Kit for detecting free breast cancer cell marker in blood
A breast cancer cell and kit technology, applied in measurement devices, instruments, scientific instruments, etc., can solve the problems that ordinary patients are difficult to accept, tumor cells are not specific, and detection methods are inaccurate.
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
[0039] The preparation of embodiment 1 magnetic beads
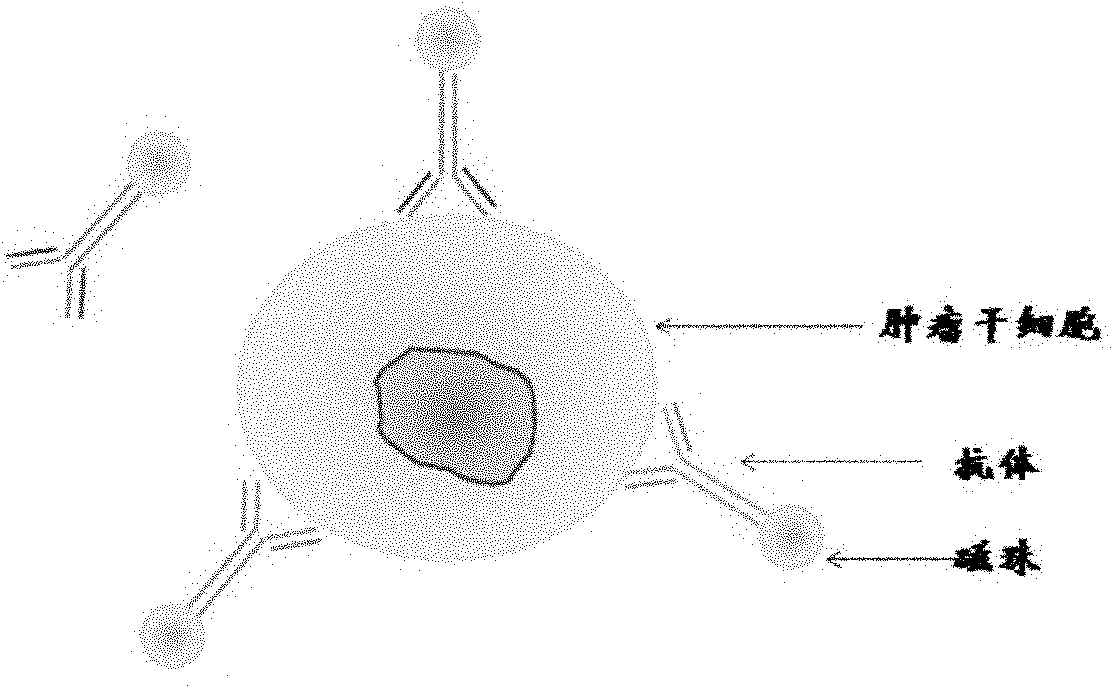
[0040] Preparation of antibody immunomagnetic beads: the antibodies used were anti-BerEP4 monoclonal antibody, anti-cytokeratin monoclonal antibody and anti-HER2 monoclonal antibody. In the present invention, the above three kinds of antibodies are labeled separately and then mixed for use. It is also possible to select one or two antibodies for separate labeling and mixed use.
[0041] Methods: Dynabeads Antibody Coupling Kit produced by Invitrogen was used. The labeling method was carried out in strict accordance with the manufacturer's instructions.
Embodiment 2
[0042] The separation of embodiment 2 breast cancer cells
[0043] 1. Sample collection:
[0044] Collect 5-7.5ml of peripheral blood from breast cancer patients, anticoagulate with EDTA, and use it within 4 hours (or use it within 48 hours after storage at 4 degrees).
[0045] 2. Select magnetic beads:
[0046] 2.1 Handling of magnetic beads:
[0047] Mix the magnetic beads evenly, use a pipette to blow gently, and do not use a vortexer;
[0048] Use PBS buffer solution to wash, and do not touch the microspheres when washing;
[0049] Draw more magnetic beads than the required sample volume and add them to a 1.5ml centrifuge tube;
[0050] Put it on the magnet for 1 minute, discard the supernatant;
[0051] Wash 3 times with 1ml PBS to remove preservatives;
[0052] Remove the supernatant;
[0053] · Aspirate 100ul microspheres containing PBS with the same volume as the original one.
[0054] 2.2 Selection of tumor cells
[0055] Put 5ml of peripheral blood into a 15...
Embodiment 3
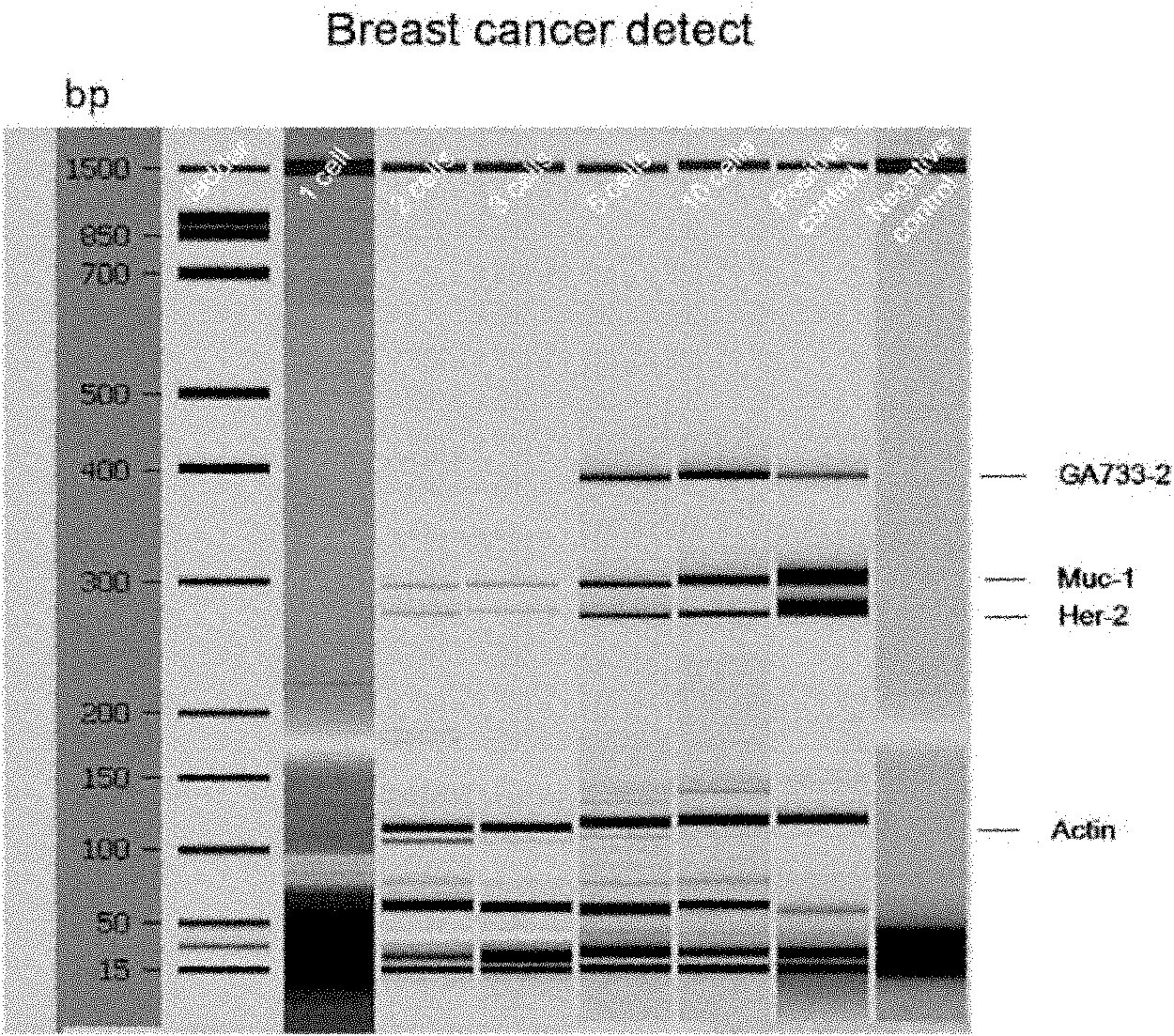
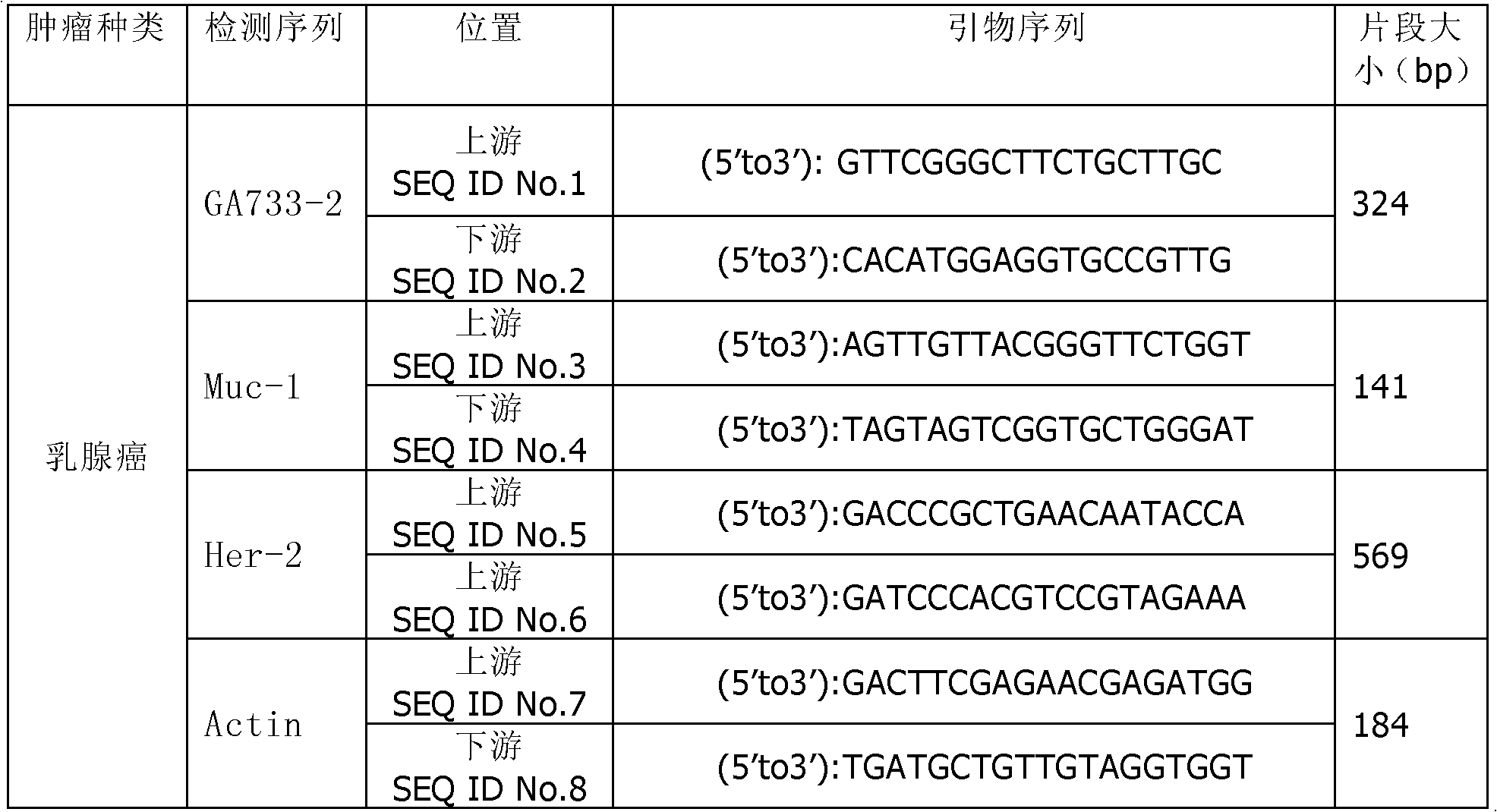
[0074] Example 3 Detection of Breast Cancer Cell Tumor Markers
[0075] 3.1 Kit preparation
[0076] Keep the test tube at room temperature;
[0077] Put the RNase-free water in the kit at room temperature;
[0078] Place the centrifuge tube above the tube containing the supernatant on ice;
[0079] · Prepare magnetic beads.
[0080] 3.2 Preparation of oligonucleotides
[0081] Take an appropriate amount of magnetic beads with oligonucleotide Oligo(dT) (it is recommended not to use a suspension apparatus to mix, but to suspend by hand);
[0082] · Transfer to a 1.5ml tube;
[0083] • Wash twice with lysis / binding buffer.
[0084] 3.3 Binding mRNA to magnetic beads
[0085] Add 20 μl of magnetic beads to each cell lysis sample;
[0086] • Incubate for 10 minutes.
[0087] 3.4 Purification of mRNA
[0088] Wash twice with buffer solution;
[0089] Wash the magnetic beads twice with buffer;
[0090] Wash again with 100 μl Tris-HCl buffer;
[0091] • Suspend the magne...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com