System and Method for RF Ablation with Generated Images of Ablated Tissue Lesions
a tissue lesions and rfa technology, applied in the field of system and method for visualizing an rfa procedure, can solve the problems of inability to propagate nerve impulses, difficult for a practitioner to determine exactly where the ablation is carried out, and slight difference in tissue density
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
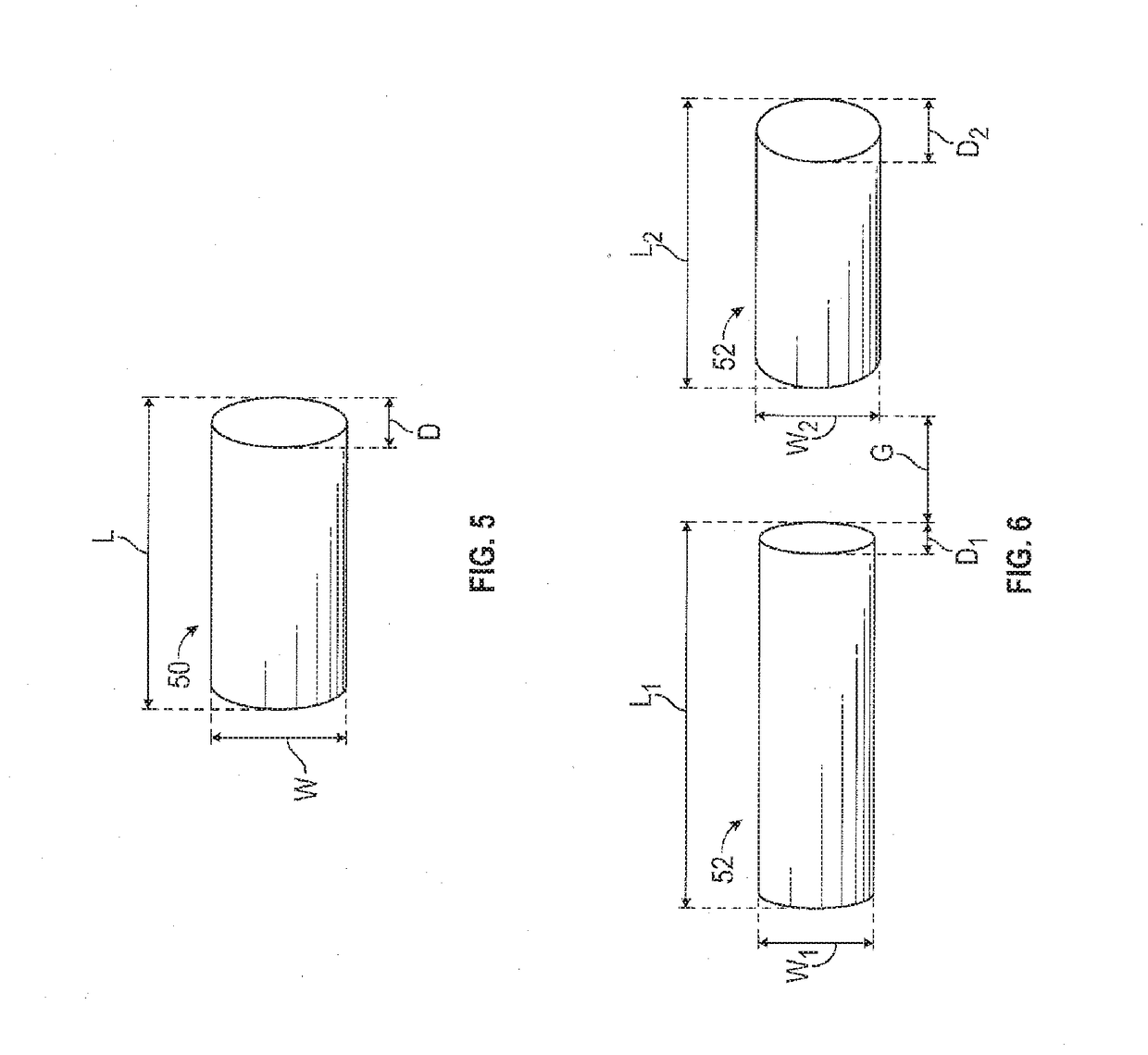
[0045]According to the system of the invention, the system produces virtual images of proposed and designated ablated tissue areas as oriented on a patient's anatomy. The virtual images include the size, shape, and location of ablated tissue areas for an RFA procedure. The virtual images may be supplemented with data such as a description of the size, shape and location of the ablated tissue areas.
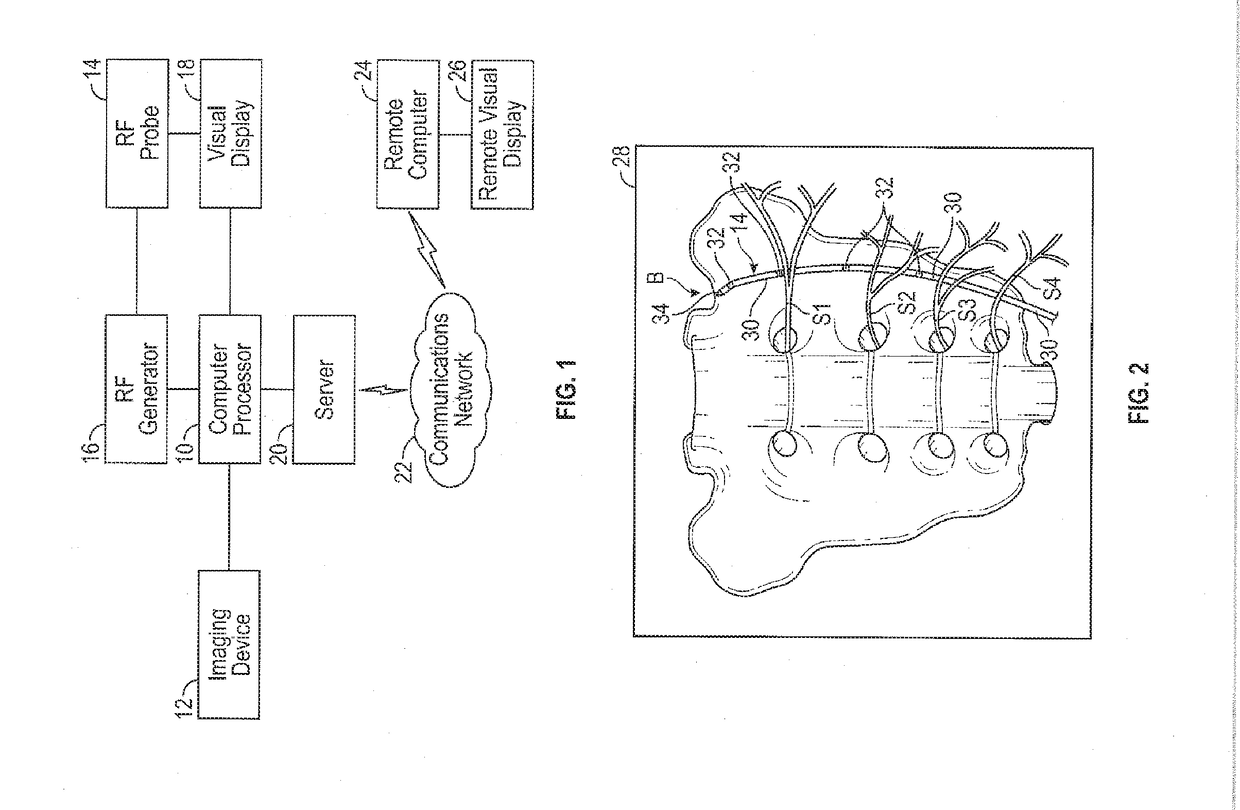
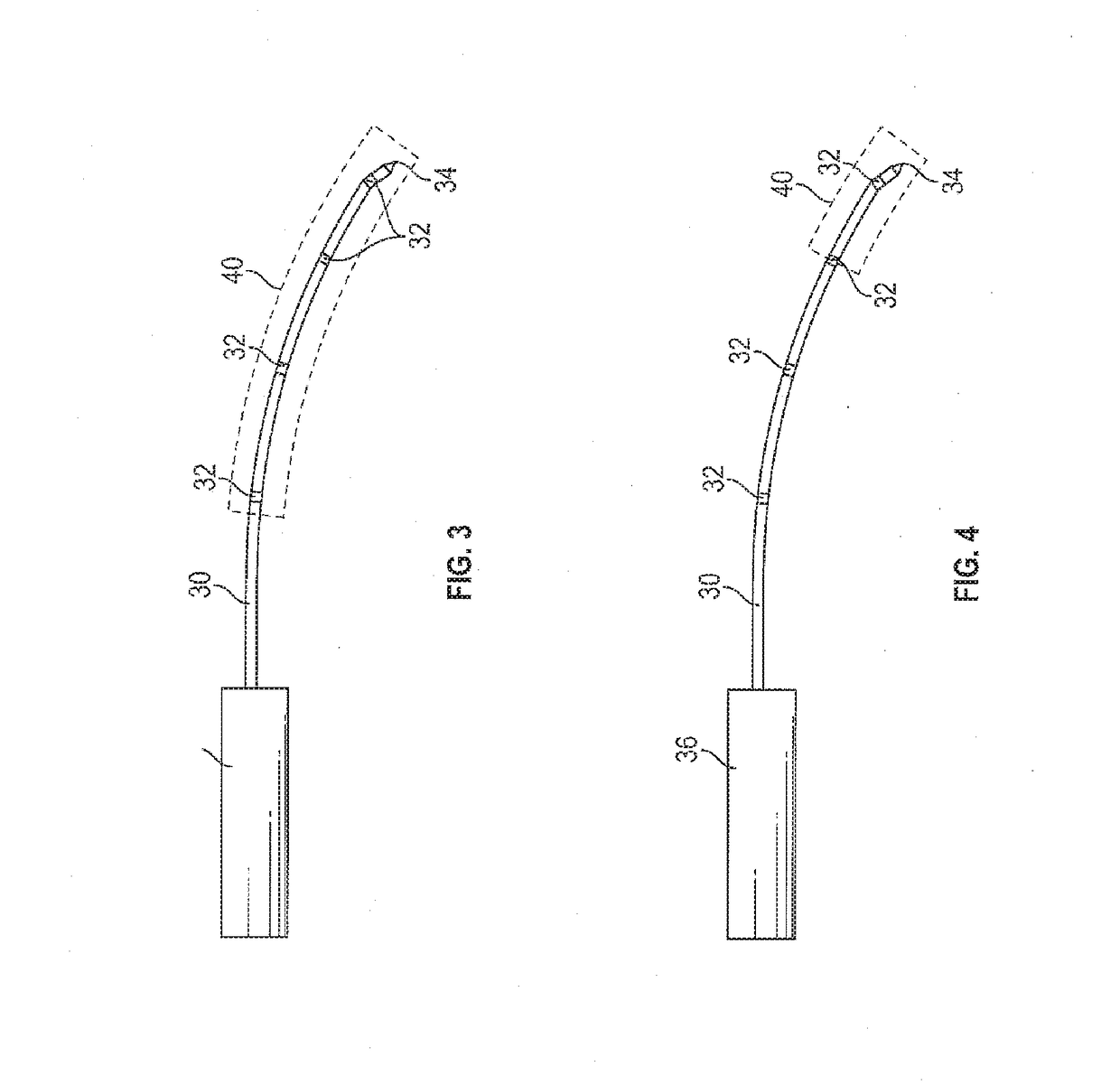
[0046]Referring to a first preferred embodiment as illustrated in FIG. 1, the system includes a computer processor 10 that communicates with an imaging source, such as an X-ray, CT, or ultrasound imaging device 12. The imaging device 12 provides real time images of a patient's anatomy where the RFA procedure takes place. A practitioner inserts and positions a RF probe 14, under imaging guidance, at the location where treatment is to occur. The energy supplied to the RF probe 14 is a RF generator 16 that has a plurality of settings that allows the practitioner to select the amount and durat...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com