Fixed length anchor and pull mitral valve device and method
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
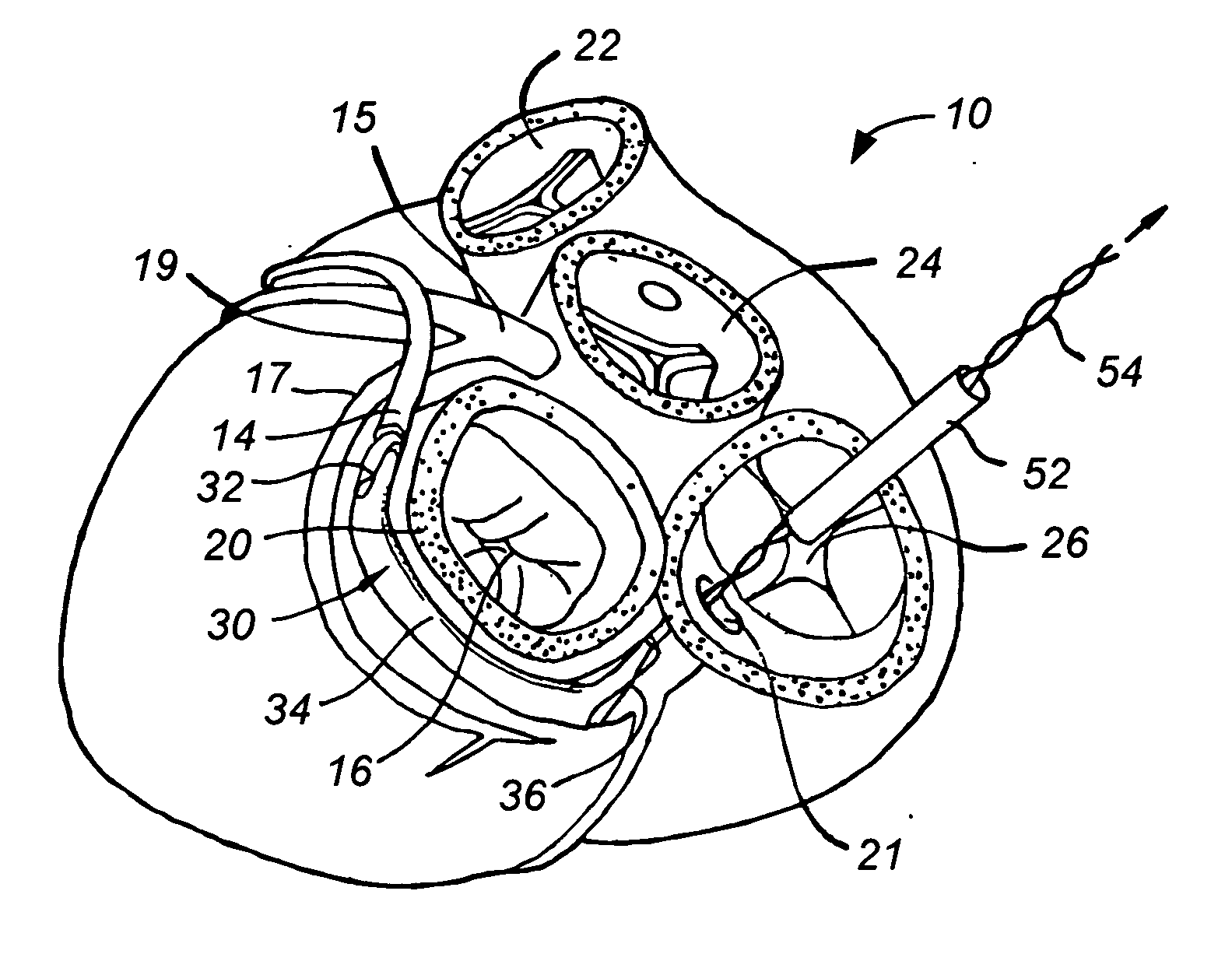
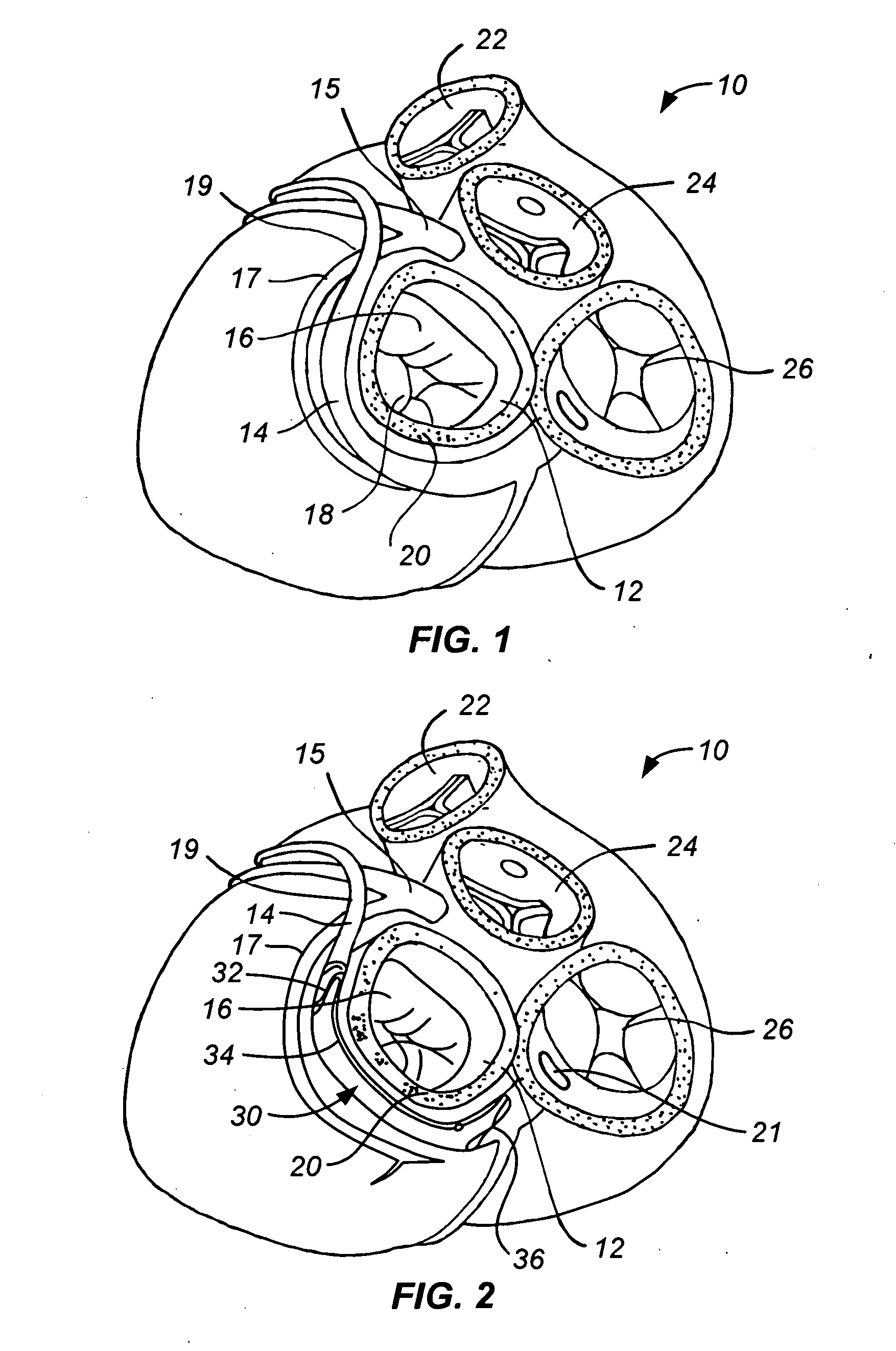
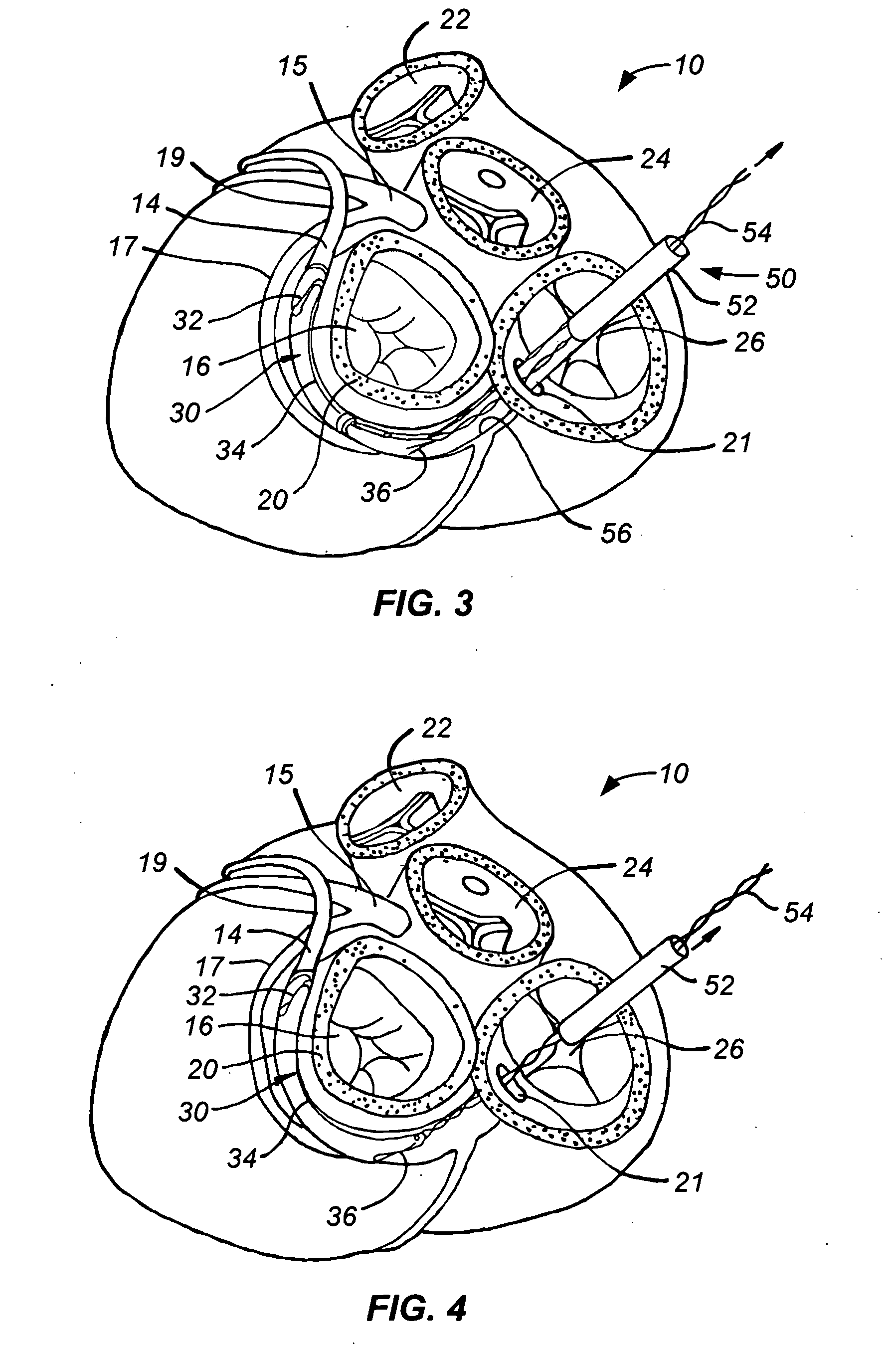
[0034] Referring now to FIG. 1, it is a superior view of a human heart 10 with the atria removed to expose the mitral valve 12, the coronary sinus 14, the coronary artery 15, and the circumflex artery 17 of the heart 10 to lend a better understanding of the present invention. Also generally shown in FIG. 1 are the pulmonary valve 22, the aortic valve 24, and the tricuspid valve 26 of the heart 10.
[0035] The mitral valve 12 includes an anterior cusp 16, a posterior cusp 18 and an annulus 20. The annulus encircles the cusps 16 and 18 and maintains their spacing to provide a complete closure during a left ventricular contraction. As is well known, the coronary sinus 14 partially encircles the mitral valve 12 adjacent to the mitral valve annulus 20. As is also known, the coronary sinus is part of the venous system of the heart and extends along the AV groove between the left atrium and the left ventricle. This places the coronary sinus essentially within the same plane as the mitral va...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com