Dilatable balloon implant
A technology of implants and airbags, applied in joint implants, joint implants, spinal implants, etc., can solve problems such as carry away, vertebrae cannot stand upright, and blockage, so as to reduce the risk of sclerosis and achieve good therapeutic effects. Effect
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
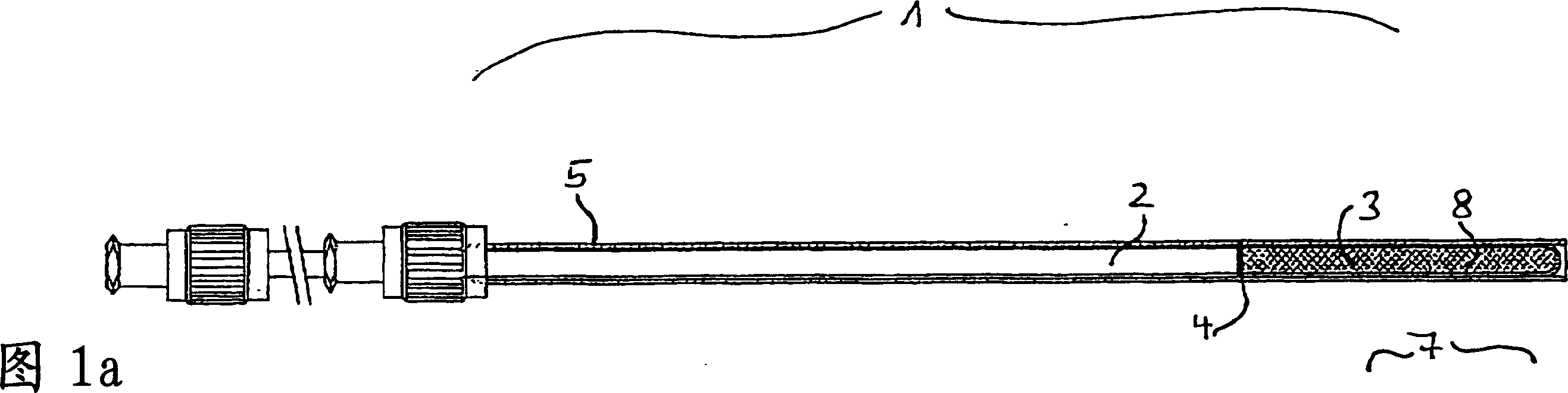
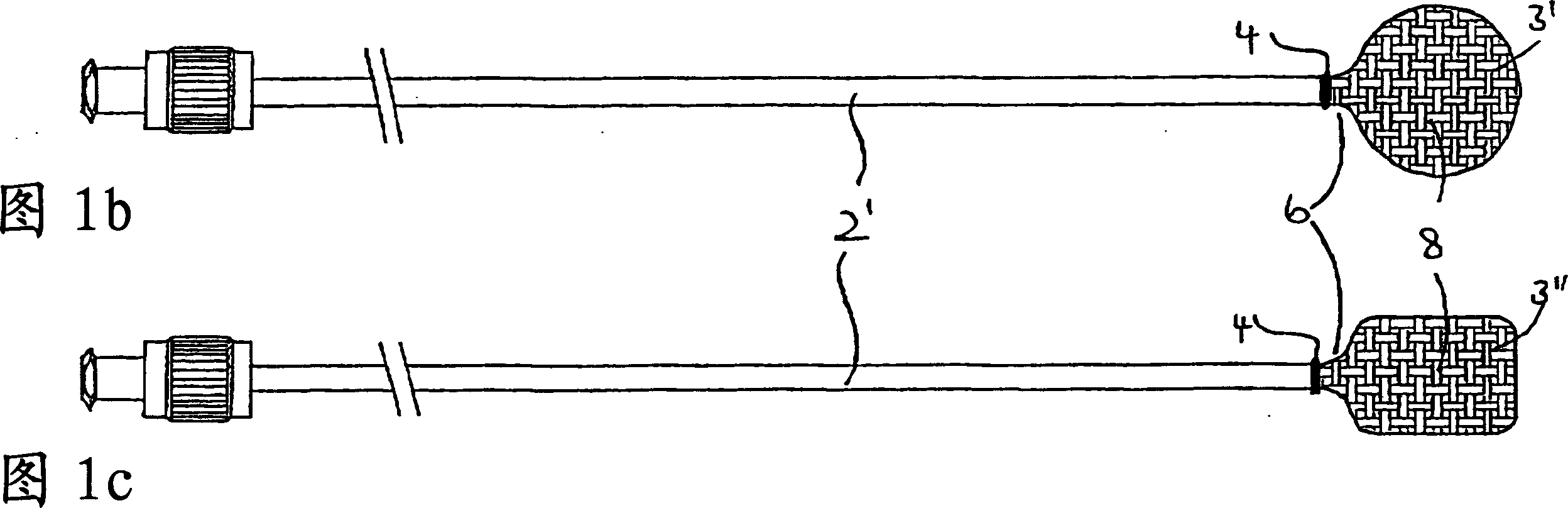
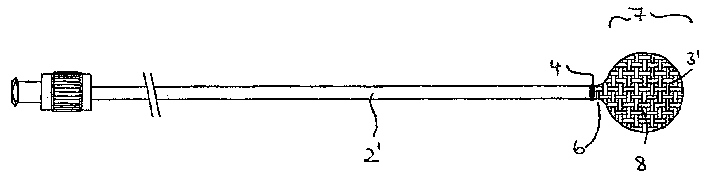
[0039] The vertebroplasty device 1 shown in FIG. 1a includes an introduction sleeve 2 and an inflatable balloon implant 3. At the end of the introduction sleeve 2, the balloon implant 3 is connected to the outer wall of the introduction sleeve 2 in a form-fitting manner by thermoforming. In order to provide additional safety, the connection is reinforced by a clamp ring designed to block the ring 4 and act on the outer periphery of the introduction sleeve 2 to prevent any movement in the direction of the end.
[0040] After using a known technique such as a trocar to establish a percutaneous passage and open the vertebrae, the introduction aid 5, such as a hollow needle of a trocar, is moved up to the vertebral opening, and the balloon implant 3 is deflated. Into the vertebral cavity under the state.
[0041] In this X-ray controlled operation, the introduction sleeve 2 is first moved up to the vertebral opening. Then, the airbag is introduced into the cavity by moving the introdu...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com