Guided ablation with end-fire fiber
a technology of end-fire fiber and ablation apparatus, which is applied in the field of surgical instruments, can solve the problems of reduced physical activity, stroke, atrial fibrillation, and particularly difficult, and achieves the effects of reducing physical activity, and reducing the risk of strok
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
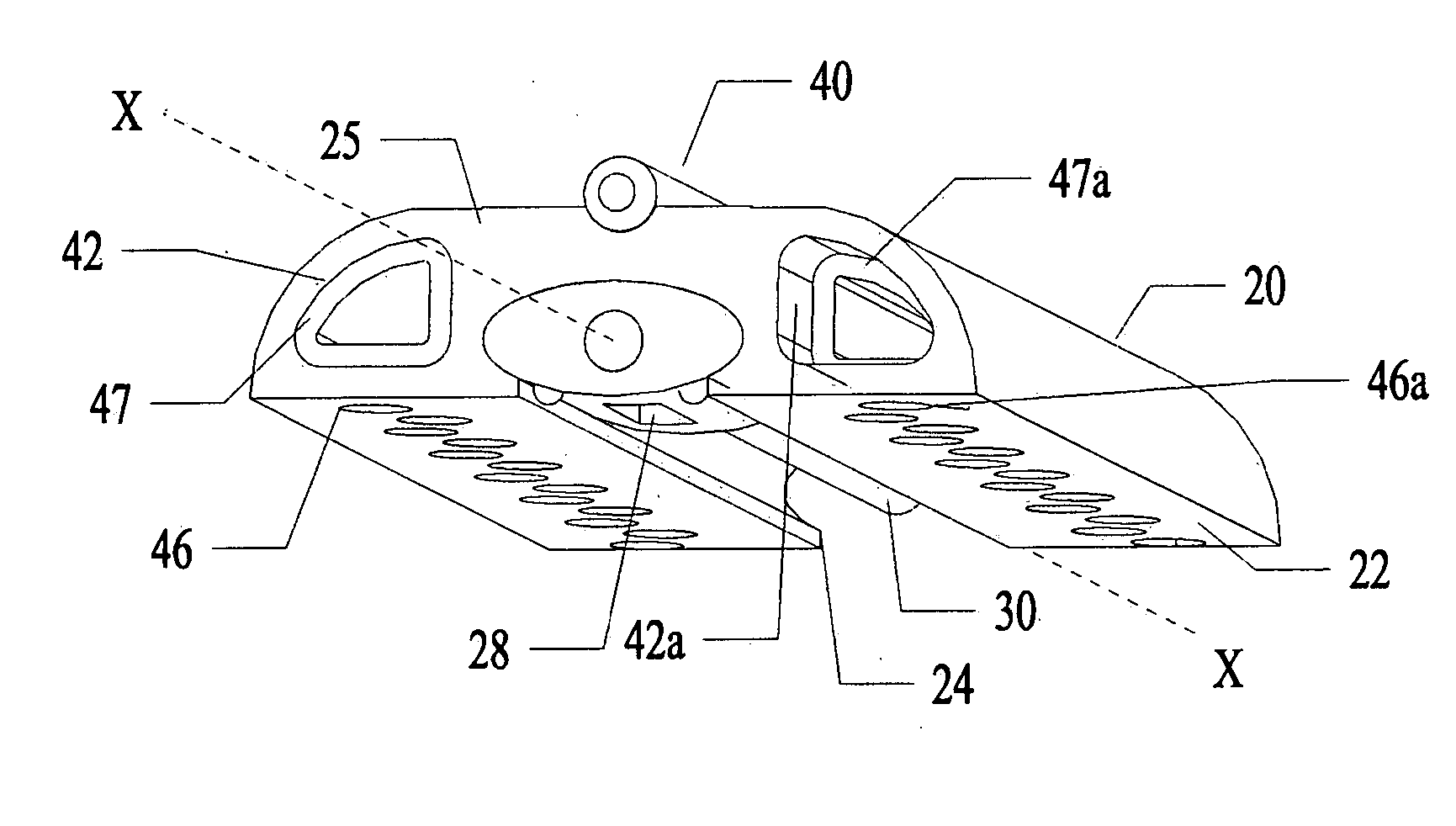
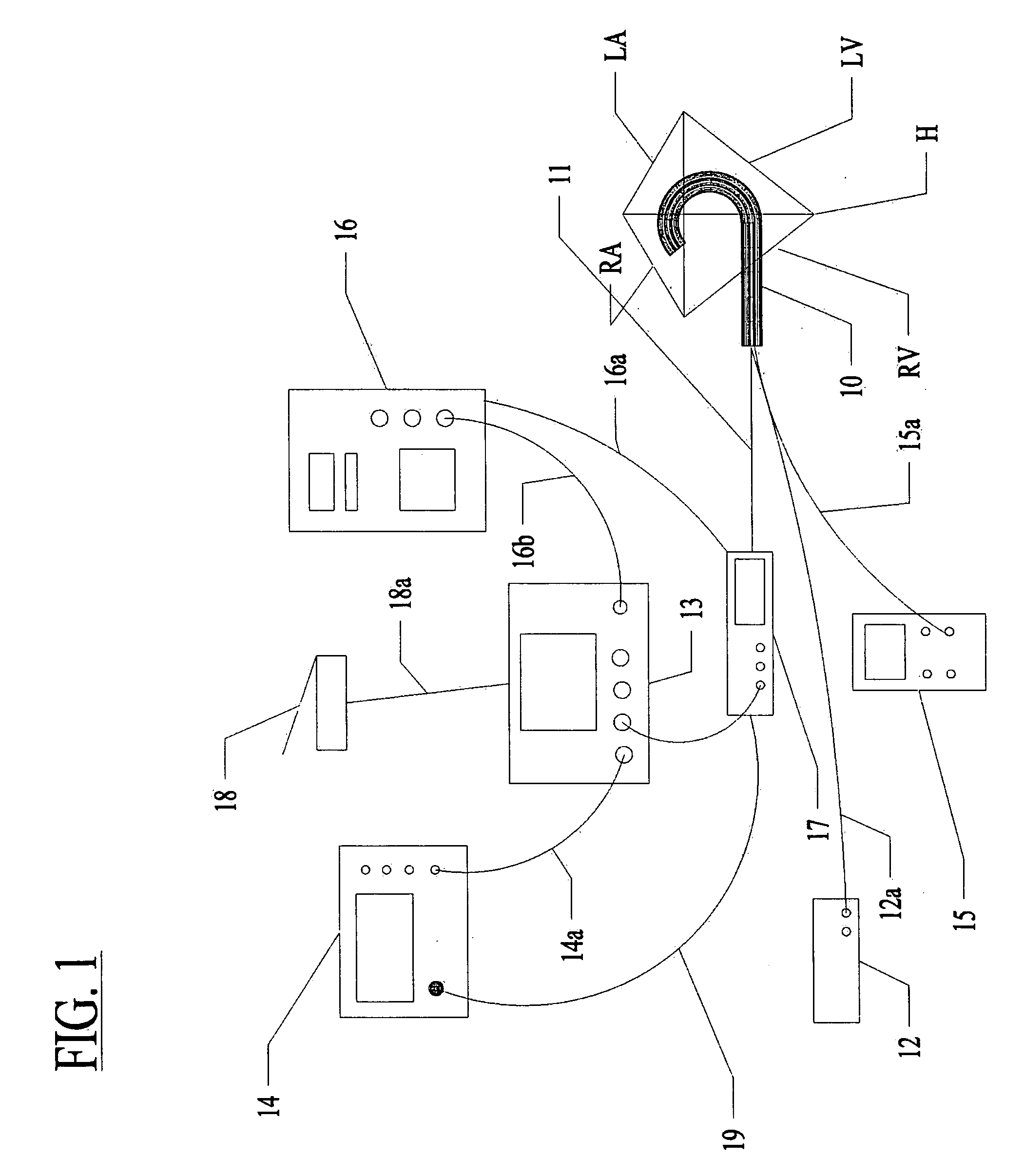
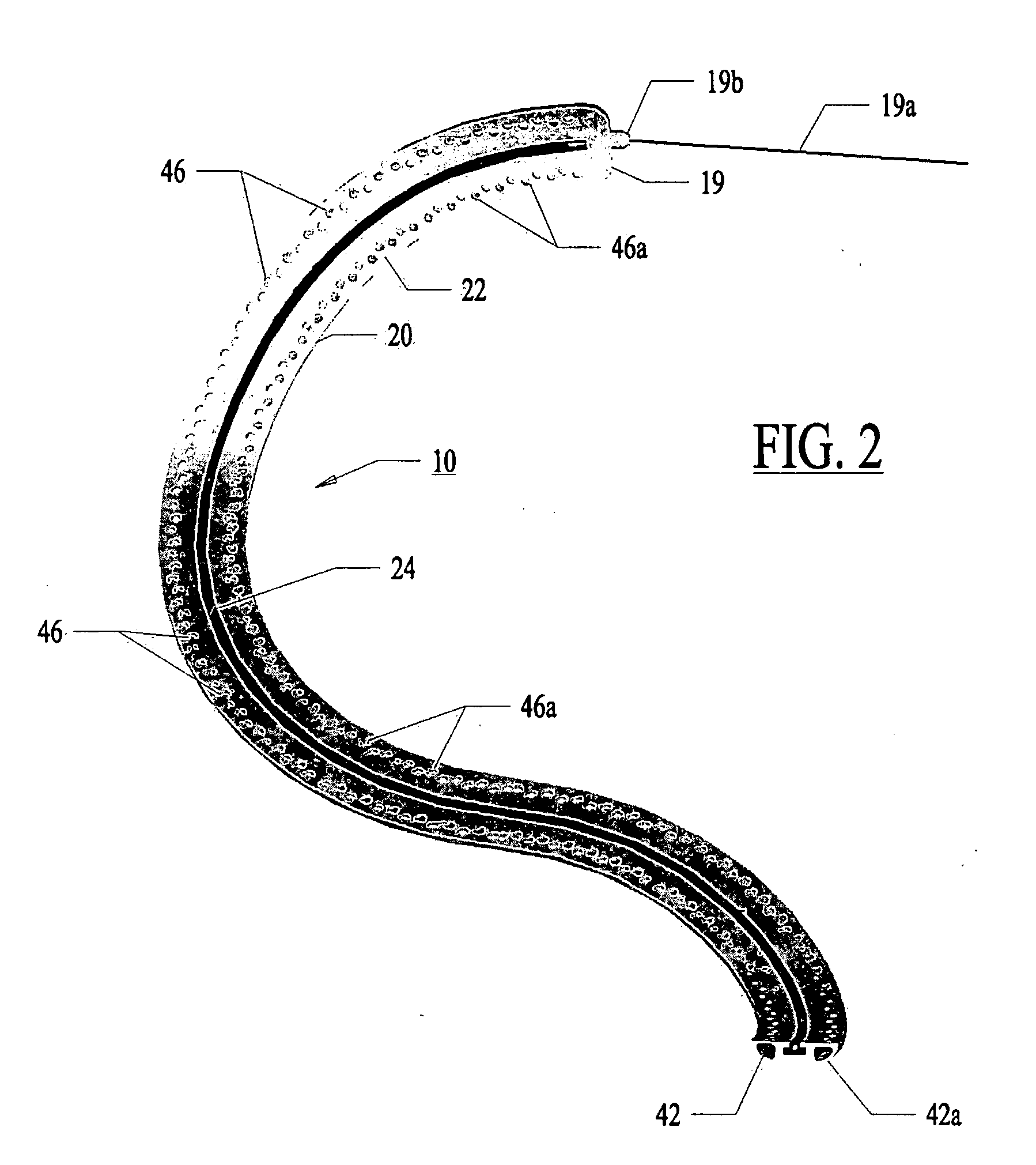
[0074] Referring now to the several drawing figures in which identical elements are numbered identically throughout, a description of a preferred embodiment of the present invention will now be provided. In the preferred embodiment, the invention is described as a lesion formation tool for applying laser energy to the epicardial surface of the heart to create a transmural ablation line along the heart. As used in this application, the term “ablation” is used in the context of creating necrosed tissue in the myocardium while avoiding tissue perforation or removal. In the following description, a guide member is described for guiding a lesion formation tool in a MAZE pattern. It will be appreciated the teachings of the present application could be applied to other types of ablation tools (e.g., RF ablation, ultrasound or other). Also, this application may refer to a lesion as “linear”. The use of “liner” is not meant to be limited to a straight line but is intended to include a curved...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com