Devices for intraocular drug delivery
a technology eye, which is applied in the field of devices and methods for intraocular drug delivery, can solve the problems of limited ocular absorption, high risk of systemic toxicity for patients, and many challenges for patients to receive drugs to the eye, so as to reduce reduce the length of drug delivery implants, and increase the risk of eye damage. the effect of retina tissue and lens capsule damag
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
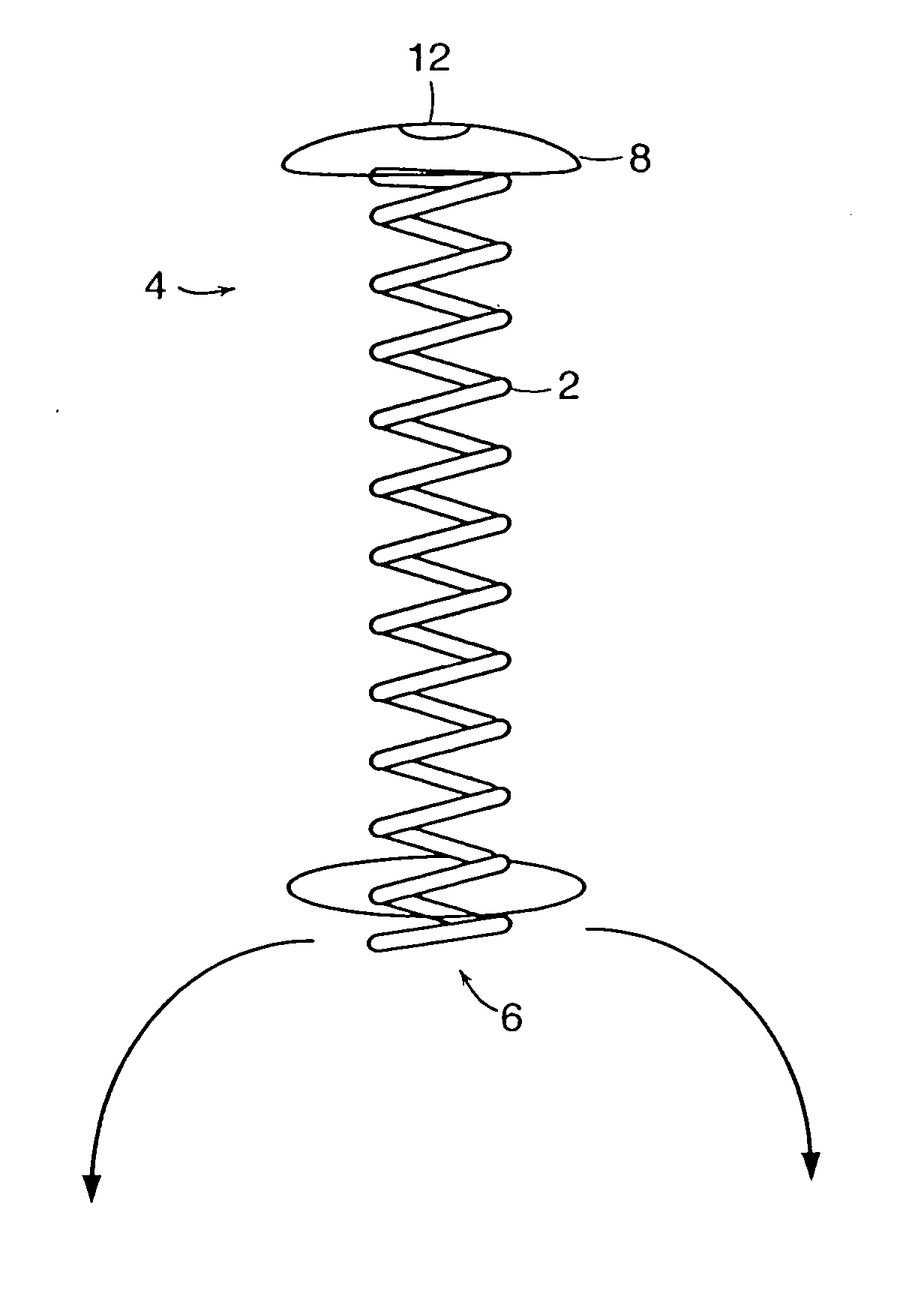
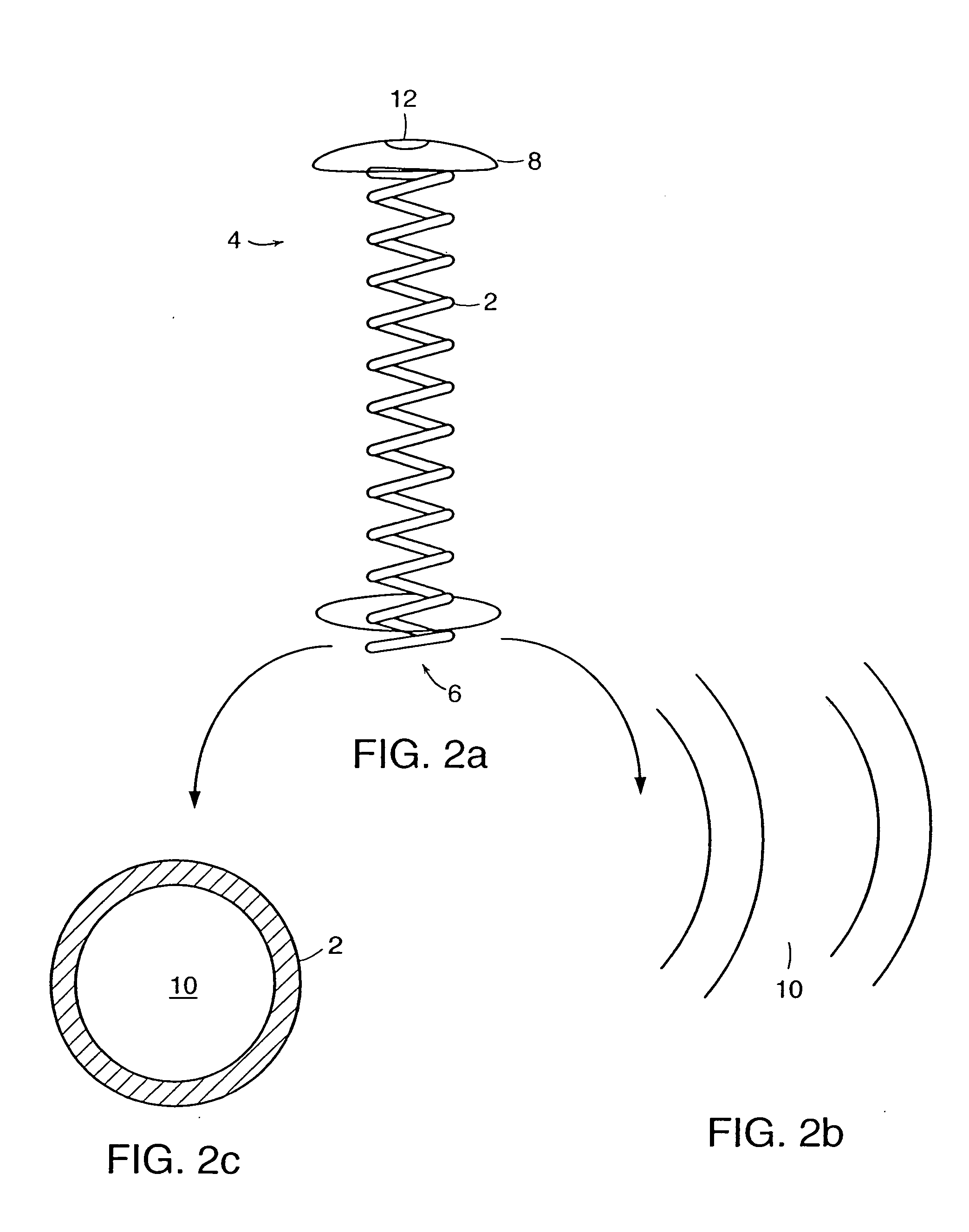
[0033] As discussed above, preferred delivery devices of the invention have a non-linear (arcuate) shape during residence within a patient's eye. Preferred designs have multiple turns or angles. For example, preferred designs the device has at least two, three, four, five, six, seven, right, nine or ten separate deviations from a linear path. A coil design is particularly preferred, although other multiple-angle configurations are also suitable such as a substantially Z-shape and the like.
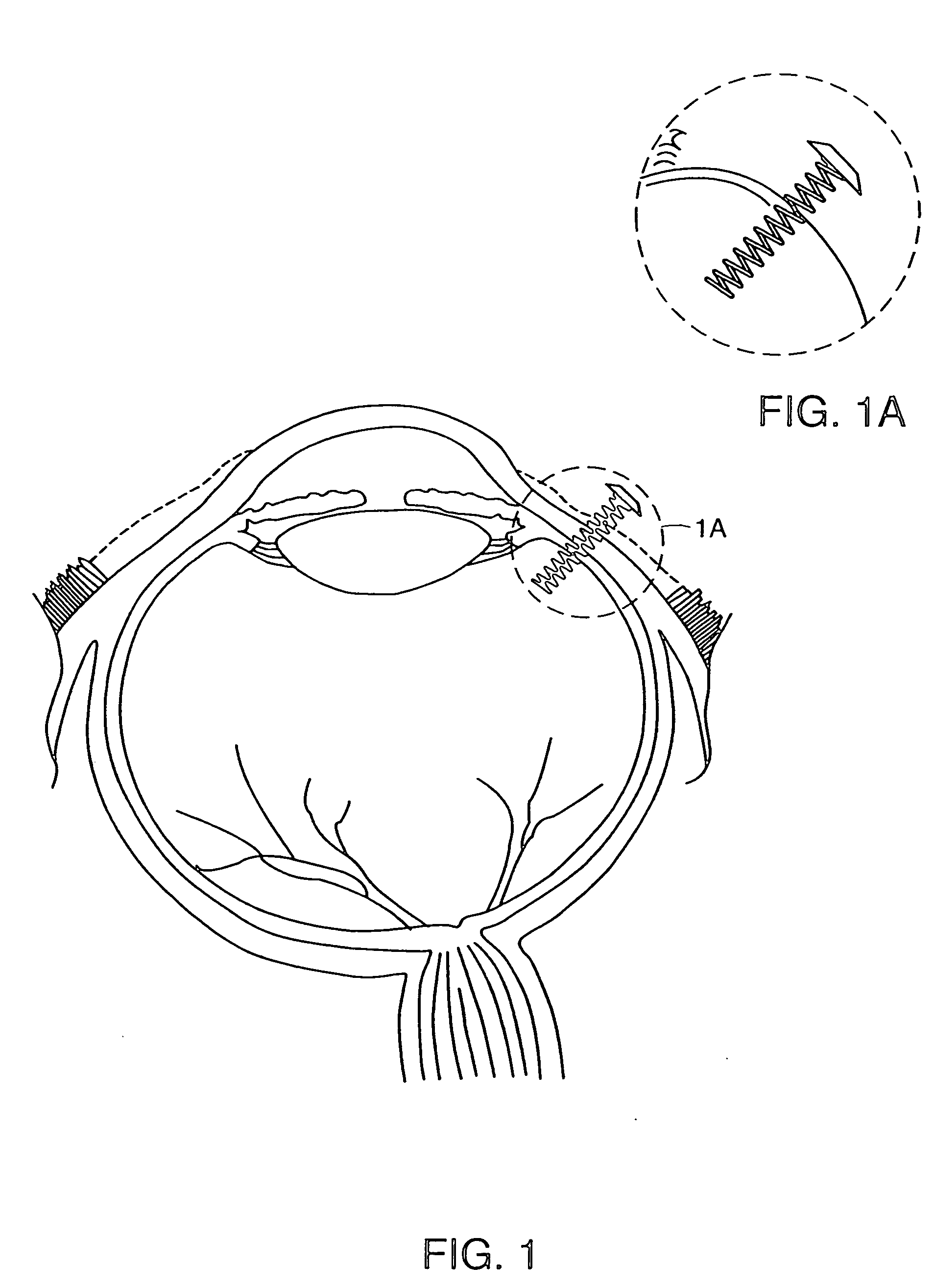
[0034] Referring now to the various figures of the drawing, wherein like reference characters refer to like parts, there is shown various views of a delivery device 1, in accordance with the invention.
[0035] As shown in FIGS. 1-5c, the delivery device 1 includes a non-linear shaped body member 2 having a proximal end 4, a distal end 6. In one preferred embodiment, the body member 2 has a coil shape, as shown in FIGS. 1-5c. However, the shape of the body member 2 is not limited to a coil shape and...
PUM
| Property | Measurement | Unit |
|---|---|---|
| length | aaaaa | aaaaa |
| length | aaaaa | aaaaa |
| distance | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com