Endovascular tissue removal device
a tissue removal and endovascular technology, applied in the field of endovascular aortic valve replacement, can solve the problems of inconvenient operation, inconvenient use, and inability to provide very precise cutting, and achieve the effect of eliminating the need for precise pressure control, reducing the need for resection, and high rotation ra
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
[0029] Aside from the preferred embodiment or embodiments disclosed below, this invention is capable of other embodiments and of being practiced or being carried out in various ways. Thus, it is to be understood that the invention is not limited in its application to the details of construction and the arrangements of components set forth in the following description or illustrated in the drawings.
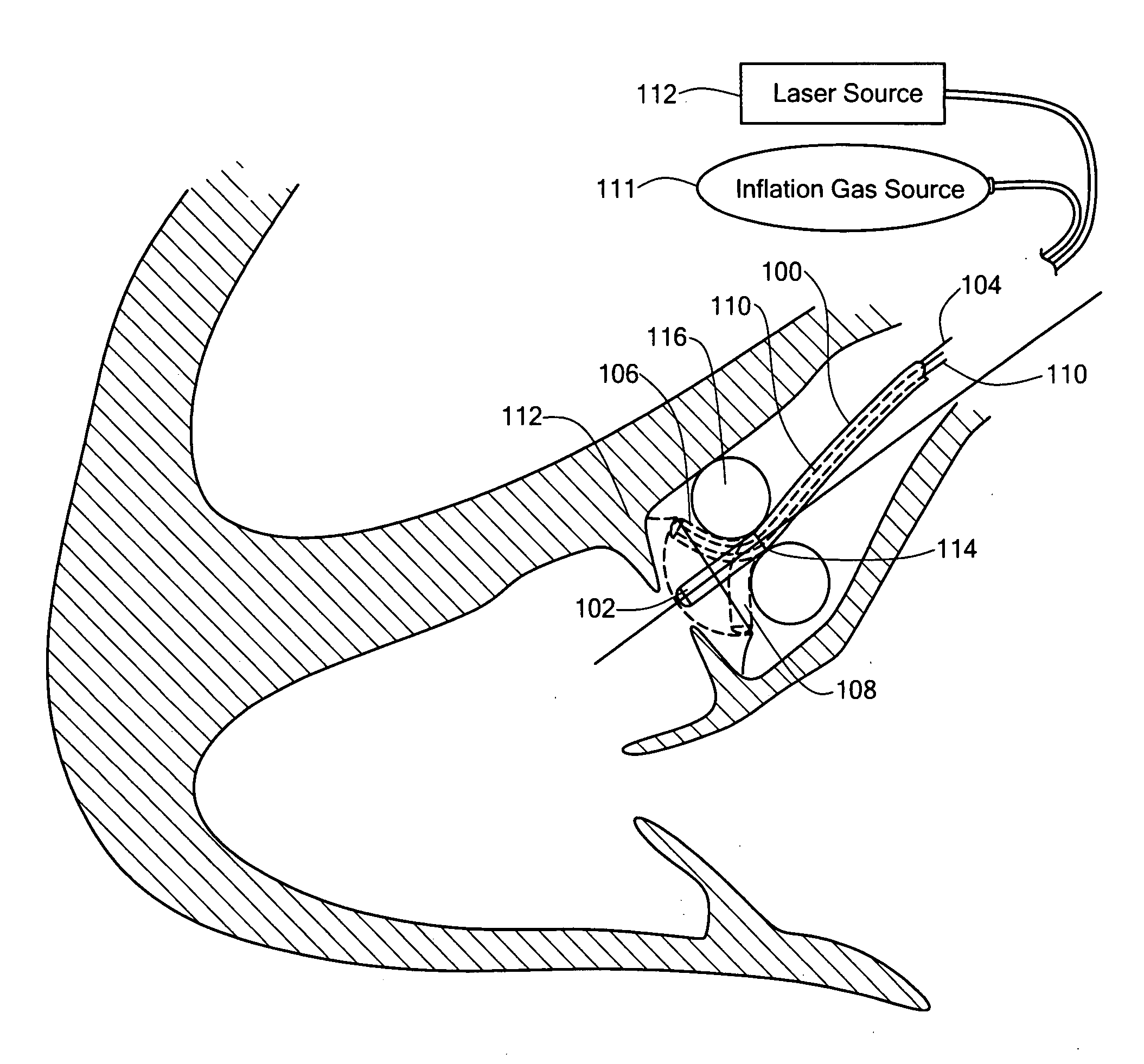
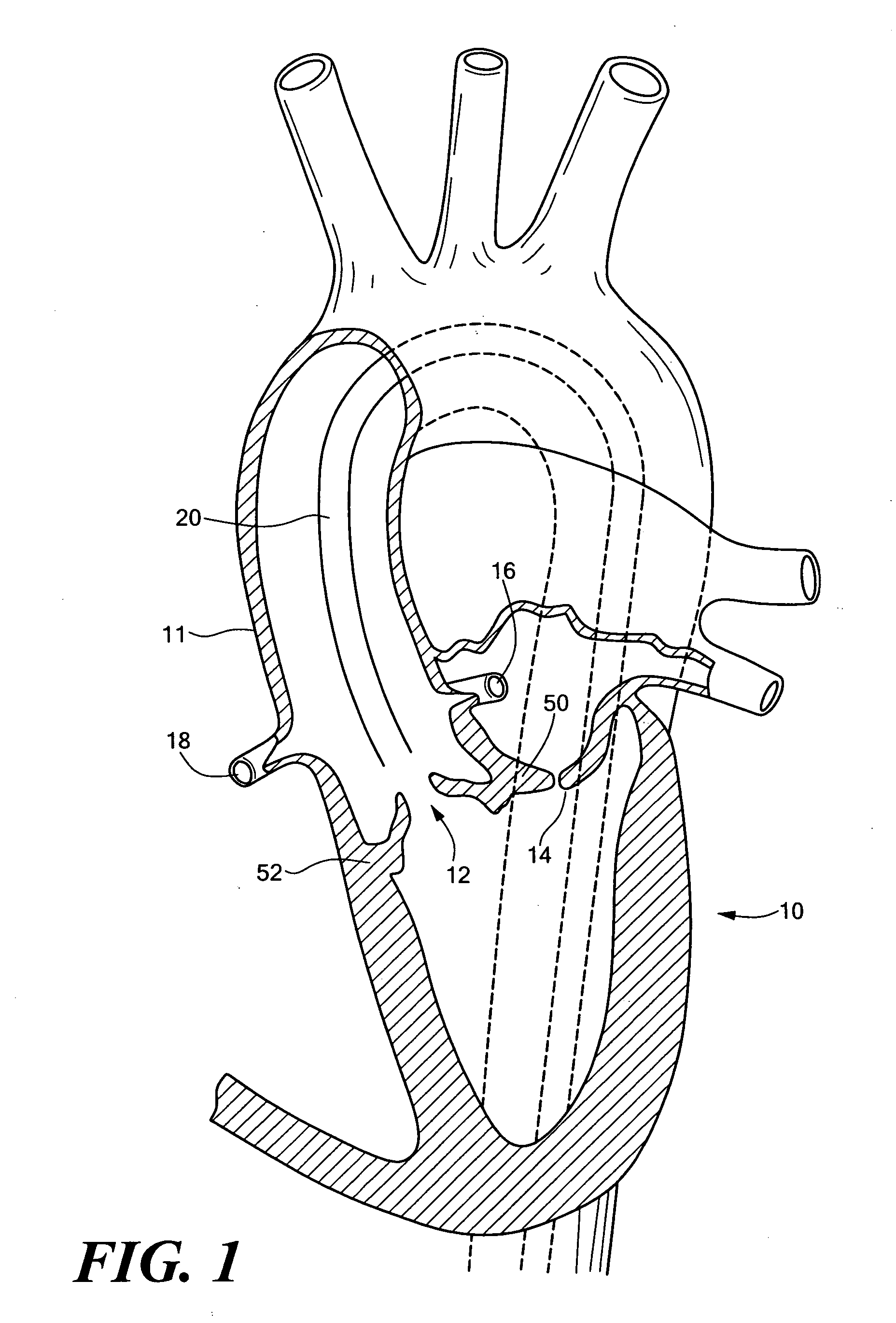
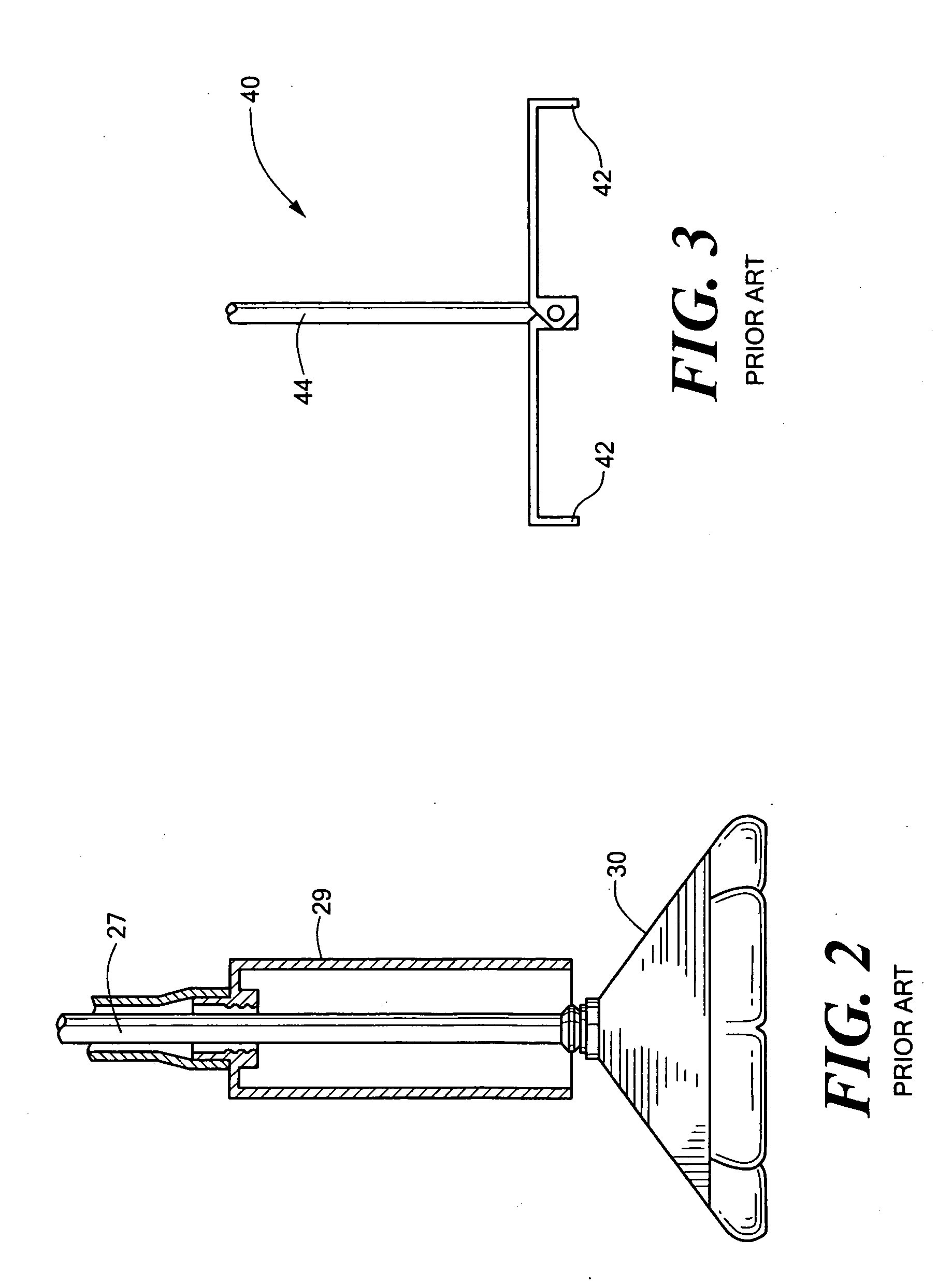
[0030]FIG. 1 schematically shows heart 10 with aorta 11, aortic valve 12, mitral valve 14, and coronary arteries 16 and 18. The idea behind percutaneous valve replacement surgery is to deliver a catheter 20 proximate valve 12 to resect it and to secure a replacement prosthetic valve in place. Resecting the native valve, however, is problematic. Those skilled in the art have devised inflatable barriers such as barrier 30, FIG. 2 used to trap tissue during resection. See also U.S. Pat. No. 6,287,321 and Published Patent Application No U.S. 2002 / 0095116 A1. Barrier 30 traps any tissue cut du...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com