Medical devices and methods for creating bubbles
a medical device and bubble technology, applied in the field of medical devices configured to generate bubbles, can solve the problems of affecting the flow of blood to tissues and organs to which it is supplied, the lungs are still growing and not yet ready to receive blood, and the risk of clots that bypass the lungs and reach the left heart is heightened, so as to achieve the effect of being seen easily
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
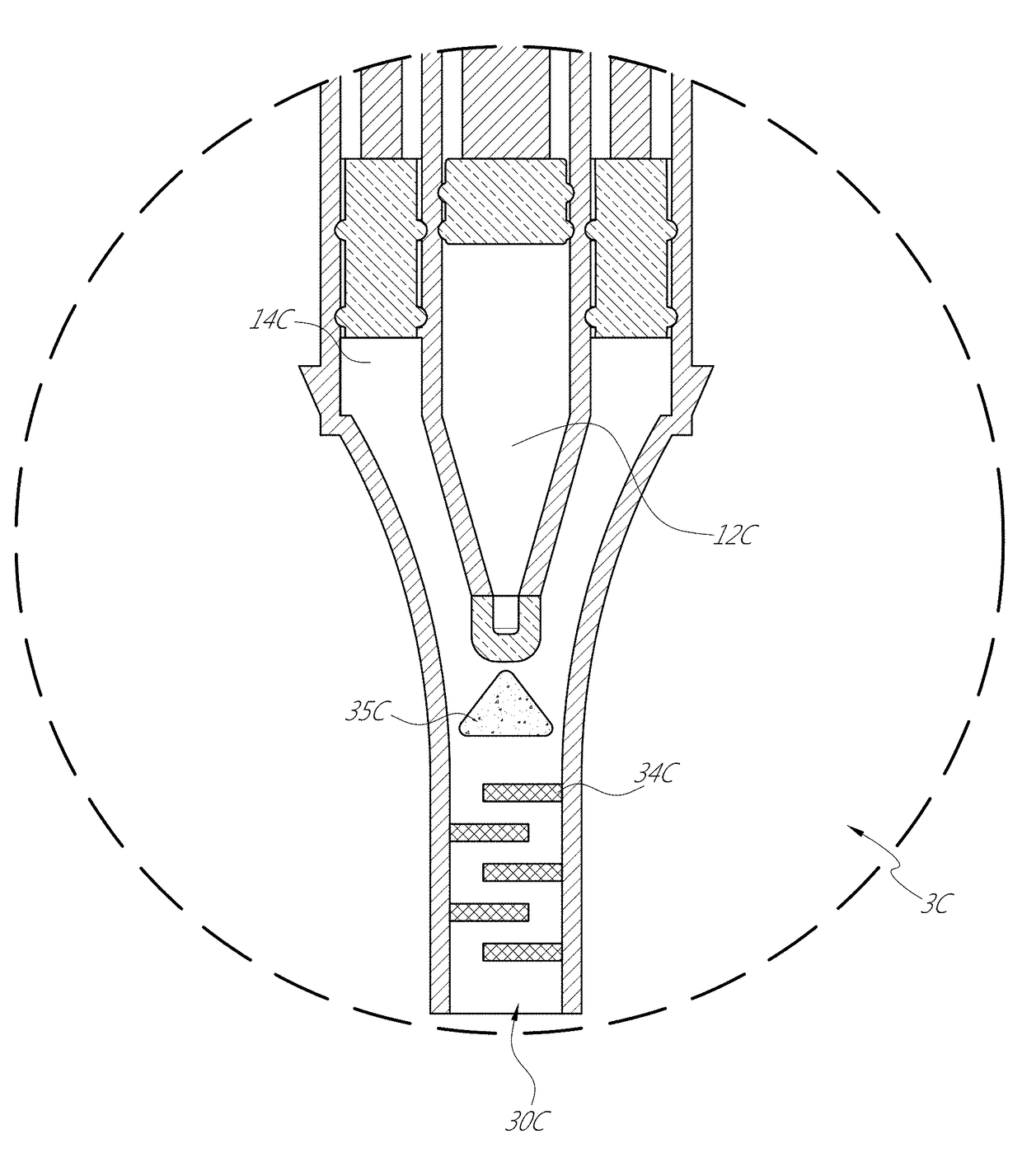
[0042]FIGS. 6, 6A-6D depict a device 1 that generates a bubble mixture that can optionally have a cloudy consistency. As discussed further below, the bubbles can be air bubbles formed in a saline solution. The bubbles can, in some embodiments, be “microbubbles”, small enough to show-up on a standard ultrasound machine in a medical setting, yet large enough to not pass through the lungs.
[0043]The device 1 can be a dedicated device that assists detecting a PFO, ASDs in the heart, or abnormal shunting in the vascular system. However, other applications are also possible, such as for detecting other features or use with other animals. As another example, the device can assist in the placement of a catheter at an appropriate place during pericardiocentesis, such as by injecting a mixture that can be imaged to indicate the location of a needle and / or catheter. Further, although the device 1 can be a medical device (and thus can be sterilized and otherwise made suitable for medical use), t...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com