Resectoscopic device and method
a technology of resectoscopic devices and methods, applied in the field of surgical devices, can solve the problems of increasing the risk of significant undesired tissue injury, reducing the ability to view what is happening with the instrument, and unplanned tissue injury,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
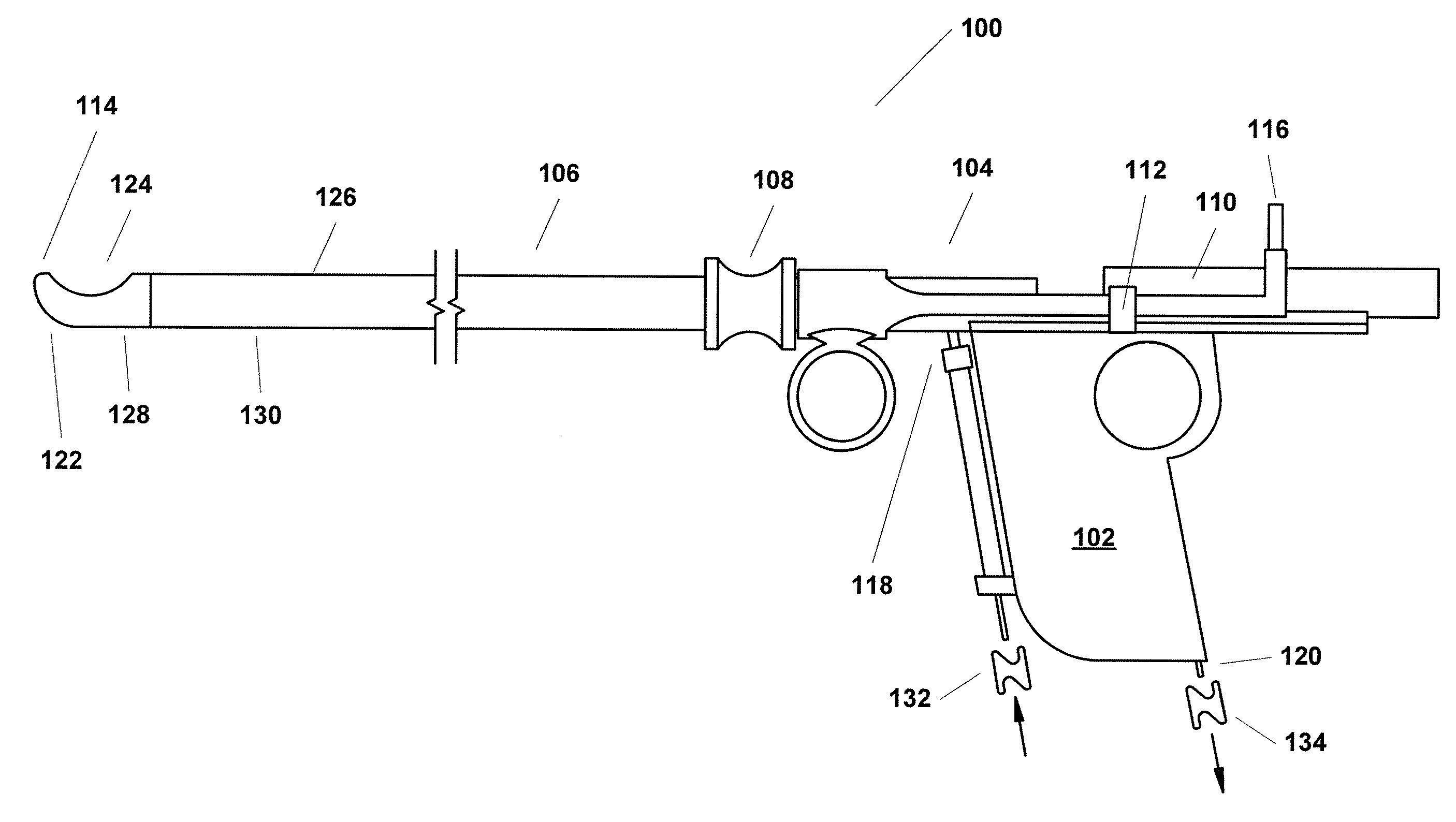
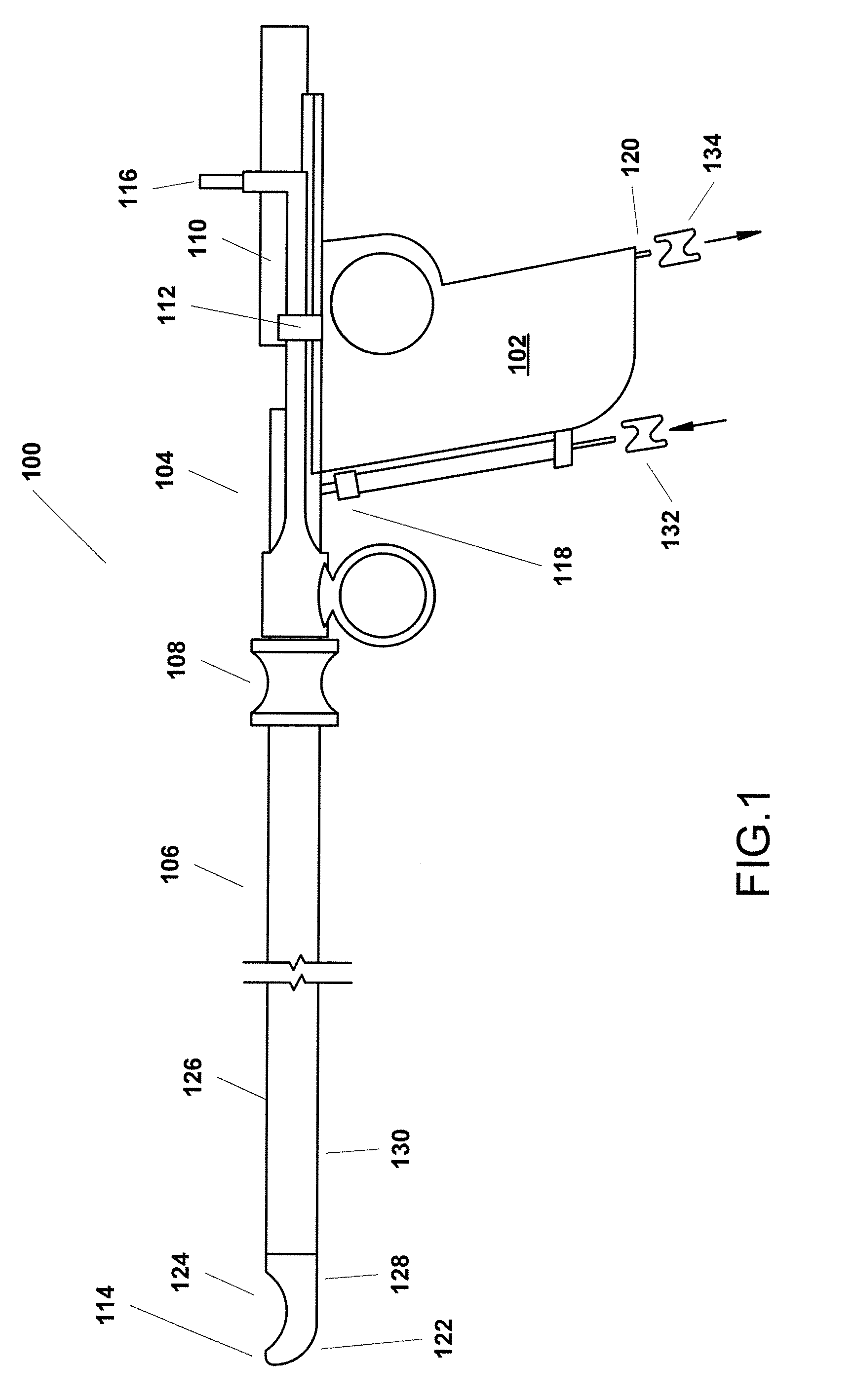
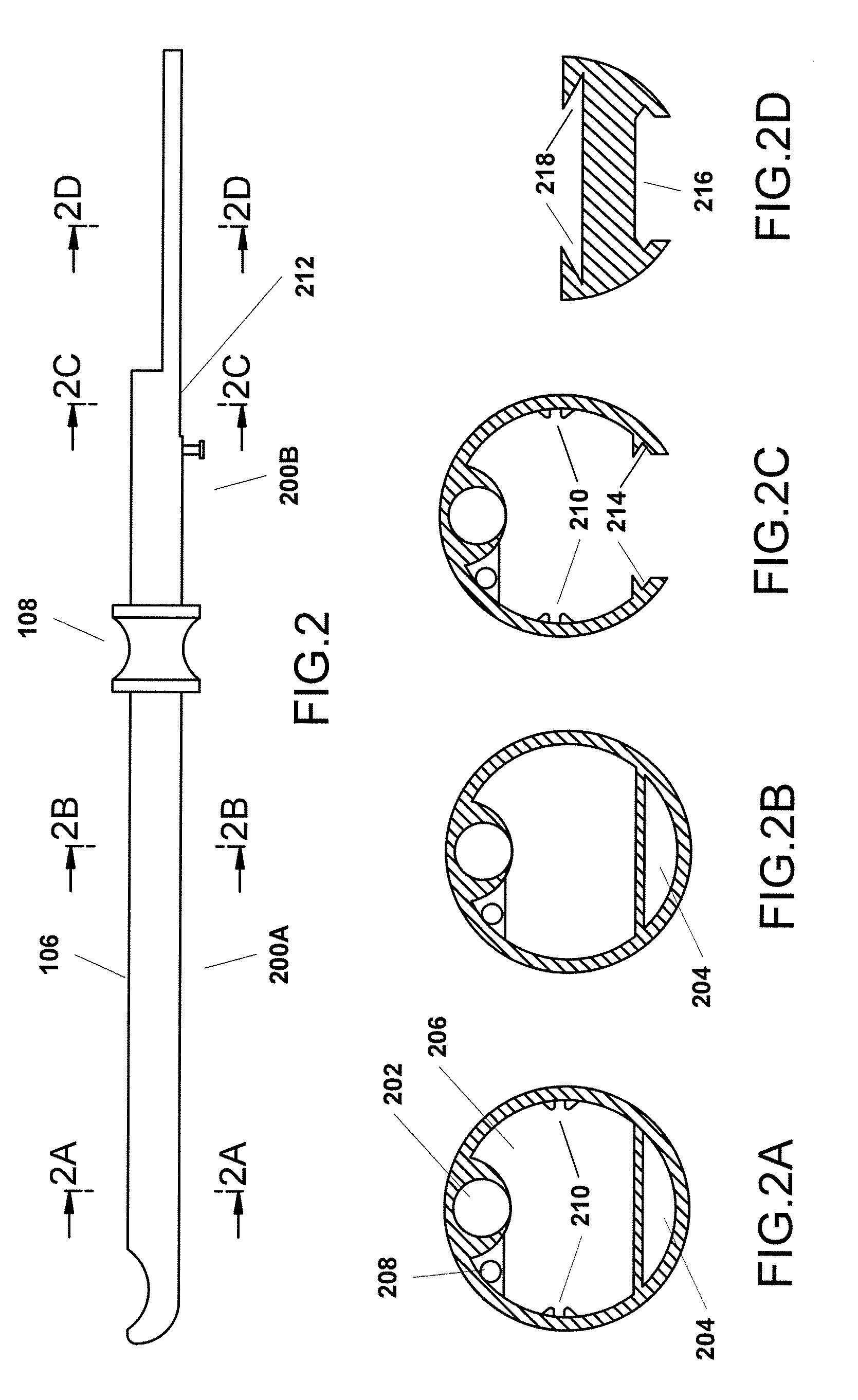
[0048]FIG. 1 is a simplified side view of one example variant of a resectoscope 100 incorporating the present invention. As shown in FIG. 1, this example resectoscope 100 is, in summary overview, made up of a partially hollowed out handle 102 and a control mechanism 104, both of which will be described in greater detail below, a shaft 106 connected at its proximal end to the handle 102, a port through which a telescope or other viewing apparatus, which may or may not involve use of fiber optic technology can be inserted (not shown), and a finger grip 108 on the shaft 106. The resectoscope 100 further includes a trolley mechanism 110 that facilitates movement of the telescope or other viewing apparatus that is contained within the shaft, a stop 112 that acts as a handle to allow manipulation of the trolley 110 and also limits movement of the trolley 110 mechanism towards the distal end 114 of the shaft, a power connector 116, a fluid inlet 118 and a vacuum port / fluid outlet 120. As c...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com