Tissue connector apparatus and methods
a technology of tissue connectors and connectors, which is applied in the field of tissue connector apparatus and methods, can solve the problems of difficulty in performing arterial replacement or bypass grafting, difficulty in constructing an arterial anastomosis, and almost a technical impossibility using minimally invasive techniques, so as to reduce the amount of surface area of the clip exposed, prevent obstruction of the surgeon's view, and facilitate the removal of the needle
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
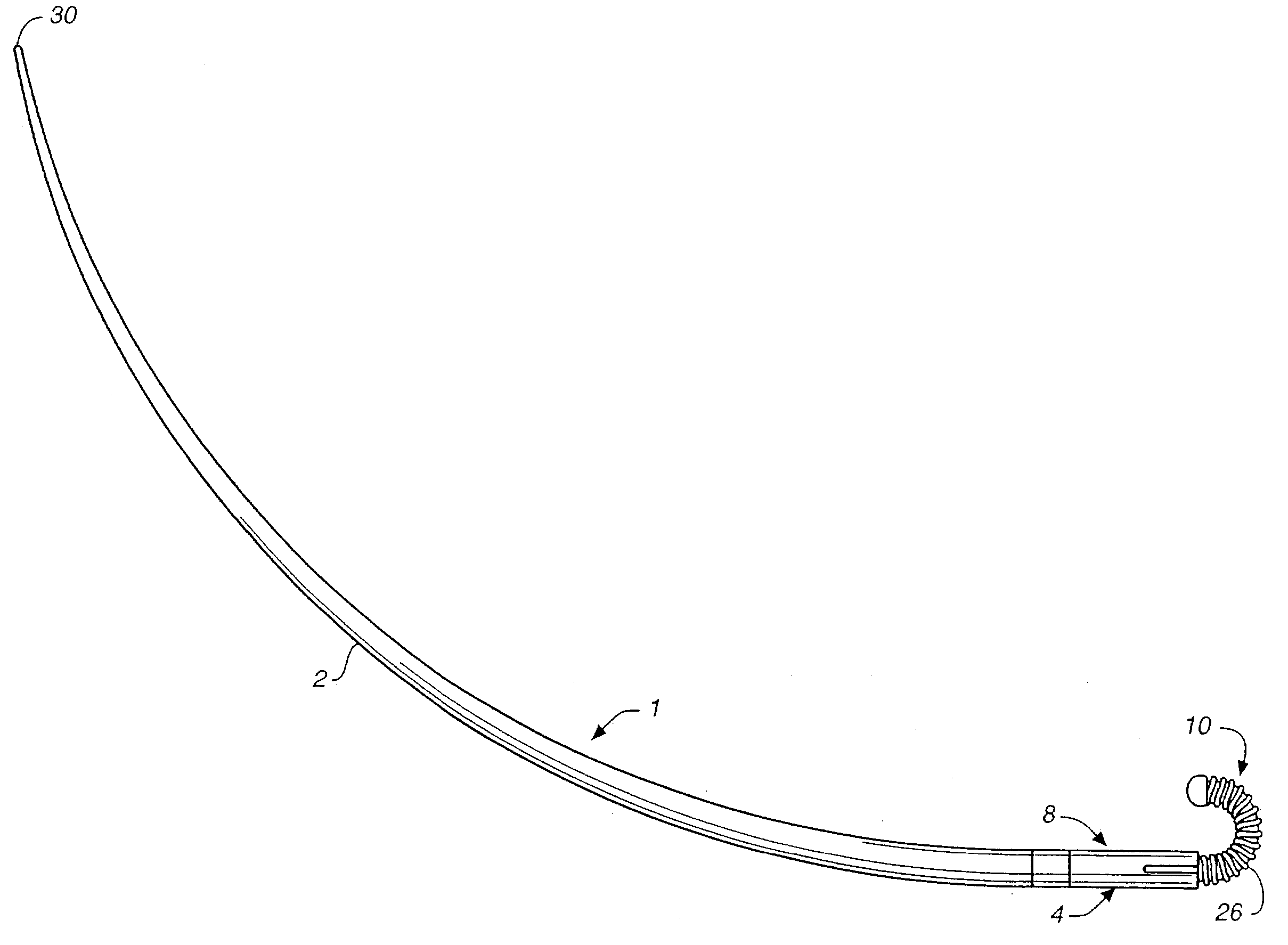
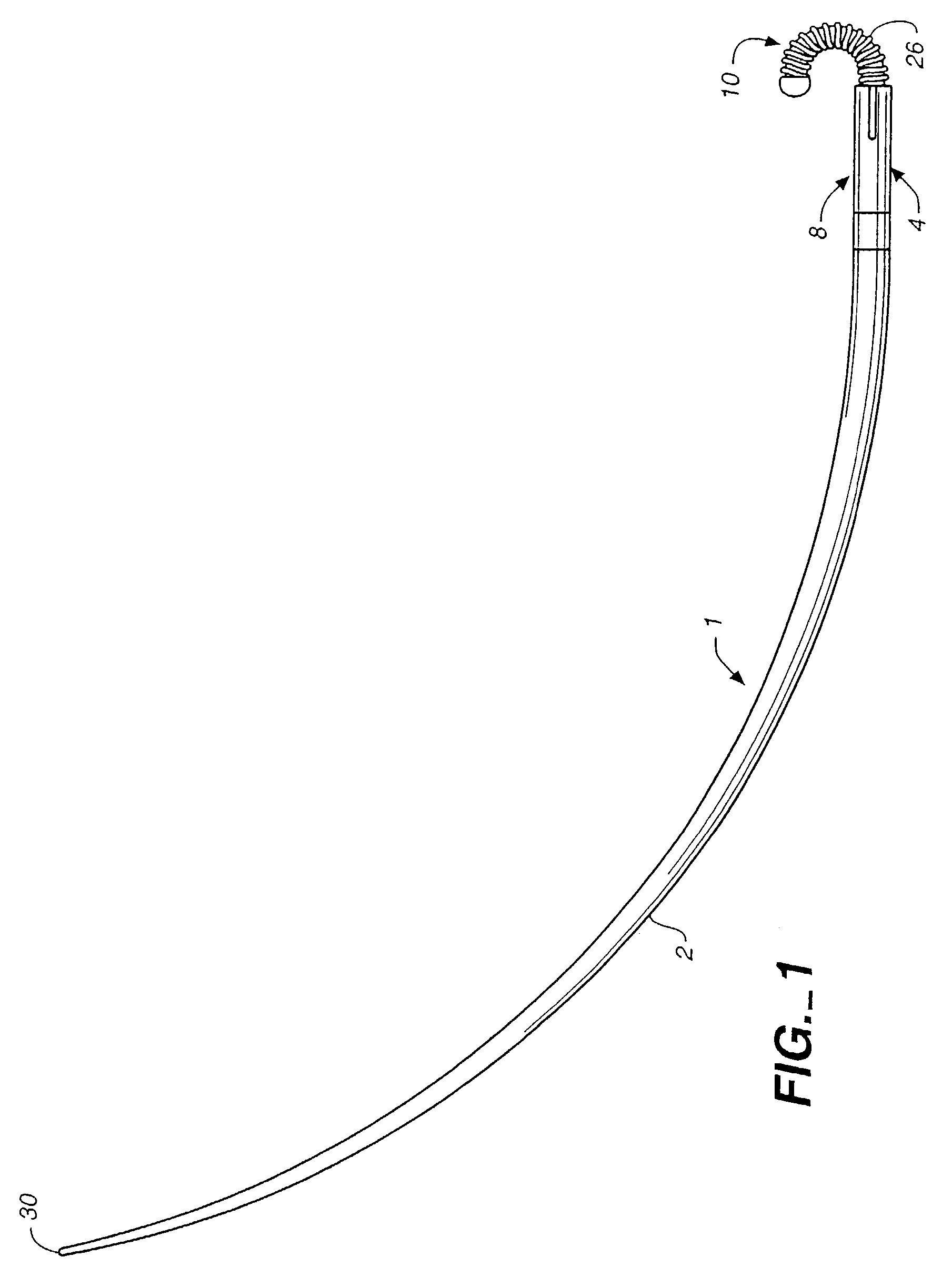
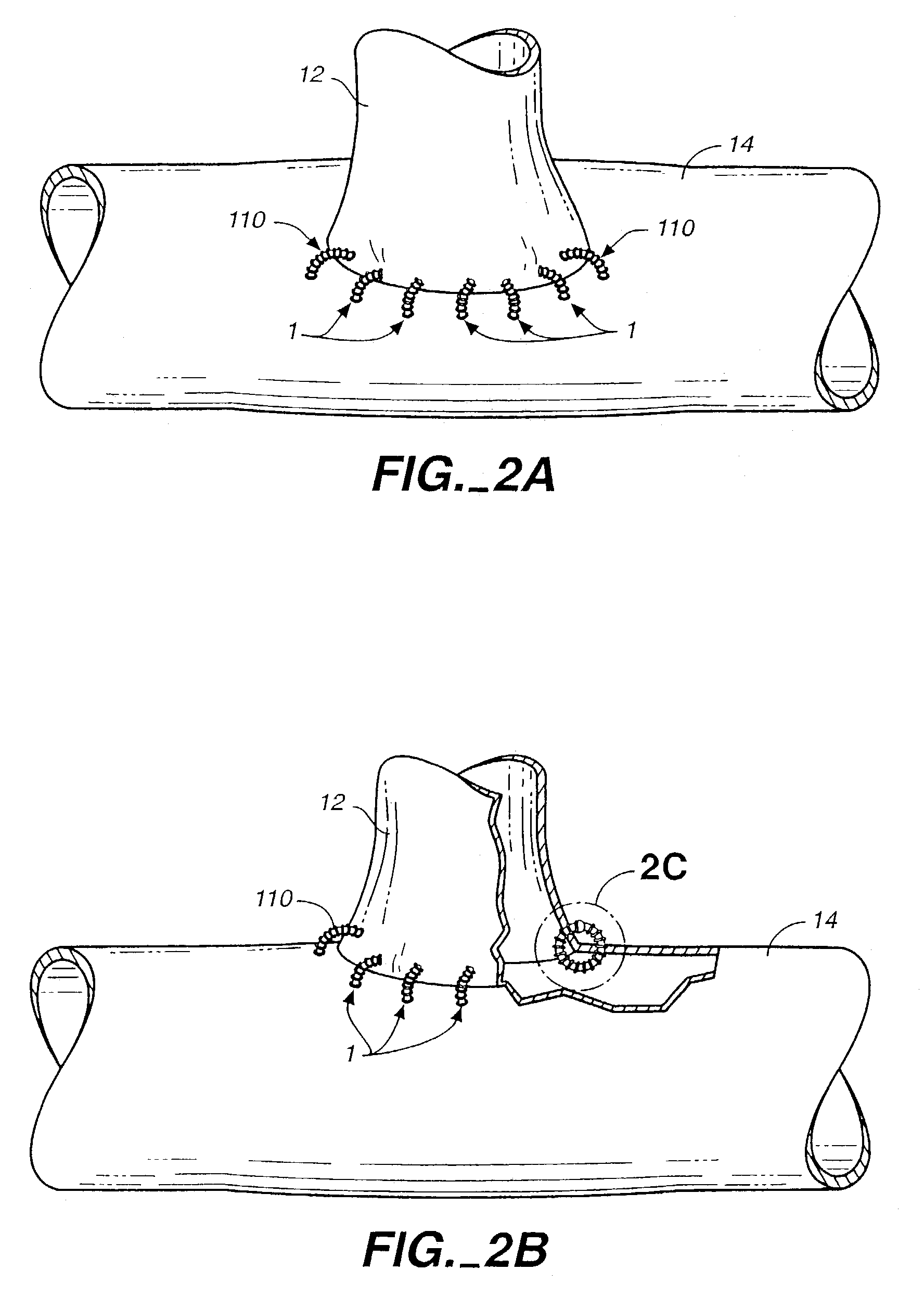
[0041]Referring now to the drawings, and first to FIG. 1, a tissue connector assembly constructed according to the principles of the present invention is shown and generally indicated with reference numeral 1. The tissue connector assembly 1 may be used to manipulate and align tissues, or tissue and graft with respect to each other and thereafter connect the tissues together (FIGS. 2A-2C). As used herein, the term graft includes any of the following: homografts, xenografts, allografts, alloplastic materials, and combinations of the foregoing. The tissue connector assembly 1 may be used in vascular surgery to replace or bypass a diseased, occluded, or injured artery by connecting a graft vessel 12 to a coronary artery 14 or vein in an anastomosis, for example. The tissue connector assembly 1 may be used in open surgical procedures or in minimally invasive or endoseopic procedures for attaching tissue located in the chest, abdominal cavity, or retroperitoneal space. These examples, ho...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com