Knee joint model capable of demonstrating pressure change in knee joint cavity in KOAPT movement
A knee joint and internal pressure technology, applied in the field of demonstrable medical models, can solve the problems of decreased curative effect, subjective discomfort of the knee joint, short follow-up time, etc., and achieve the effect of accurate pressure changes
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
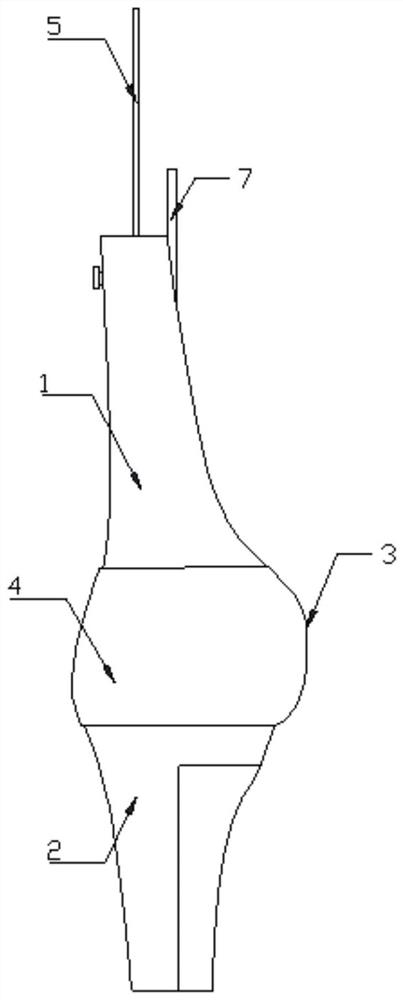
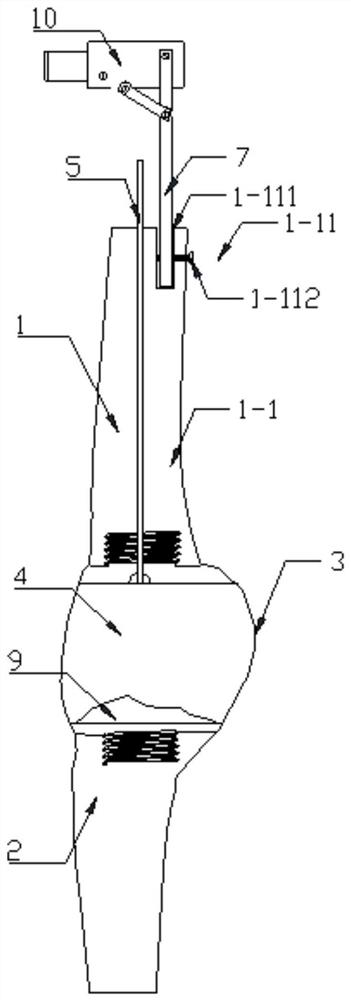
[0047] like Figures 1 to 4 As shown, the knee joint model proposed by the present invention that can demonstrate the pressure change in the knee joint cavity during KOAPT movement includes a femoral structure 1 and a tibial structure 2. The upper part of the femoral structure 1 is provided with a fixing mechanism 1-11 for connecting the swing arm 7; The middle and lower part of the tibial structure 2 is provided with a cavity 2-21 for filling the weight 6; an elastic film 3 for simulating the synovial membrane of the knee joint is sealed and connected between the femoral structure 1 and the tibial structure 2, and the elastic film 3 is wrapped inside to form a sealed integrity. There is a communication tube 5 embedded in the femoral structure 1, and the bottom end of the communication tube 5 penetrates to the bottom end of the femoral structure 1 for injecting artificial synovial fluid into the knee joint cavity 4, and the top of the communication tube 5 penetrates out of the ...
Embodiment 2
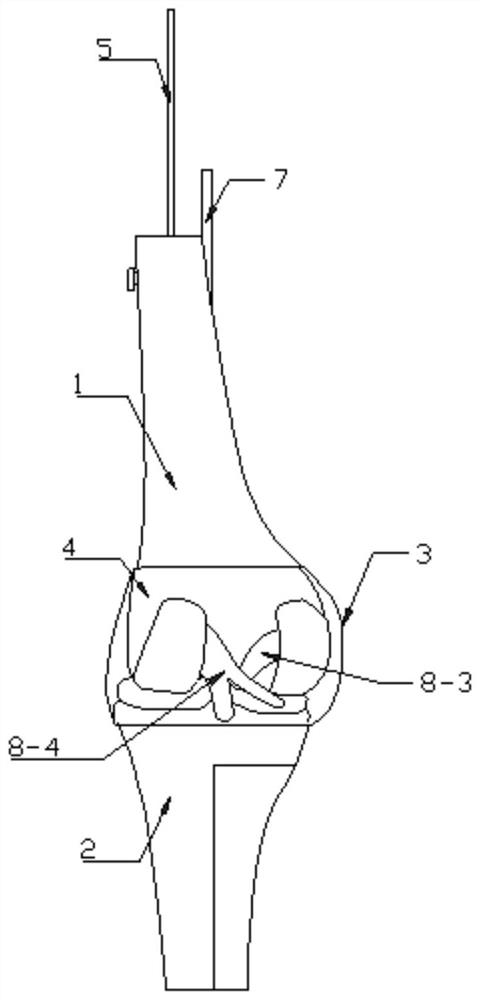
[0074]The main difference between this embodiment and Embodiment 1 is that this embodiment further includes a ligament 8, and the ligament 8 includes a patellar ligament 8-1 fixed between the upper femoral structure 1-1 and the lower tibial structure 2-2. Collateral ligament 8-2, and anterior cruciate ligament 8-3, posterior cruciate ligament 8-4 fixed between lower femoral structure 1-2 and upper tibial structure 2-1; the patellar ligament 8-1 and medial collateral ligament 8 -2 are fixed by the first ligament fixing screw holes 1-13 on the surrounding wall of the upper femoral structure 1-1, the fourth ligament fixing screw holes 2-23 on the surrounding wall of the lower tibial structure 2-2, and screws; Both the anterior cruciate ligament 8-3 and the posterior cruciate ligament 8-4 pass through the second ligament fixing screw holes 1-23 arranged on the surrounding wall of the lower femoral structure 1-2, and the third ligament on the surrounding wall of the upper tibial str...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com