Method and System for Organ Positioning and Stabilization
a technology applied in the field of organ positioning and stabilization, can solve the problems of insufficient blood flow to various areas of the heart, discomfort of angina, and coronary artery disease, and achieve the effects of reducing the risk of stroke, and improving the quality of li
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
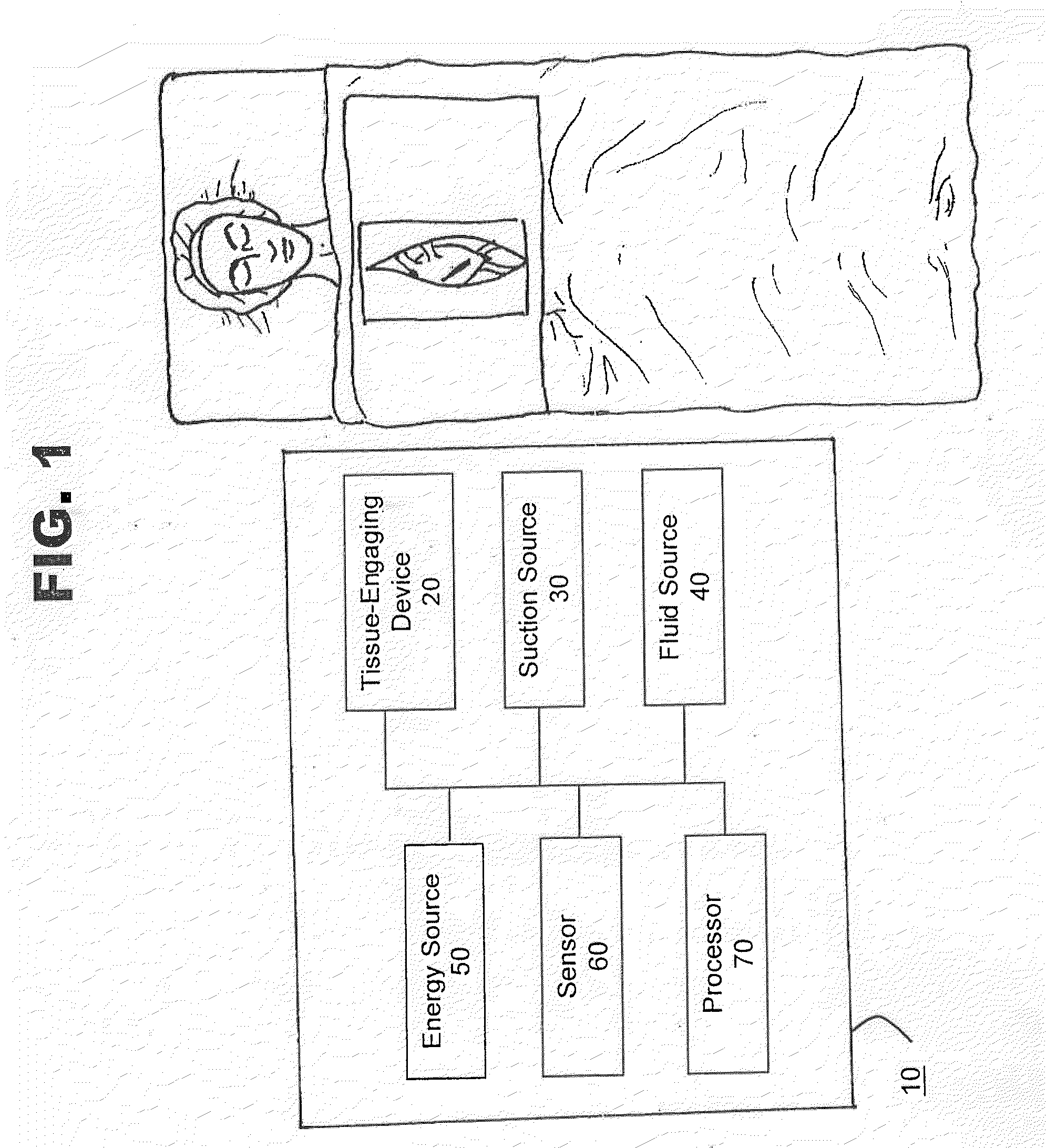
[0085]FIG. 1 shows a schematic view of one embodiment of system 10 for positioning, manipulating, holding, grasping, immobilizing and / or stabilizing tissue in accordance with the present invention. In this embodiment, system 10 is shown to comprise tissue-engaging device 20, a suction source 30, a fluid source 40, an energy source 50, a sensor 60 and a processor 70. System 10 may also include an indifferent electrode, a drug delivery device and / or an illumination device (all not shown in FIG. 1). The indifferent electrode may be placed on the patient's body such as the back, thigh or shoulder or another site other than the suction site. The drug delivery device may be used to deliver drugs to a patient. The illumination device may be used to illuminate a surgical site.
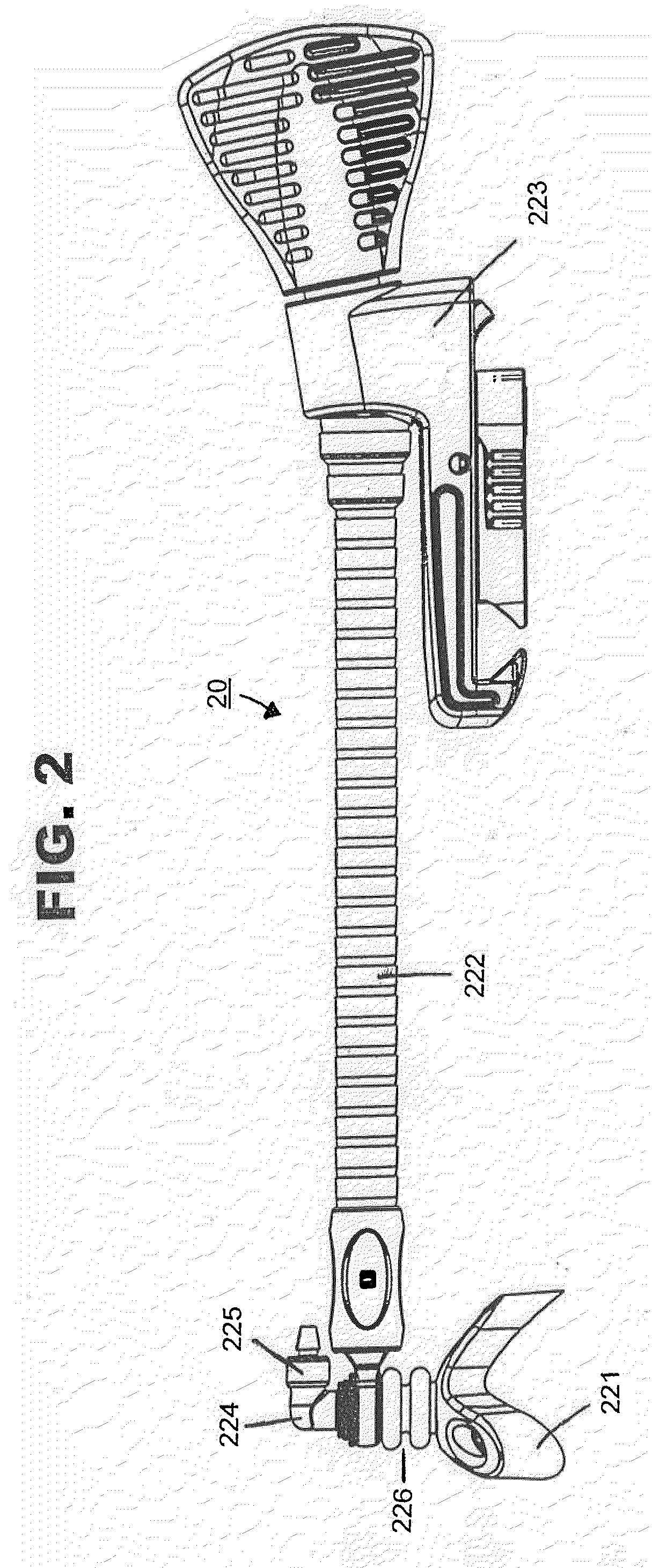
[0086]As shown in FIG. 2, in one embodiment of the present invention, tissue-engaging device 20 may comprise a tissue-engaging head 221, a support apparatus 222 and a clamping mechanism 223 for attaching device 20 to a...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com