Transvalvular intraannular band and chordae cutting for ischemic and dilated cardiomyopathy
a transvalvular band and chordae technology, applied in the field of transvalvular band, can solve the problems of loss of ventricular function and geometry, insufficient durability of the valve, and inability to properly function one or more of the valves
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
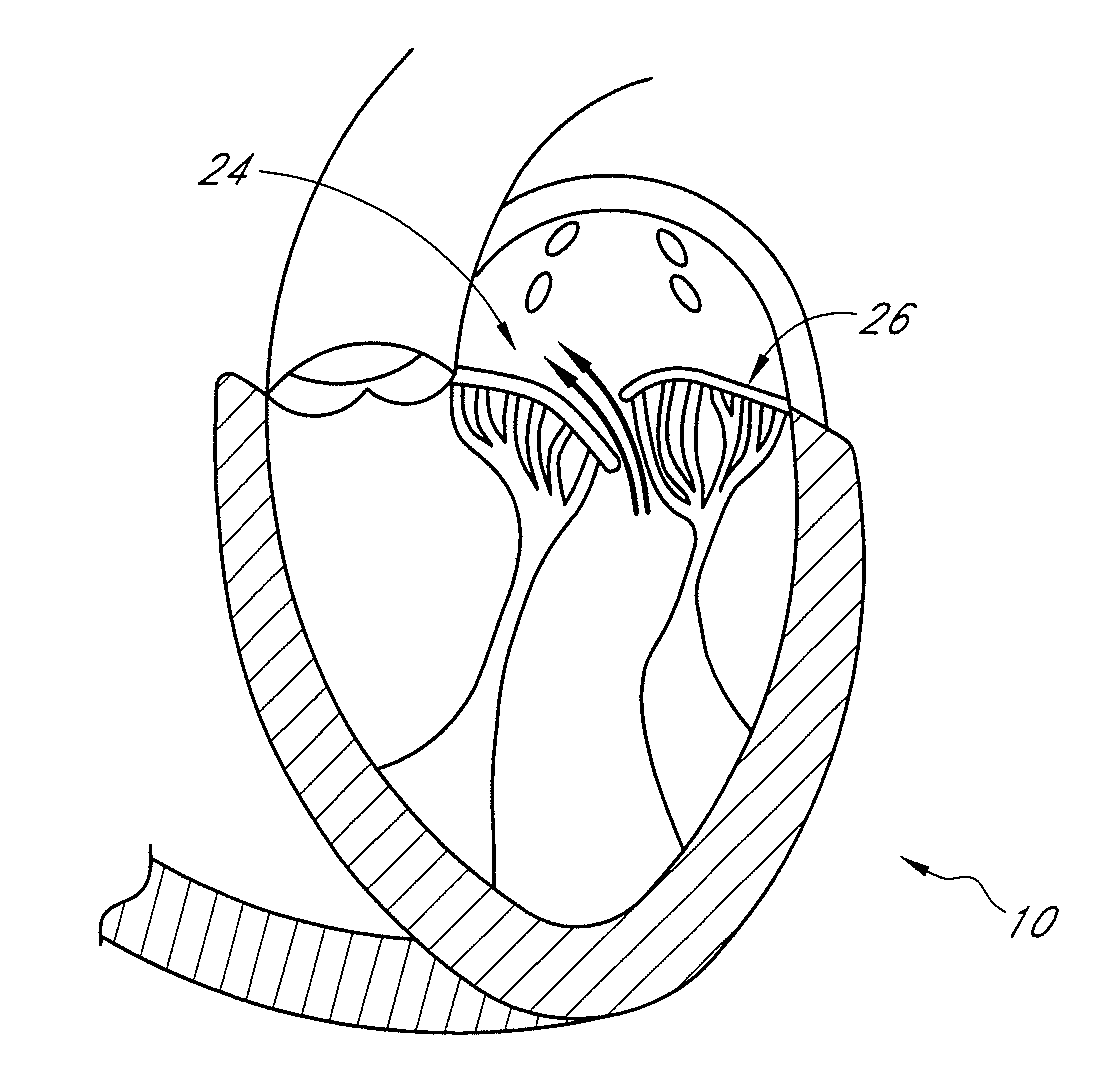
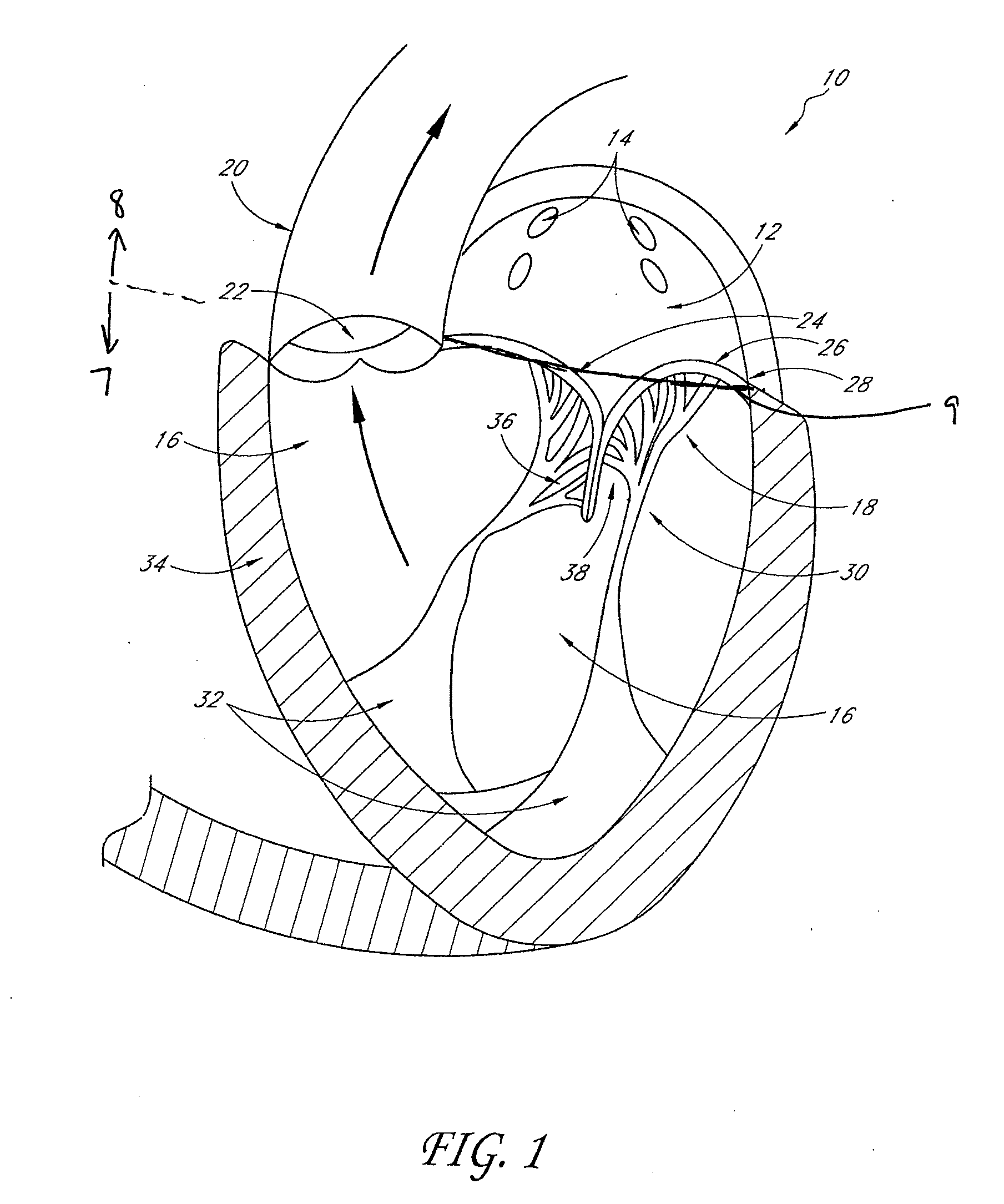
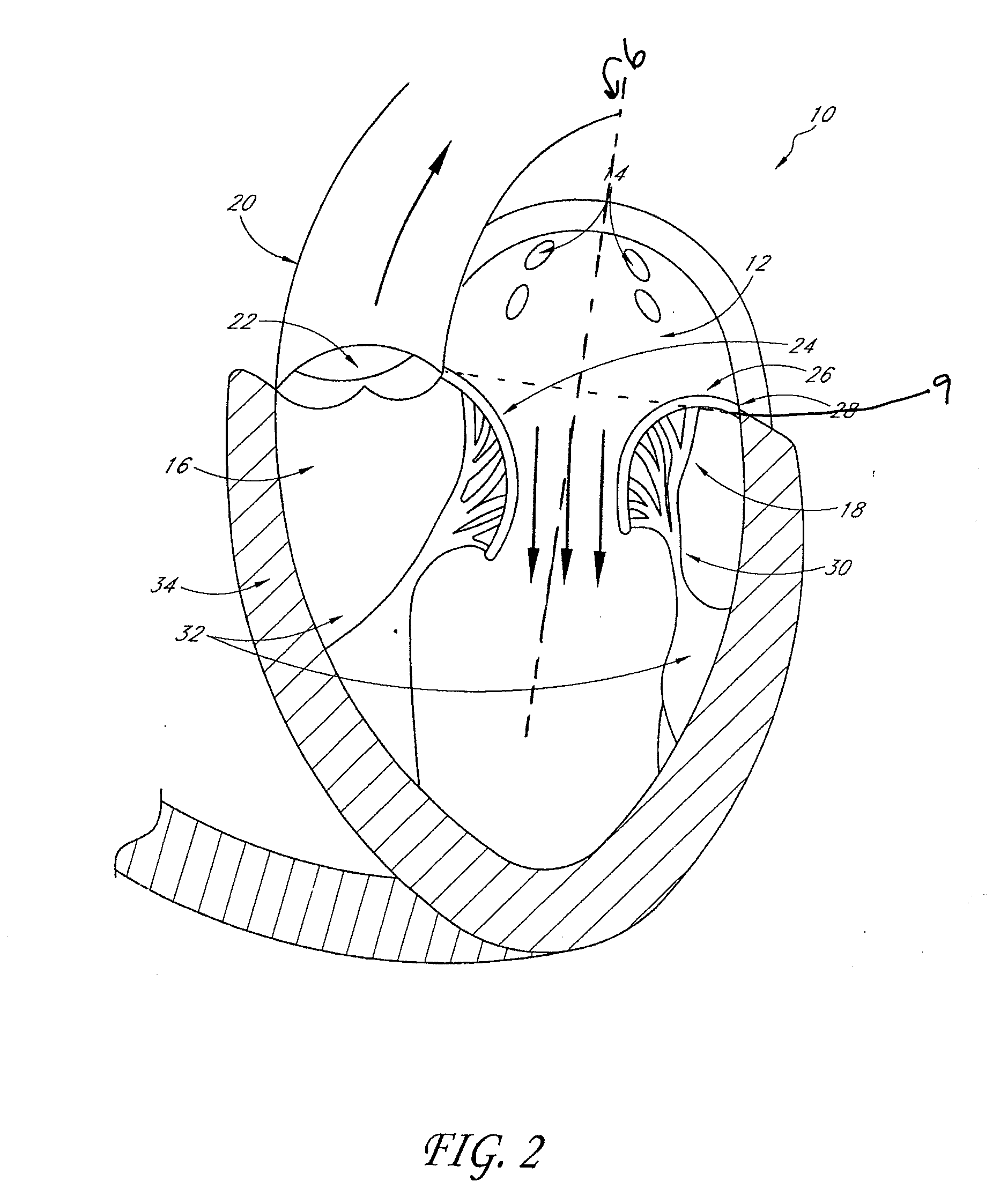
[0106]FIG. 1 illustrates a cross-sectional view of the heart 10 with a normal mitral valve 18 in systole. As illustrated, the heart 10 comprises the left atrium 12 which receives oxygenated blood from the pulmonary veins 14 and the left ventricle 16 which receives blood from the left atrium 12. The mitral valve 18 is located between the left atrium 12 and left ventricle 16 and functions to regulate the flow of blood from the left atrium 12 to the left ventricle 16. During ventricular diastole, the mitral valve 18 is open which allows blood to fill the left ventricle 16. During ventricular systole, the left ventricle 16 contracts, which results in an increase in pressure inside the left ventricle 16. The mitral valve 18 closes when the pressure inside the left ventricle 16 increases above the pressure within the left atrium 12. The pressure within the left ventricle 16 continues increasing until the pressure within the left ventricle 16 exceeds the pressure within the aorta 20, which...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com