Thermal sensing device for thermal mapping of a body conduit
a sensing device and thermal mapping technology, applied in the direction of surgical instruments for cooling, therapeutic heating, therapeutic cooling, etc., can solve the problems of blood vessels subjected to angioplastic treatment having a marked tendency to undergo restnosis, evaporative cooling is not amenable to precise control of cooling process, and implementations described are limited to cryogenic cooling, etc., to achieve accurate control of balloon temperature, increase pressure, and high uniform distribution of cold
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
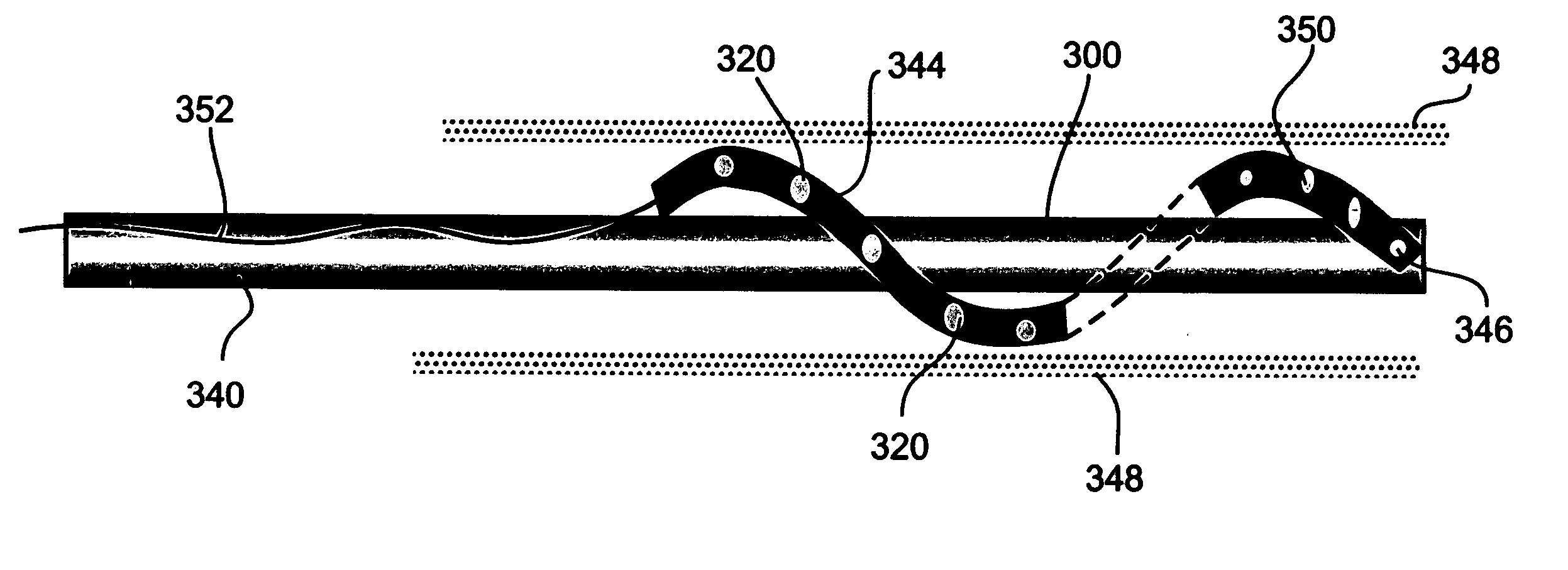
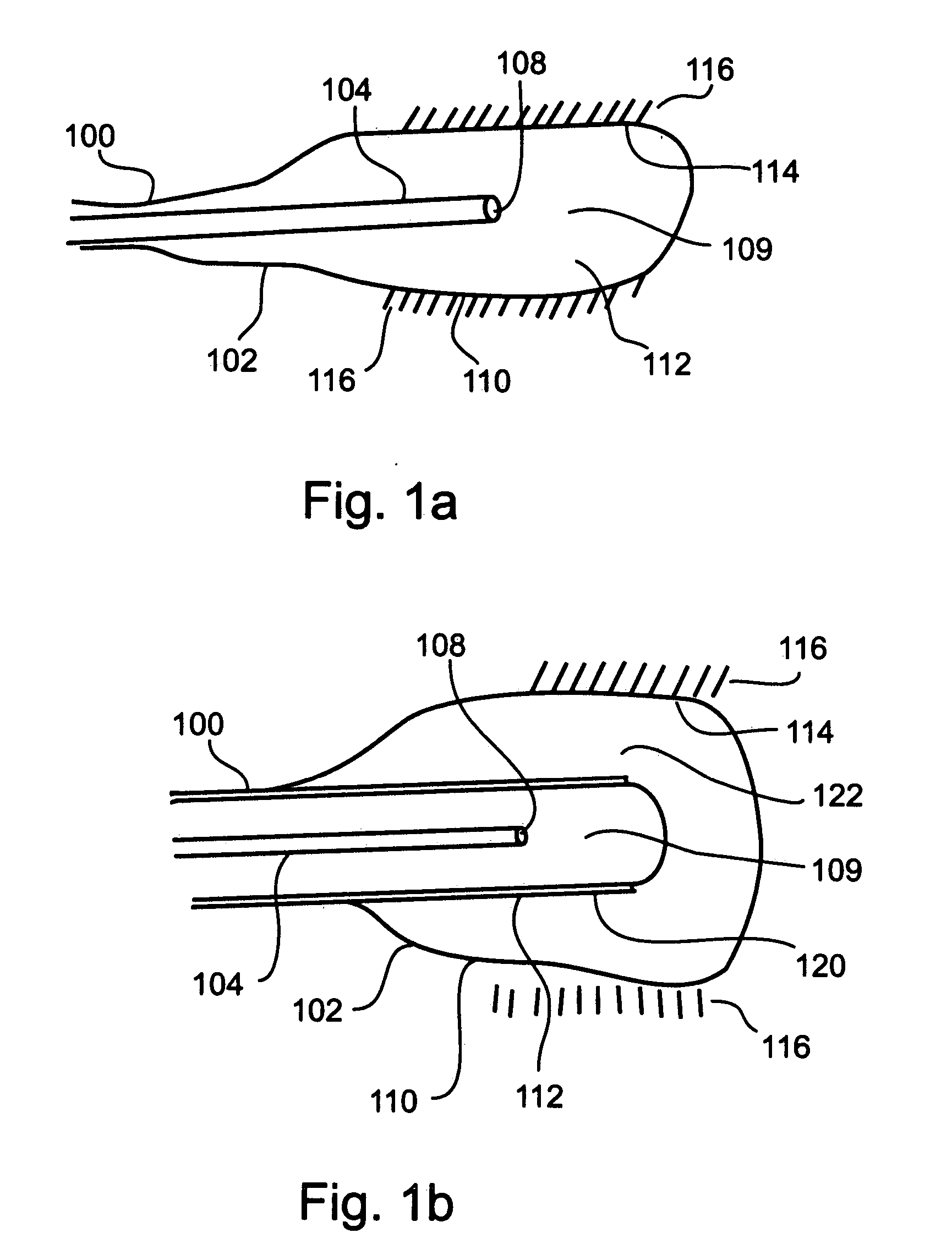
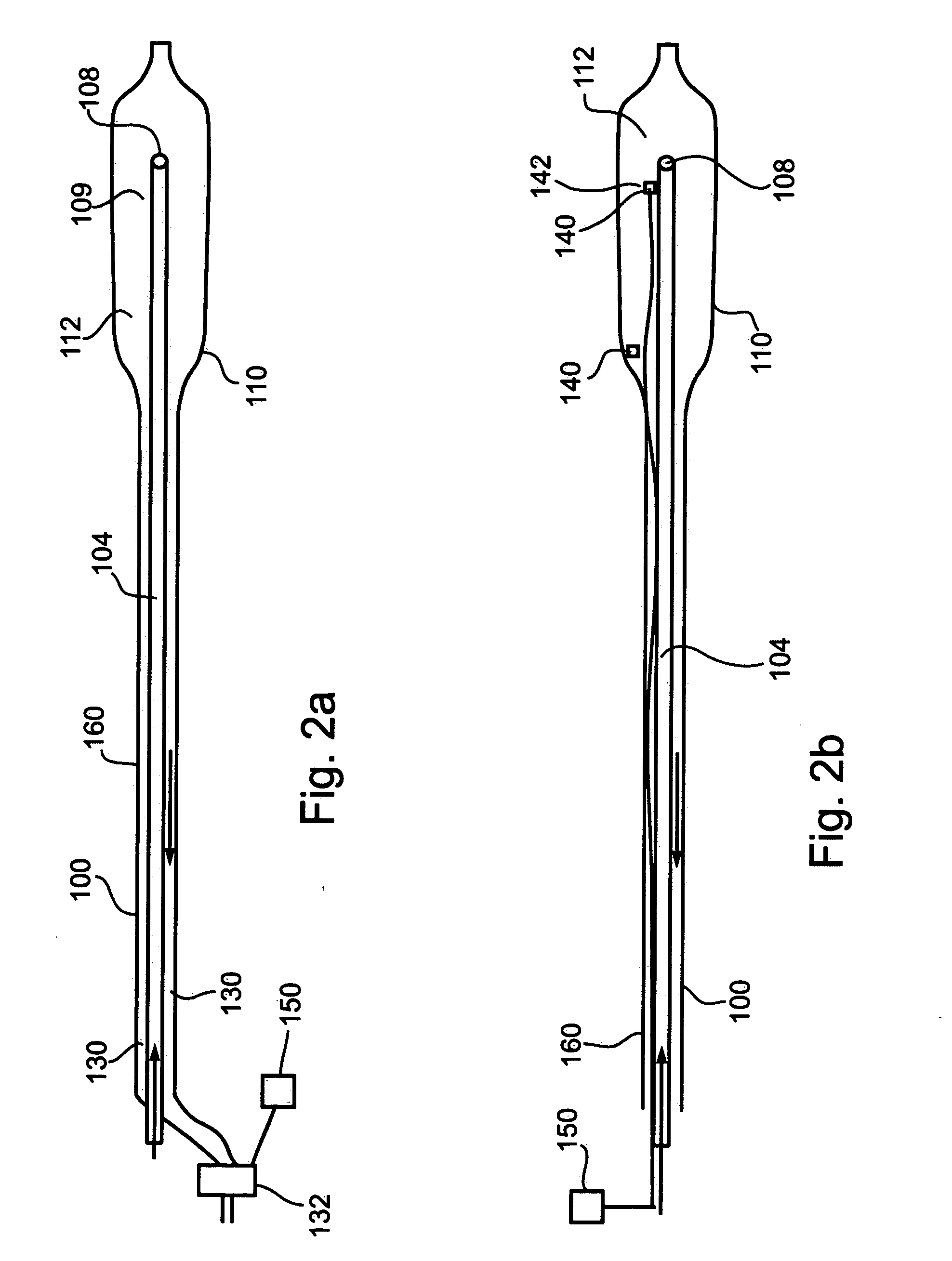
[0122] The present invention is of an angioplasty balloon catheter operable to utilize compressed gas for direct Joule-Thomson cooling of an angioplasty balloon with a high degree of temperature control, and having a plurality of temperature sensors operable to measure temperatures at a variety of locations within an artery, thereby providing information permitting to identify a locus for placement of an angioplasty balloon for treatment of arterial stenosis.
[0123] Specifically, the present invention can be used to accurately place an angioplasty balloon in a position appropriate for balloon angioplasty treatment of stenosis, and to directly cool an angioplasty balloon during use in treatment of stenosis, thereby discouraging or preventing restenosis.
[0124] The principles and operation of a cryogenic angioplasty balloon catheter according to the present invention may be better understood with reference to the drawings and accompanying descriptions.
[0125] Before explaining at leas...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com