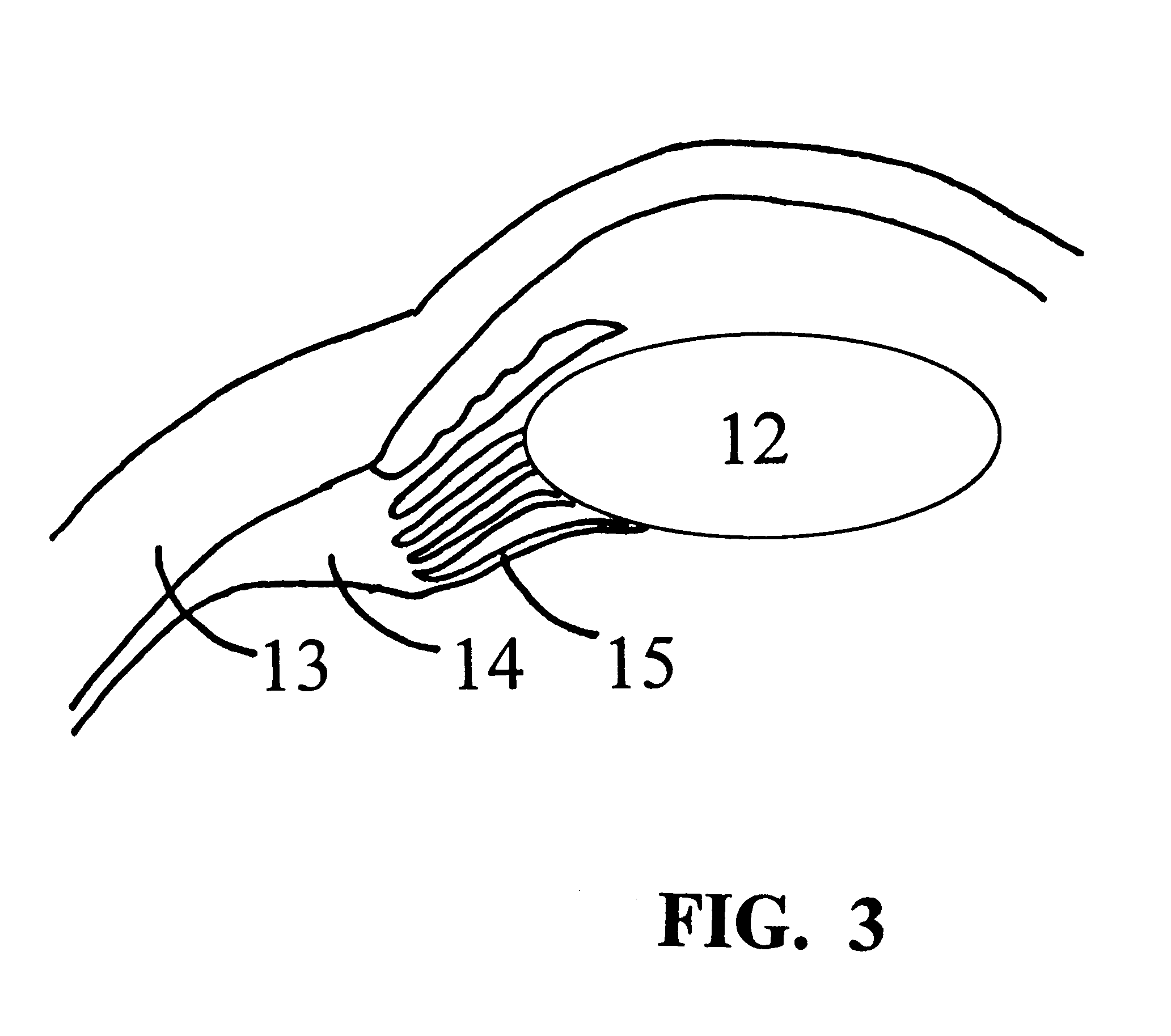
Treatment of presbyopia and other eye disorders using a scanning laser system
InactiveUS6263879B1Efficient and accurate expansionPreventing of open angle glaucomaLaser surgeryDiagnosticsDiseaseGlaucoma
Presbyopia is treated by a method which uses ablative lasers to ablate the sclera tissue and increase the accommodation of the ciliary body. Tissue bleeding is prevented by an ablative laser having a wavelength of between 0.15 and 3.2 micron. A scanning system is proposed to perform various patterns on the sclera area of the cornea to treat presbyopia and to prevent other eye disorder such as glaucoma. Laser parameters are determined for accurate sclera expansion.
Owner:NEOS OCULAR
Devices and techniques for light-mediated stimulation of trabecular meshwork in glaucoma therapy
An apparatus and technique for transscleral light-mediated biostimulation of the trabecular plates of a patient's eye in a treatment for glaucoma or ocular hypertension. The apparatus includes; (i) a working end geometry for contacting the anterior surface of the sclera and cornea to insure that a laser emission reaches the trabecular meshwork from a particular location on the anterior surface of the sclera, (ii) a laser energy source providing a wavelength appropriate for absorption beneath the anterior scleral surface to the depth of the trabecular plates, and (iii) a dosimetry control system for controlling the exposure of the laser emission at the particular spatial locations. The device uses a light energy source that emits wavelengths in the near-infrared portion of the spectrum, preferably in the range of about 1.30 mum to 1.40 mum or from about 1.55 mum to 1.85 mum. The depth of absorption of such wavelength ranges will extend through most, if not all, of the thickness of the sclera (750 mum to 950 mum). In accordance with a proposed method of trabecular biostimulation, the targeted region is elevated in temperature to a range between about 40° C. to 55° C. for a period of time ranging from about 1 second to 120 seconds or more.
Owner:SOLX
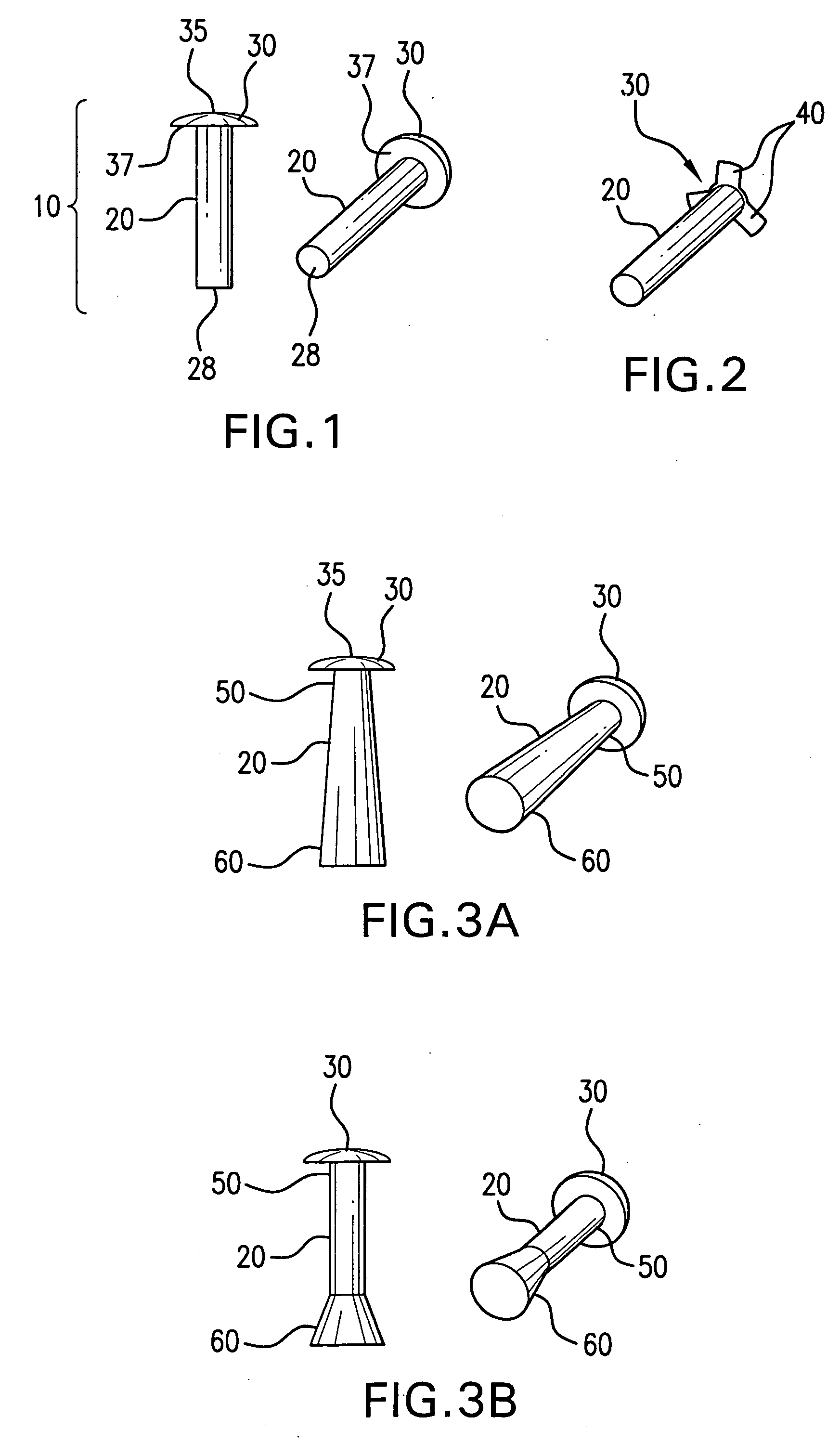
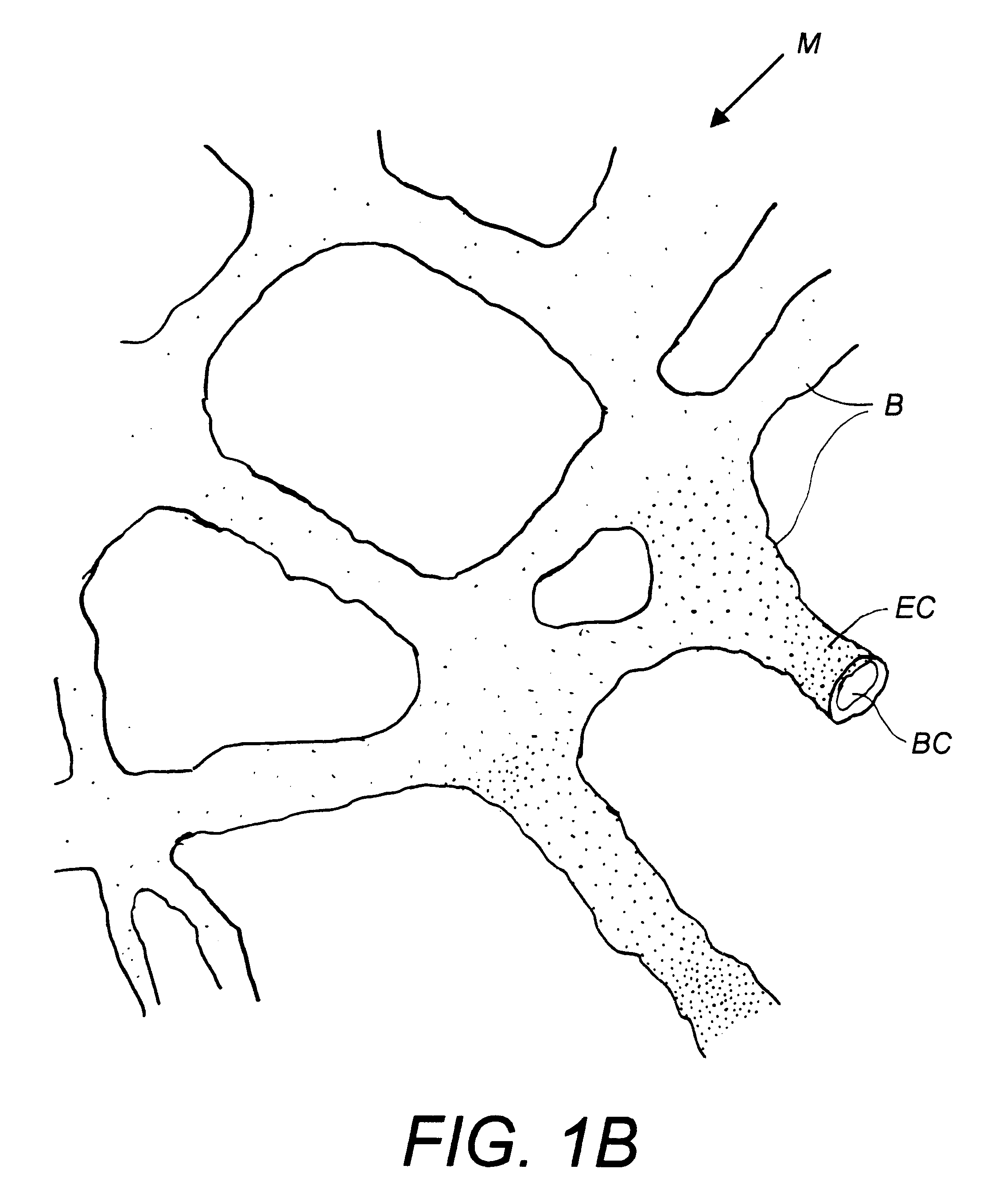
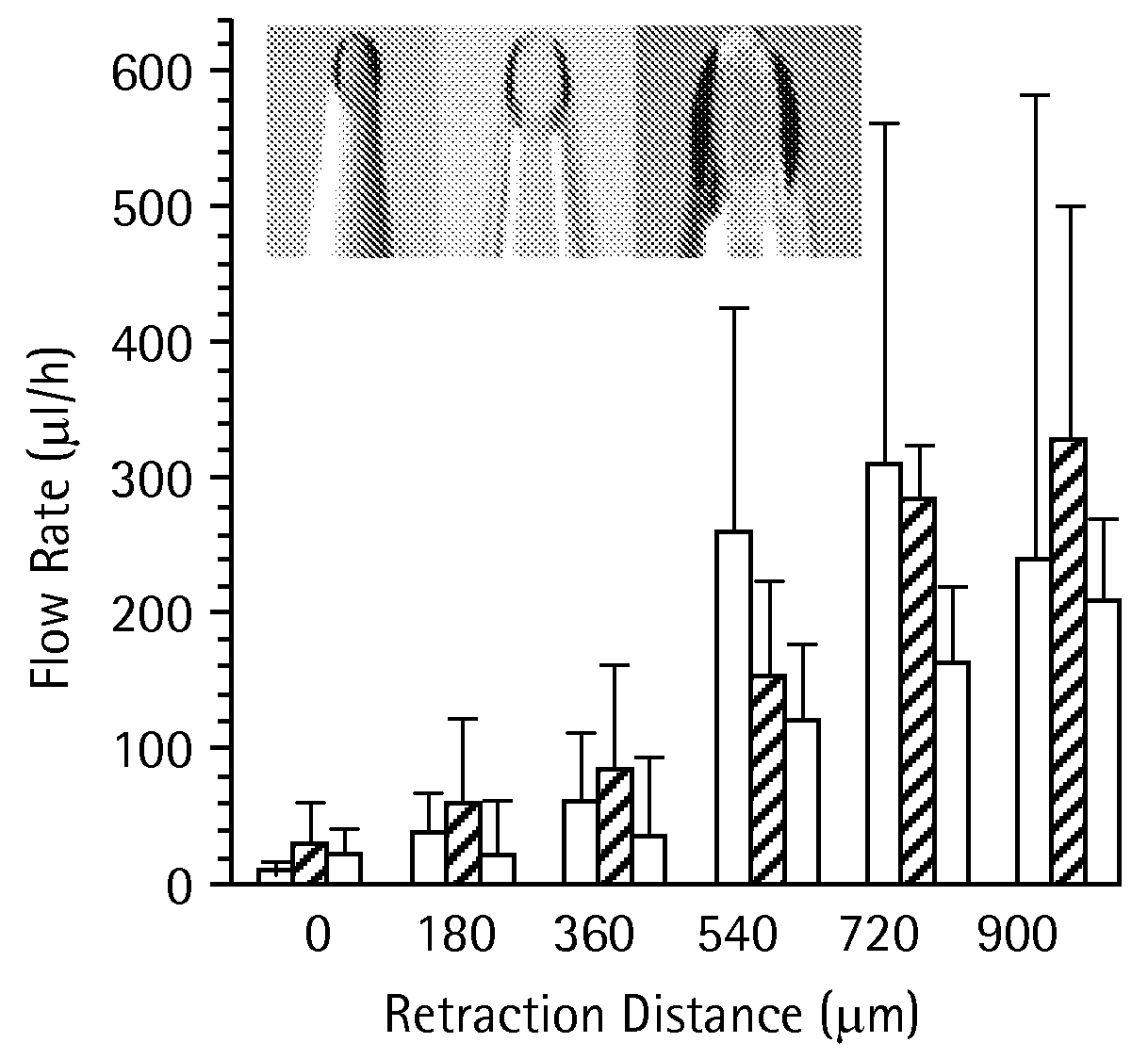
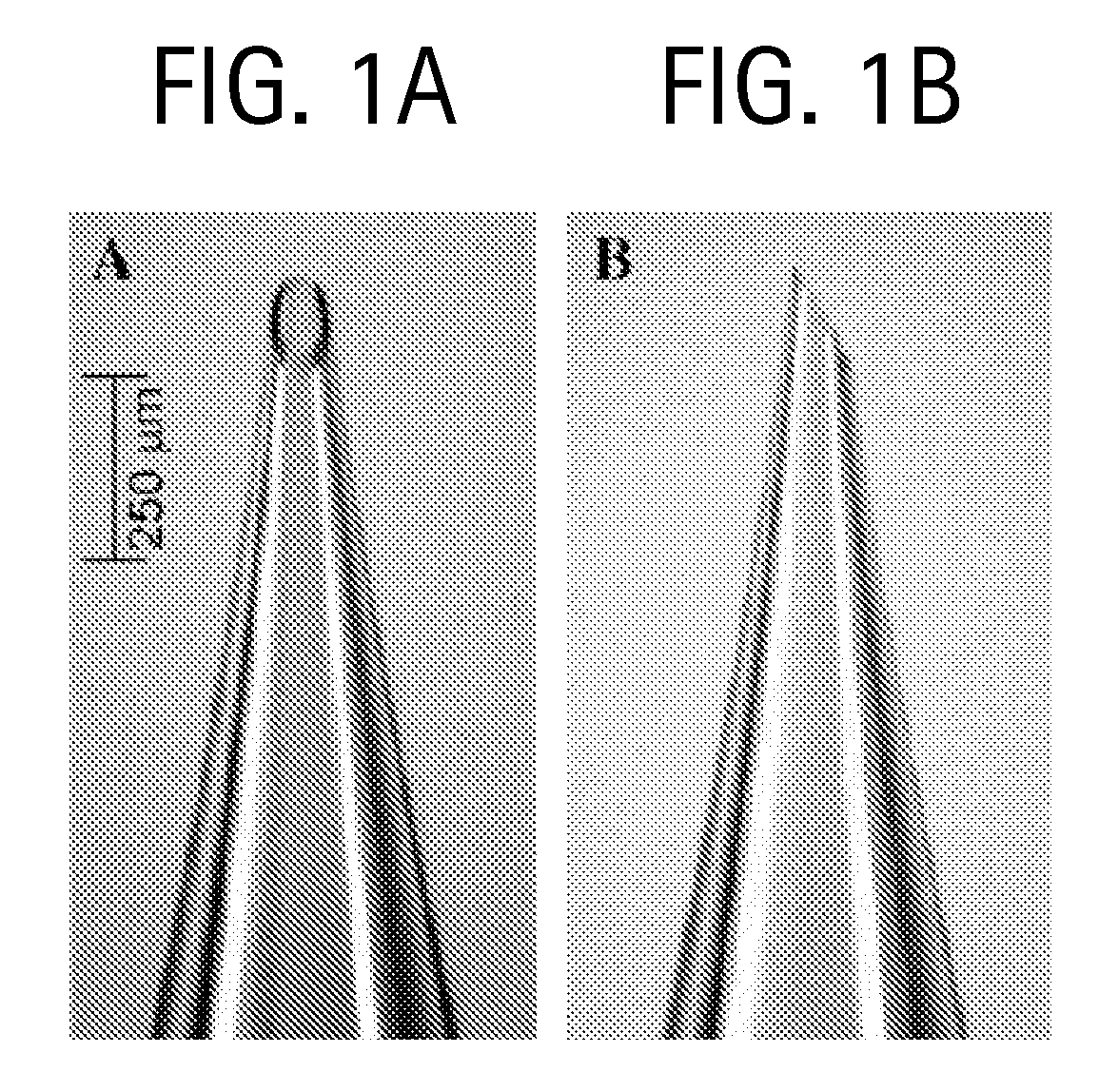
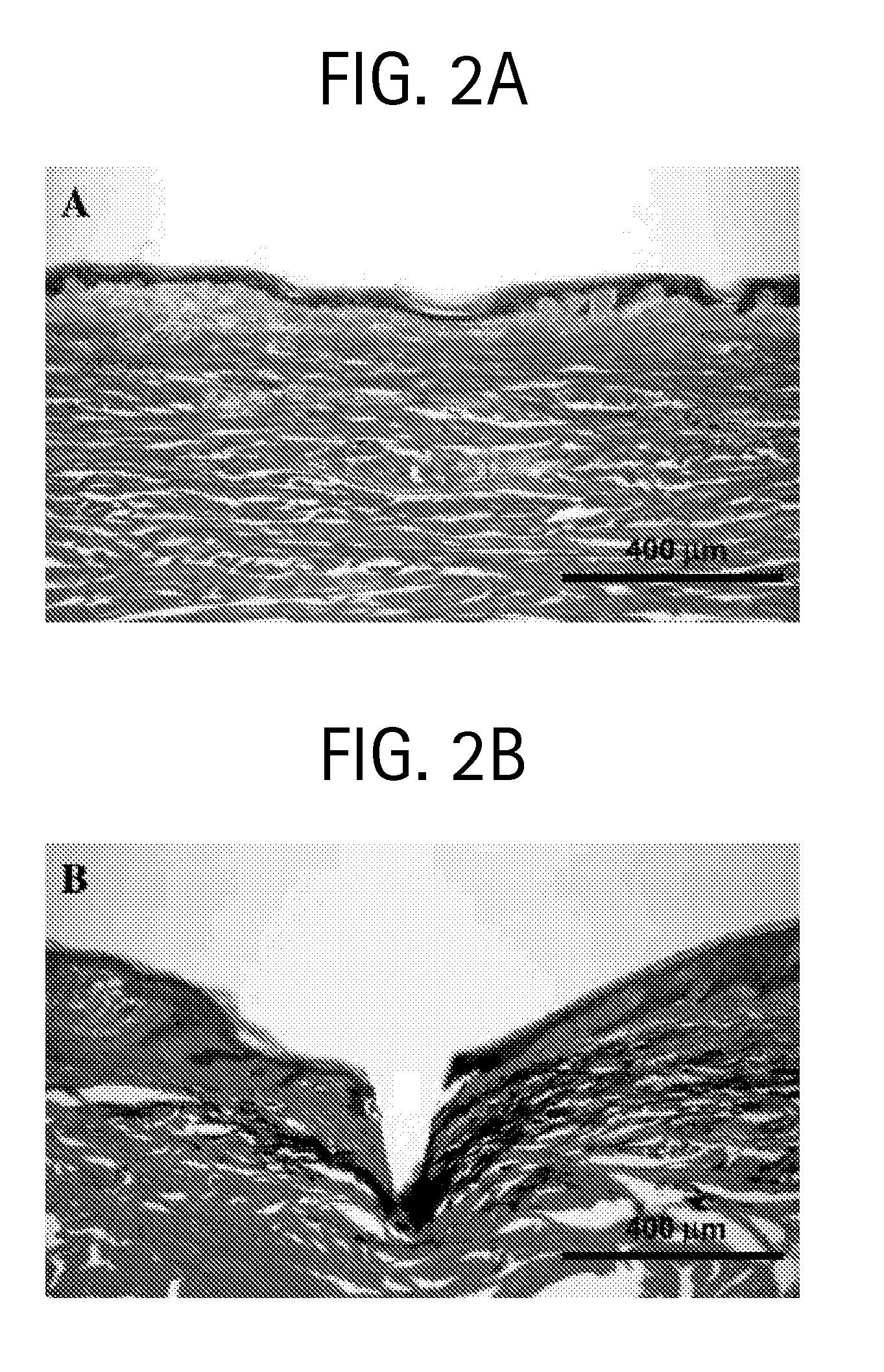
Microneedles and Methods for Microinfusion
Methods and devices are provided for delivering a drug to or withdrawing a fluid from a biological tissue, such the skin, sclera, cornea, and conjunctiva. One method includes the steps of inserting at least one microneedle into the biological tissue; partially retracting the at least one microneedle from the tissue; and then delivering at least one drug formulation into the biological tissue via the partially retracted at least one microneedle. The microneedle deforms and penetrates the biological tissue during the insertion step, and the retraction step at least partially relaxes the tissue deformation while maintaining at least part of the tissue penetration, facilitating drug delivery or fluid withdrawal.
Owner:GEORGIA TECH RES CORP
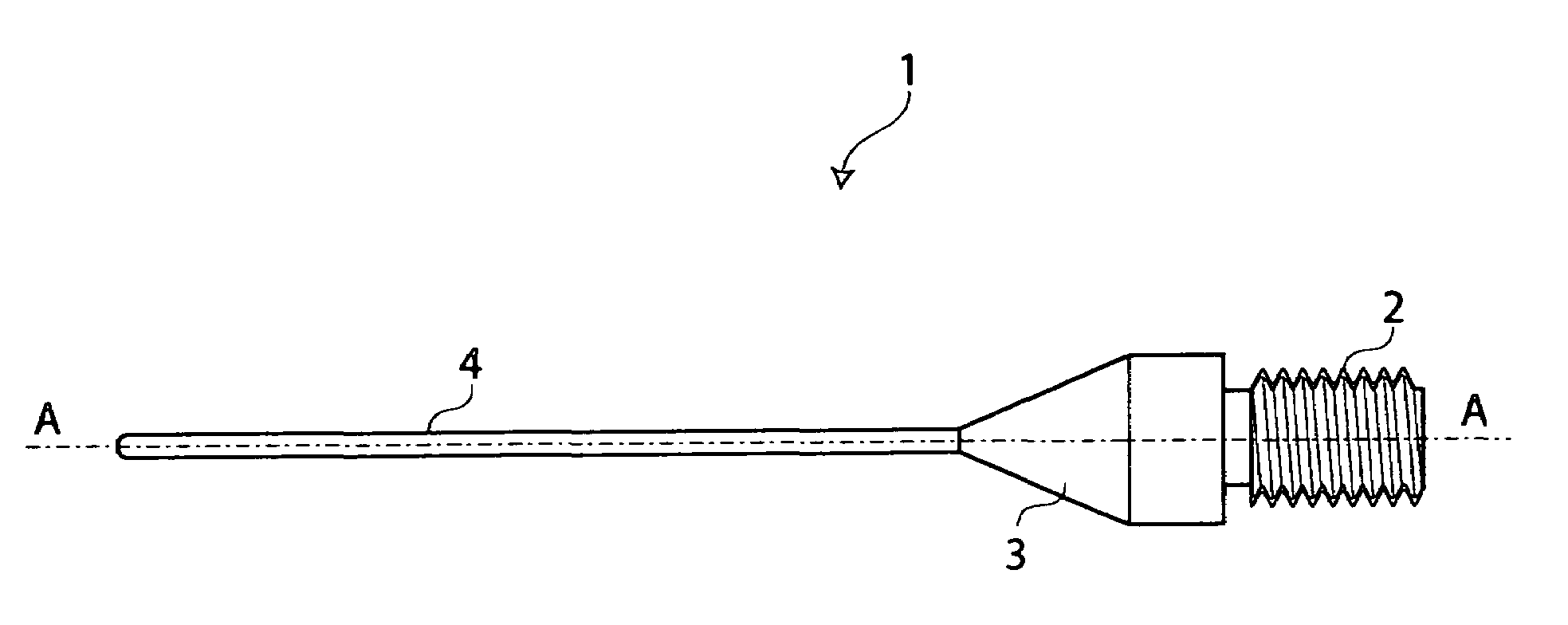
Emulsificated tip for oculistic surgery, particularly for phacoemulsification of cataract
InactiveUS7018389B2Improve adhesionEye surgerySurgical instrument detailsPhacoemulsificationSurgical department
The invention concerns an improved tip (1) for oculistic surgery, particularly for the removal of cataract, having a proximal joint end (2) and a distal end (4), contacting the crystalline during the surgical intervention, wherein the distal end (4) contacting a corneal or sclera tissue is coated with an anti-friction treatment, based on carbon and tungsten carbide.
Owner:OPTIKON 2000
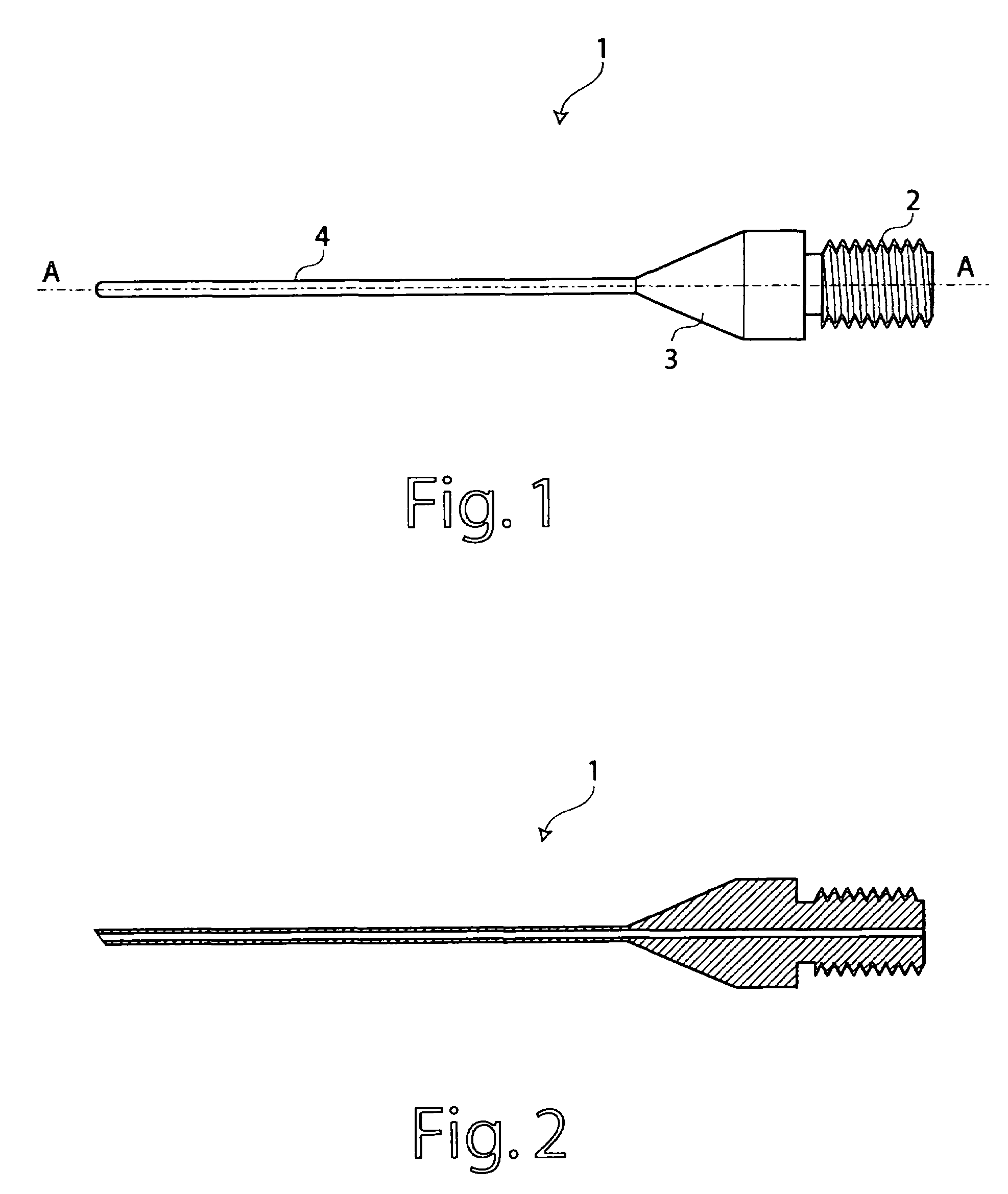
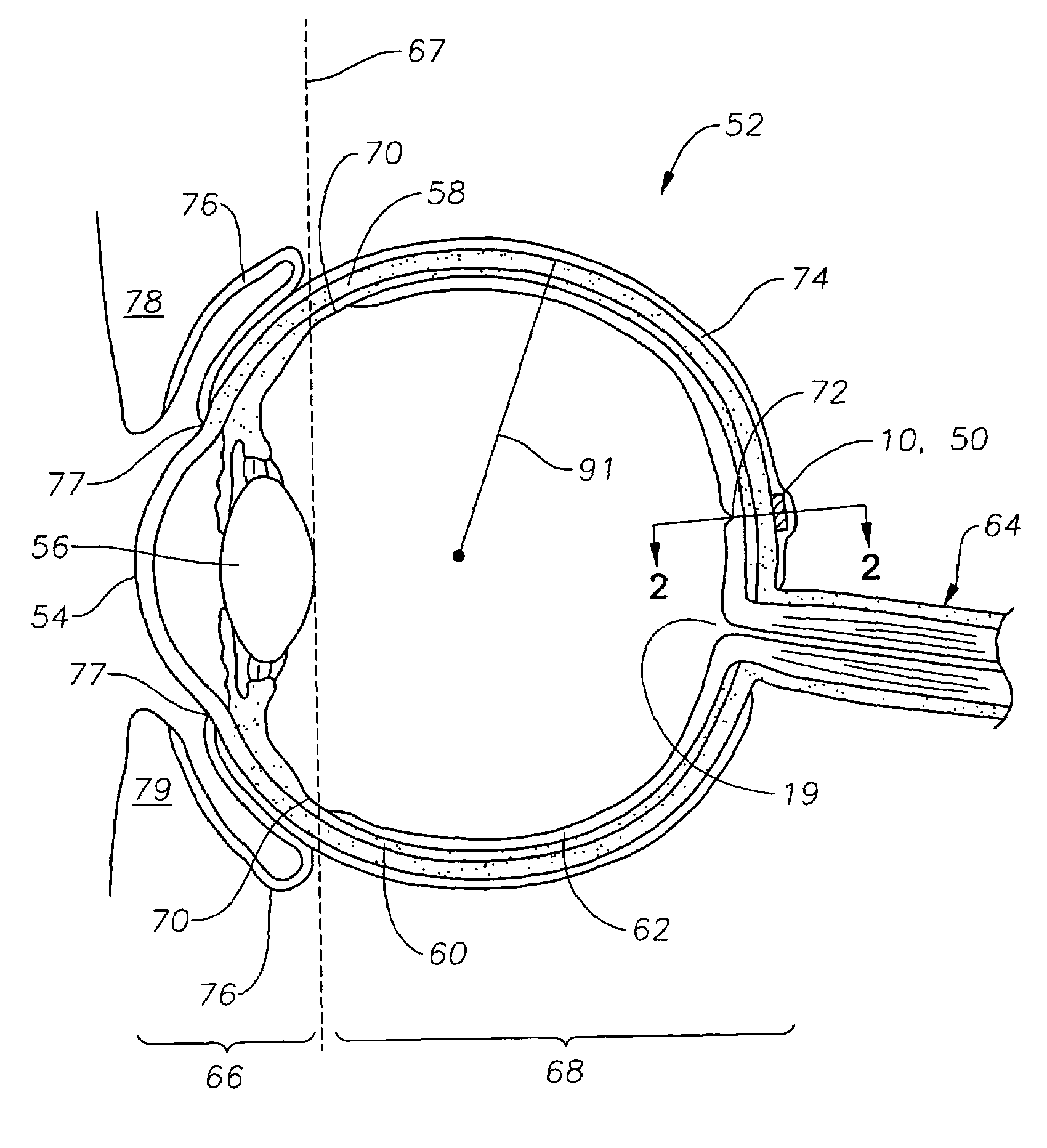
Glaucoma shunts with flow management and improved surgical performance
ActiveUS20100249691A1Improving glaucoma shuntReduce postoperative complicationsEye surgeryIntravenous devicesGlaucoma tube shuntGlaucoma
A method of treating glaucoma in an eye by managing fluid flow past an implanted shunt having an elastomeric plate and a non-valved elastomeric drainage tube. The plate is positioned over a sclera of the eye with an outflow end of the elastomeric drainage tube open to an outer face of the plate. An inflow end of the drainage tube tunnels through the sclera to the anterior chamber of the eye. The plate may have regions of greater propensity for cell adhesion alternating with regions of lesser cell adhesion. For example, regions of texturing around the plate or drainage tube may be provided to control the size of a bleb that forms over the implant. The effective surface area of the plate may be balanced against a number of fenestrations. The drainage tube has a reduced profile and may be shaped with a non-circular external cross-section to reduce its height. A scleral groove may be used to further reduce the height of the drainage tube on the sclera. A flow restrictor for the early post operative period will immediately lower the intraocular pressure (IOP) and simultanously prevent hypotony.
Owner:JOHNSON & JOHNSON SURGICAL VISION INC
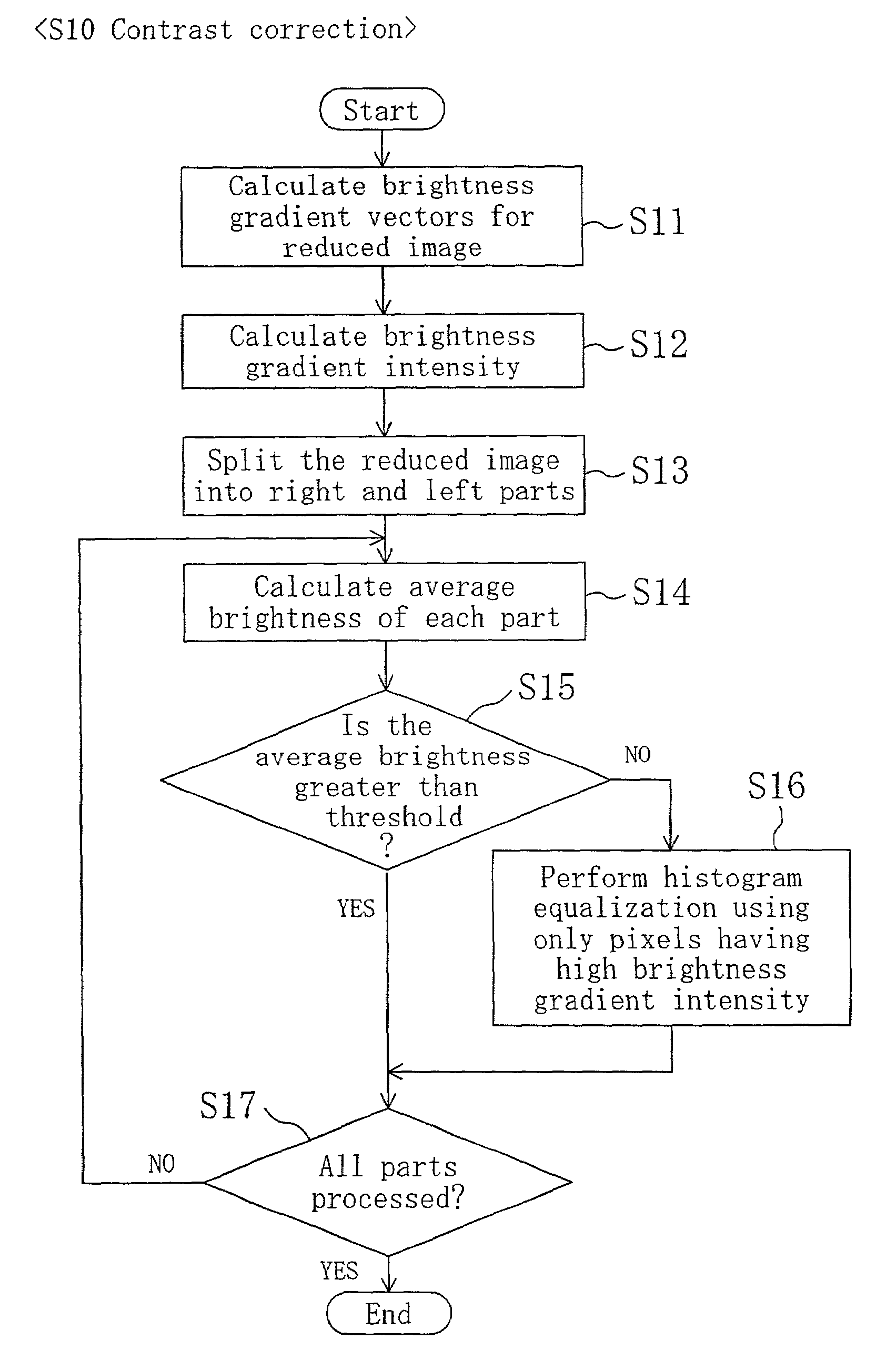
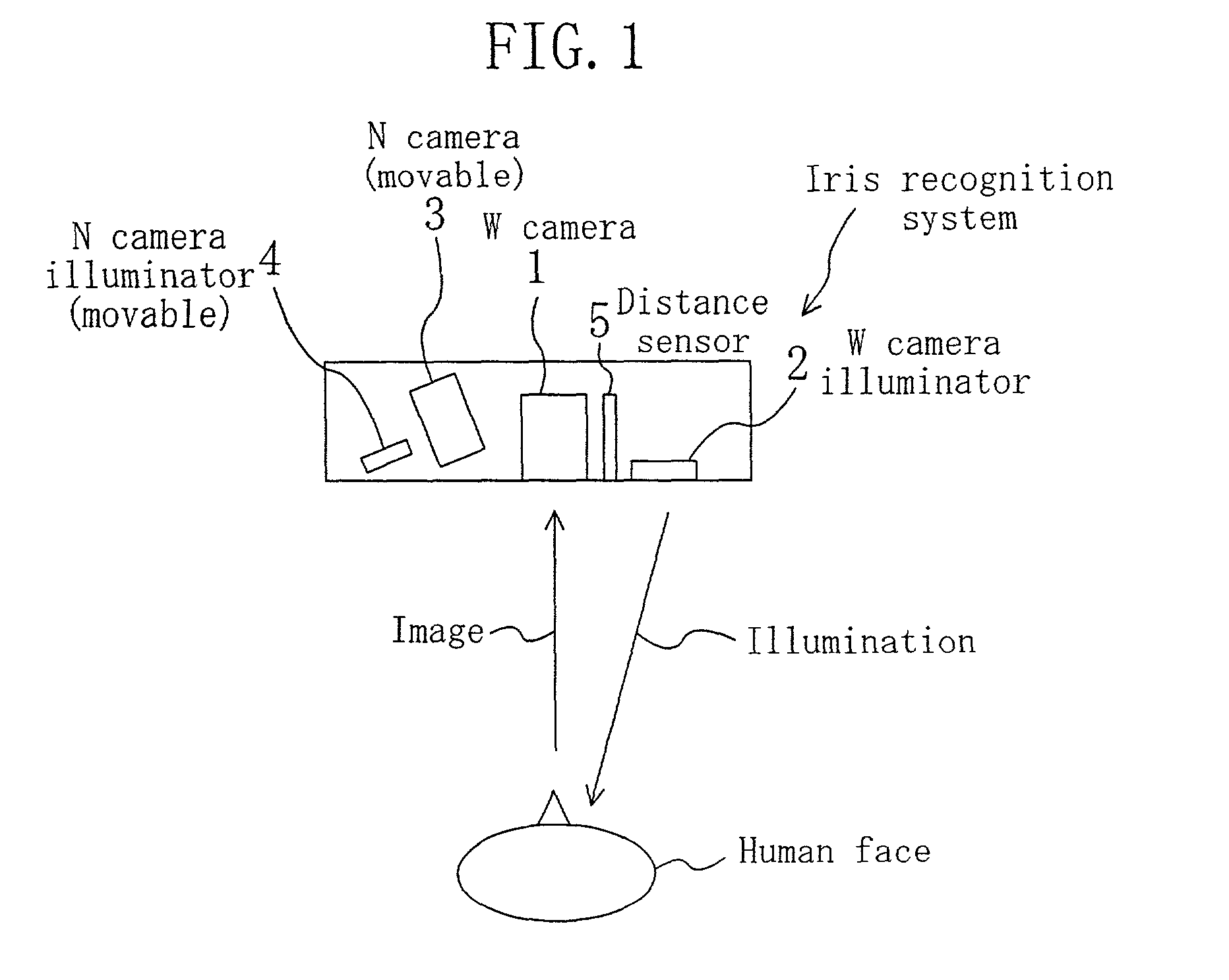
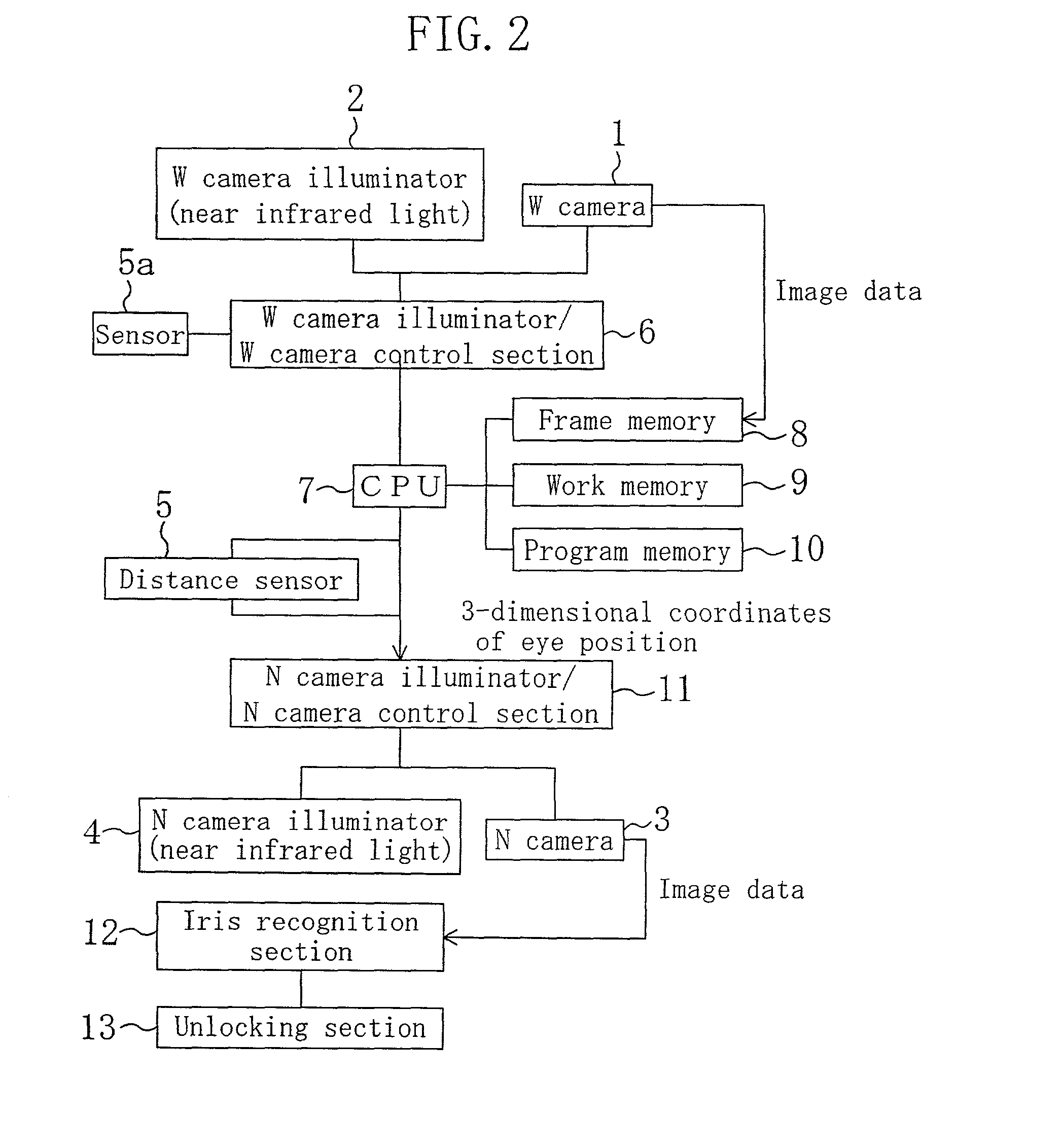
Eye position detection method and device
ActiveUS7130453B2Improve accuracyShort timeImage analysisPerson identificationPupilBrightness gradient
The position of an eye is detectable with high precision from a face image of a person taken under near infrared illumination or the like. After pre-processing, the face image is subjected to brightness correction to increase the contrast between the sclera portion and iris portion of the eye. Brightness gradient vectors are calculated for the brightness-corrected image, and matching is performed between a brightness gradient image generated using the calculated brightness gradient vectors and an eye template. Further, matching with a pupil template is performed to correct the eye center position. Final positions of both eyes are then determined.
Owner:PANASONIC CORP
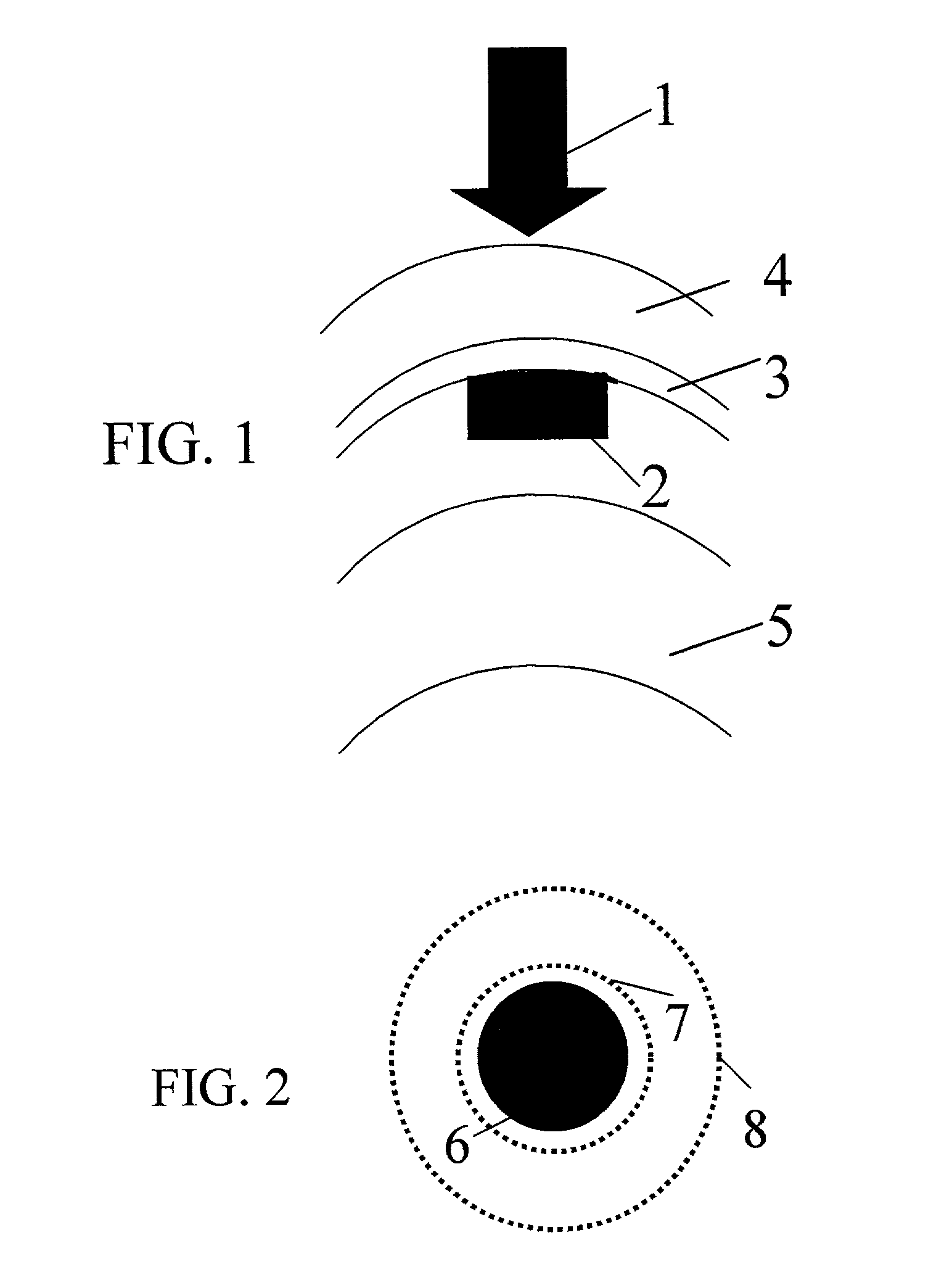
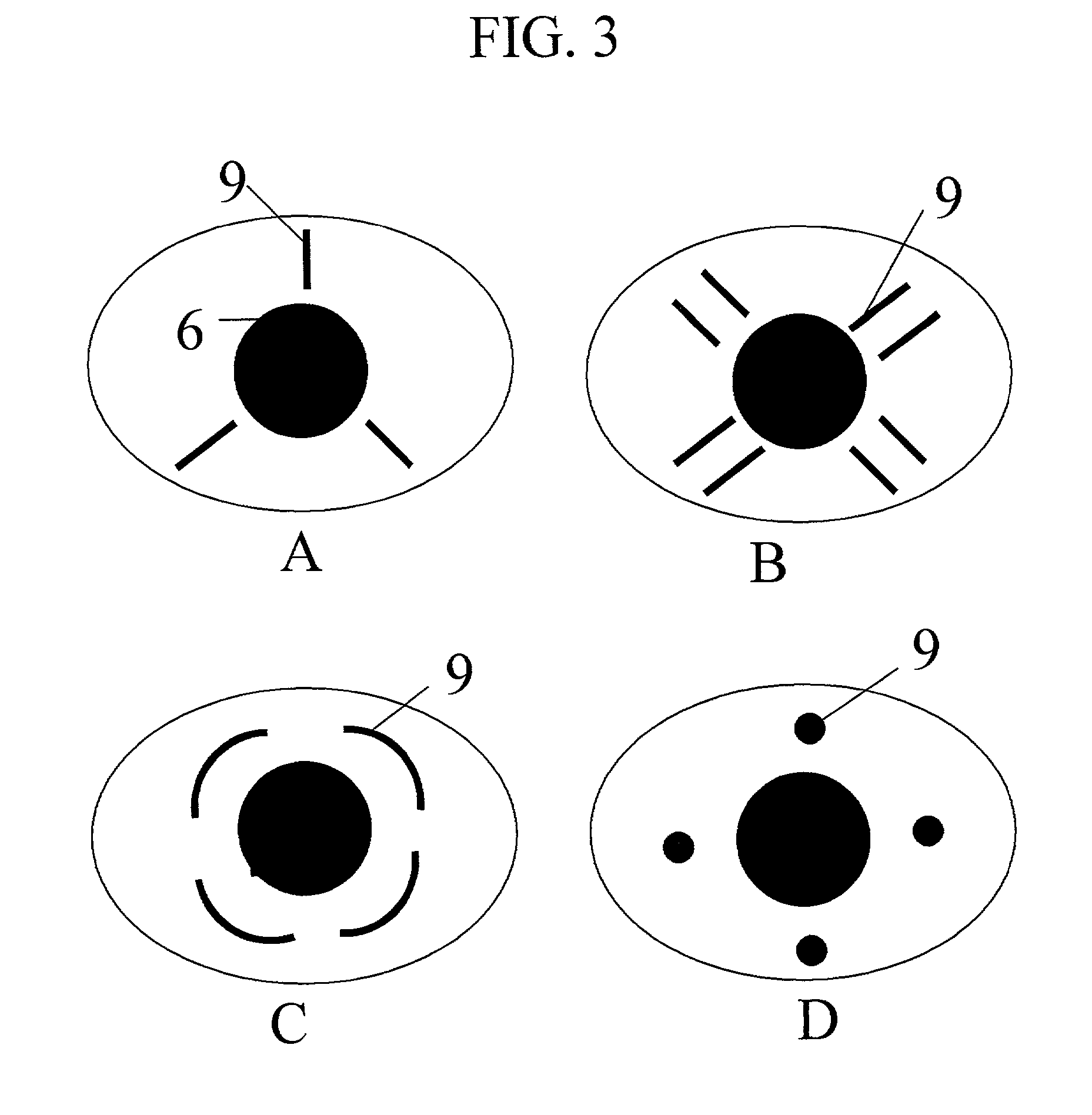
Method and apparatus for treatment of presbyopia by lens relaxation and anterior shift
A surgical method and apparatus for presbyopia correction removal of the sclera tissue are disclosed. Mechanisms based on sub-conjunctiva filled-in of the sclera area and cause the sclera-ciliary-body and zonule "complex" become more flexible (or less rigidity) are proposed. Total accommodation based a lens relaxation and lanes anterior shift is calculated and proposed as the guidance of the parameters for device design and clinical outcomes The preferred embodiments for the ablation patterns include radial lines, curved lines, ring dots or any non-specific shapes in a symmetric geometry. The surgery apparatus includes non-laser device of radio frequency wave, electrode device, bipolar device and plasma assisted device. Another preferred embodiment is to use post-operation medication such as pilocarpine (1%-10%) or medicines with similar nature which may cause ciliary body contraction for more stable and enhancement after the treatment.
Owner:LIN J T
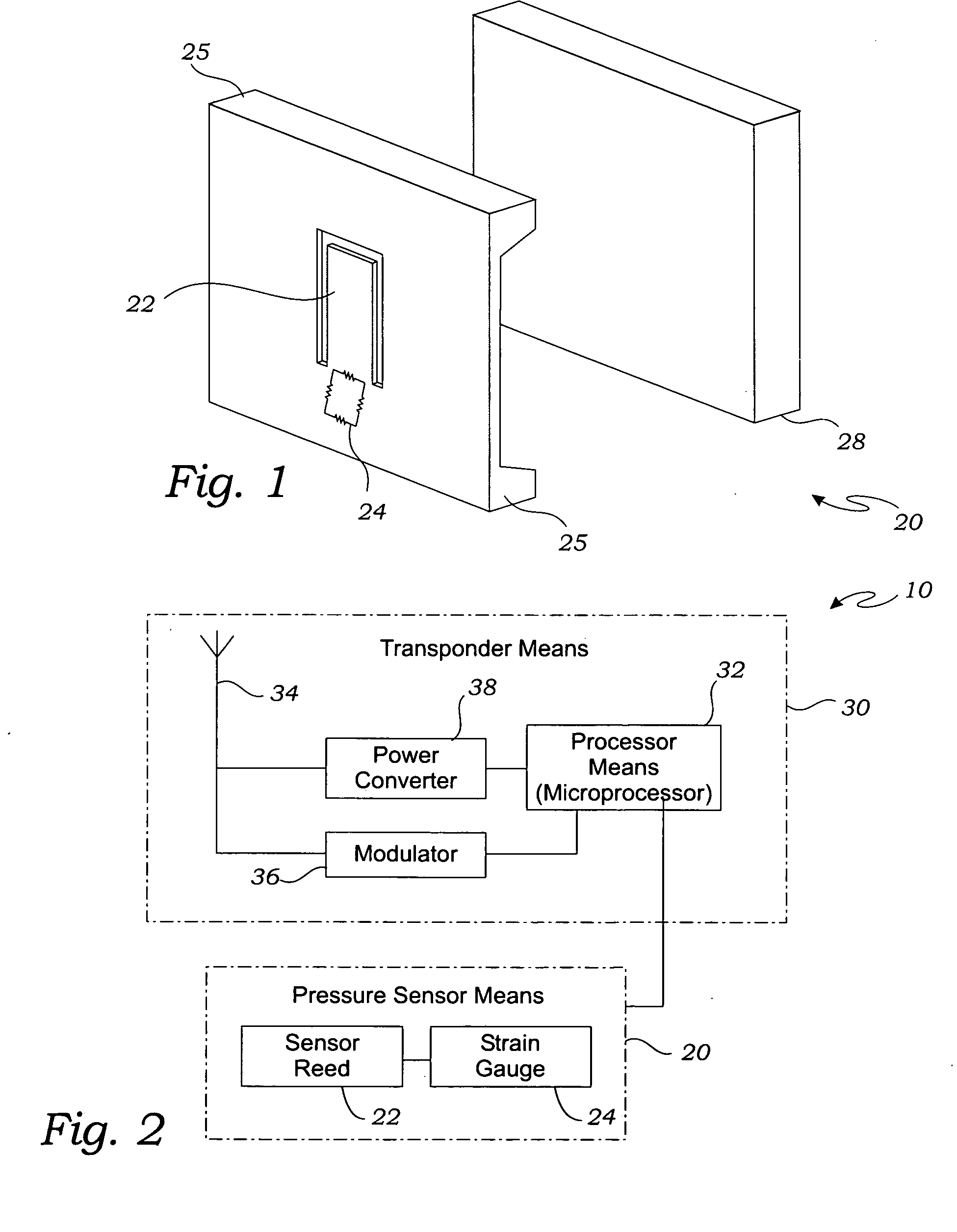
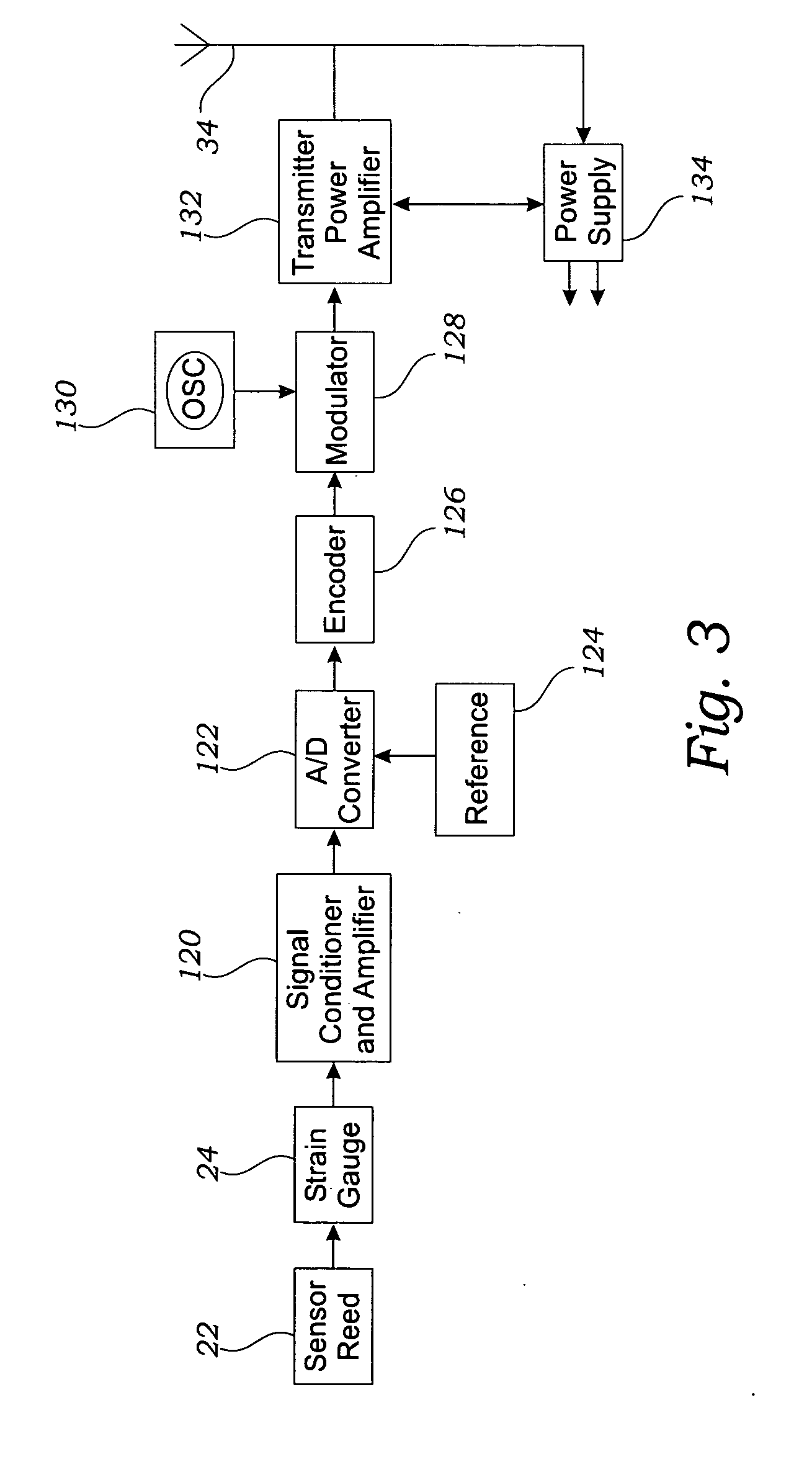
Intraocular pressure sensor and method of use
A method for measuring an intraocular pressure within an eye has several steps. An intraocular pressure sensor that is adapted to be implanted intrasclerally is provided. An incision is cut through a scleral layer of the eye. The scleral layer is lifted with a grasping tool. The intraocular pressure sensor is inserted under the scleral layer, and the incision of the scleral layer is closed.
Owner:MONTEGRANDE VALENTINO +1
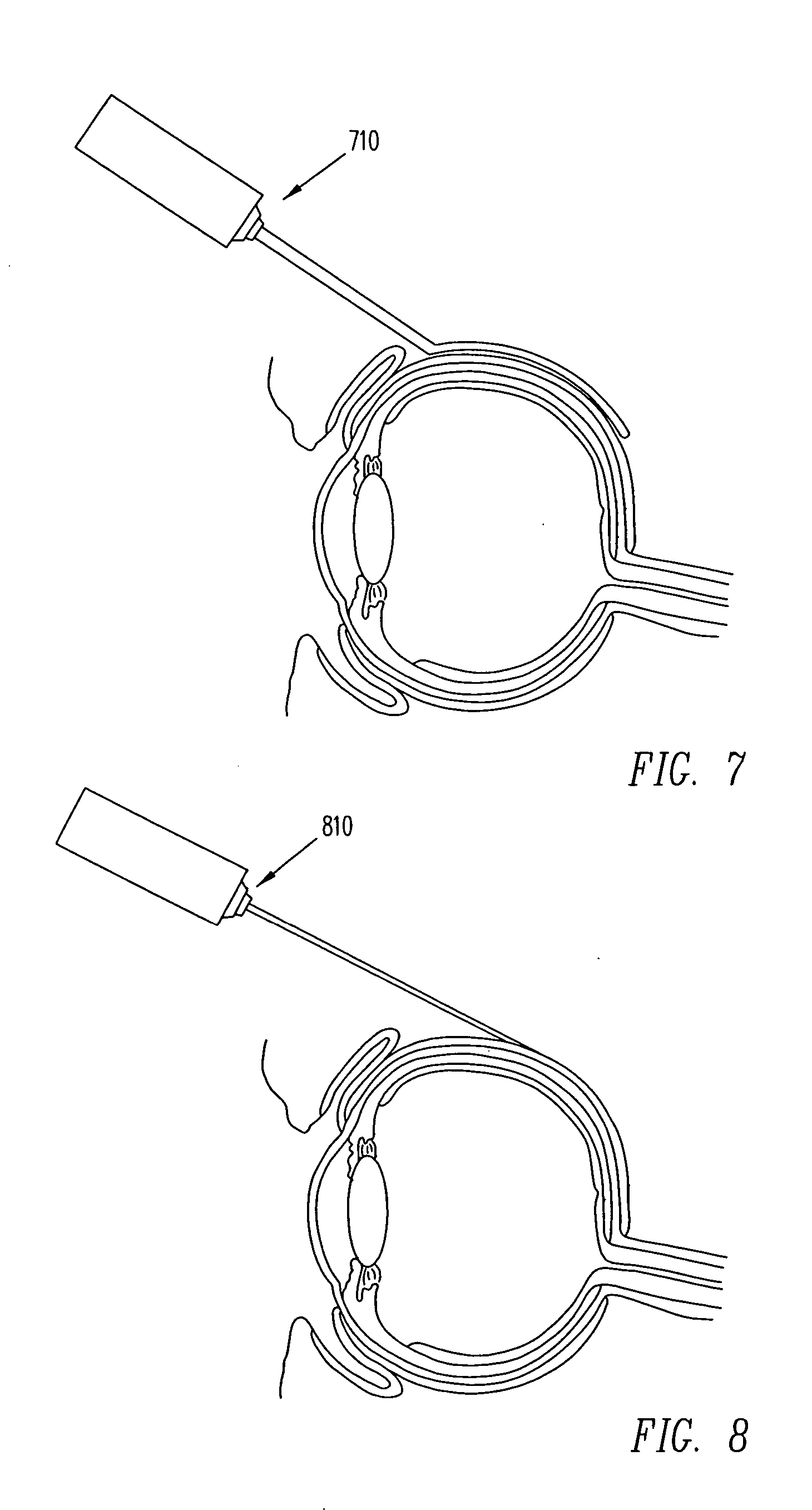
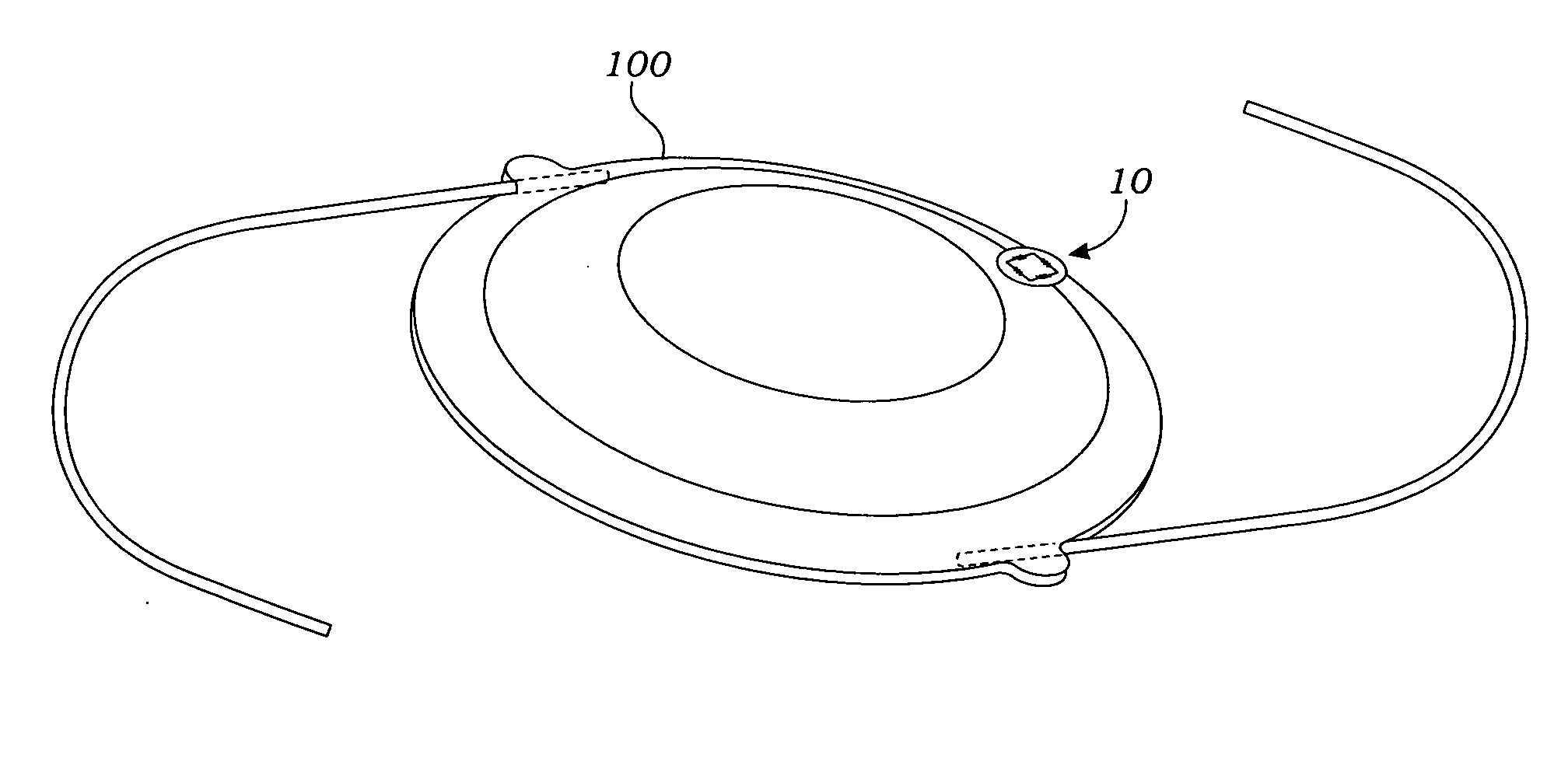
Implantable delivery device for administering pharmacological agents to an internal portion of a body
InactiveUS20060258994A1Injection is simpleGood curative effectMedical applicatorsEye treatmentProximateImplanted device
An implantable refillable device to deliver pharmacologic agents through a sclera to an internal portion of an eye is shown. The device comprises a hollow reservoir and a delivery tube. The delivery tube has a proximal end and a distal end. The proximal end communicates with the hollow reservoir and the distal end terminates in a dispensing outlet. The delivery tube is configured in a selected shape to extend from the hollow reservoir anterior in an eye to a posterior segment posterior in an eye adjoining a sclera. The second end is configured to position the dispensing outlet in contact with or contiguous the sclera and is located posteriorly in an eye and proximate to an internal portion of an eye to be treated with a pharmacologic agent. An implantable device to deliver pharmacologic agents through an outer surface tissue of an organ is also shown.
Owner:AVERY ROBERT L
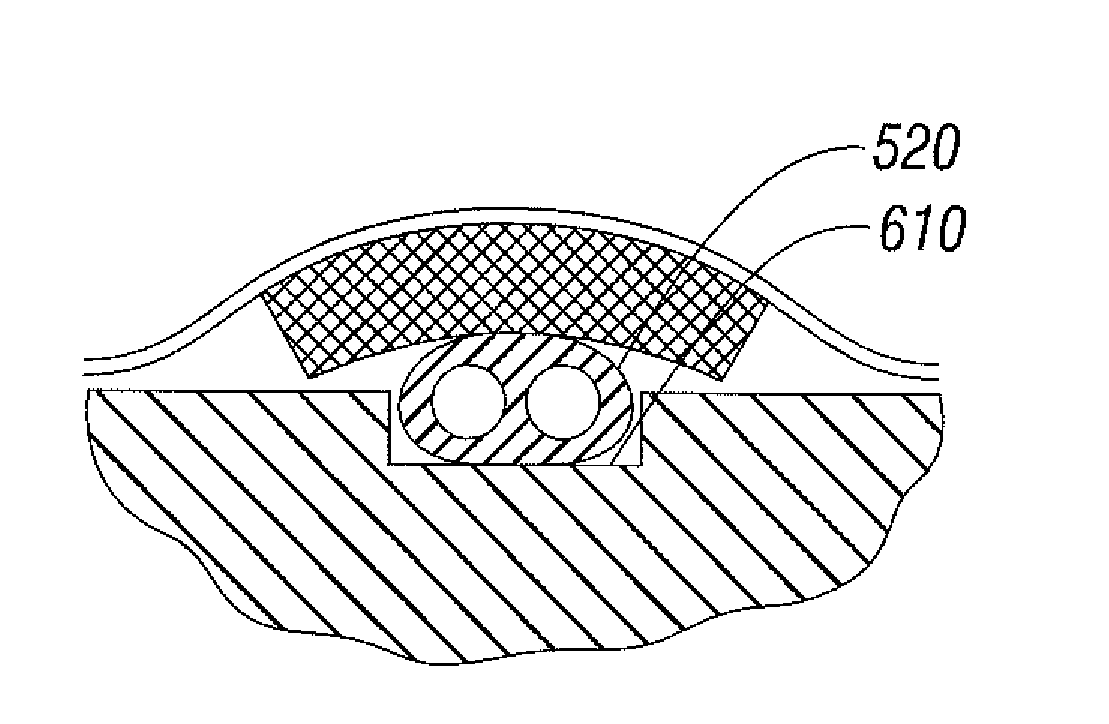
Uveoscleral shunt and methods for implanting same
ActiveUS8506515B2Lower eye pressureSmall sectionSenses disorderEar treatmentCiliary bodySuprachoroidal space
Devices and methods for treating intraocular pressure are disclosed. The devices include shunts for draining aqueous humor from the anterior chamber to the uveoscleral outflow pathway, including the supraciliary space and the suprachoroidal space. The shunts are preferably implanted by ab interno procedures.
Owner:GLAUKOS CORP
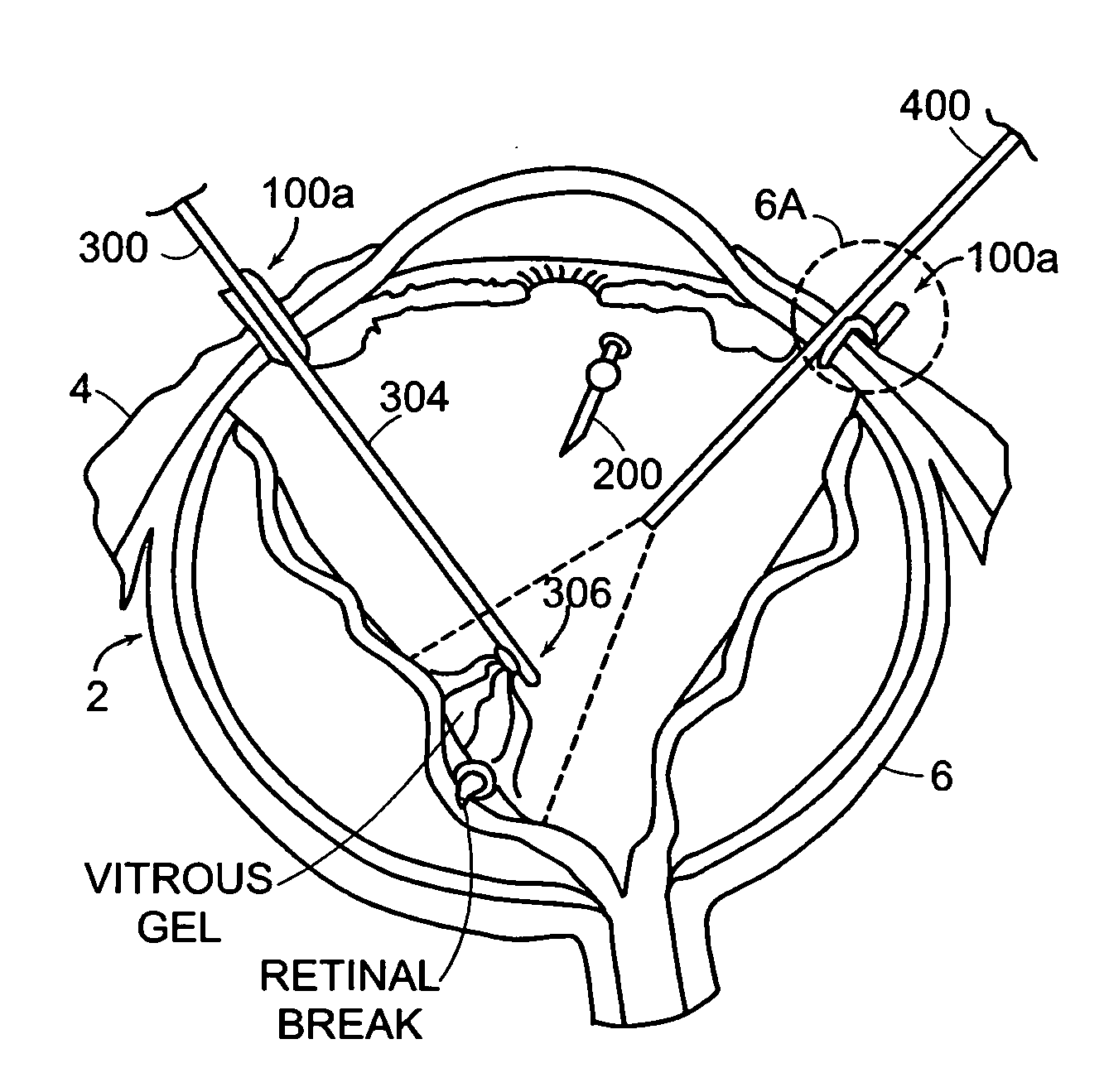
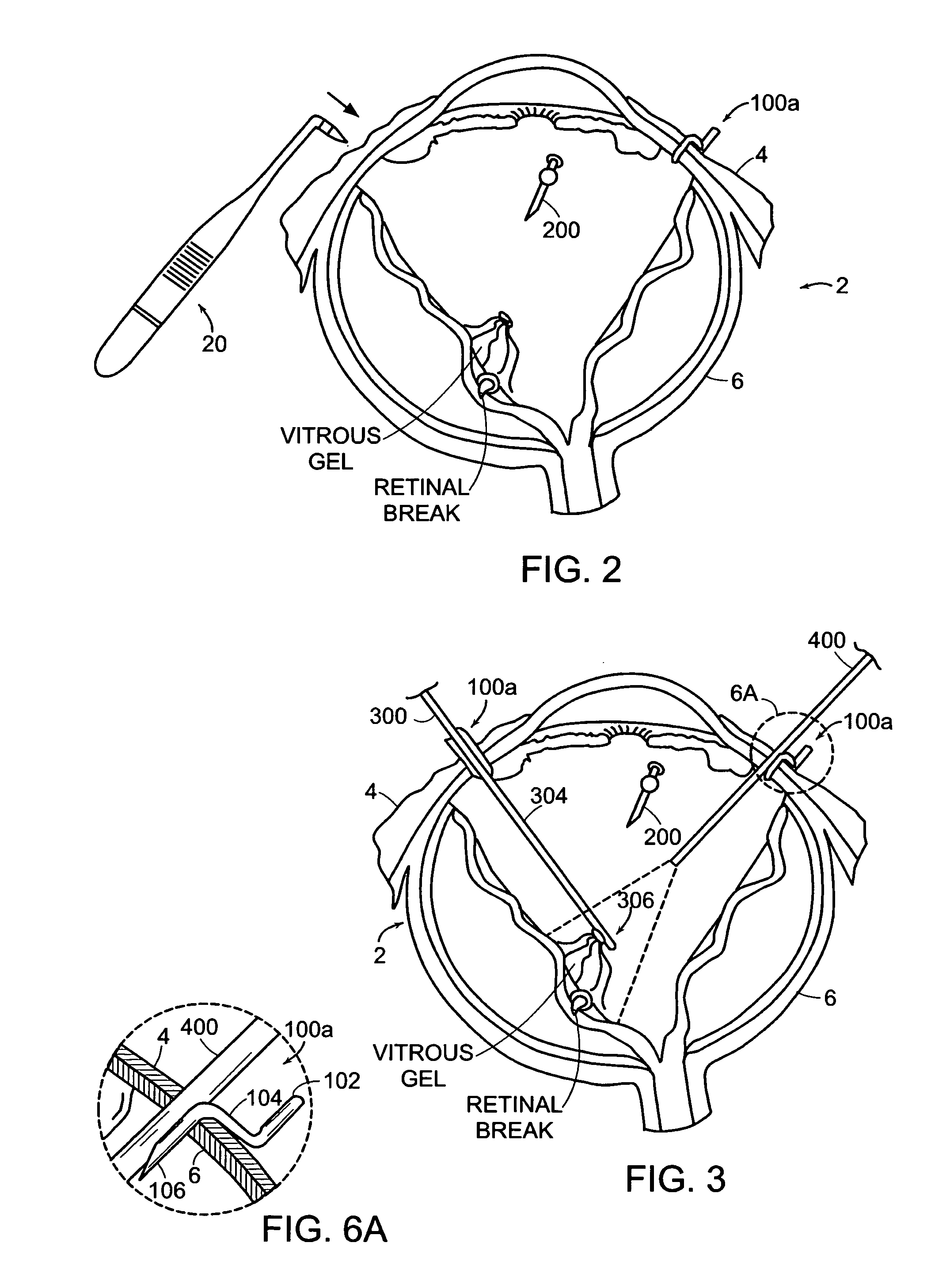
Sutureless occular surgical methods and instruments for use in such methods
Featured are new methods for performing intra-ocular surgery that allow surgical personnel to access the intra-ocular volume to perform a surgical procedure or technique but which does not require the use of sutures to seal the sclera and / or conjunctiva following the procedure. The methods of the present invention generally include providing an entry alignment device and inserting the entry alignment device into an eye through both the conjunctiva and sclera so as to form an entry aperture that extends between the exterior of the eye and the intra-ocular volume within the eye. The provided alignment device is configured so as to form or provide an aperture or opening in each of the conjunctiva and sclera of the eye and to maintain these apertures or openings in each of the conjunctiva and sclera aligned during the surgical procedure so these apertures or openings form the entry aperture. In more particular aspects, the provided entry alignment device is sized such that when the entry alignment device is removed from the eye following the completion of the surgical procedure, the aperture or opening formed in the sclera seals without the use of sutures. In a more specific aspect of the present invention, the provided entry alignment device is sized such that the apertures or openings and thus the entry aperture are self sealing. In other embodiments, a plurality of entry alignment devices are provided so a plurality of entry apertures can be formed in the eye. The invention also features a high speed vitreous cutting and aspirating device particularly configured for use in such methods and surgical procedures and techniques as well as the related entry alignment devices and other surgical instruments.
Owner:THE JOHN HOPKINS UNIV SCHOOL OF MEDICINE
Ophthalmic drug delivery device
An ophthalmic drug delivery device having a scleral surface, an orbital surface, an injection port on the orbital surface, and a fluid conducting passageway disposed within the device that is fluidily coupled to the injection port and terminates in an opening for communicating the fluid to an outer surface of the sclera is disclosed. The fluid contains a pharmaceutically active agent useful for the treatment of a disease of the posterior segment of the eye.
Owner:NOVARTIS AG
Treatment of myopia
InactiveUS20050271590A1Improve mechanical stabilityHigh modulusUltrasonic/sonic/infrasonic diagnosticsSenses disorderMedicineUltimate tensile strength
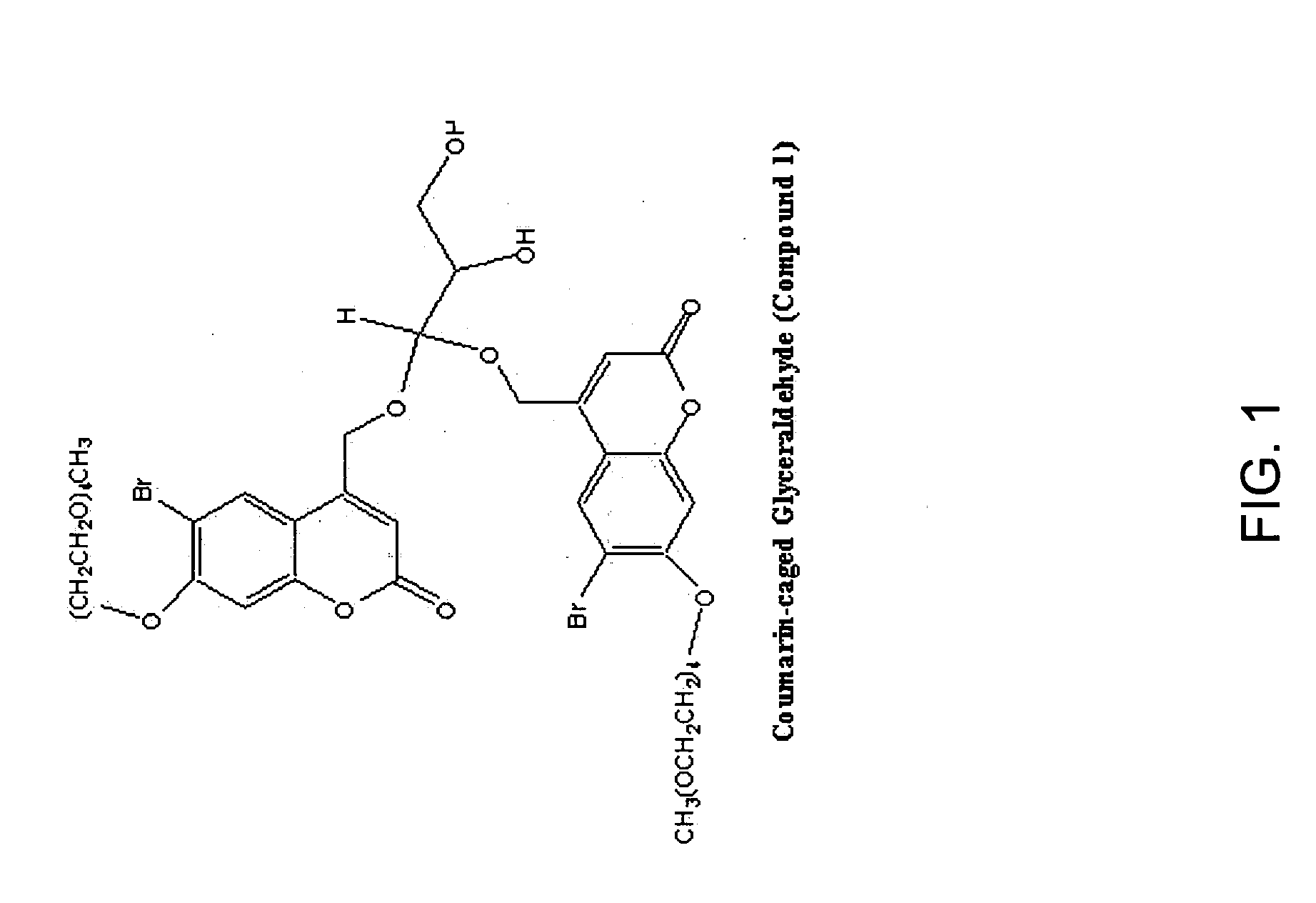
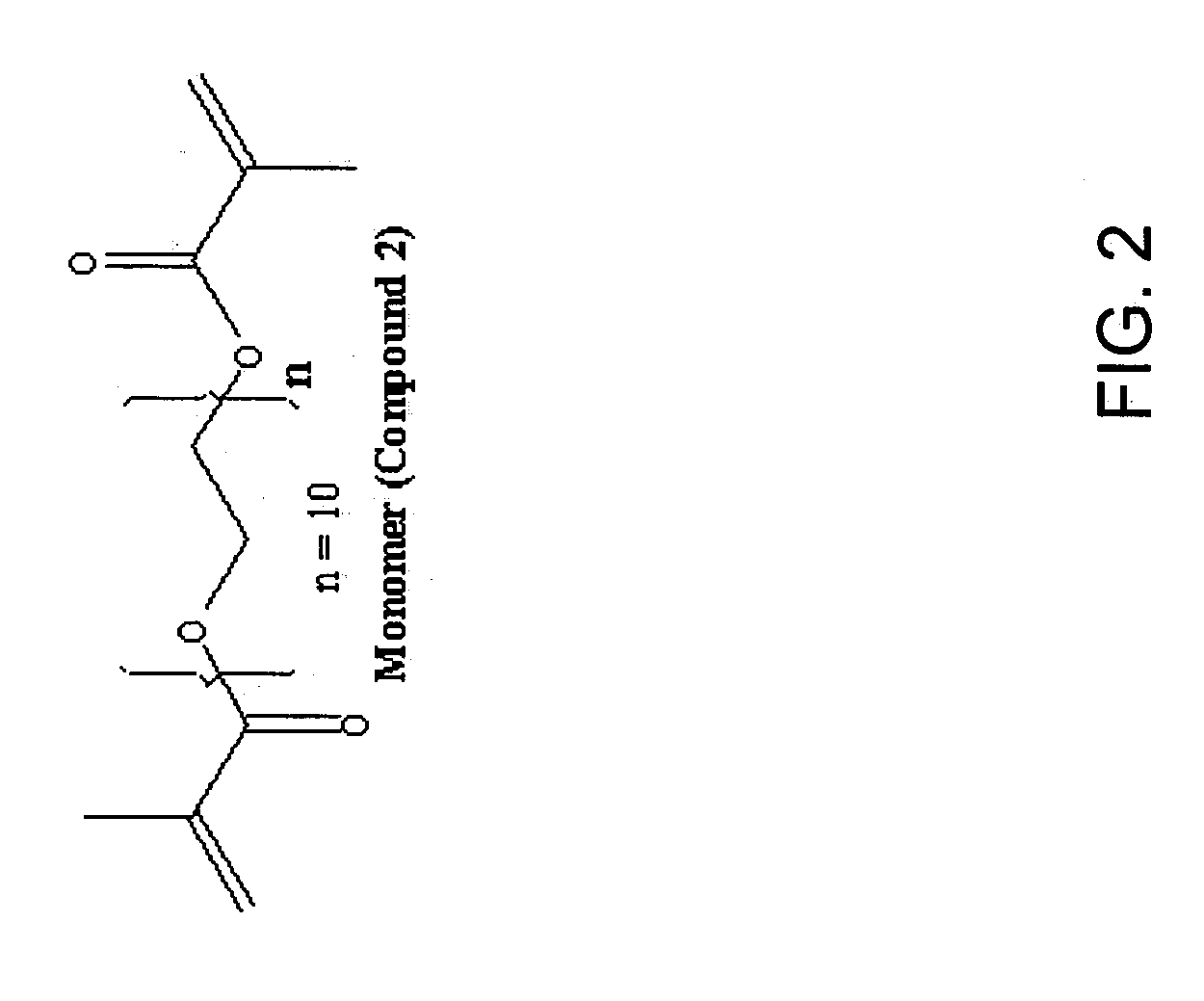
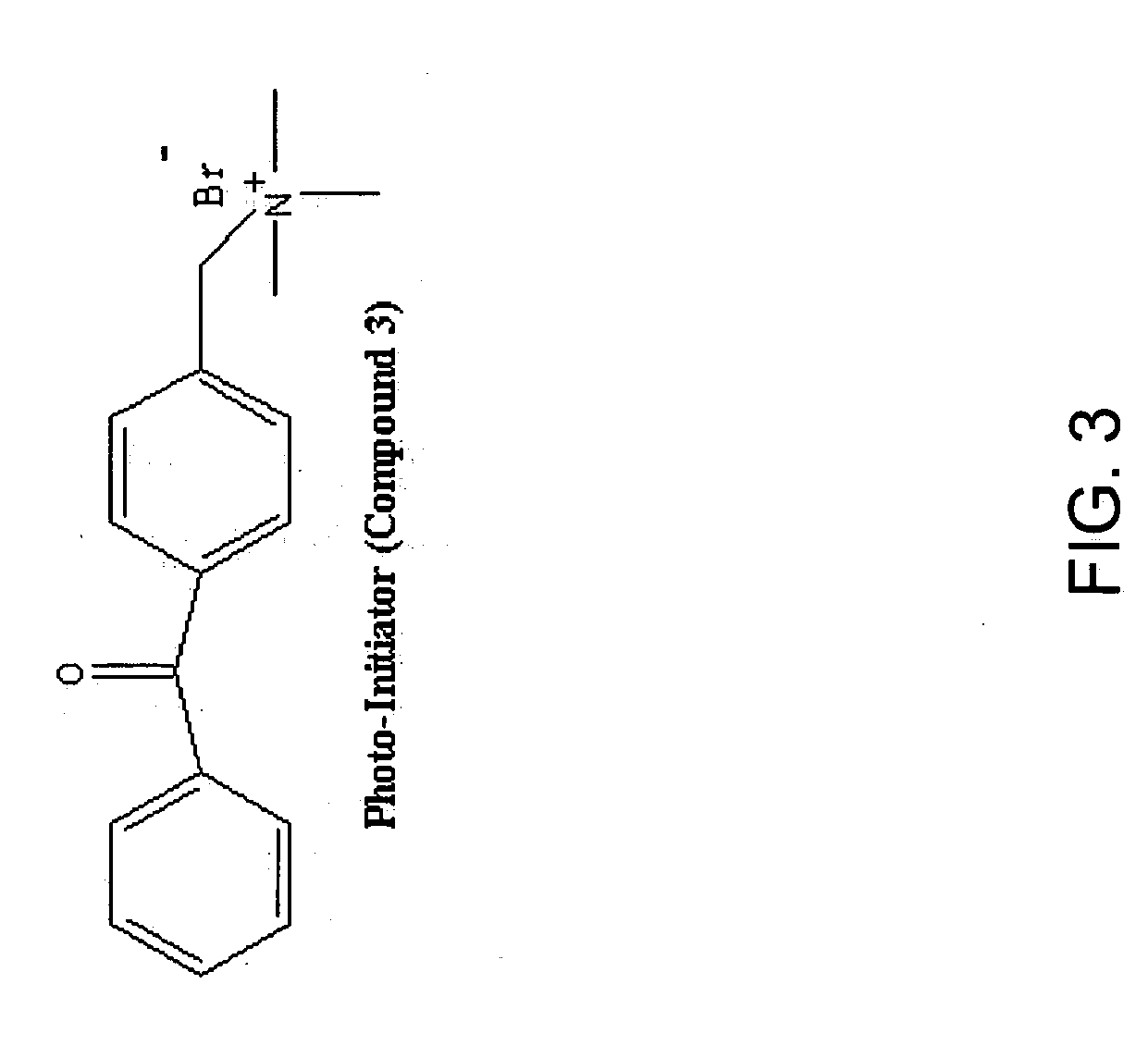
The present invention relates to altering the physical and / or chemical properties of at least part of at least one tissue in the eye. In a specific embodiment, it relates to the treatment and / or prevention of myopia. An activating energy source is utilized to photopolymerize or crosslink molecules in the sclera, thereby increasing the strength of the tissue. The individual is administered a crosslinking reagent or photopolymerizable molecule that becomes associated with the membrane, which is then precisely exposed to an energy source, such as light or ultrasound.
Owner:CALIFORNIA INST OF TECH +1
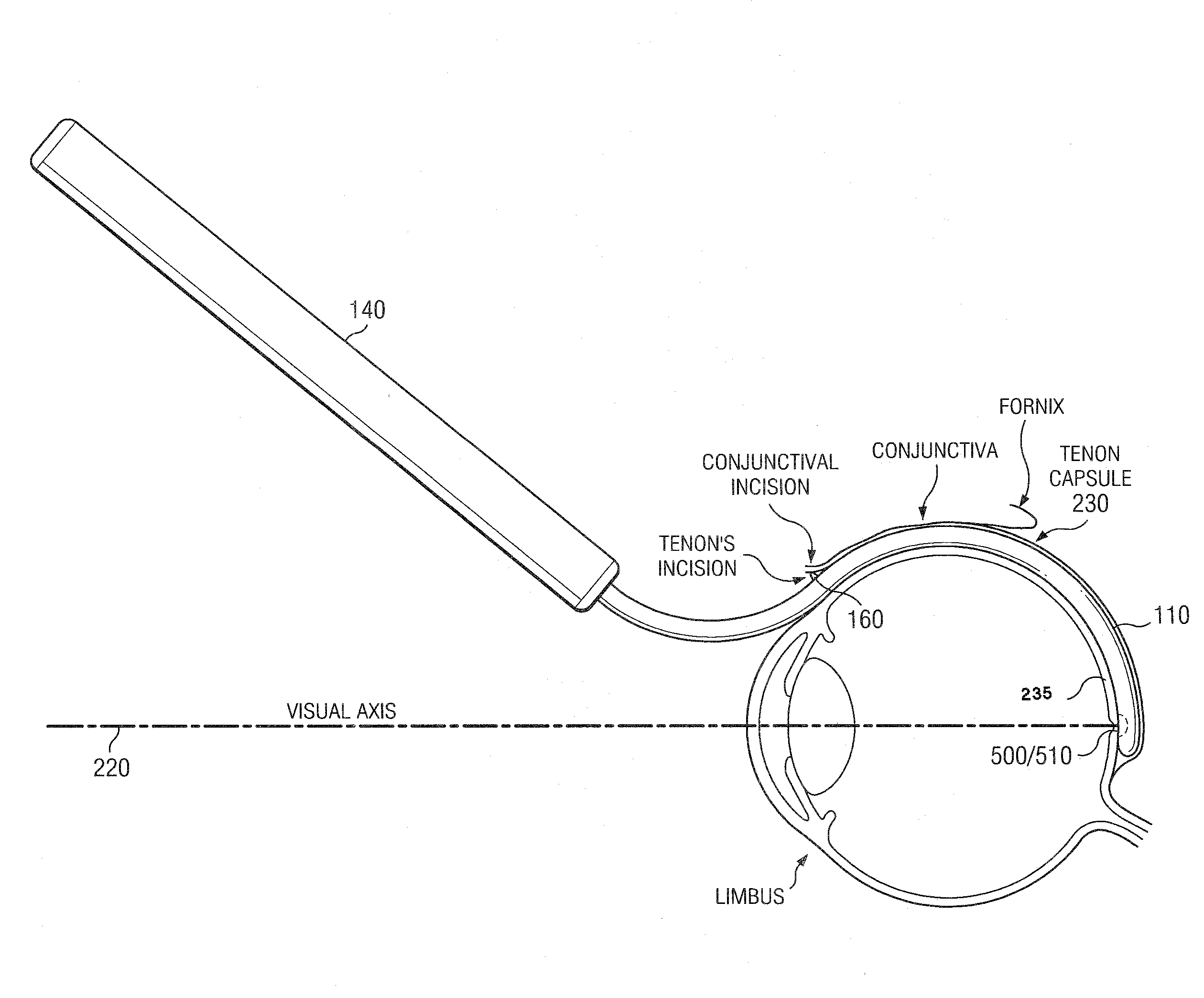
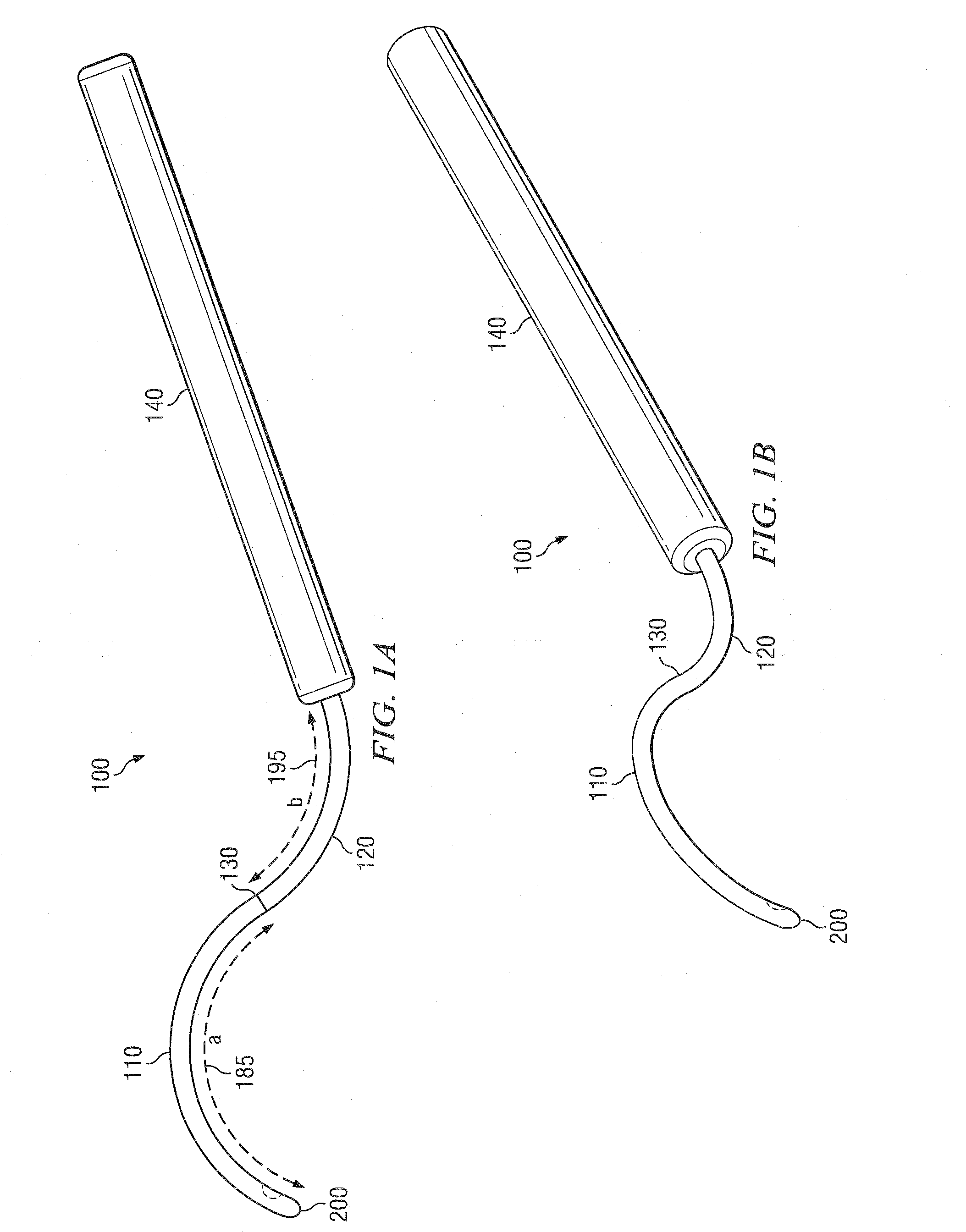
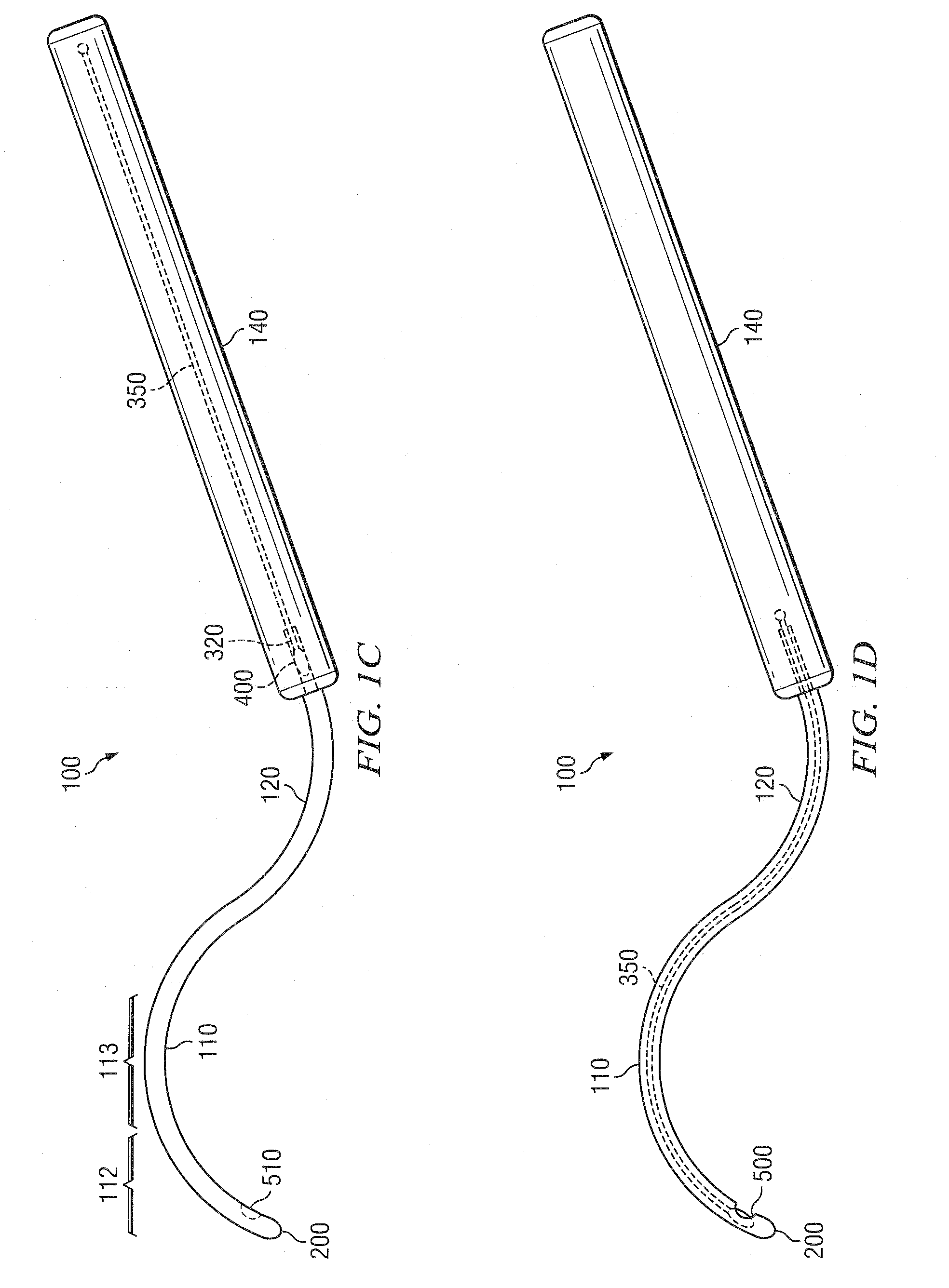
Methods and devices for minimally-invasive extraocular delivery of radiation to the posterior portion of the eye
Methods and devices for minimally-invasive delivery of radiation to the posterior portion of the eye including a cannula comprising a distal portion connected to a proximal portion and a means for advancing a radionuclide brachytherapy source (RBS) toward the tip of the distal portion; a method of introducing radiation to the human eye comprising inserting a cannula between the Tenon's capsule and the sclera of the human eye and emitting the radiation from the cannula on an outer surface of said sclera.
Owner:SALUTARIS MEDICAL DEVICES INC
Method for drug delivery to ocular tissue using microneedle
Methods and devices are provided for administering a drug to a patient's eye. The methods include (a) inserting a hollow microneedle into the sclera or corneal stroma without penetrating across the sclera or corneal stroma; and (b) infusing a fluid drug formulation through the microneedle and into the sclera or cornea. It further may include partially retracting the microneedle before infusion to enhance delivery. Alternatively, the methods may include (a) inserting a solid microneedle into the sclera or corneal stroma without penetrating across the sclera or corneal stroma, wherein the solid microneedle comprises a first quantity of a drug formulation and inserting causes the solid microneedle to form a pocket in the sclera or corneal stroma; and (b) releasing the drug formulation into the pocket to form a drug depot, whereby a drug is released from the depot. The methods and devices may include an array of multiple microneedles.
Owner:GEORGIA TECH RES CORP +1
Scleral prosthesis for treatment of presbyopia and other eye disorders
InactiveUS6299640B1Increase the effective working distanceIncrease the working distanceLaser surgeryEye implantsDiseaseOpen angle glaucoma
Presbyopia is treated by implanting within a plurality of elongated pockets formed in the tissue of the sclera of the eye transverse to a meridian of the eye, a prosthesis having an elongated base member having an inward surface adapted to be placed against the inward wall of the pocket and having a ridge on the inward surface of the base extending along at least a major portion of the major dimension of the base. The combined effect of the implanted prostheses is to exert a radially outward traction on the sclera in the region overlying the ciliary body which expands the sclera in the affected region together with the underlying ciliary body. The expansion of the ciliary body restores the effective working distance of the ciliary muscle in the presbyopic eye and thereby increases the amplitude of accommodation. Hyperopia, primary open angle glaucoma and / or ocular hypertension can be treated by increasing the effective working distance of the ciliary muscle according to the invention.
Owner:REFOCUS GROUP
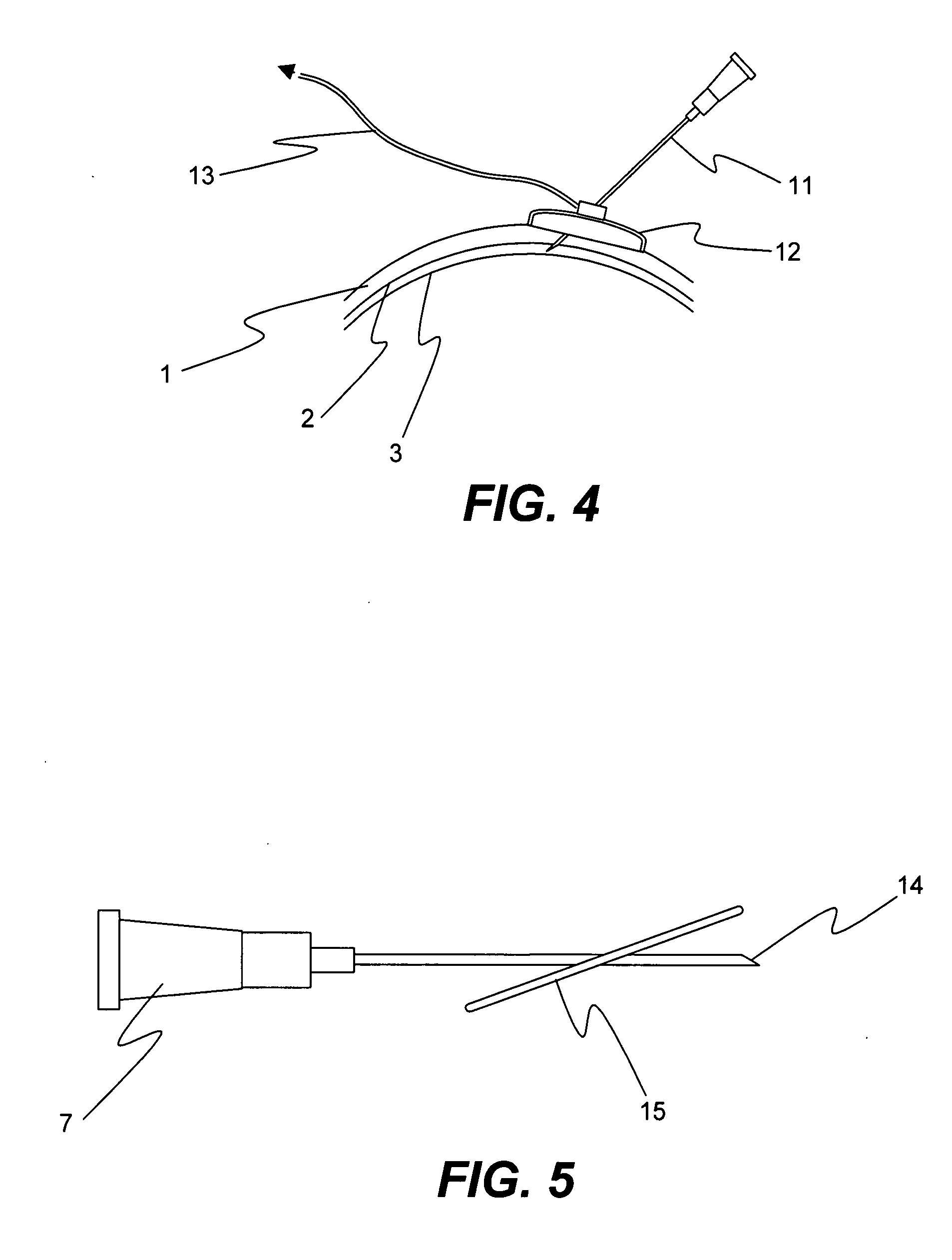
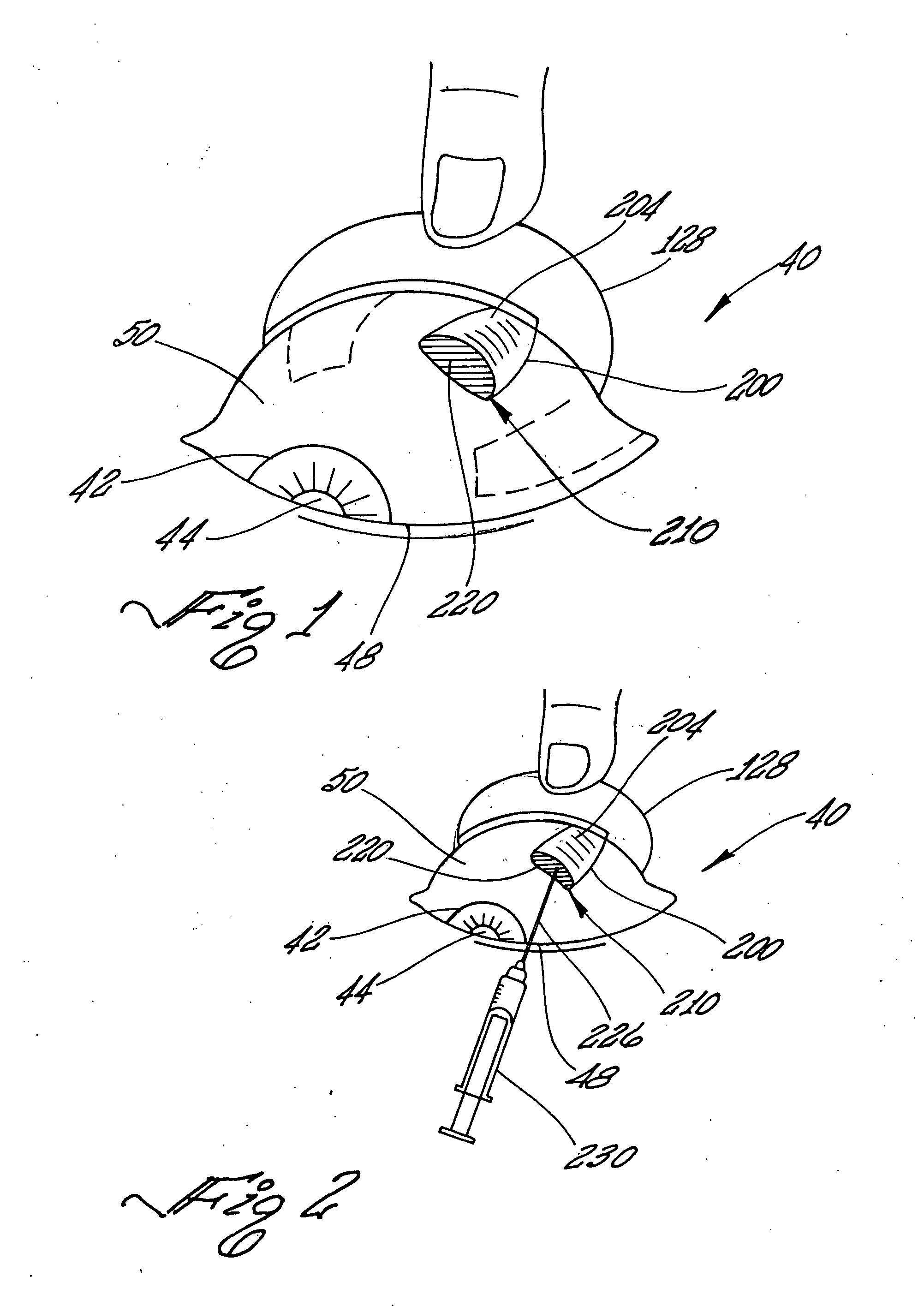
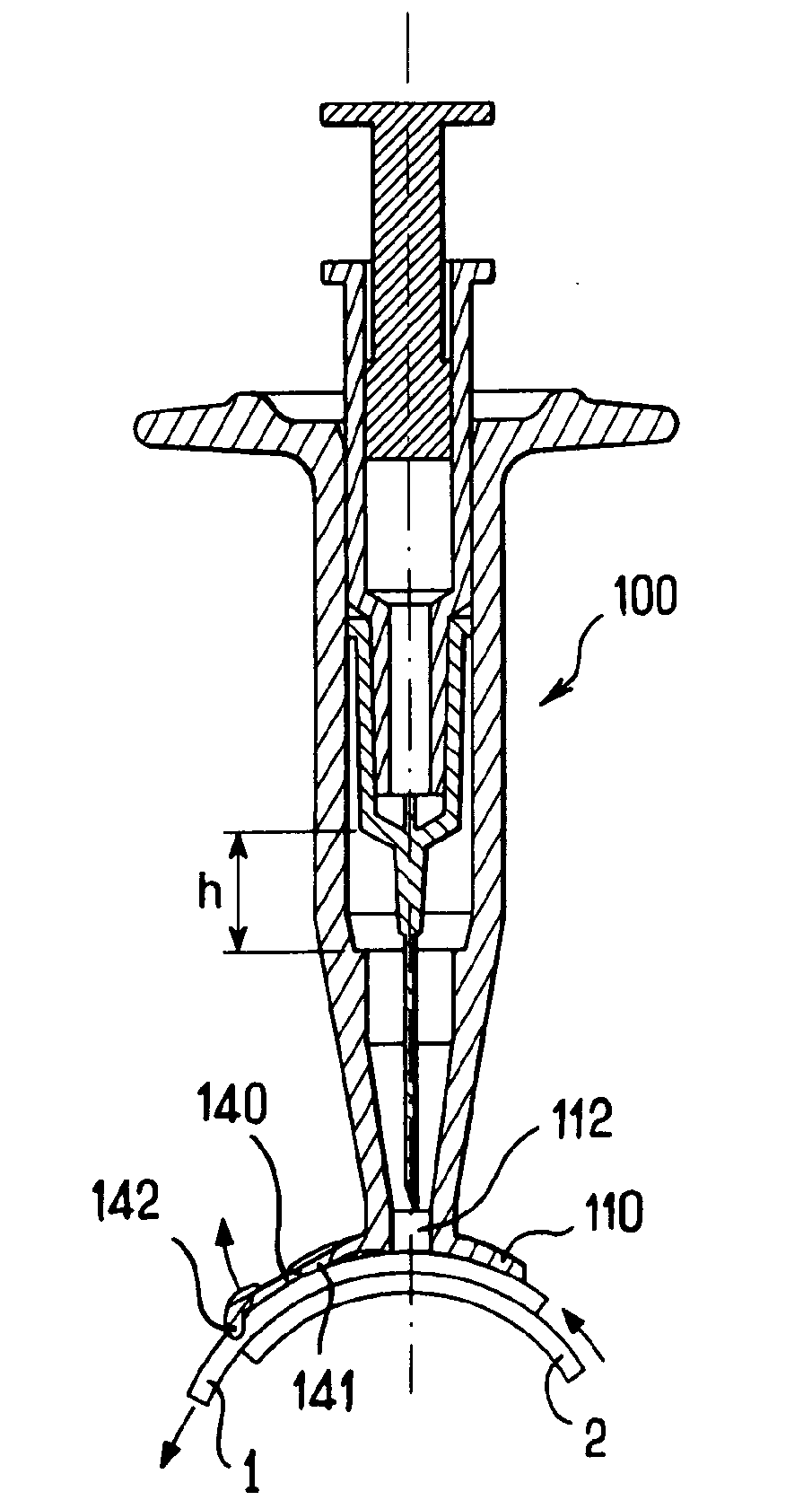
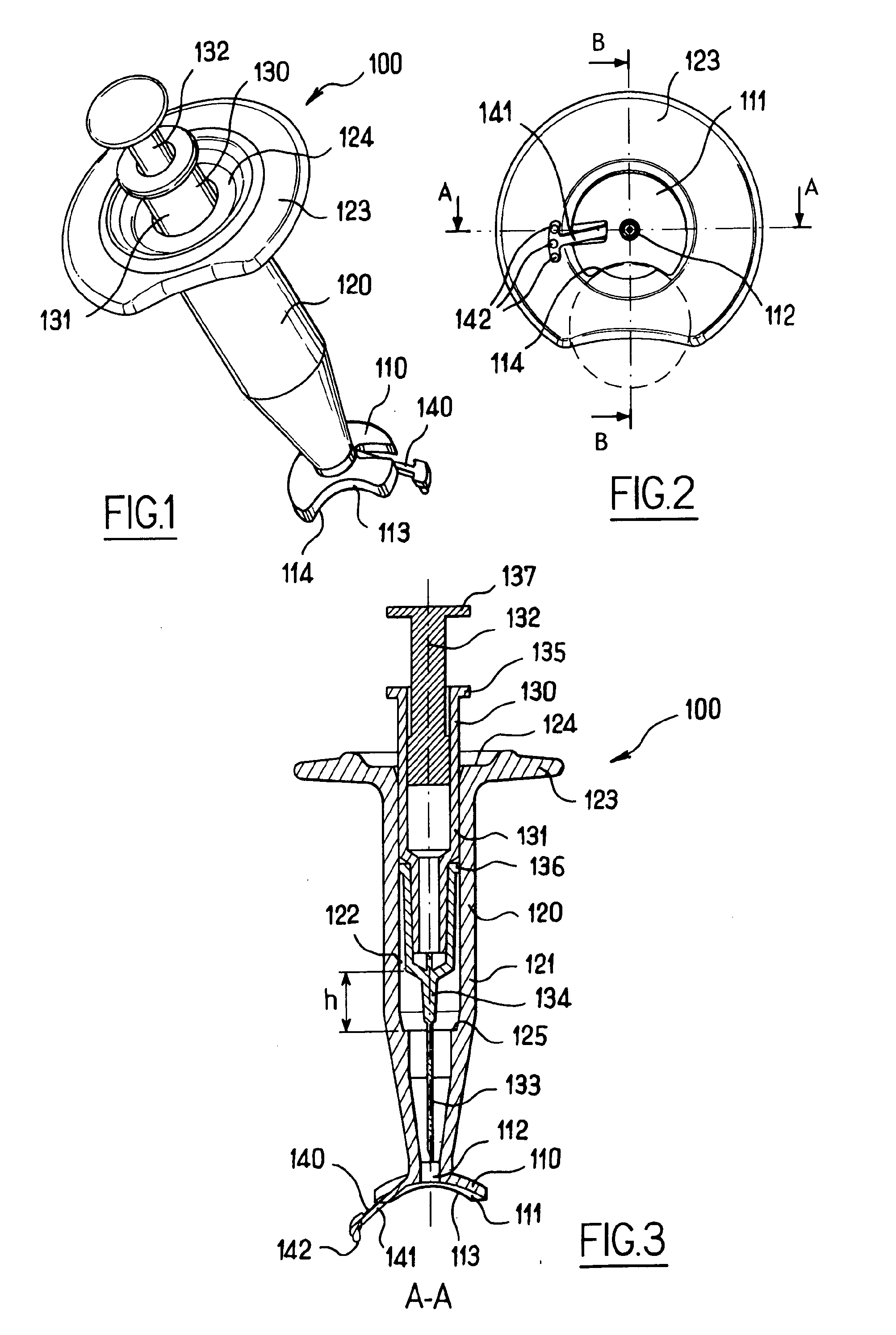
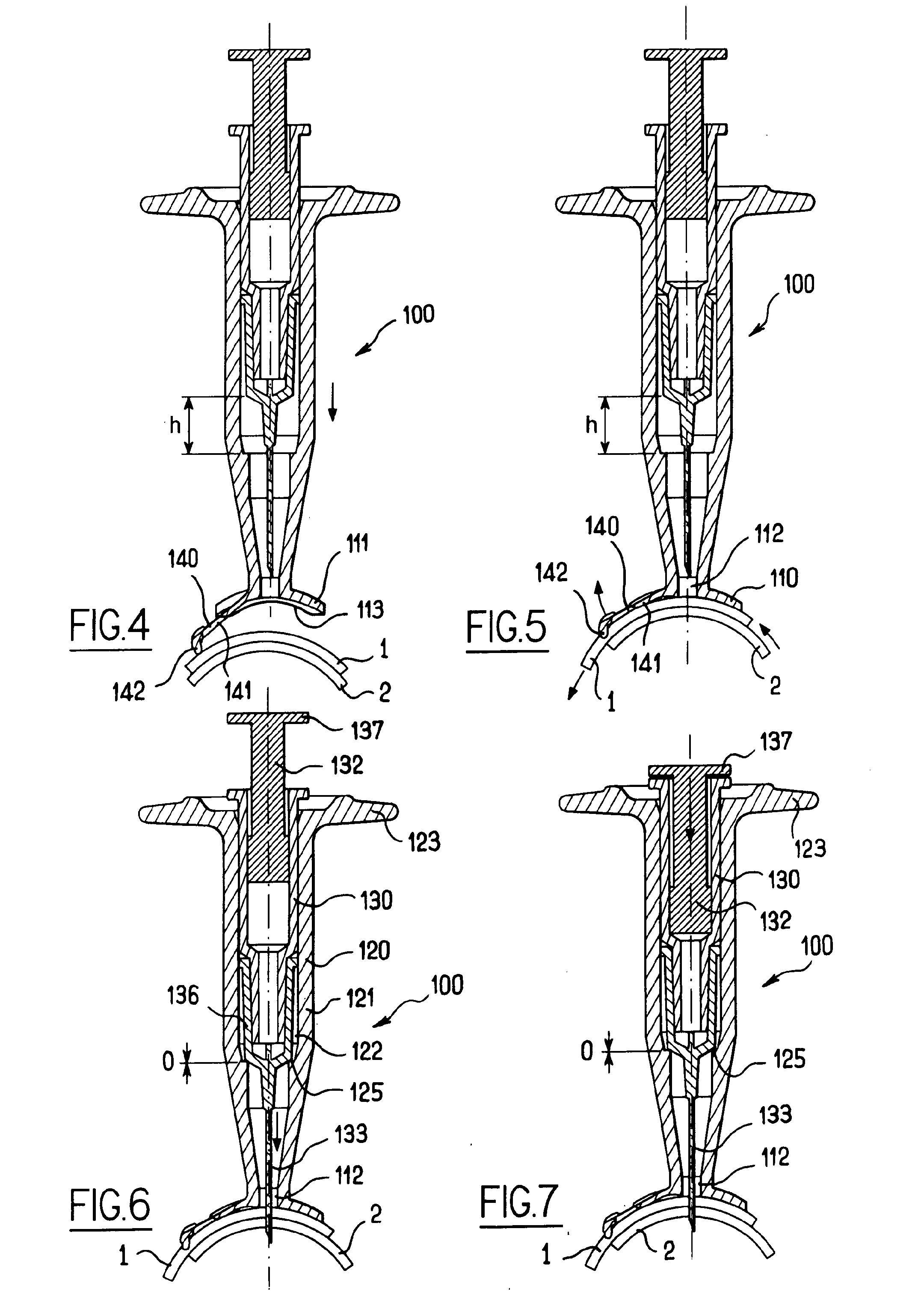
Apparatus for intra-ocular injection
The application relates to an apparatus for intraocular injection comprising a plate adapted for being brought into contact with an eye and guiding means for guiding a needle into the interior of an eye, characterized in that the plate comprises a cut-out having an edge adapted to be positioned along the limbus delimiting the cornea and the sclera of the eye, so as to adjust the position of the guiding means with respect to the limbus.
Owner:FOVEA PHARMA +1
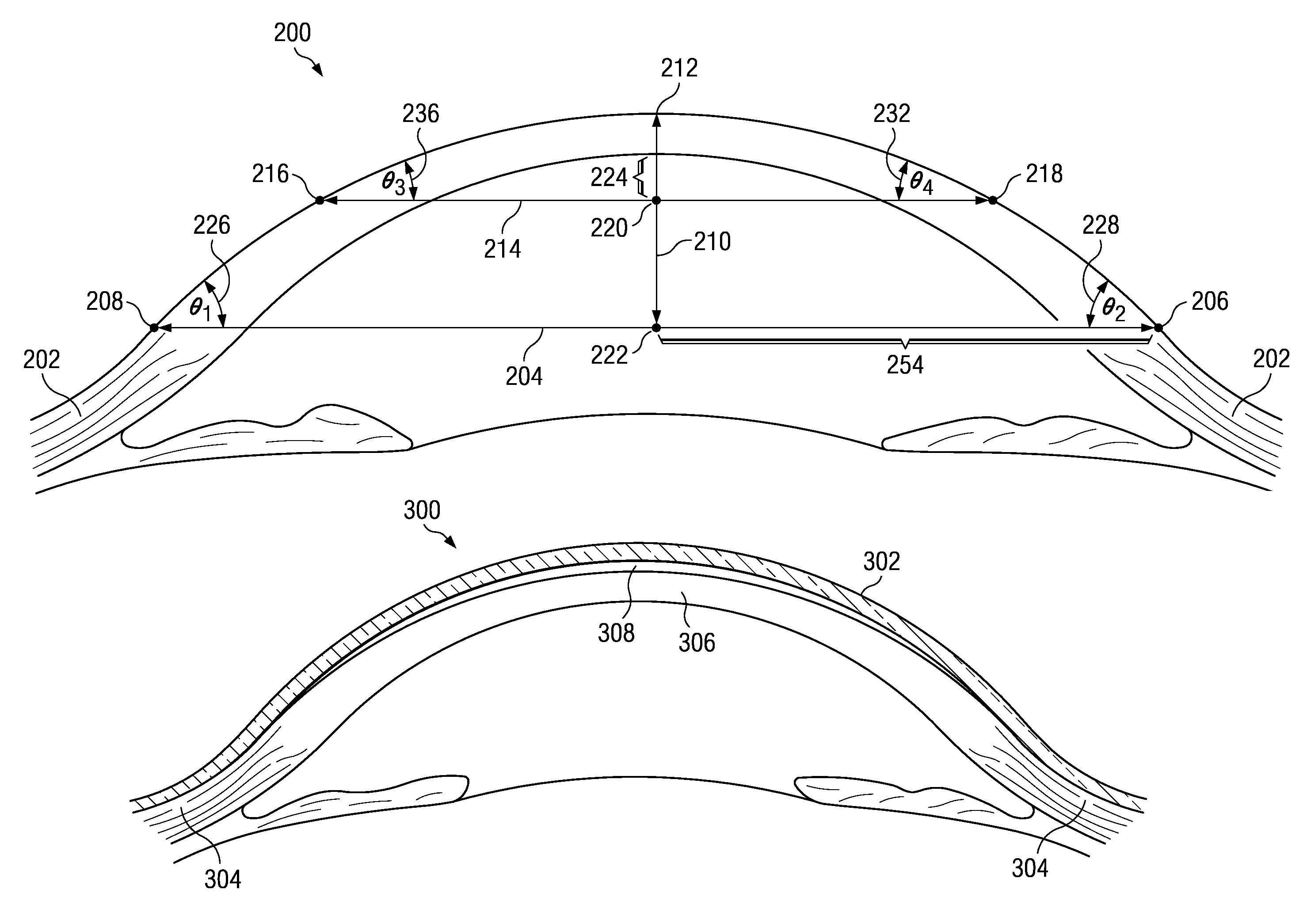
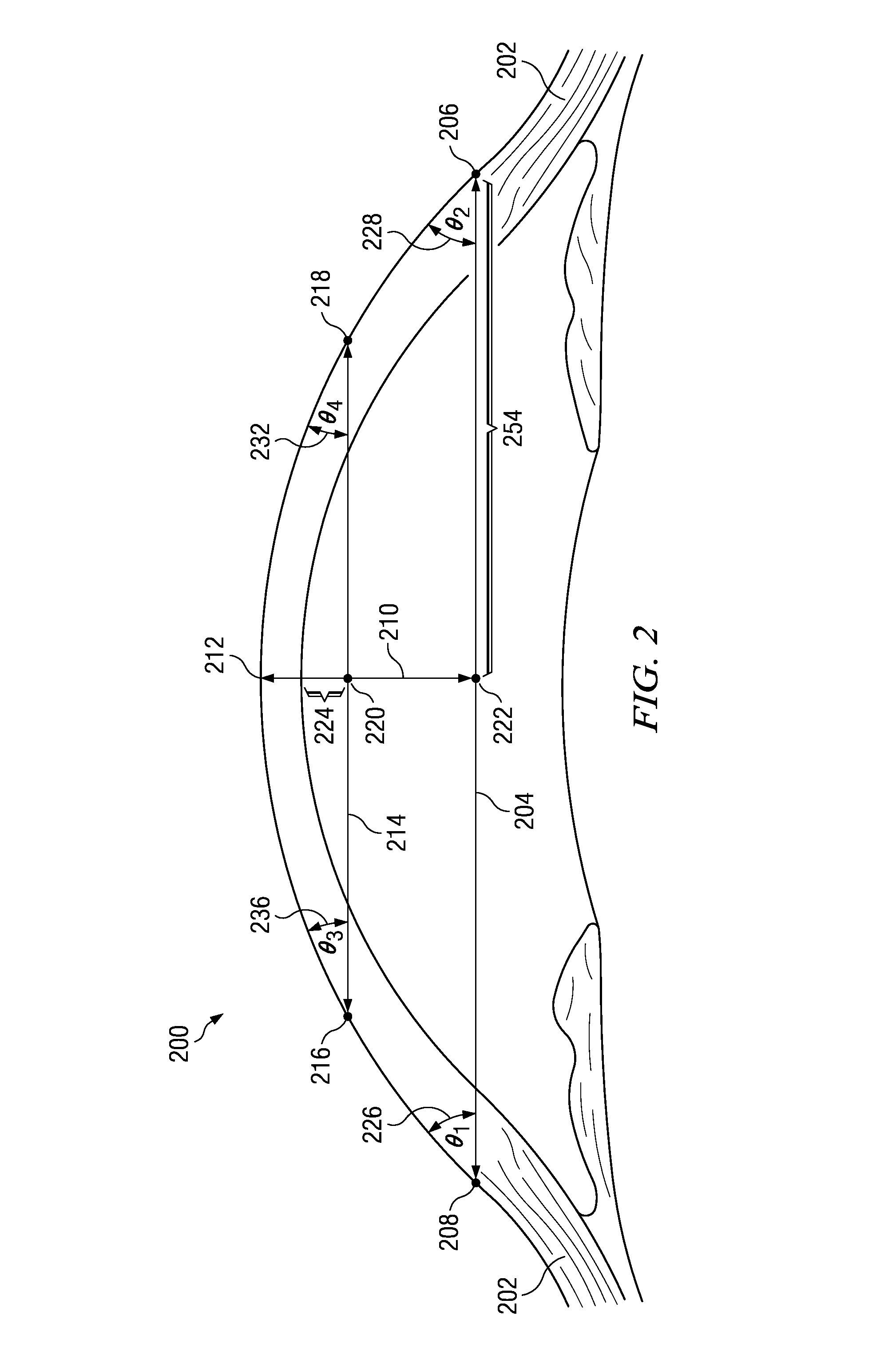
Method of fitting rigid gas-permeable contact lenses from high resolution imaging
A method, computer program product, and data processing system for designing a contact lens. A sagittal image of an anterior portion of an eye having a sclera is measured. Measuring is performed using a digital imaging device. Measuring includes measuring the sclera. A sagittal image is formed. A shape of the eye is derived using the sagittal image, wherein the shape includes the sclera. The shape is converted to a curvature of a contact lens. The curvature is designed such that the contact lens, once manufactured, can be worn over a surface of the eye.
Owner:TRU FORM OPTICS
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com