System and Method for Joint Resurface Repair
a joint and surface repair technology, applied in the field of devices and methods for the repair of defects, can solve the problems of deterioration of joint function, less durability, and non-typical replacement of cells
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
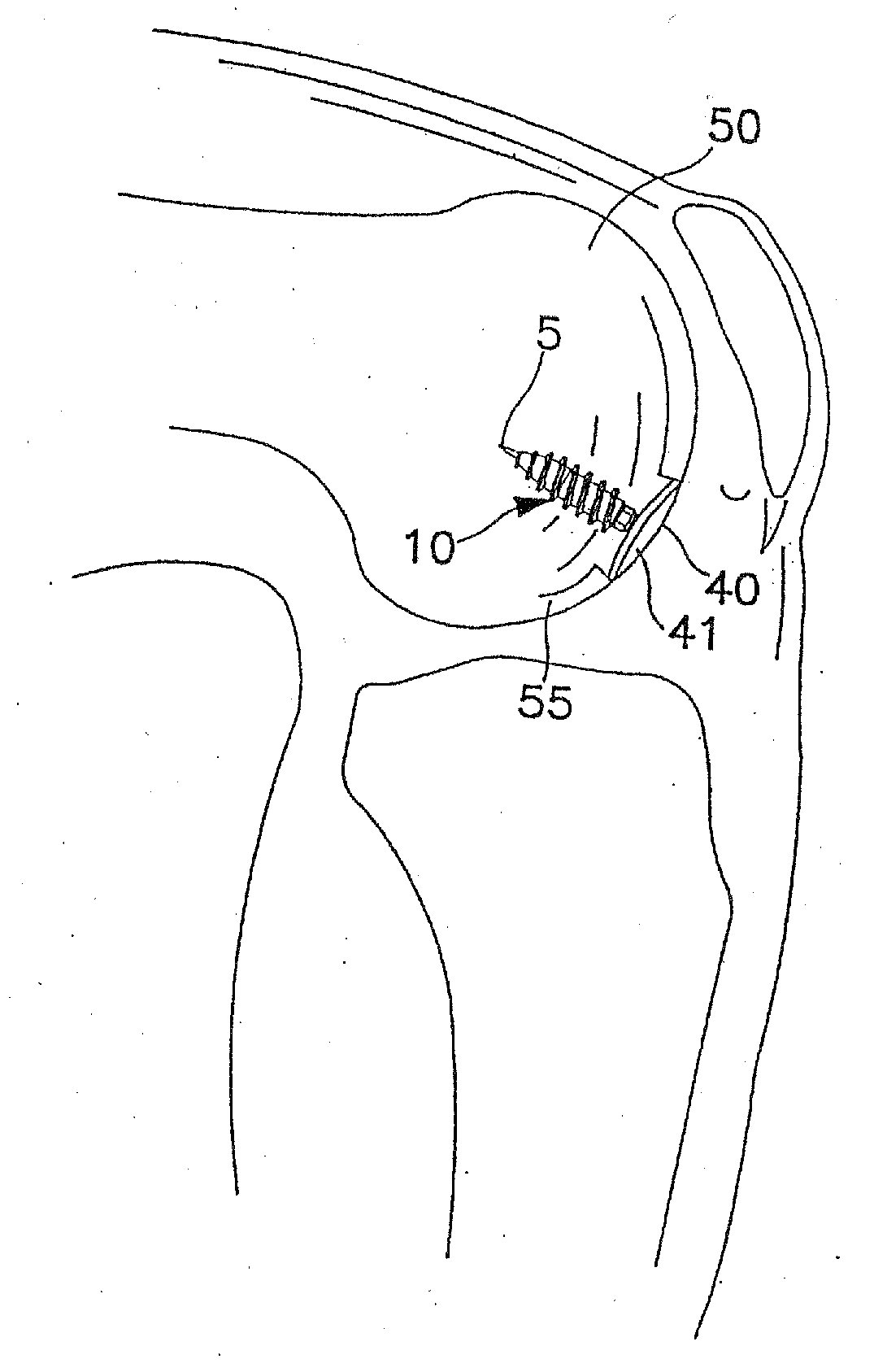
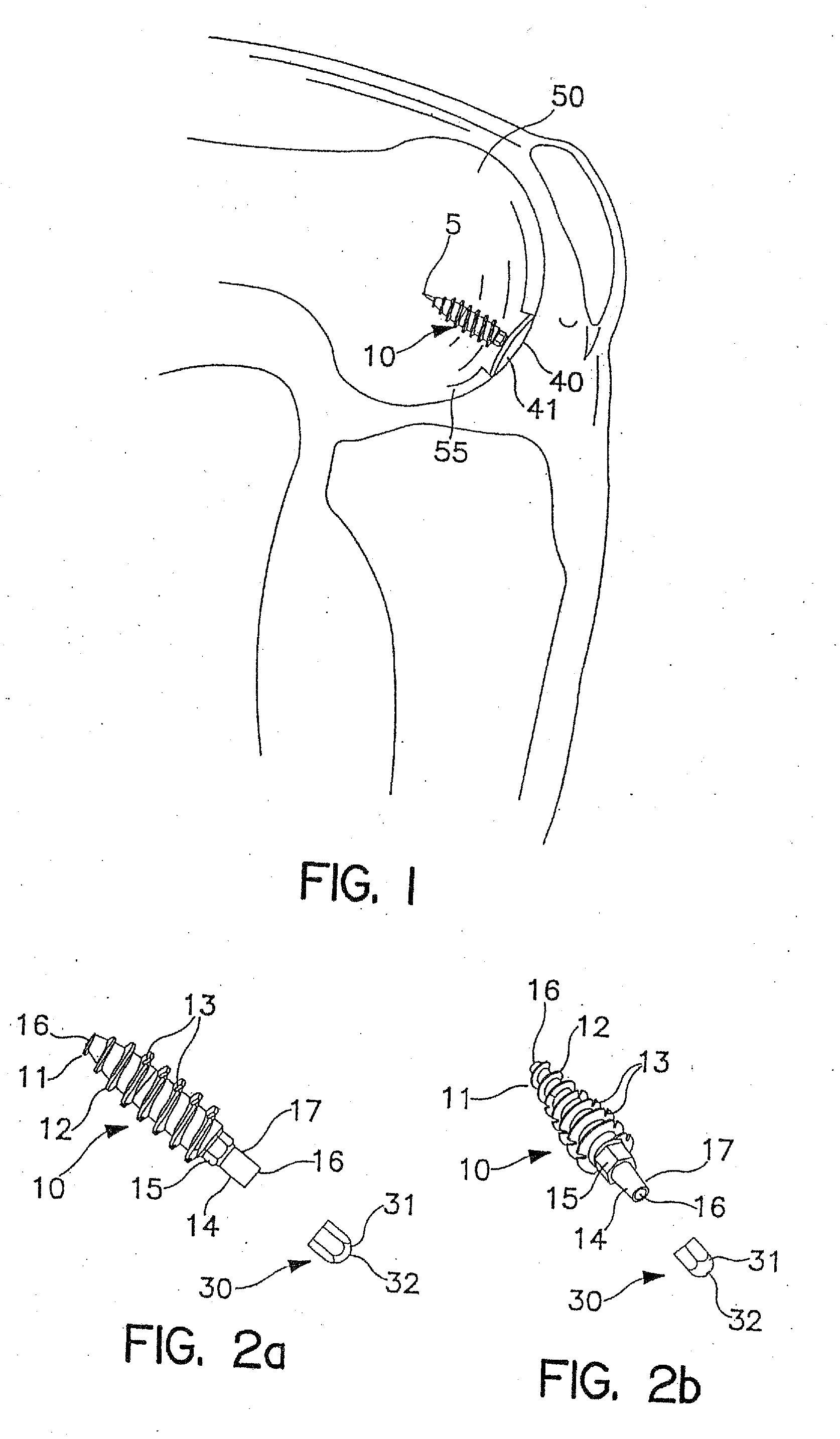
[0154]As an overview, FIG. 1 shows a surgically implanted articular joint surface repair system consistent with the present invention. As shown, the assembled fixation device includes fixation screw 10, implant 40, and anchoring pin 5, implanted in the defect in the medial femoral chondral surface 55 of knee 50. Implant 40 is configured so that bearing or bottom surface 41 of the implant reproduces the anatomic contours of the surrounding articular surface of the knee 50.
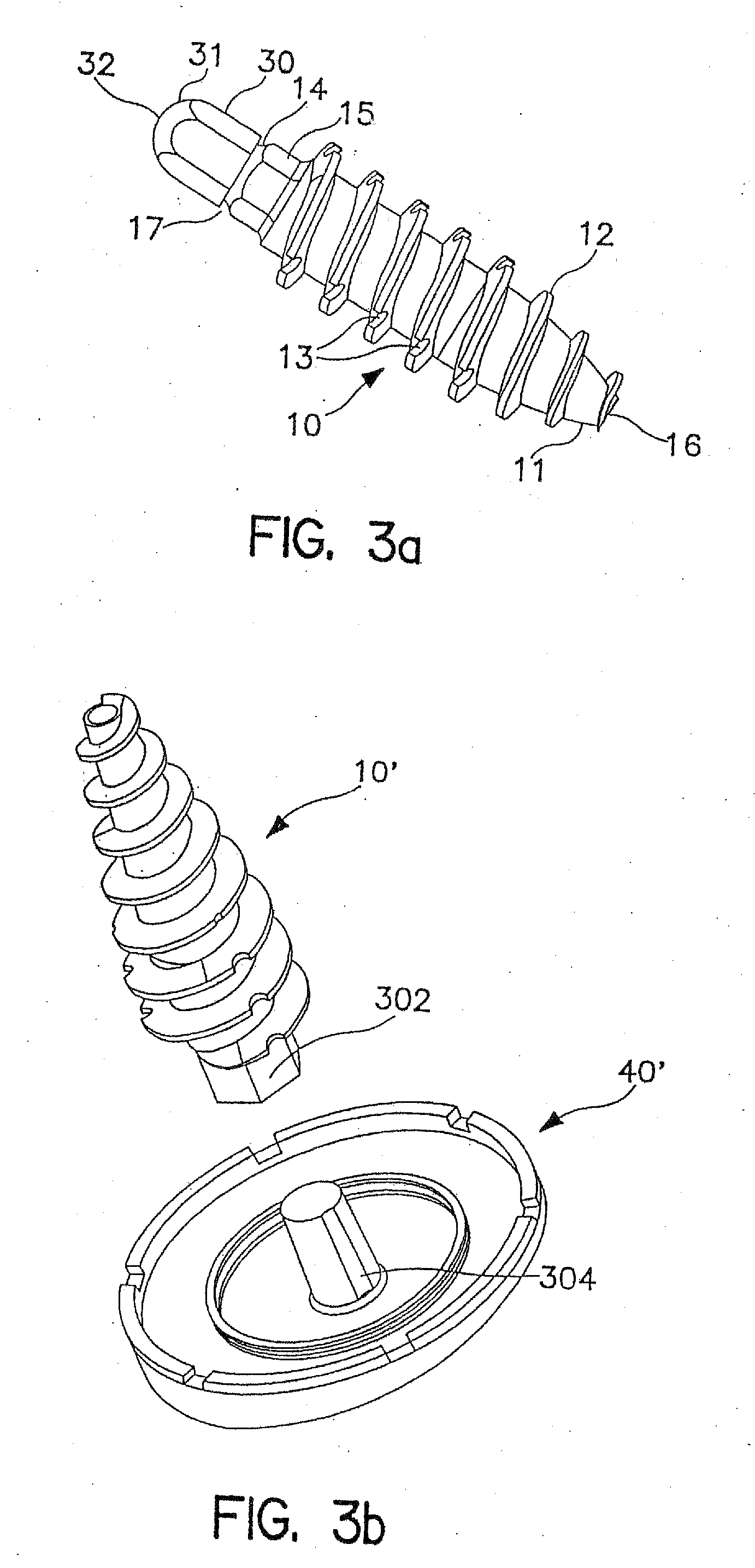
[0155]As illustrated in FIGS. 2a, 2b and 3a, fixation screw 10 comprises threads 12 running the length of the screw from tapered distal tip 11 to hex-shaped drive 15. In the embodiment shown, the screw includes a tapered distal end 11, and aggressive distal threads 12, so that, as screw 10 is driven into the subchondral bone 100 (as shown in FIG. 7a) the screw dilates open and radially compress the subchondral bone, increasing its local density and thereby increasing the fixation strength of the screw. The screw 10 ...
PUM
| Property | Measurement | Unit |
|---|---|---|
| length | aaaaa | aaaaa |
| circular shape | aaaaa | aaaaa |
| width | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com