Method for a fully automated monoclonal antibody-based extended differential
a monoclonal antibody and extended differential technology, applied in the field of fully automated monoclonal antibody-based extended differential, can solve the problems of inability to readily differentiate multiple subsets of cells in a single sample, difficulty in the performance of accurate 5-part white blood cell performance, and common shortcomings of current analytic systems
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
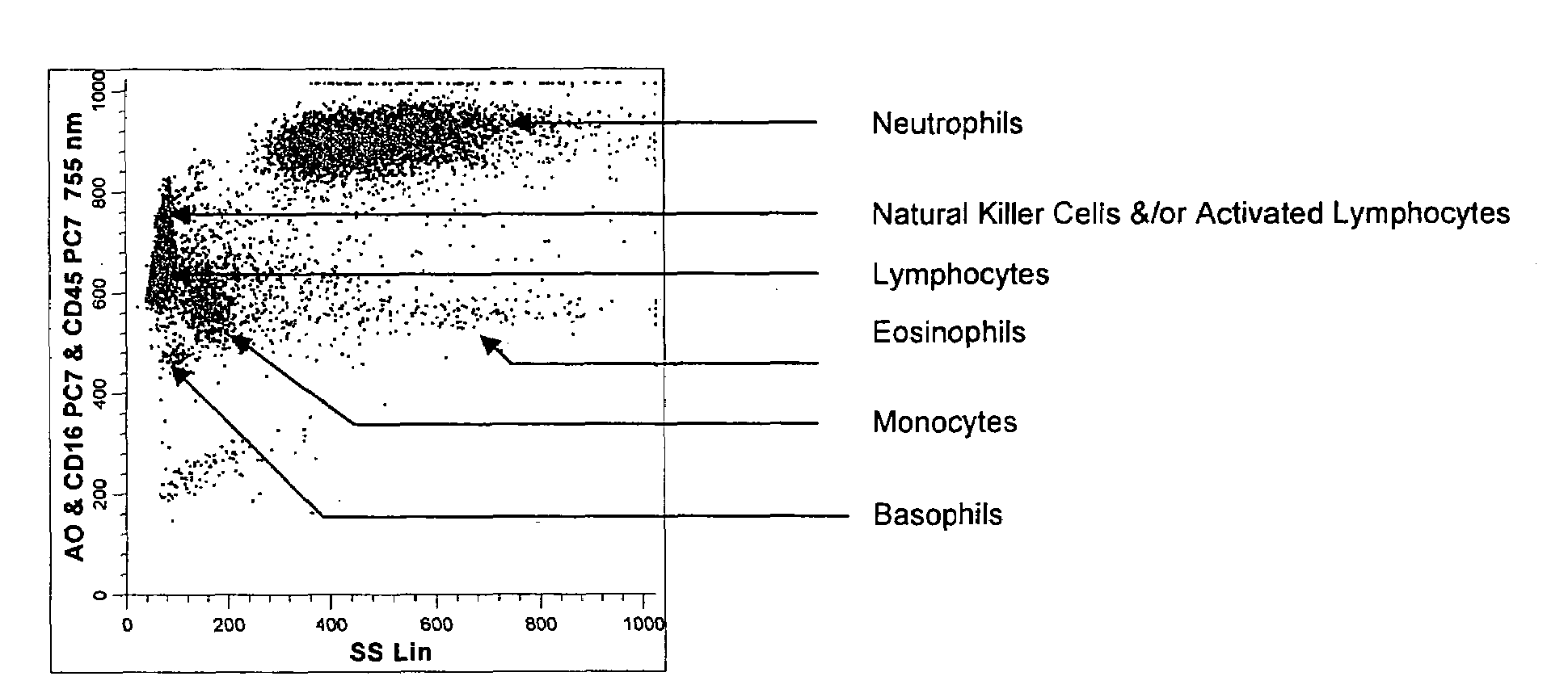
[0186]A single reaction mixture was prepared by reacting 100 μL of normal human peripheral blood with about 1 μg of anti-CD45-PC7, i.e., a first antibody labeled with a first fluorochrome having a first emission spectrum, the first antibody binding to an antigenic determinant that is differentially expressed on populations of leukocytes and non-leukocytes and about 1 μg of anti-CD16-PC7, i.e., an additional antibody labeled with same fluorochrome having the same emission spectrum. The anti-CD16 antibody binds to an antigenic determinant that is differentially expressed on populations of mature and immature granulocytes or myeloid cells. This reaction mixture is mixed briefly and incubated at room temperature for approximately 10 minutes. The reaction was performed in the absence of a fluorescent dye.
[0187]This reaction mixture is then reacted for about 8 seconds with the lytic system (about 600 μL of Immunoprep™ reagent A; see U.S. Pat. No. 5,030,554) that differentially lyses the n...
example 2
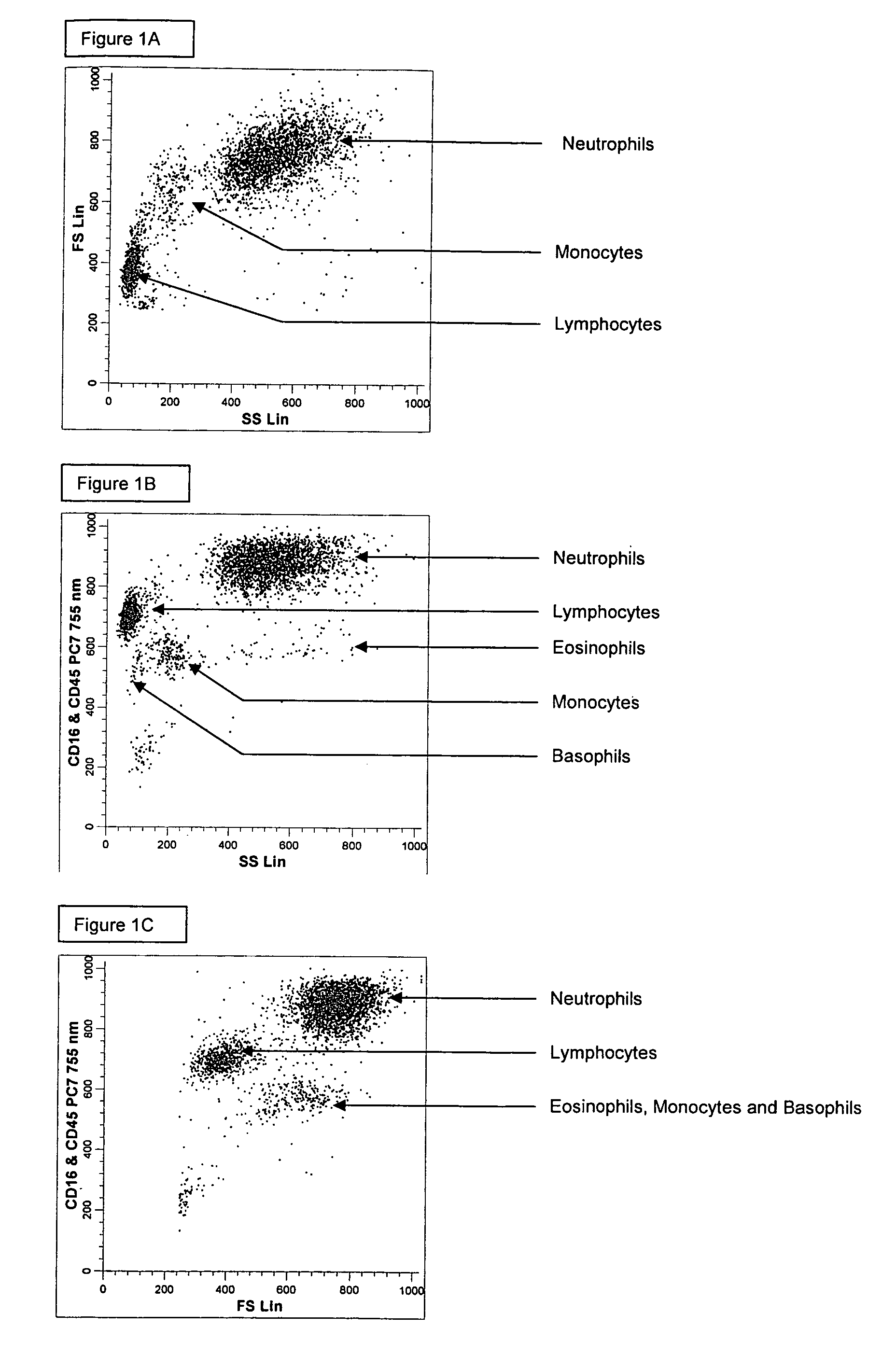
[0192]A single reaction mixture was prepared by reacting 100 μL of normal human peripheral blood with about 1 μg of anti-CD45-PE, i.e., a first antibody labeled with a first fluorochrome having a first emission spectrum, the first antibody binding to an antigenic determinant that is differentially expressed on populations of leukocytes and non-leukocytes and about 1 μg of anti-CD16-PC7, i.e., an additional antibody labeled with a second fluorochrome that has an emission spectrum distinguishable from the emission spectrum of the fluorochrome PE. The anti-CD16 antibody binds to an antigenic determinant that is differentially expressed on populations of mature and immature granulocytes or myeloid cells. This reaction mixture is mixed briefly and incubated at room temperature for approximately 10 minutes. The reaction was performed in the absence of a fluorescent dye.
[0193]This reaction mixture is then reacted for about 8 seconds with the lytic system (about 600 μL of Immunoprep™ reagen...
example 3
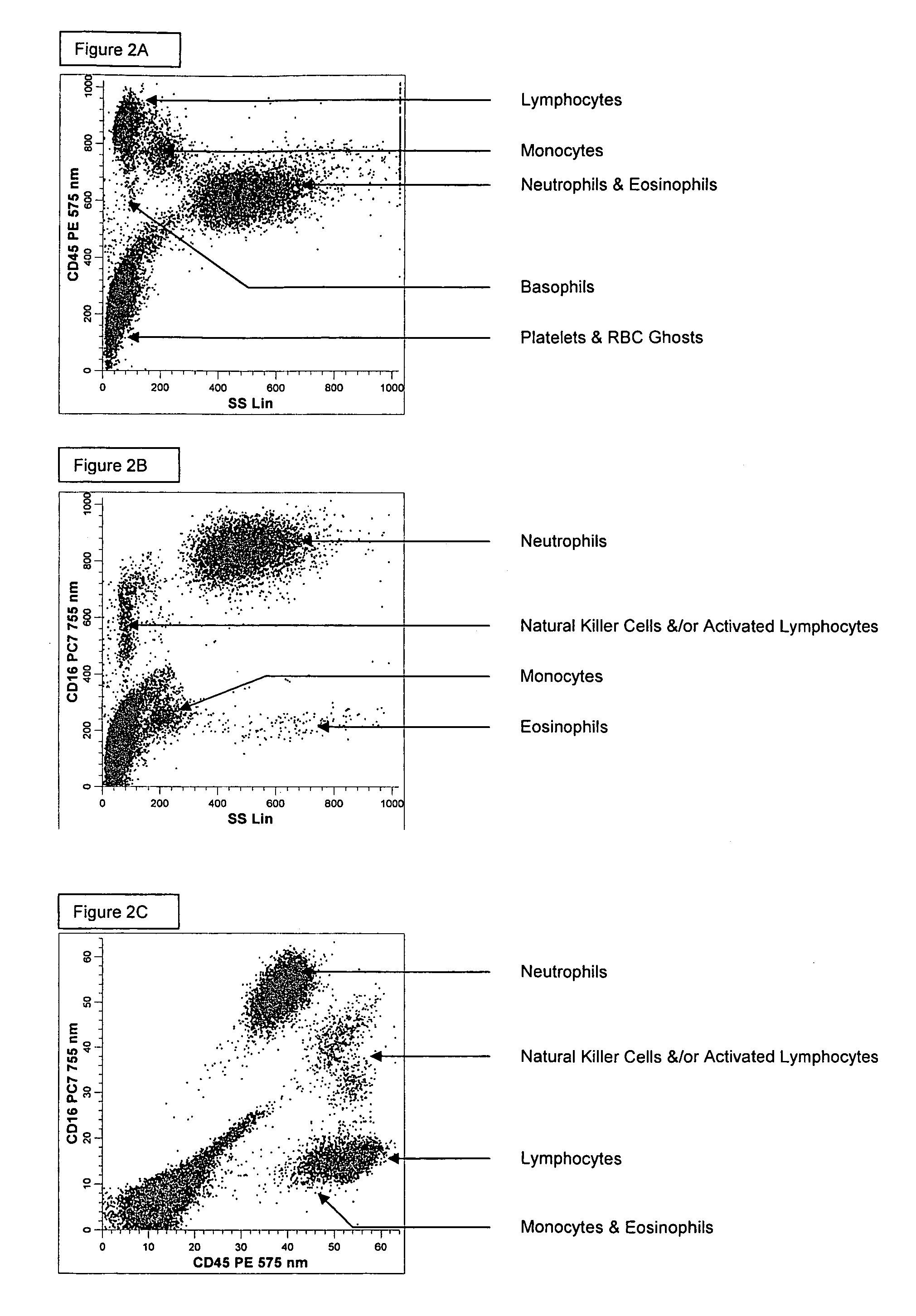
[0196]A single reaction mixture was prepared by reacting 200 μL of normal human peripheral blood with about 1 μg of anti-CD45-PC5, i.e., a first antibody labeled with a first fluorochrome having a first emission spectrum, the first antibody binding to an antigenic determinant that is differentially expressed on populations of leukocytes and non-leukocytes and about 1 μg of anti-CD16-PE, i.e., an additional antibody labeled with a second fluorochrome that has an emission spectrum distinguishable from the emission spectrum of the fluorochrome PC5. The anti-CD16 antibodybinds to an antigenic determinant that is differentially expressed on populations of mature and immature granulocytes or myeloid cells. This reaction mixture is mixed briefly and incubated at room temperature for approximately 10 minutes. The reaction was performed in the absence of a fluorescent dye.
[0197]A portion (about 34 μL) of this reaction mixture is then reacted for about 6 seconds with the lytic system (about 5...
PUM
| Property | Measurement | Unit |
|---|---|---|
| forward angle | aaaaa | aaaaa |
| peak emission wavelength | aaaaa | aaaaa |
| wavelength | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com