Method to inhibit airway hyperresponsiveness using aerosolized t cell receptor antibodies
a technology of t cell receptor and anti-airway, which is applied in the direction of antibody medical ingredients, aerosol delivery, spray delivery, etc., can solve the problems of drug-induced lung disease, and increased susceptibility to infection, so as to reduce the airway hyperresponsiveness of the mammalian body
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
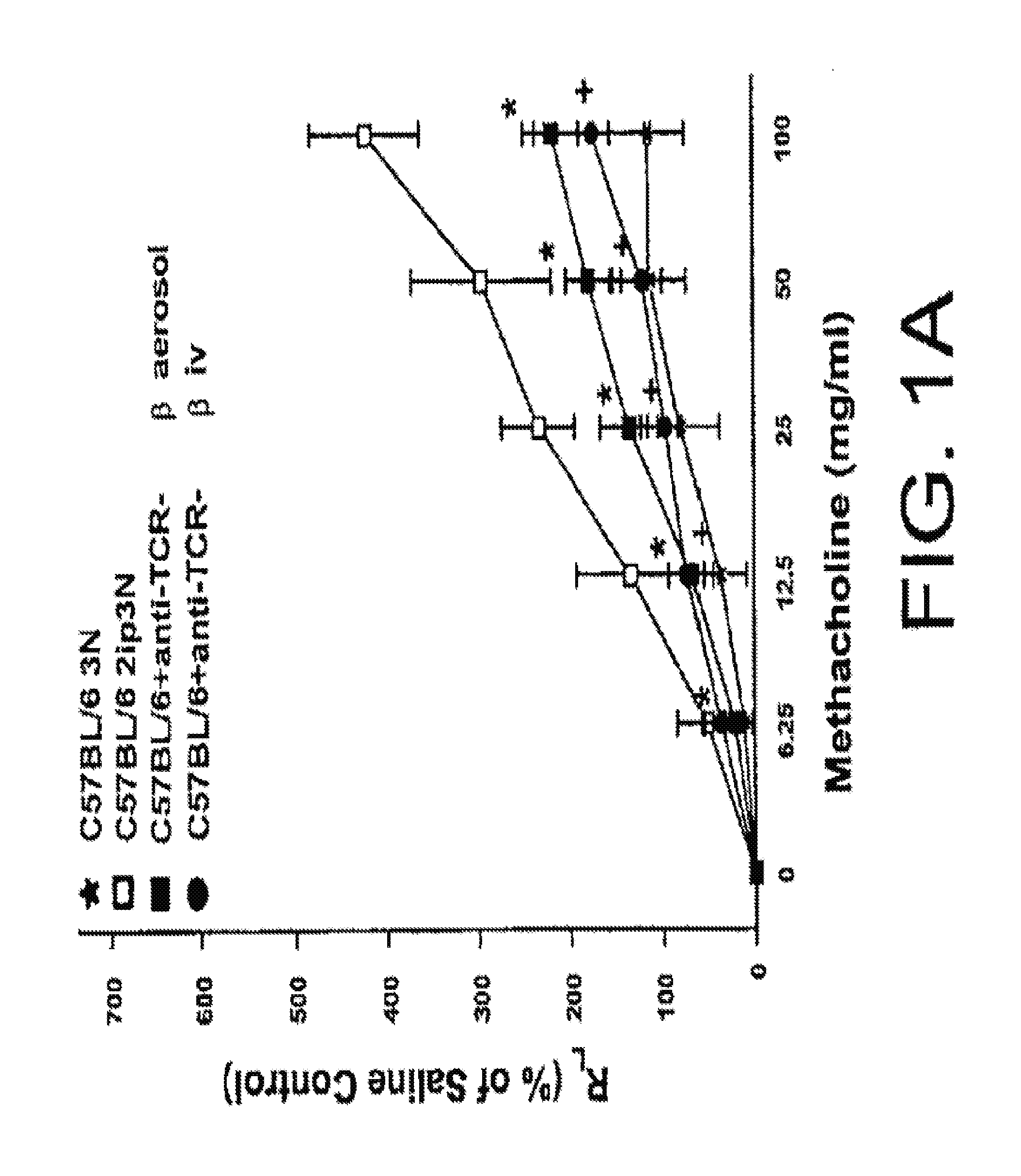
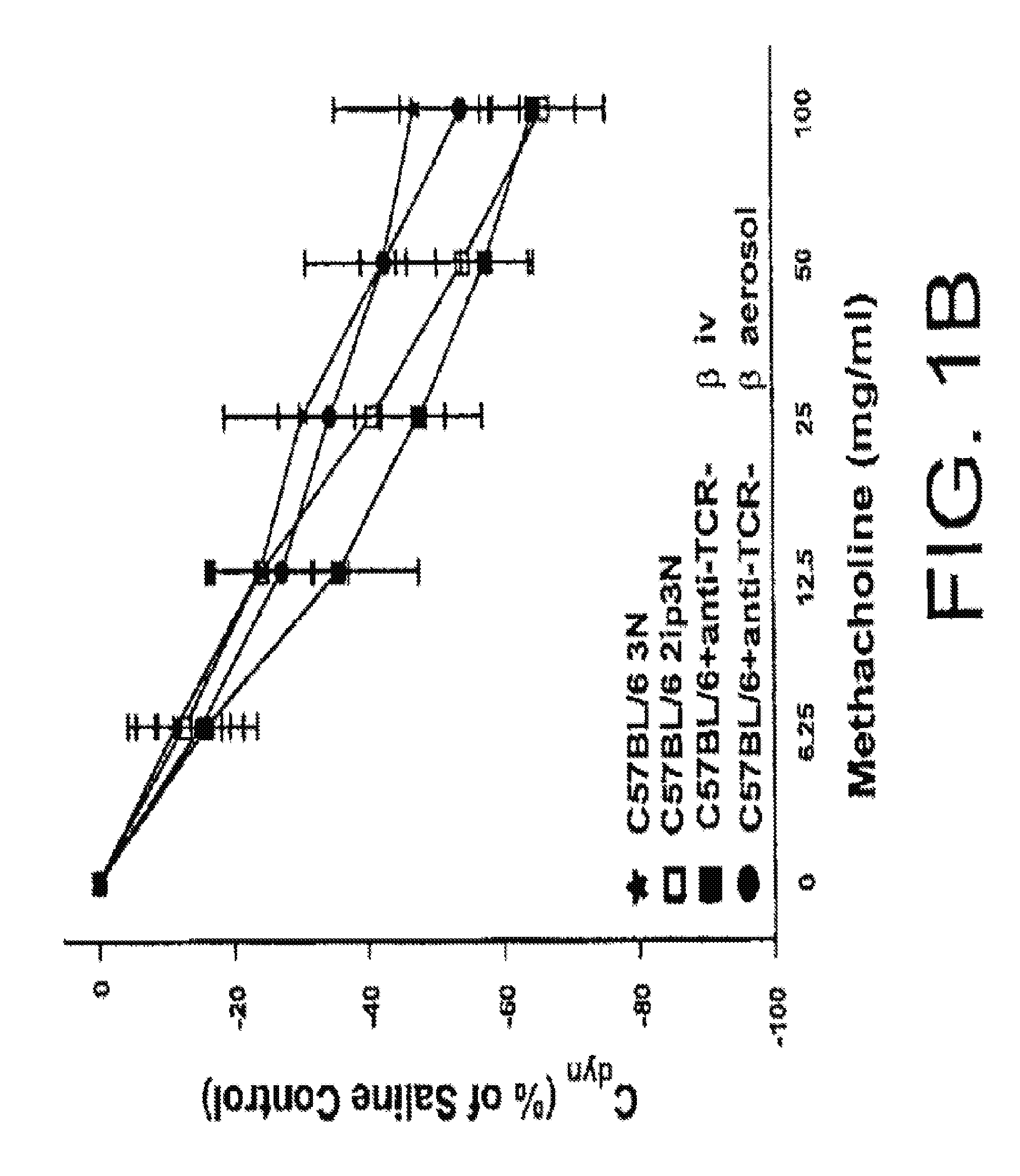
[0095]The following example describes the comparison of aerosolized versus intravenously given mAbs against TCR-β in ovalbumin (OVA) sensitized and challenged mice.
[0096]The classical animal model of allergic inflammation (see, e.g., Takeda et al., (1997). J. Exp. Med, 186, 449-454; Renz et al., 1992, J. Allergy Clin. Immunol. 89:1127-1138; Larsen et al., 1992, J. Clin. Invest. 89:747-752; and Saloga et al., 1993, J. Clin. Invest. 91:133-141) was used to assess the ability of aerosolized mAbs to influence AHR. The present inventors and others have previously shown that αβ T cells are necessary for the development of allergic inflammation and airway hyperresponsiveness (AHR) (Holt, J. Exp. Med. 183:1297-1301 (1996); Lahn et al., Nature Med. 5:1150-6 (1999)). In this experiment, C57BL / 6 mice were injected twice with Alum / OVA intraperitoneally (sensitization) before a three day exposure to aerosolized OVA (challenge). The exact procedure has been previously published (Lahn et al., Natu...
example 2
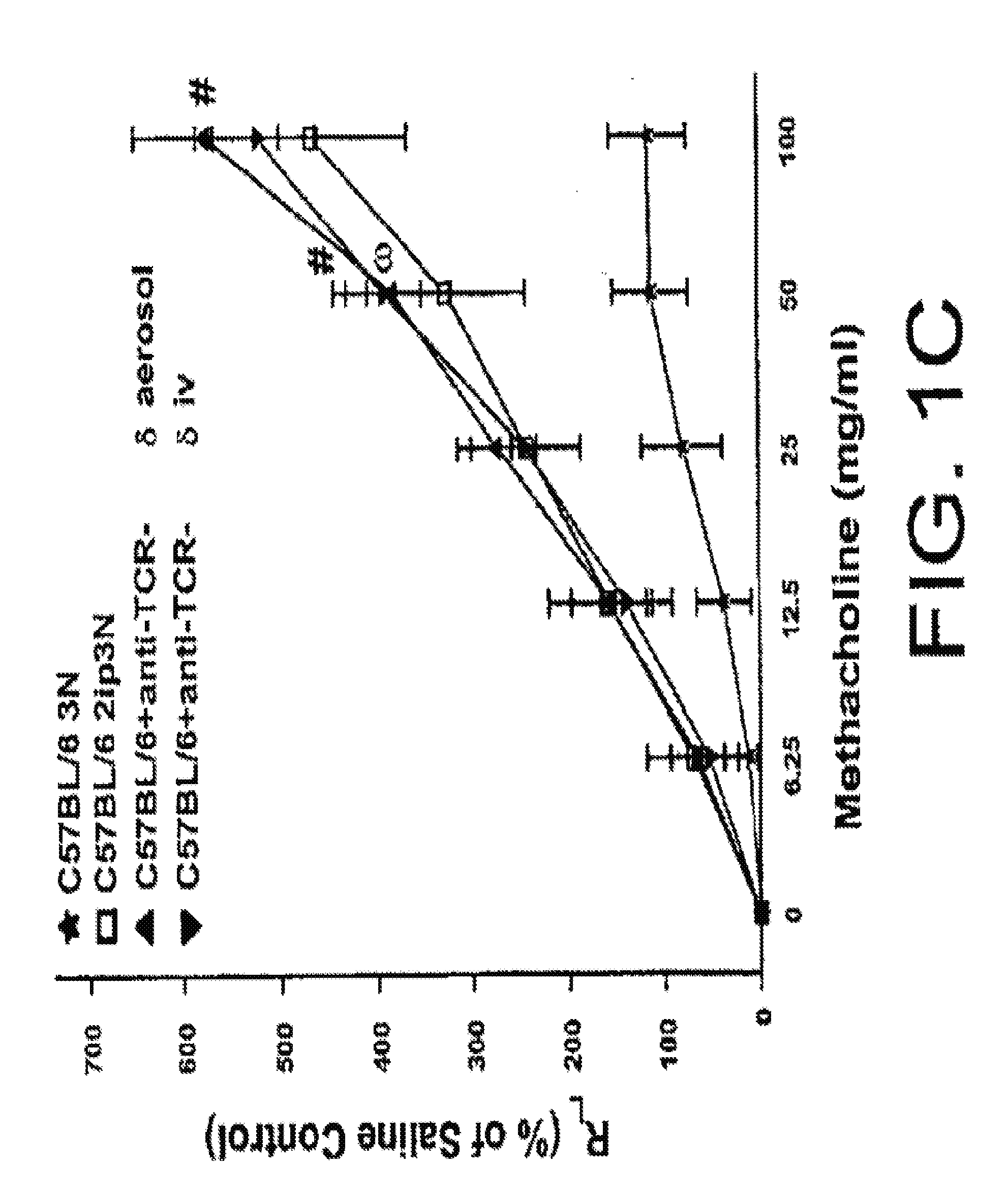
[0101]The following example describes the comparison of aerosolized versus intravenously given mAbs against TCR-δ in ovalbumin (OVA) sensitized and challenged mice.
[0102]In this example, experiments were conducted as described in Example 1, but with the use of a mAb against TCR-δ (a 1:1 mixture of mAbs GL3 (Goodman et al., J. Exp. Med. 170:1569 (1989)) and 403A10 Itohara et al., Proc. Natl. Acad. Sci. USA 86:5094-5098 (1989)). As previously published (Lahn et al., Nature Med. 5:1150-6 (1999)), the intravenous injection of mAbs against TCR-δ (▾ in FIGS. 1C and 1D) caused only a slight increase in AHR when compared to 2ip3N treated C57BL / 6 mice in the absence of antibody (□ in FIGS. 1C and 1D). The significant differences between 2ip3N treated mice and 2ip3N mice treated with i.v. anti-TCR-δ are shown by “ω” in FIG. 1C. Again, the addition of 10 μg / ml of anti-TCR-δ to the last OVA aerosol application (▴ in FIGS. 1C and 1D) had a similar effect as the intravenous injection of the same ...
example 3
[0103]The following example describes the comparison of aerosolized mAbs against TCR-Vγ1 and TCR-Vγ4 in ovalbumin (OVA) sensitized and challenged mice.
[0104]Finally, the γδ T cell subsets Vγ1 and Vγ4 were examined for their contribution to the regulation of AHR. Experiments were performed as described in Examples 1 and 2 above, but with the use of mAbs against γδ TCR subsets having Vγ1 or Vγ4.
[0105]The aerosol application of mAbs against Vγ1 showed a significant reduction in AHR of 2ip3N treated C57BL / 6 mice (top in FIGS. 1E and 1F). The significant differences between 2ip3N treated mice and 2ip3N treated mice with aerosol anti-Vγ1 are indicated by “τ” in FIGS. 1E and 1F). This result indicates that the removal of this particular subset of γδ T cells, which may be recruited during allergic inflammation to the lung, has a beneficial effect on regulating AHR associated with allergic inflammation. Thus, an aerosol of a particular subset of γδ T cells in humans, presumably the Vγ9 subs...
PUM
| Property | Measurement | Unit |
|---|---|---|
| body weight | aaaaa | aaaaa |
| body weight | aaaaa | aaaaa |
| body weight | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com