Methods and devices for the treatment of ocular diseases in human subjects
a technology for ocular diseases and human subjects, applied in the field of ophthalmic therapies, can solve the problems of significant side effects, difficult to deliver effective doses of drugs to the posterior segment, and difficulty in delivery of drugs to the eye, so as to reduce the severity of one side effect and reduce the number of side effects
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
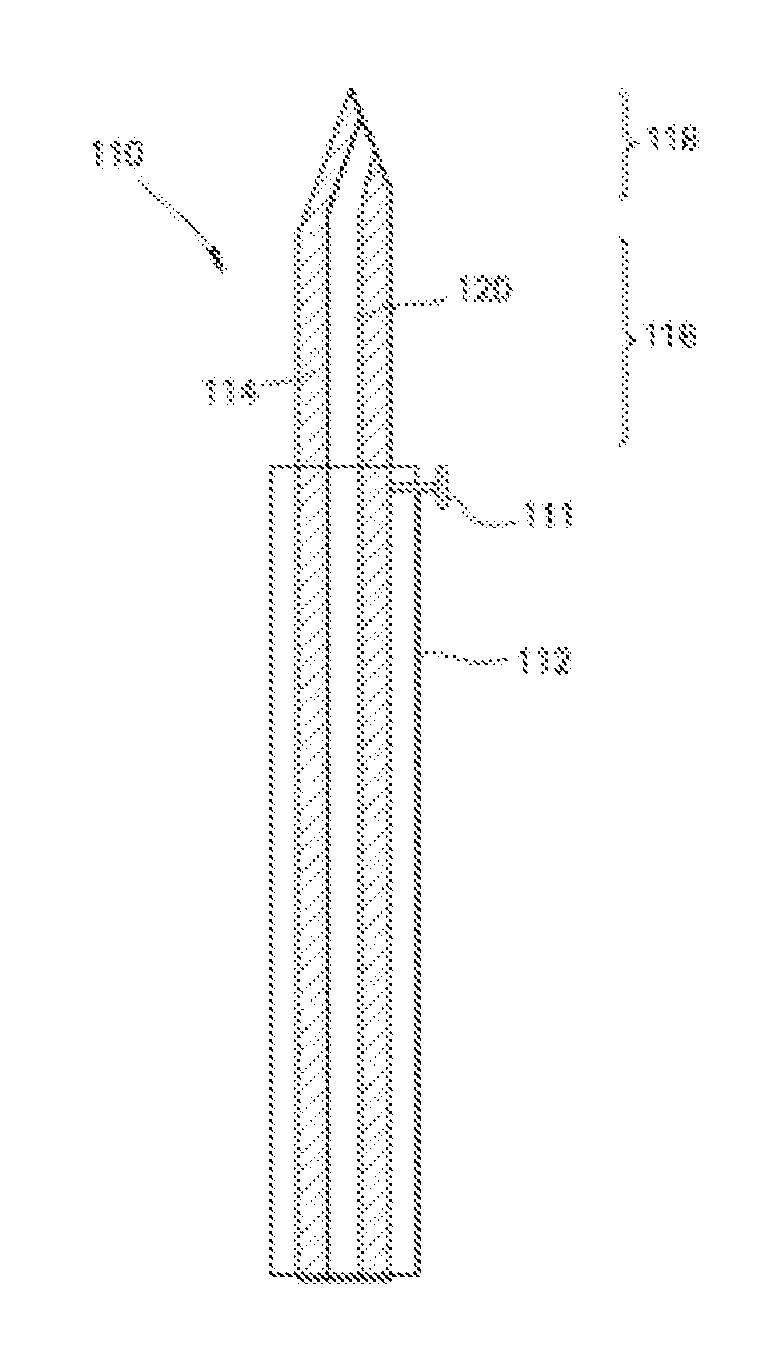
Delivery of a Model Compound to the Suprachoroidal Space Using a Hollow Microneedle
[0224]Red-fluorescent sulforhodamine B was used as a model compound and injected into pig eyes ex vivo using a single hollow microneedle inserted just to the base of the sclera in order to target the suprachoroidal space. A brightfield microscopic image of the saggital cross section of an untreated pig eye, shown in FIGS. 8A and 8B (Scale bar: 500 m), was taken both before and after injection of 35 μL of sulforhodamine B. The normal ocular tissue (FIG. 8A) can be distinguished to identify the sclera, choroid, retina, and vitreous humor. After infusion of the model compound (FIG. 8B), the sulforhodamine solution can be seen just below the sclera and above the choroid in the suprachoroidal space, confirming that the solution was injected and spread within the suprachoroidal space from the initial injection site. Volumes up to 35 μL were able to be injected without leakage, but larger volumes leaked out ...
example 2
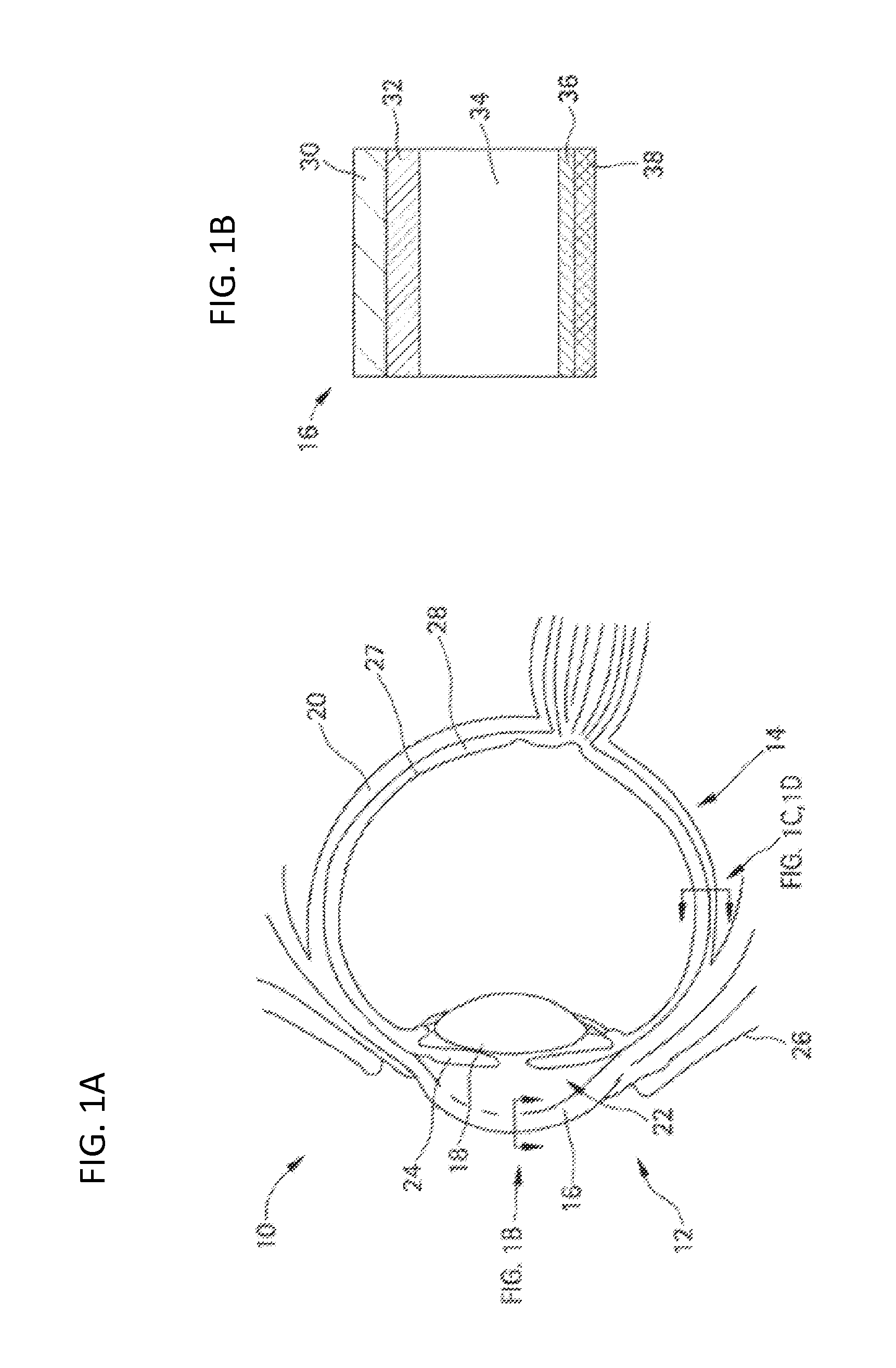
Delivery of Particles to the Suprachoroidal Space Using Hollow Microneedles
[0225]Particles with diameters of 300 nm or 1000 nm were injected into the suprachoroidal space of rabbit, pig and human eyes ex vivo and imaged to evaluate the distribution and localization of the particles just below the sclera. The sclera (1), choroid (2), and retina (3) were identified in a fluoroscopic image of a cryosection of a pig eye with no infusion into the suprachoroidal space (FIG. 9A, Scale bar: 500 μm). Fluoroscopic images of cryosections of a rabbit eye after injection of 500 nm particles were taken in the axial plane and the images were collaged to form a panoramic view (FIG. 9B, Scale bar: 500 μm). The spread of the fluorescent particles (which appear as the bright white regions in the images) was observed along the equator of the eye in a thin sheath just below the sclera. A volume of 15 μL was injected and, in this particular cross-section taken in the plane of the insertion site, the inj...
example 3
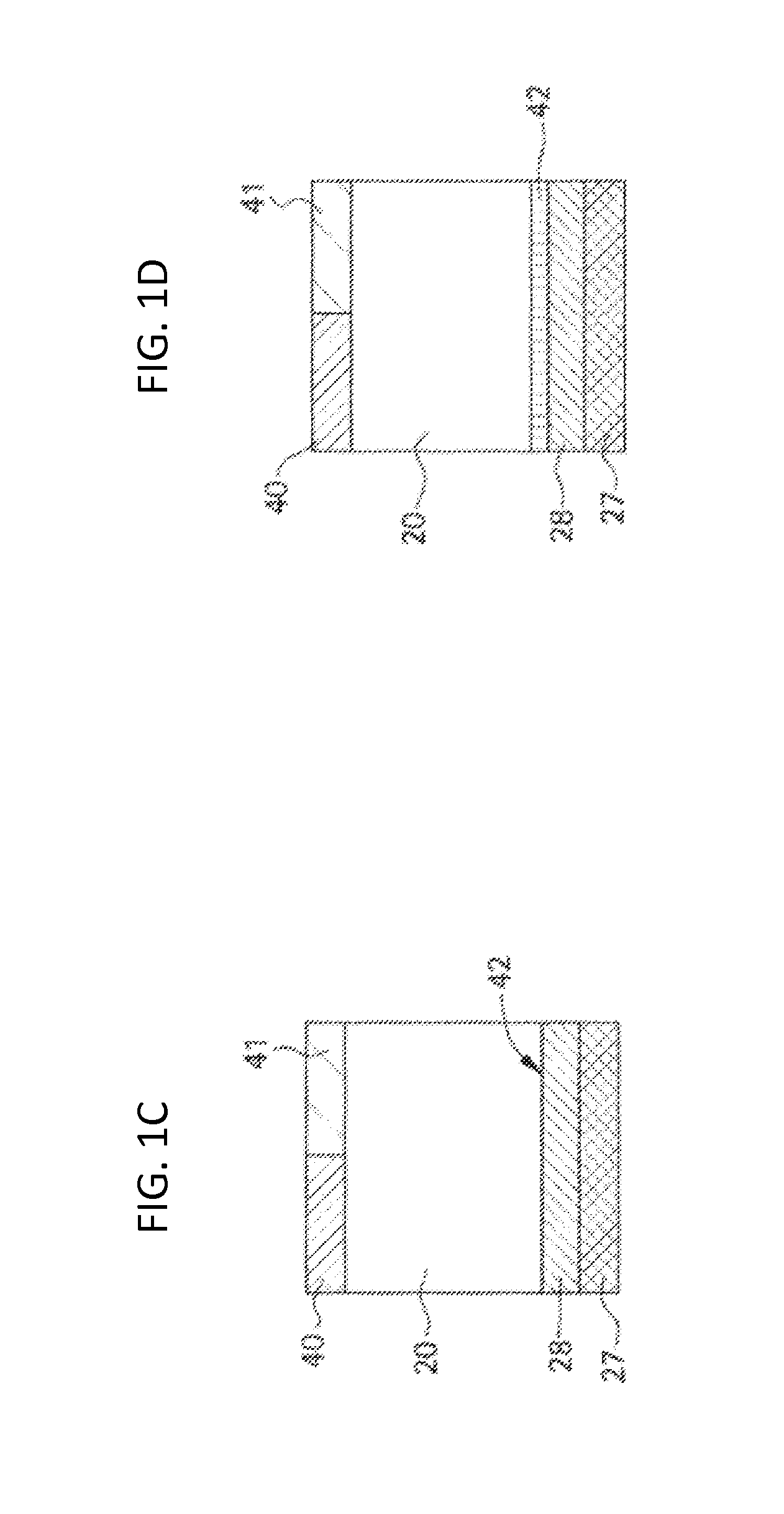
Effect of Operating Parameters on Particle Delivery to the Suprachoroidal Space
[0229]Particles of 20, 100, 500, and 1000 nm diameter were injected into pig eyes ex vivo using a range of different microneedle lengths and infusion pressures to determine the success rate of suprachoroidal delivery. An attempted injection was considered to be either fully successful (complete injection of the 25 L particle suspension into the suprachoroidal space) or fully unsuccessful (an inability to inject at all). No partial injections were observed. The effect of infusion pressure and microneedle length on the success rate of suprachoroidal delivery of particles are shown for 20 nm (FIG. 11A), 100 nm (FIG. 11B), 500 nm (FIG. 11C), and 1000 nm (FIG. 11D) particles into pig eyes.
[0230]The success rate increased with greater infusion pressure and with greater microneedle length (ANOVA, p<0.05). For the 20 nm particles (FIG. 11A). 100% successful injections were achieved using a pressure of 250 kPa at ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com