Adjustable prosthetic valve implant
a prosthetic valve and implant technology, applied in the field of adjustable prosthetic valve implants, can solve the problems of ineffective closure of valve leaflets, insufficient valve leaflets, and inability to adjust the size of the implant,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
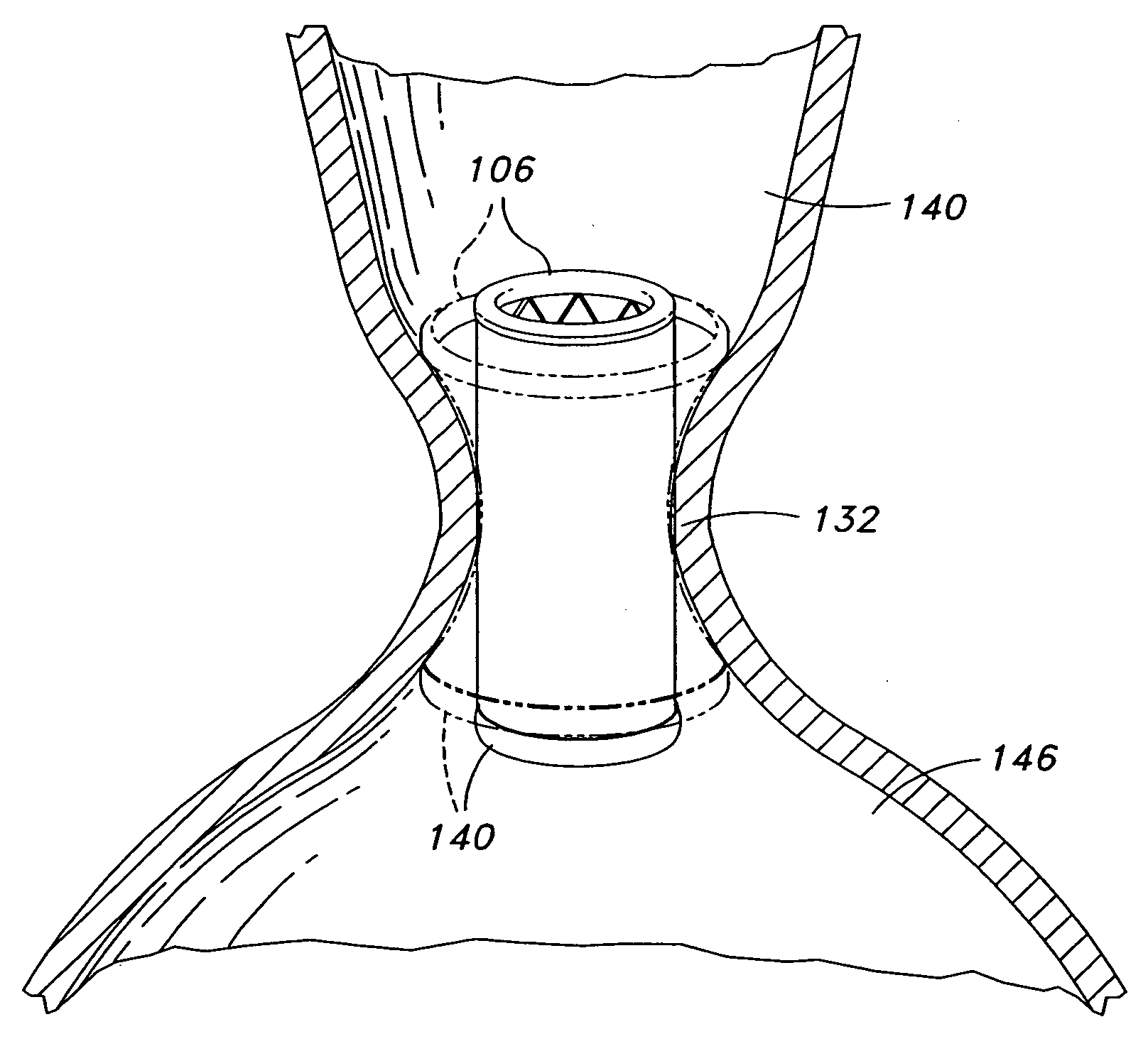
embodiment 100
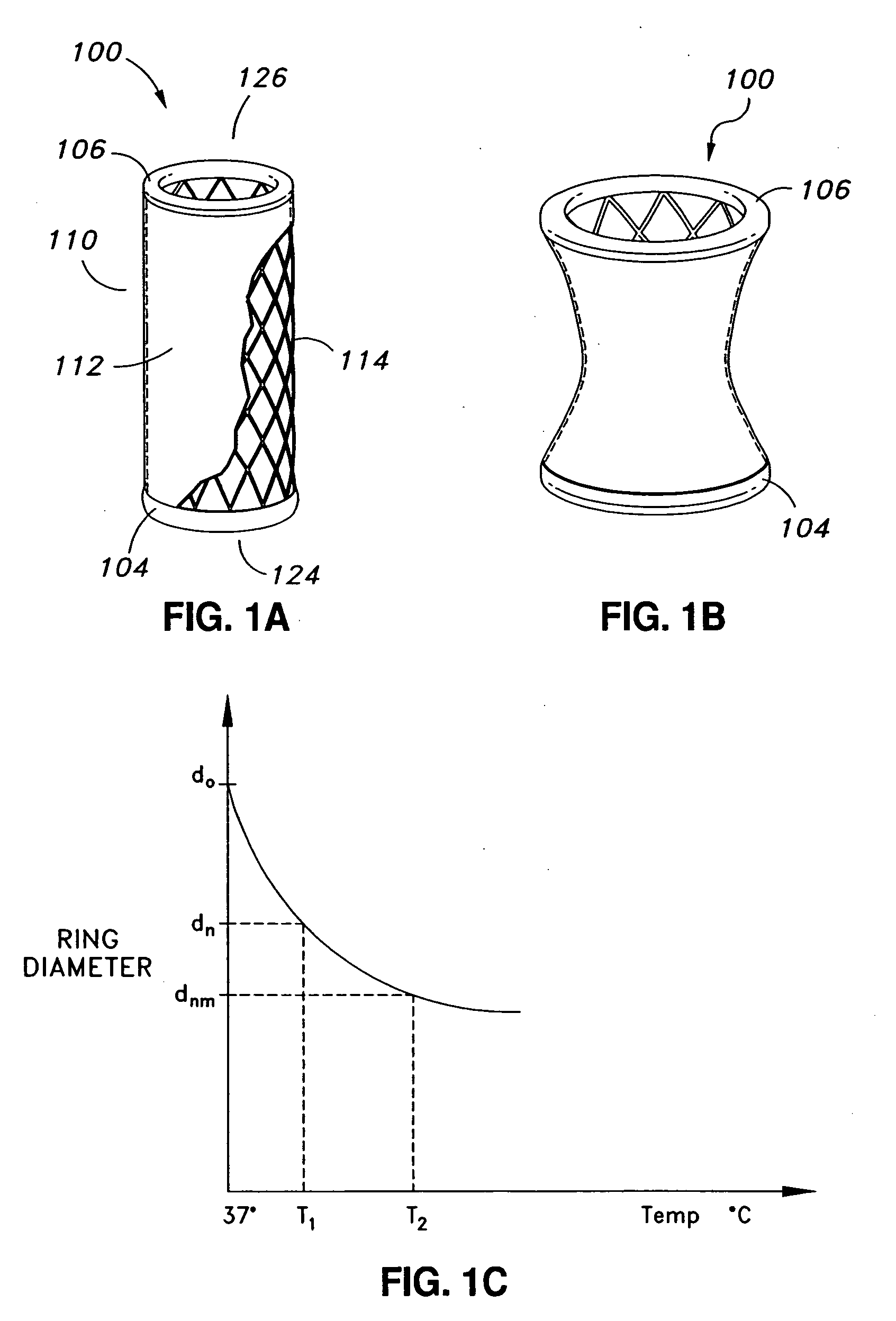
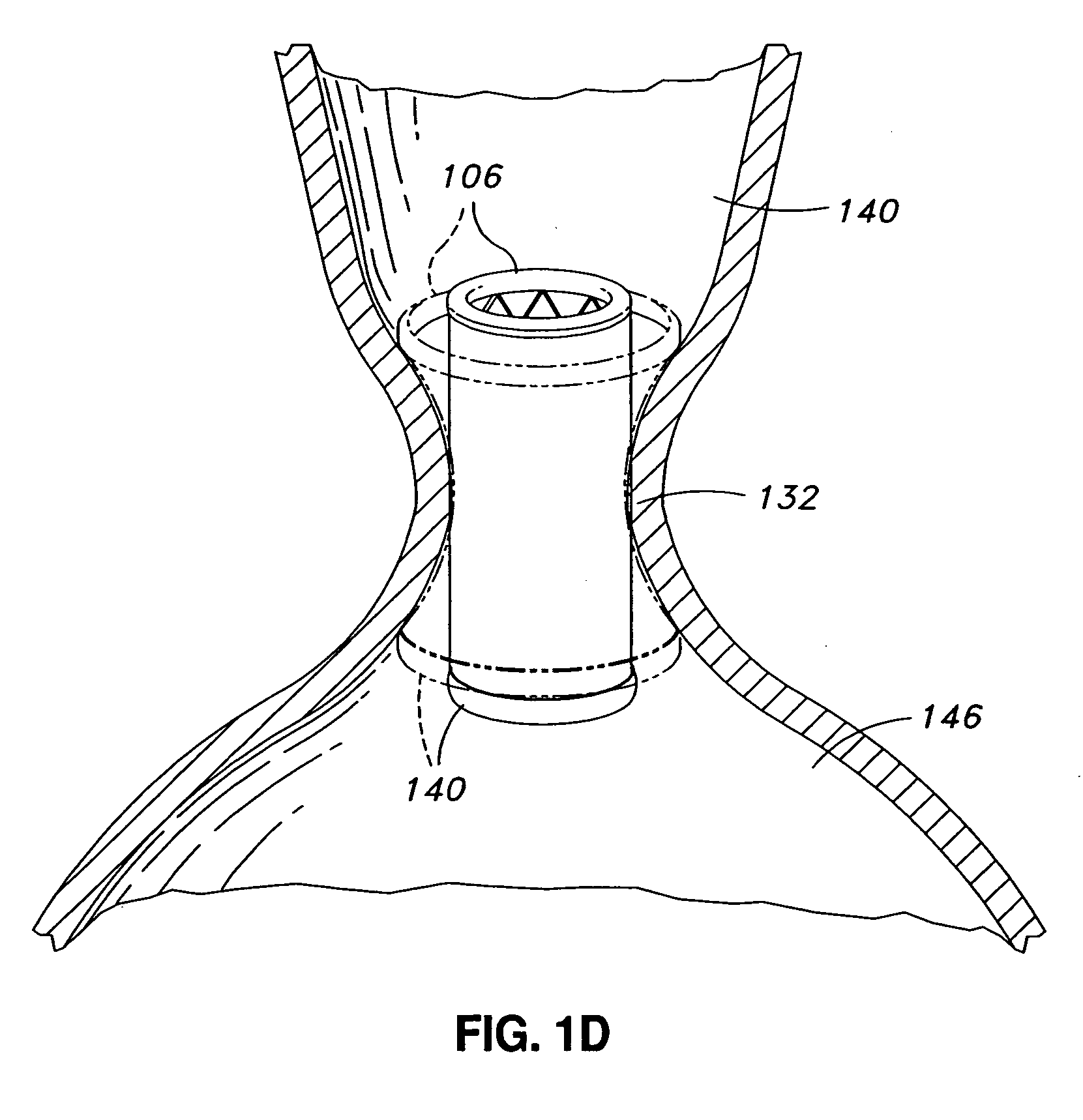
[0107] The illustrated embodiment 100 comprises a plurality of adjustable elements which, in the illustrated embodiment, are adjustable rings 104 and 106. Those skilled in the art will understand that the following description of the adjustable rings 104 and 106 is equally applicable to other types of adjustable elements. As used, the term “ring” broadly refers to shapes that are closed or open. In the illustrated embodiment, the adjustable rings 104 and 106 are substantially circular, closed rings.
[0108] In certain embodiments, the prosthetic valve implant may comprise additional adjustable rings. For example, in certain embodiments, the prosthetic valve implant may comprise an adjustable ring in a location substantially equidistant from the rings 106 and 104 located at the proximal and distal ends 126 and 124 of the implant 100, respectively.
[0109] In the illustrated embodiment, adjustable rings 106 and 104 are located at the proximal 126 and distal ends 124 of the implant 100, r...
embodiment 800
[0150]FIG. 9 illustrates a side view of an embodiment of a prosthetic valve implant 900 according to certain embodiments. The implant 900 is illustrated in an unadjusted configuration in solid lines, and in an adjusted configuration in phantom. The central region 902 of the implant 900 comprises an inward depression 908 on one side, similar to the embodiment 800 illustrated in FIG. 8. The construction and materials for this embodiment are substantially similar as described above for the embodiment illustrated in FIG. 6. Upon adjustment of the prosthetic valve implant 900, the depression 908 increases in depth and width. The depression 908 in the side of the implant 900 in its adjusted shape has become substantially larger than in the unadjusted configuration. In certain embodiments, the upstream end 906 portion and the downstream end 904 portion remain unaffected by the adjustment.
[0151] Although the embodiments of the adjustable prosthetic valve implant described so far are substan...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com