Apparatus and method for protecting tissues during cryoablation
a neurovascular bundle and apparatus technology, applied in the field of apparatus and method for protecting tissues during cryoablation, can solve the problems of neurovascular bundle, no schatzberger's technique nor any other known technique has proved sufficiently accurate, and the effect of less effective ablation
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
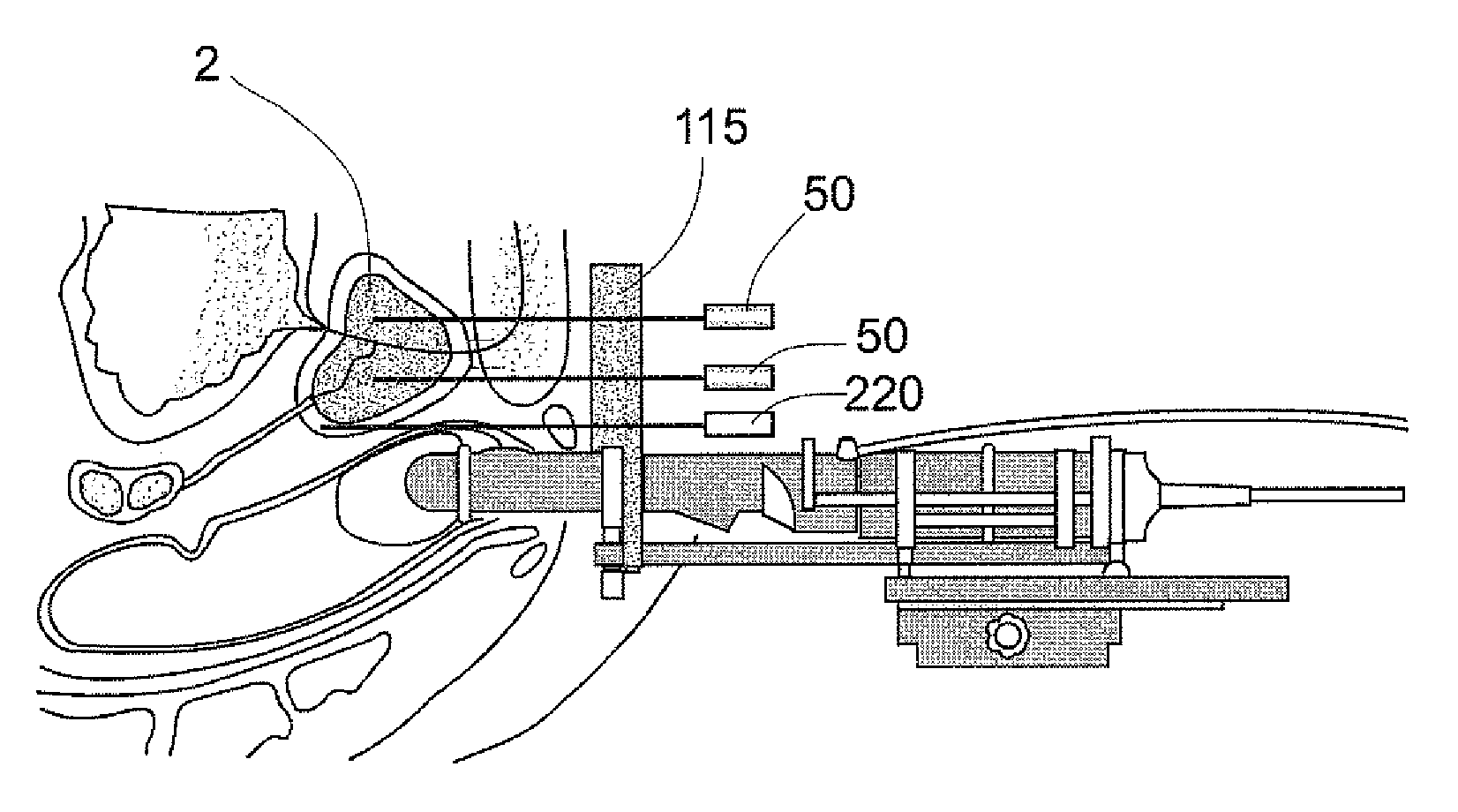
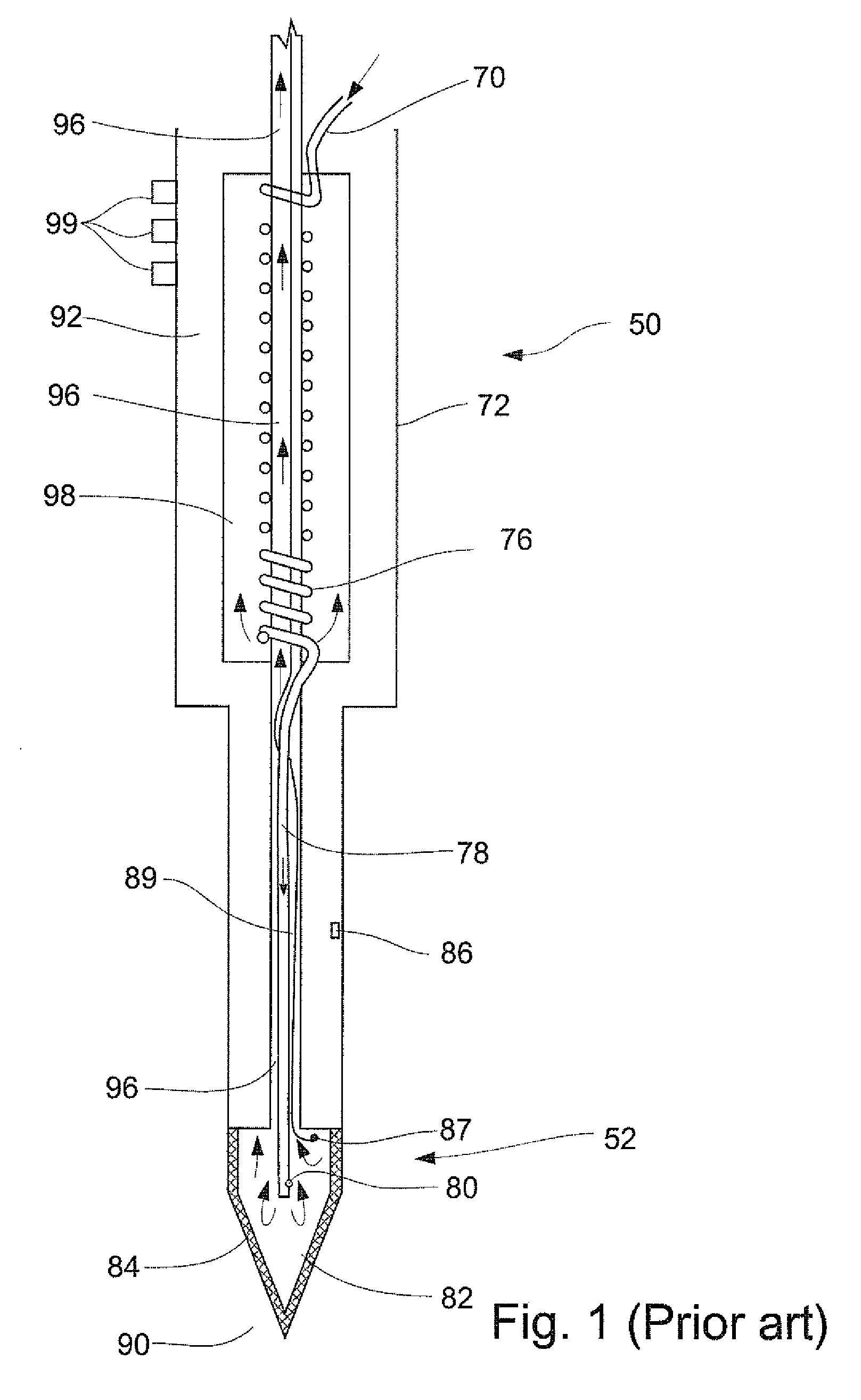
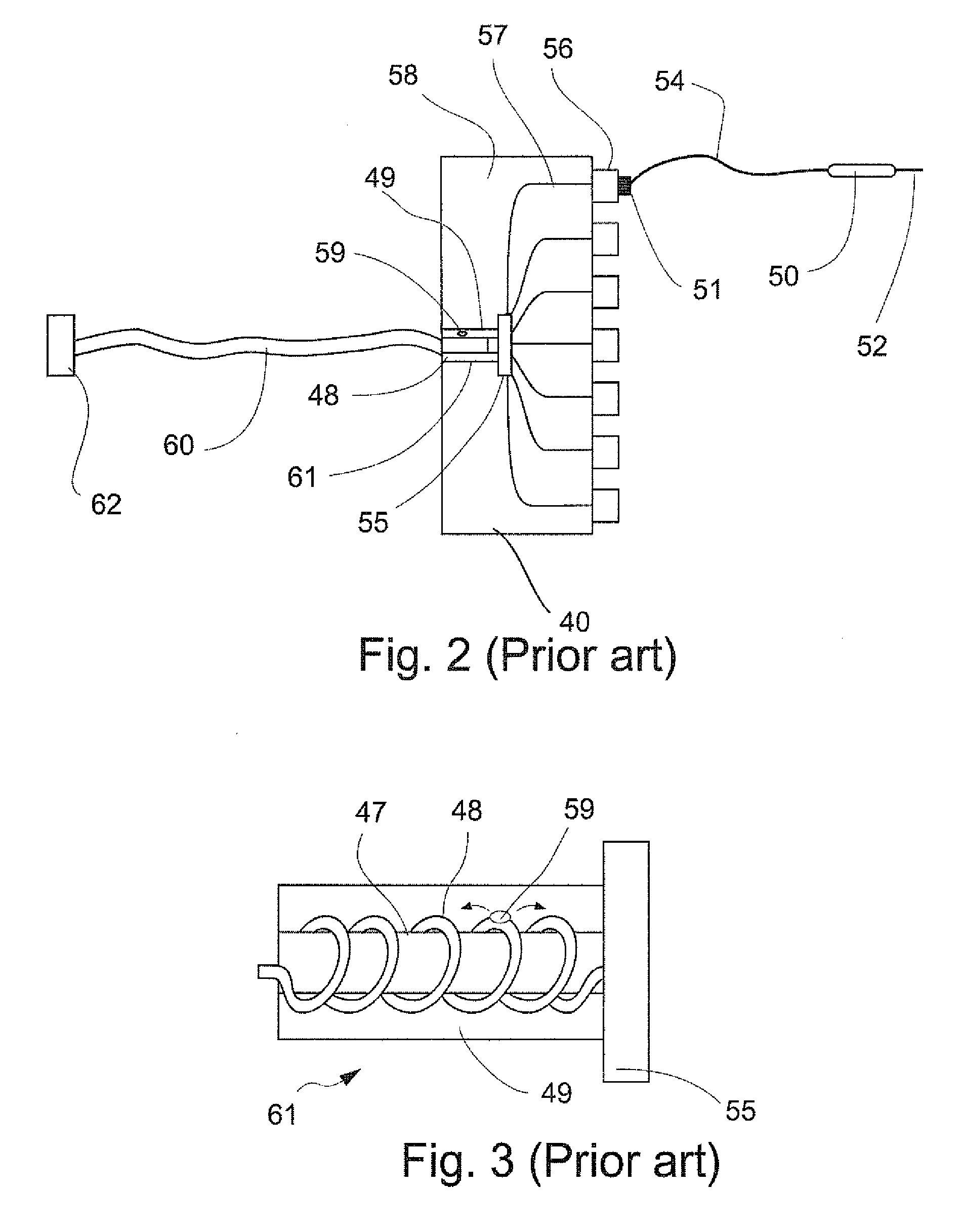
[0056]The present invention is of apparatus and method for protecting healthy tissues from damage, while cryoablating pathological tissues nearby. More particularly, the present invention relates to heating a first selected tissue area in or near a prostate, such as the neurovascular bundle area, while cooling to cryoablation temperatures a second selected tissue area in or near a prostate, such as benign or malignant tumor tissue, thereby cryoablating selected pathological tissues while protecting the neurovascular bundle or other selected healthy tissues from damage. The invention can be used to protect the neurovascular bundle during cryosurgery of prostate tissues, thereby reducing the risk of adverse effects of prostate cryosurgery to penile erectile functioning of a patent so treated.
[0057]Before explaining at least one embodiment of the invention in detail, it is to be understood that the invention is not limited in its application to the details of construction and the arran...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com