System for tissue cavity closure
a tissue cavity and tissue technology, applied in the field of tissue cavity closure systems, can solve the problems of significant bleeding, inability to adequately create the desired suture stitch, abrasion and trauma between the metallic staple and the soft tissue surface, etc., to achieve less invasive treatment, prevent tissue expansion, and reduce the volume of the atria
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
embodiment 109
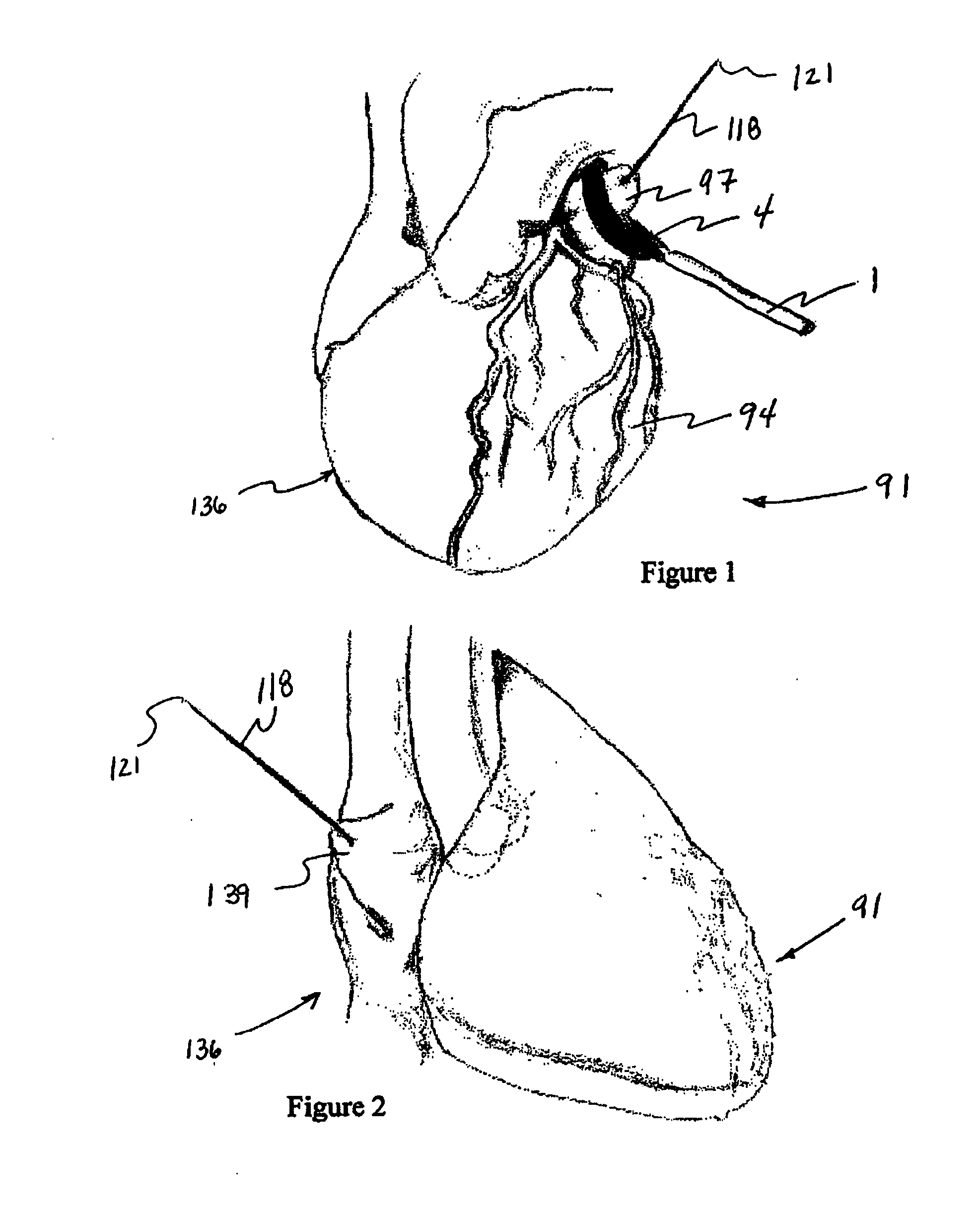
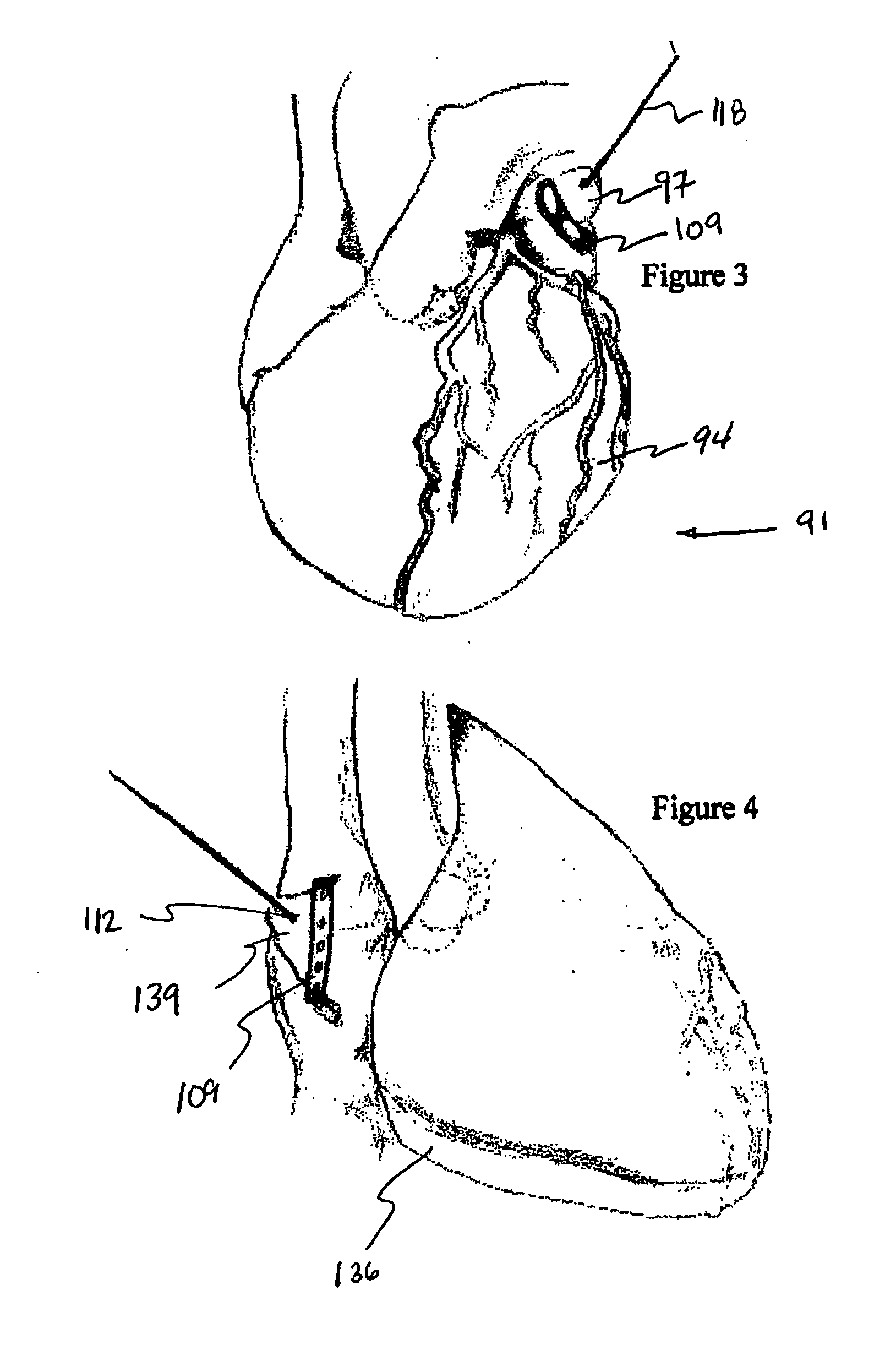
[0040]FIG. 3 shows a side view of heart 91 that contains pledgeted stitch 109 isolating left atrial appendage 97 by juxtaposing opposing endocardial walls of left atrium 94 between two reinforced pledgets 109 such that clots within and the trabeculated interior surface of the left atrial appendage is separated from blood flow. In addition, left atrial volume is significantly reduced. Each suture strand 118 extends from outside the first reinforced pledget where continuous length of strand 115 defines an anchor, through an opening or puncture site in the first reinforced pledget, through the juxtaposed atrial walls, through an opening or puncture site in the second reinforced pledget, and outside the second reinforced pledget where suture strand free ends are tied into a knot or otherwise anchored to prevent relaxation of tightened stitch 112. Once the stitch is tightened, the reinforced pledgets are positioned intimately against the epicardial surfaces of the left atrial appendage a...
embodiment 1
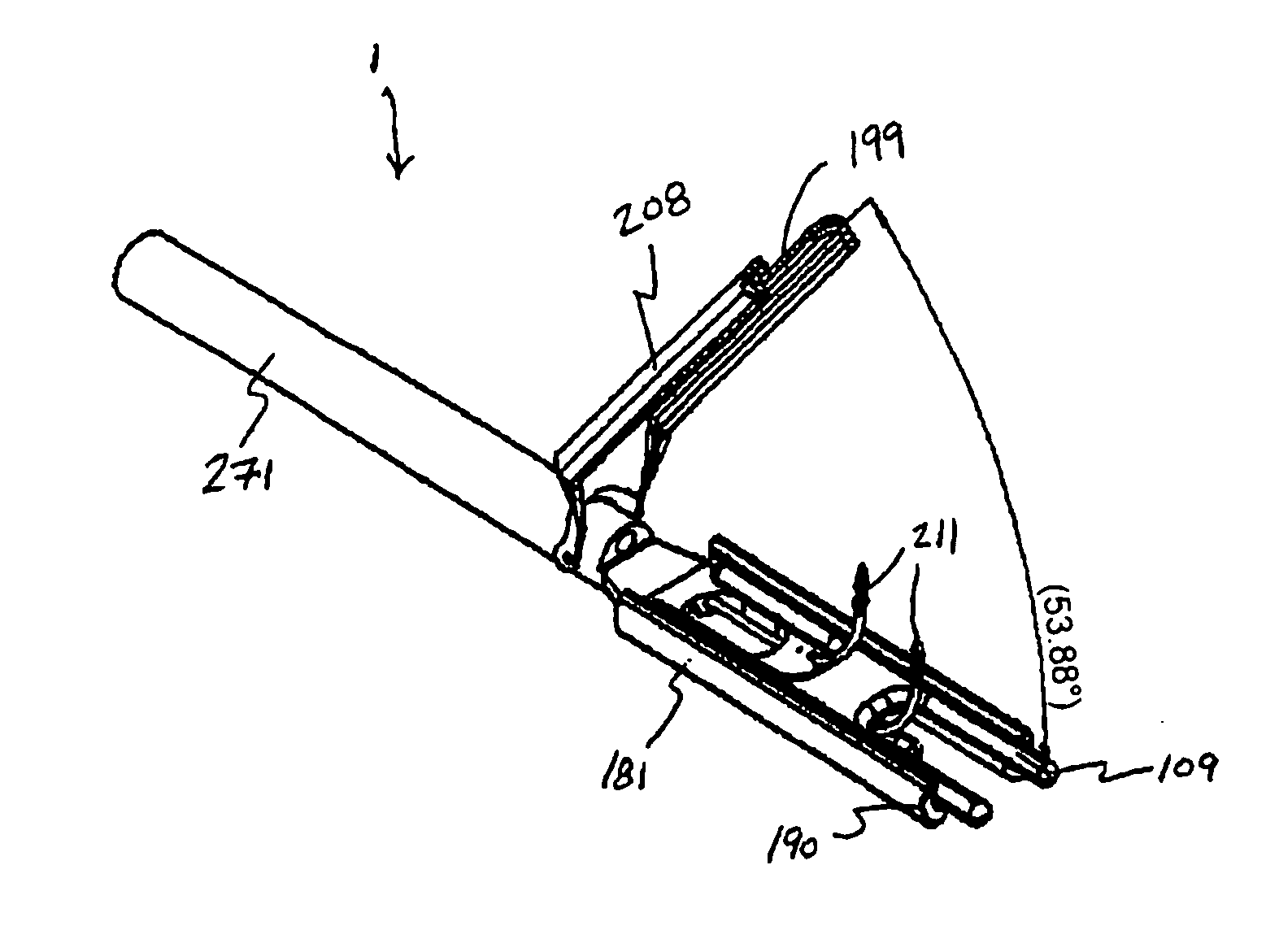
[0042] In embodiment 1 in FIGS. 5A to 5D and FIGS. 6A to 6C, appendage isolation grasper 1 is shown with single reinforced pledget 109 housed in lower jaw 181 (upper jaw 208 does not show a reinforced pledget purely for illustration purposes; in practice the upper jaw may or may not contain a reinforced pledget, depending on the application), and two resilient (or deformable) needles 211. FIGS. 5A to 5D show the grasper with the jaws in a closed orientation and with two resilient (or deformable) needles fully deployed. FIGS. 6A to 6C show the grasper with the upper jaw in an open orientation.
[0043] Appendage isolation grasper 1 incorporates two lumens into which the needles are compressed into a low profile for insertion through trocar, cannulae, or introducer. Lower jaw 181 incorporates two separate channels 190 associated with confining lumens and containing exit points 195 through which needles 211 pass. The lower jaw channels are curved to guide / direct the needles upward through...
embodiment 451
[0056]FIGS. 11A to 11C show a perspective view, a top view and a side view of another reinforced pledget embodiment 451. This reinforced pledget embodiment incorporates two openings 454 separated by an axially oriented central link 457 and defining spaces through a support structure 463 through which suture strand free ends 121 are advanced using actuated needles 211 of appendage isolation system 1. The length (“I2”) of the central link is chosen based on the distribution requirements. As the flattened profile increases, the length of the central link is increased to accommodate the desire to distribute the forces along a greater length. The openings through the support structure match channel exit point spacing 193 for the grasper.
[0057]FIGS. 12A to 12C show a perspective view, a top view and a side view of a reinforced pledget embodiment 496. This reinforced pledget embodiment is fabricated from a resilient polymer through which suture strand free ends 121 can be advanced using ac...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com