Inflatable medical devices
a medical device and inflatable technology, applied in the field of inflatable structures, can solve the problems of difficult dilation or opening, difficult to pass through ctos, and difficult to dilate or open, and achieve the effect of improving the stability and stability of the devi
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
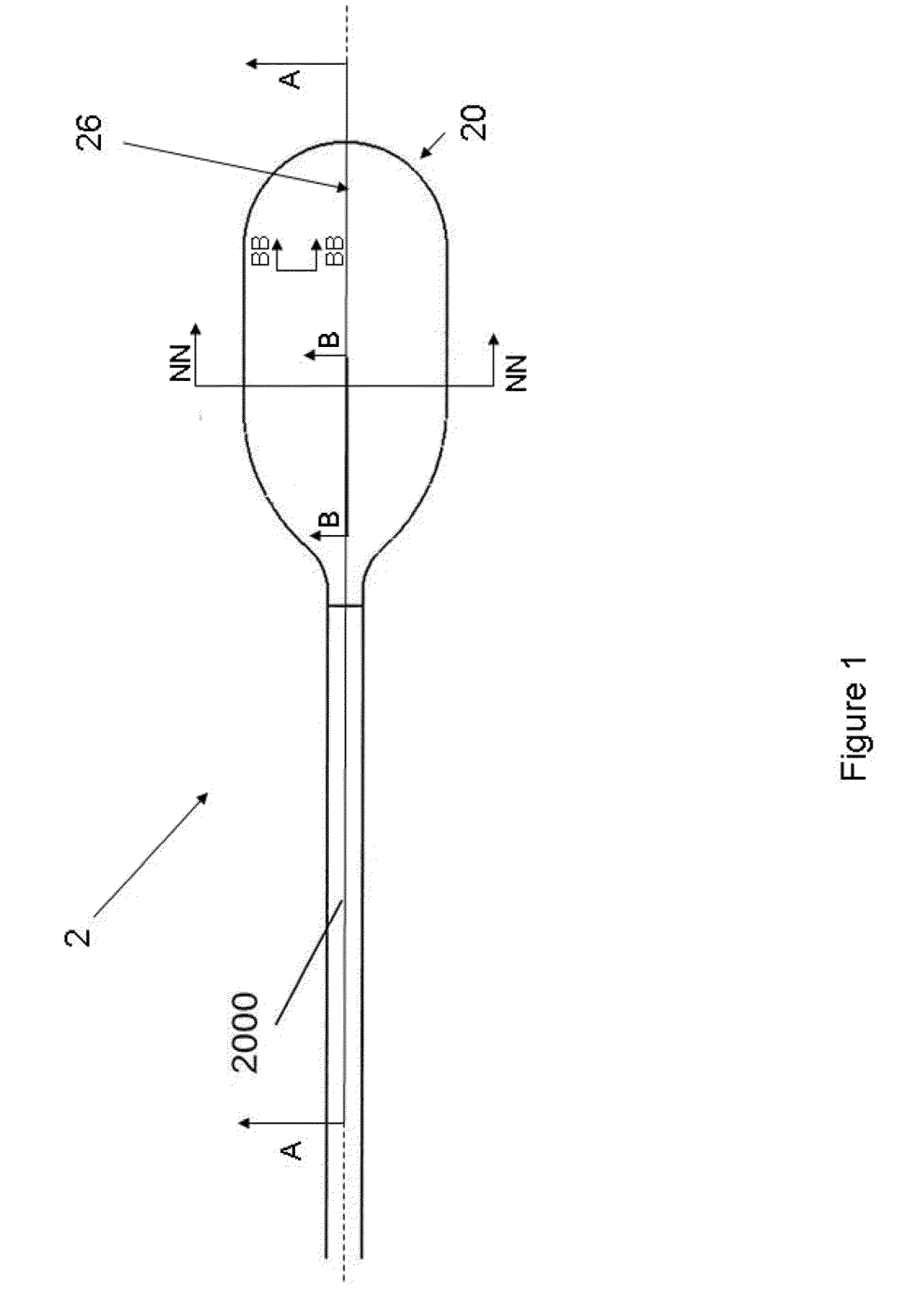
[0232]FIG. 1 illustrates that a medical inflatable device 2 can have a balloon 20 and a hollow shaft 2000. An inflation system (shown herein) can be attached to the hollow shaft to deliver a fluid pressure through the hollow shaft and to the balloon. The balloon can be resilient (i.e., elastic) or non-compliant (i.e., inelastic). The balloon 20 can have a balloon longitudinal axis 26. The balloon 20 can have a balloon wall 22. The balloon wall 22 can define a cavity having a balloon volume 24.
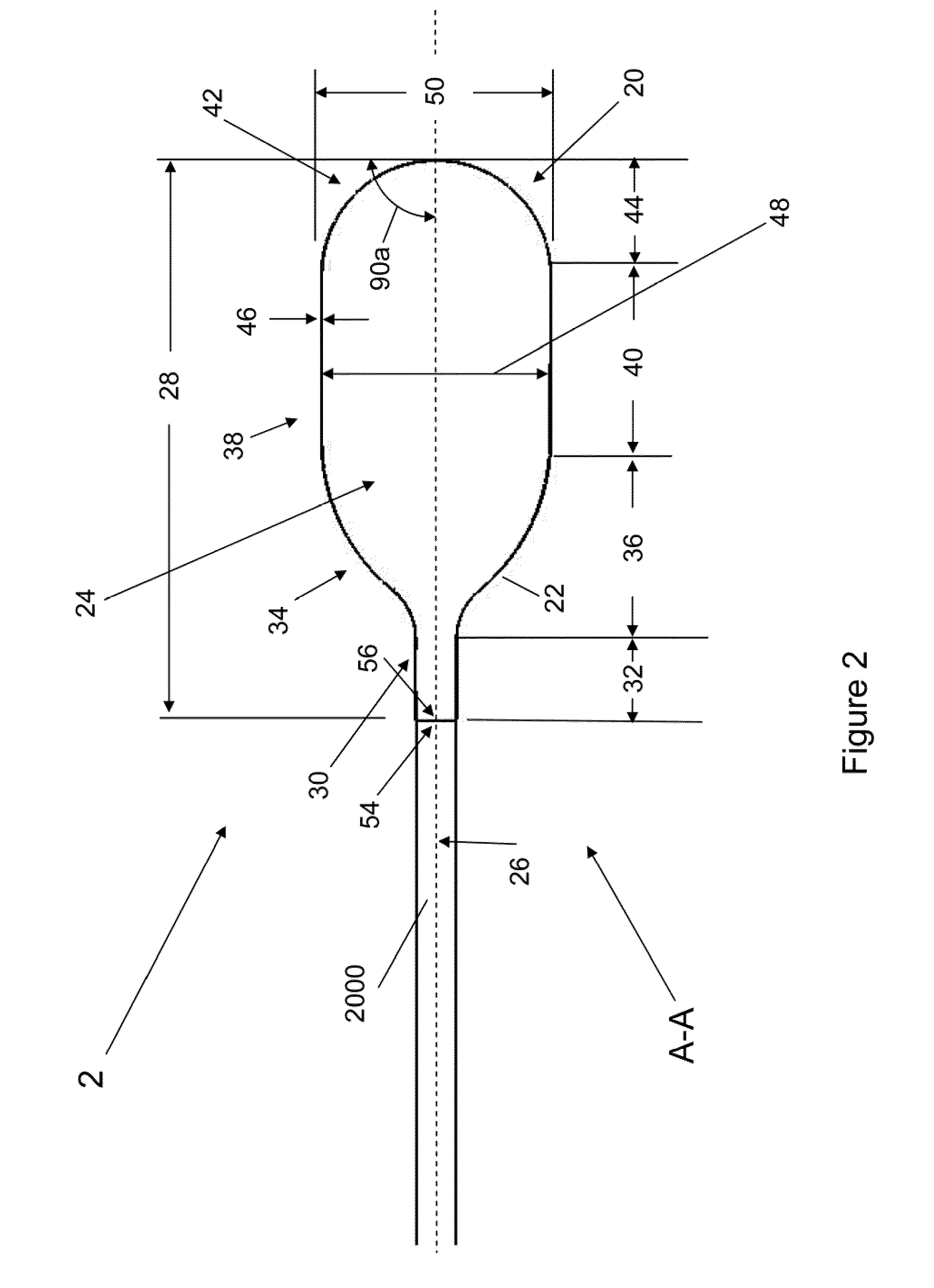
[0233]FIG. 2 illustrates that the balloon 20 can have balloon length 28. The balloon 20 can have a balloon proximal stem 30 having a balloon proximal stem length 32. The proximal stem length 32 can be from about 5 mm (0.2 in.) to about 15 mm (0.6 in.). The balloon can have a balloon proximal taper 34 having a balloon proximal taper length 36. The balloon proximal taper length 36 can be from about 0 mm (0 in.) to about 20 mm (0.8 in.), more narrowly from about 0 mm (0 in.) to about 15 mm (0.6 in...
PUM
| Property | Measurement | Unit |
|---|---|---|
| inner diameter | aaaaa | aaaaa |
| inner diameter | aaaaa | aaaaa |
| burst pressure | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com