Spine surgery method and inserter
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
first embodiment
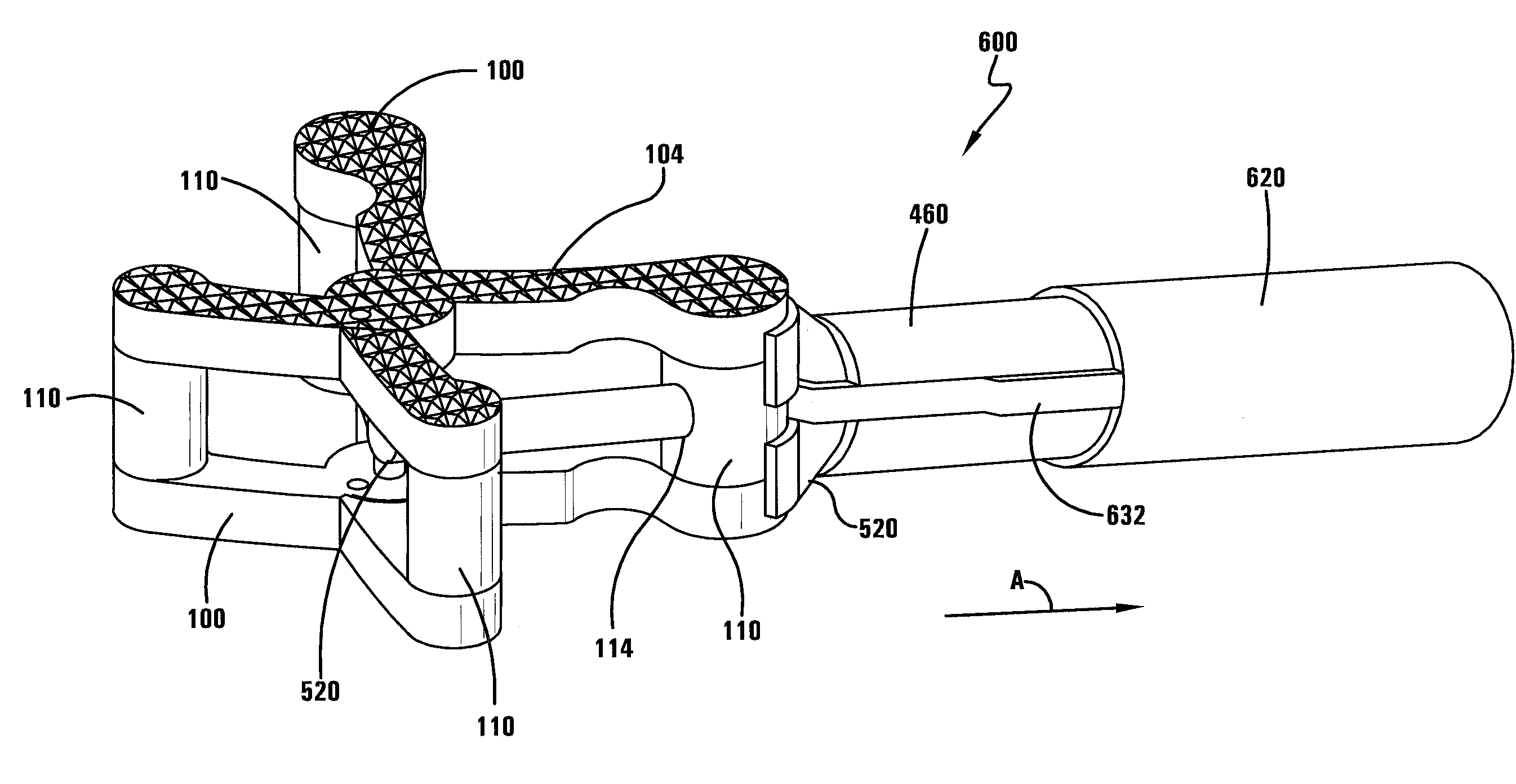
[0107]The first embodiment is shown in FIGS. 32-33. For this embodiment the wire 520 takes a linear path as it exits the inserter 200 and contacts the implant 100. In one specific embodiment, the post 110 gripped by the gripper 420 has a linear opening 114 that receives the wire 520 when it is extended out from the inserter 200. Continued extension of the wire 520 causes the distal end of the wire 520 to contact another implant surface, such as another post 110, to cause the implant 100 to deploy.
second embodiment
[0108]The second embodiment is shown in FIGS. 50-51. For this embodiment the wire 520 takes a curvilinear path as it contacts the implant 100. In one specific embodiment, the post 110 gripped by the gripper 420 has a curvilinear opening 116 that receives the wire 520 when it is extended out from the inserter 200. Continued extension of the wire 520 causes the distal end of the wire 520 to contact another implant surface, such as another post 110, to cause the implant 100 to deploy. In a more specific embodiment, the portion of the implant 100 that contacts the distal end of the wire 520 has a divot 118 on its surface that matches the surface shape of the distal end of the wire 520. In this way, the distal end of the wire 520 is received in the divot 118 making it easier for the wire 520 to stay in contact with the implant surface as it moves through the curvilinear motion.
[0109]With reference now to FIGS. 34-46, as also noted above with regard to a cable 560, in another embodiment a...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D Engineer
- R&D Manager
- IP Professional
- Industry Leading Data Capabilities
- Powerful AI technology
- Patent DNA Extraction
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2024 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com