Methods and Apparatus for Endovascular Heart Valve Replacement Comprising Tissue Grasping Elements
a heart valve and tissue grasping technology, applied in the field of endovascular heart valve replacement methods and apparatuses, can solve the problems of heart valve replacement surgery, adverse reactions to anesthesia medications, bleeding, stroke, etc., and achieve the effect of preventing blood backflow and allowing blood flow
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
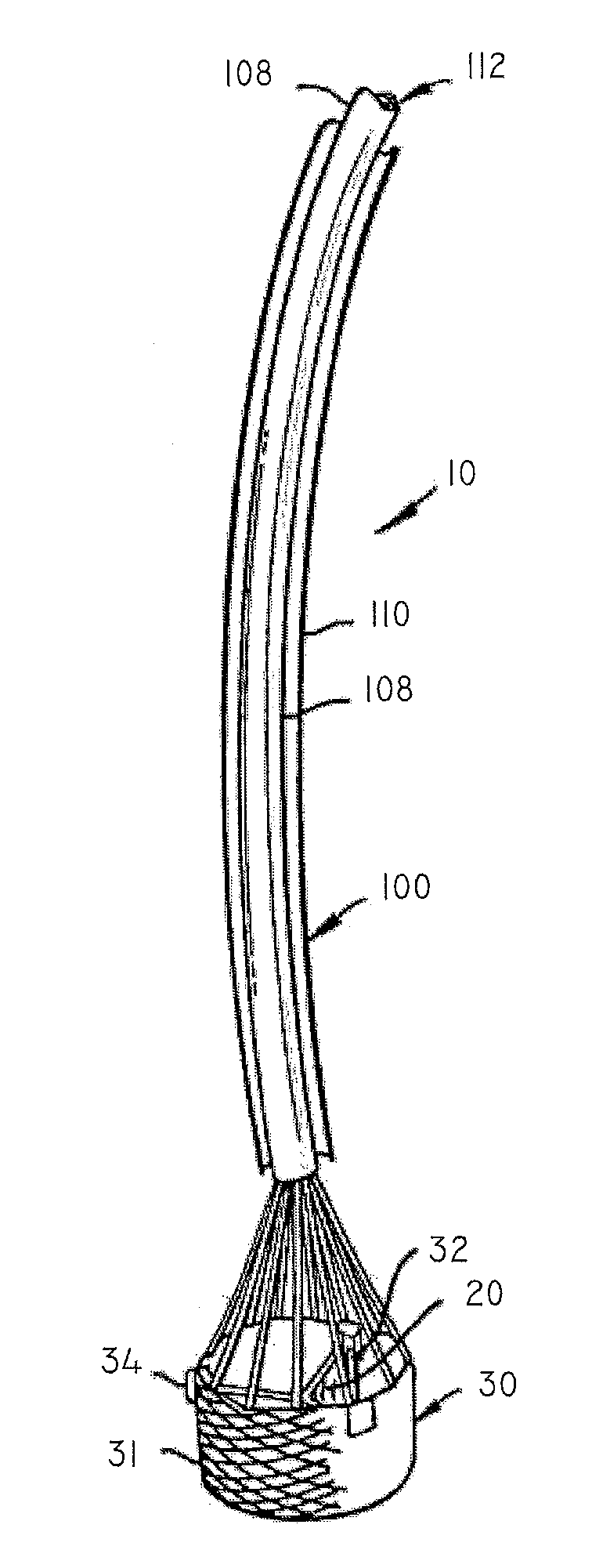
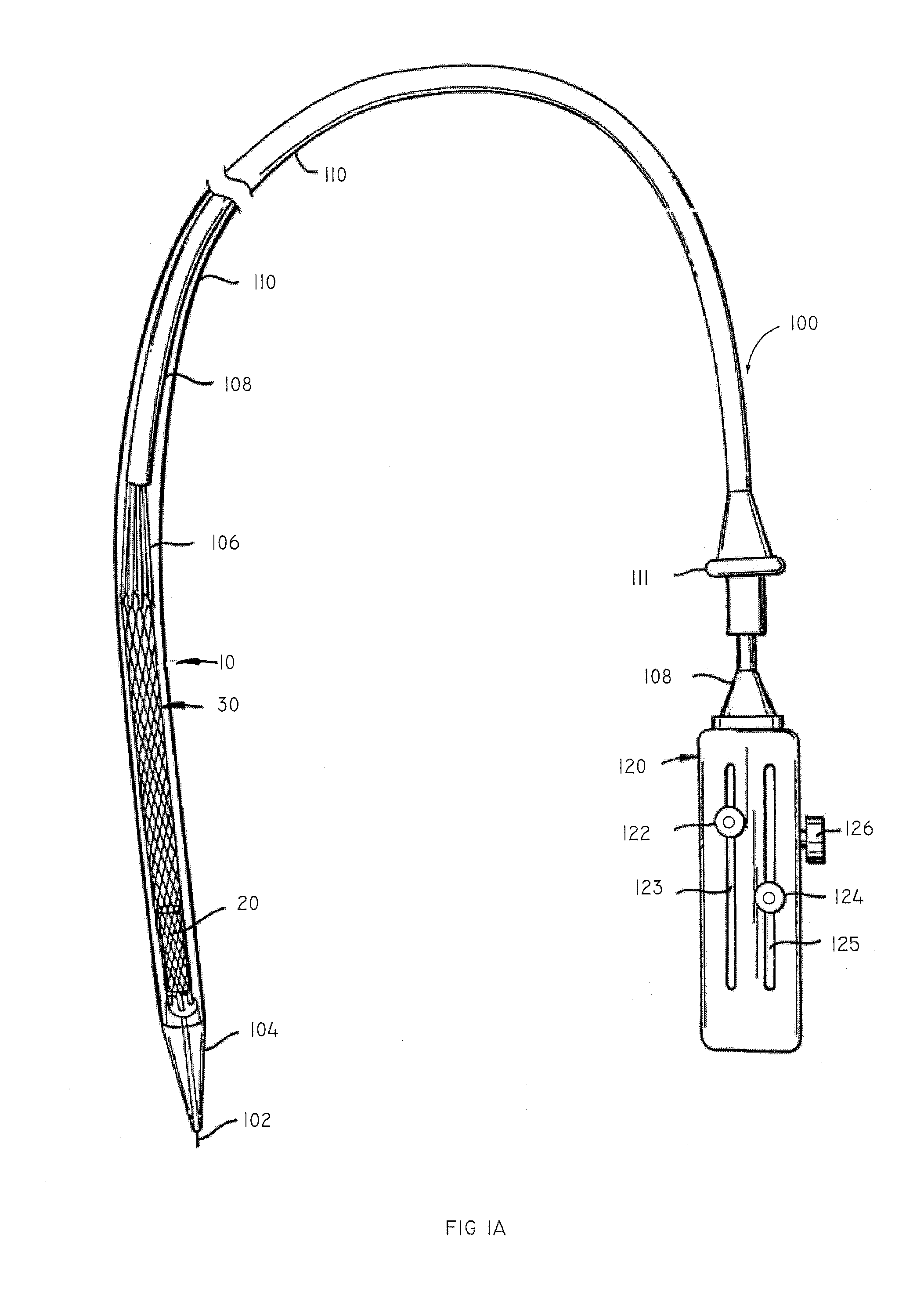
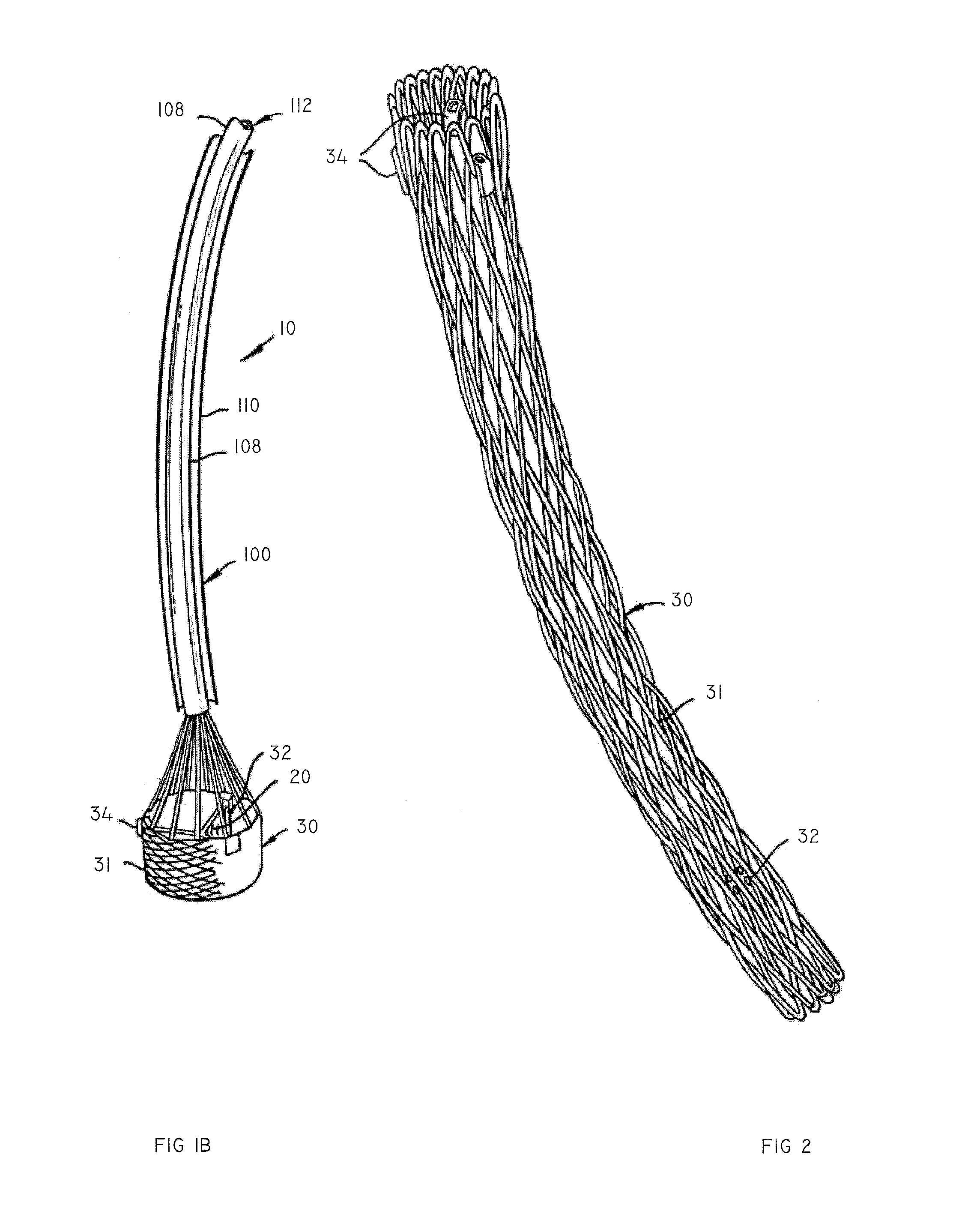
[0048]The present invention relates to an apparatus and methods for endovascularly delivering and deploying an aortic prosthesis within a patient's native heart valve, referred to hereinafter as “replacing” a patient's heart valve. The delivery system includes a sheath assembly, a multi-lumen shaft, and a guide wire for placing the apparatus endovascularly within a patient and a user control allowing manipulation of the aortic prosthesis. The apparatus includes an anchor and a replacement valve. The anchor and the replacement valve are adapted for percutaneous delivery and deployment within a patient's heart valve.
[0049]In some embodiments, the apparatus includes engagement elements and / or a seal inverting element situated along a proximal region of the anchor. The engagement elements are adapted to engage the native leaflets of the patient's heart, or more preferably the proximal edge and / or the commissural attachments of the native leaflets. The engagement elements need not extend...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com