Tissue ablation apparatus and method
a tissue and apparatus technology, applied in the field of tissue ablation apparatus and method, can solve the problems that current ablative therapies have not considered nor provided solutions to these problems, and achieve the effects of reducing power levels, facilitating ablation, and facilitating ablation
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
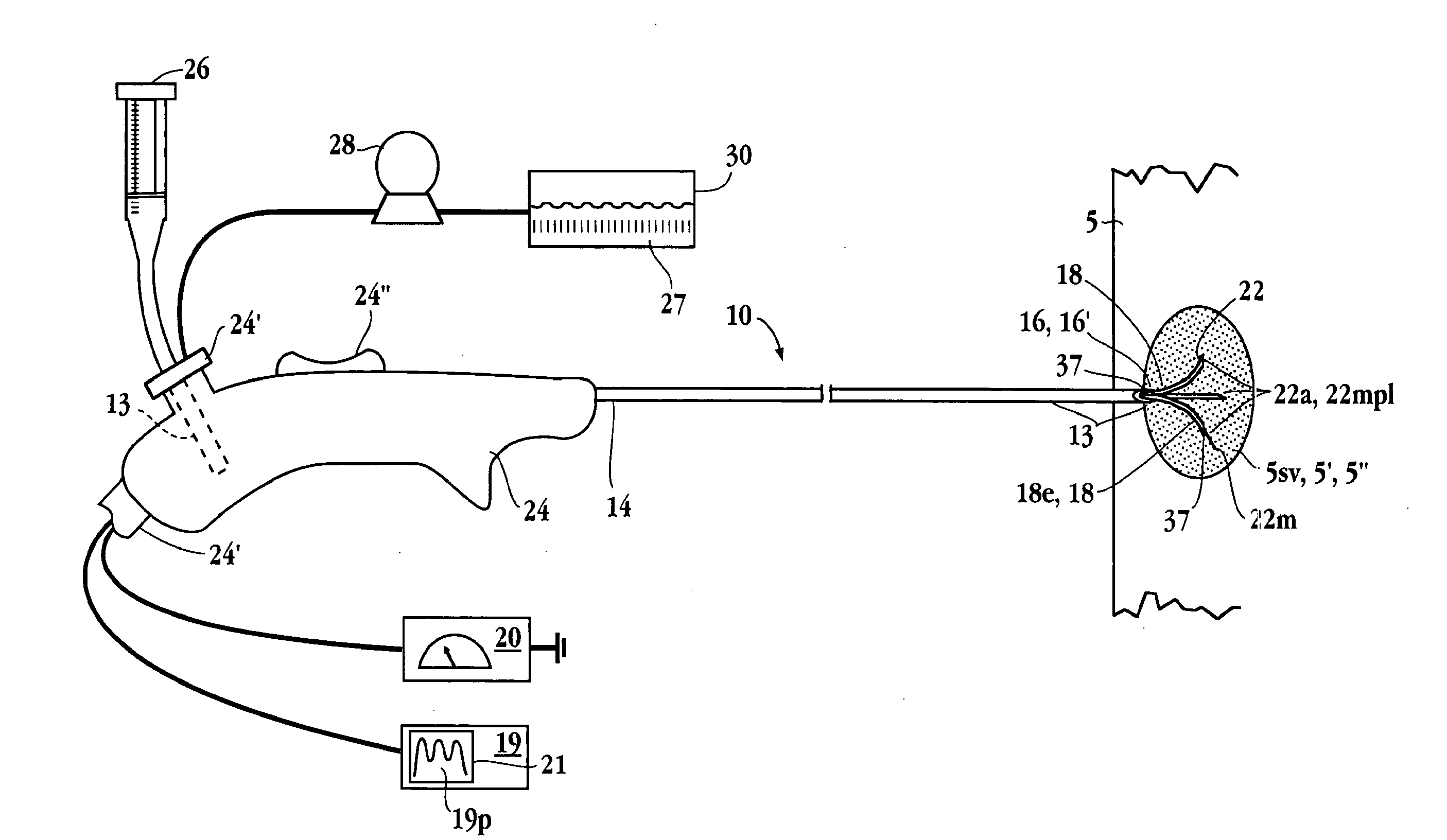
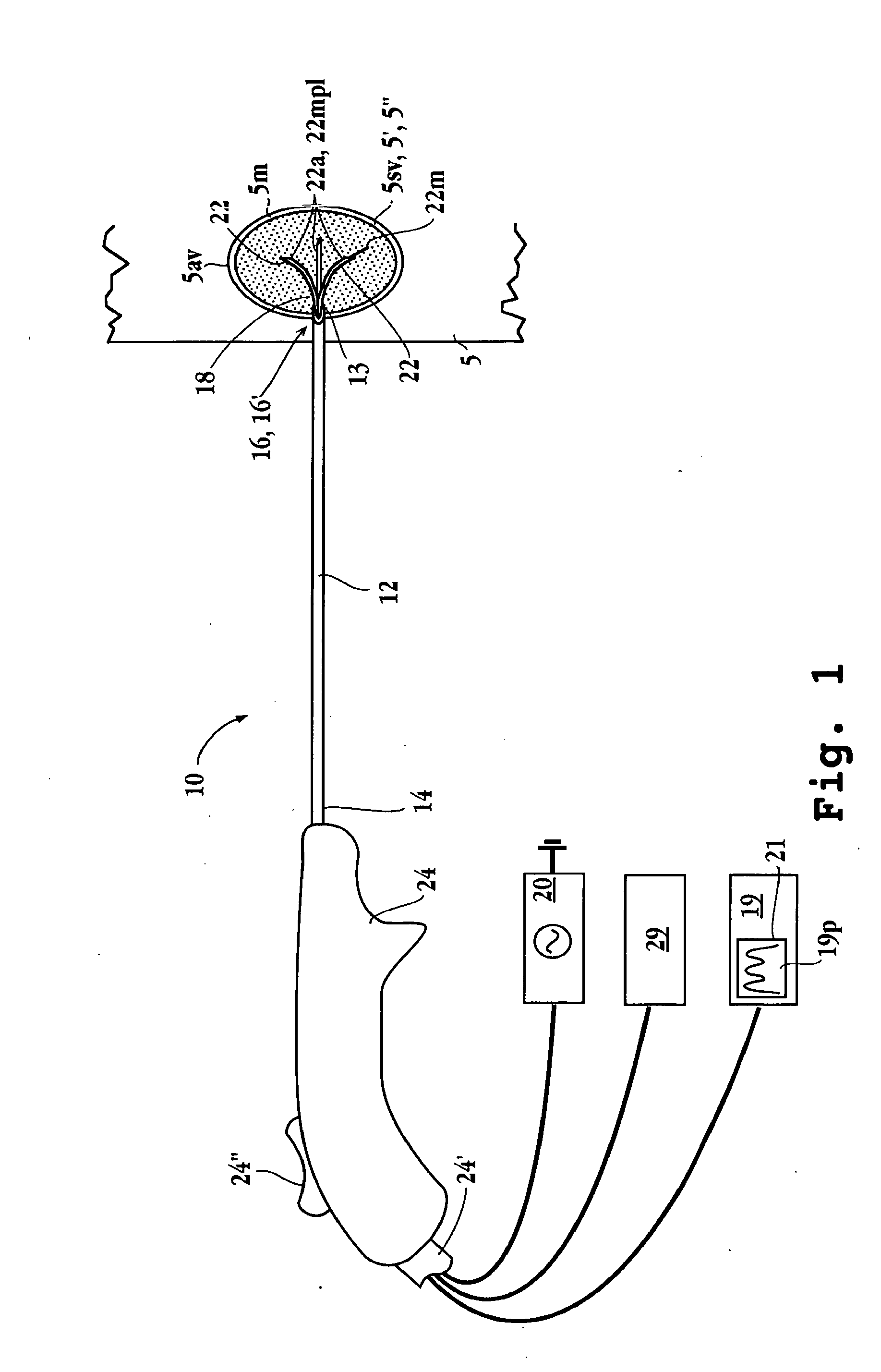
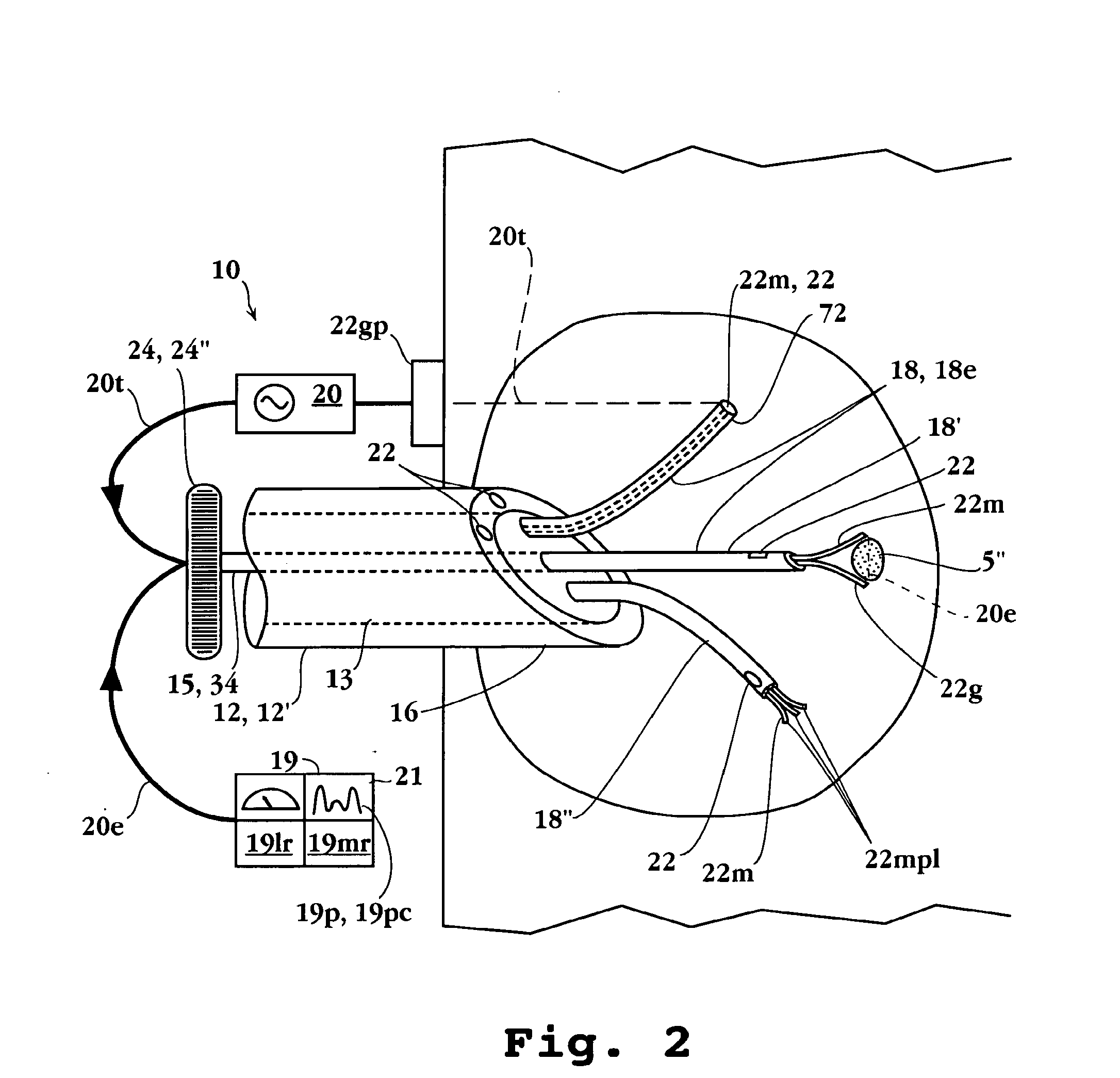
Image
Examples
Embodiment Construction
Definitions
[0052]The terms below, as used herein, have the following meanings, unless indicated otherwise:
[0053]“Electrode”, “resilient member” and “antenna” are interchangable and refer to a needle or wire for conducting energy to a tissue site. Electrodes may be passive, active or switchable between passive and active. Further, an electrode may be a ground pad electrode positionable at an exterior position on the patient.
[0054]A “sensing member” is a passive or active electrode for sensing an ablation parameter.
[0055]“Fluid delivery device” and “infusion device” are interchangable and refer to a device connected to, or including (i) a source of fluid to be infused, and (ii) one or more electrodes or the elongated delivery device for delivery of the fluid to a target tissue.
[0056]“Feedback control device”, “control unit”, “control resources”, “feedback control system”, and “controller” are interchangable and refer to a control capable of modulating an ablation parameter, i.e. power...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com