Electromyography system
a technology of electromyography and nerve detection, applied in the field of electromyography, can solve the problems of increasing the danger of inadvertent contact and/or severing of the nerve of the patient, difficult to avoid inadvertent contact with the nerve, and reducing the visibility of the patient's tissues, so as to improve the accuracy of nerve detection warnings, reduce the risk of nerve contact, and improve the likelihood of nerve conta
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
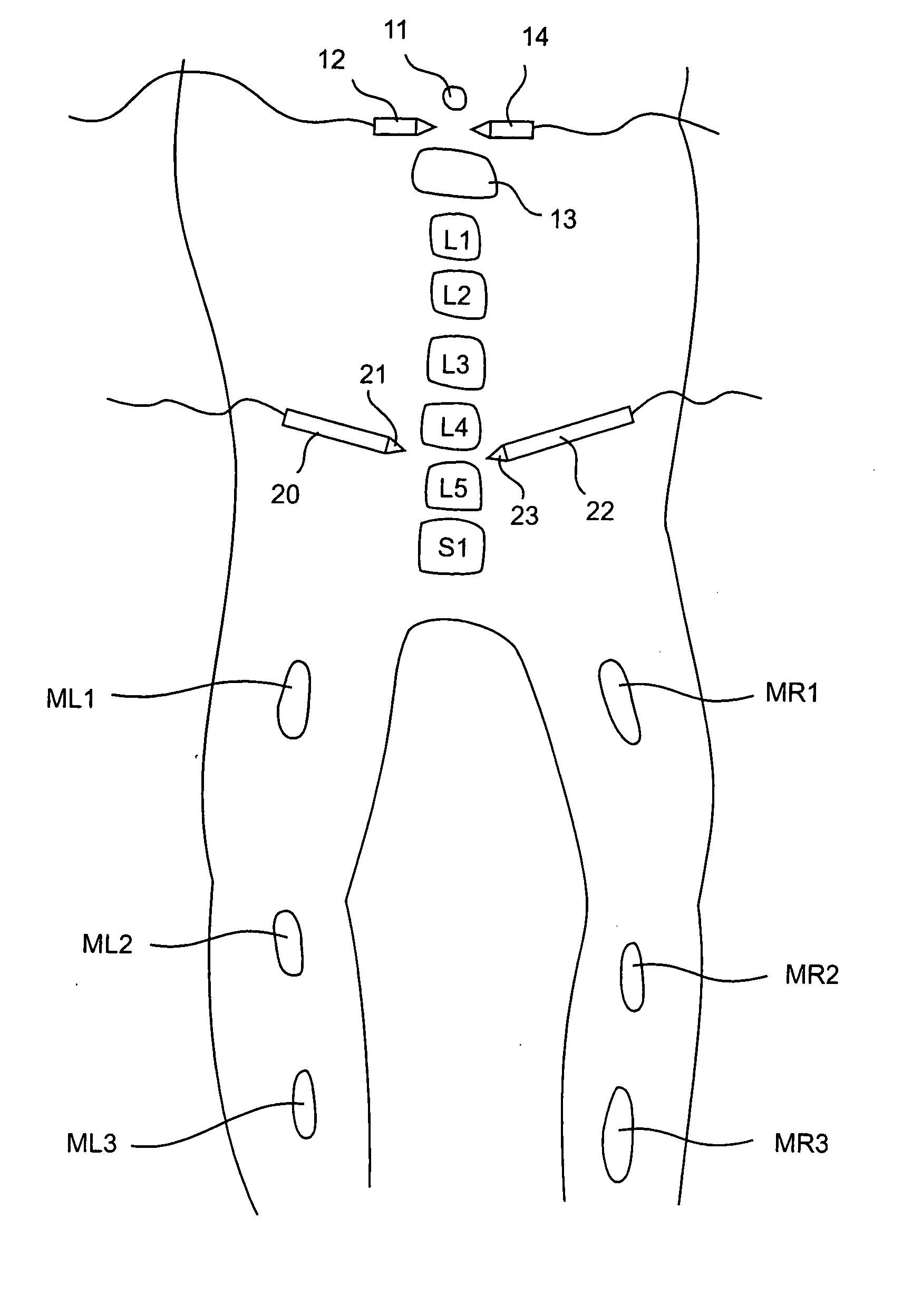
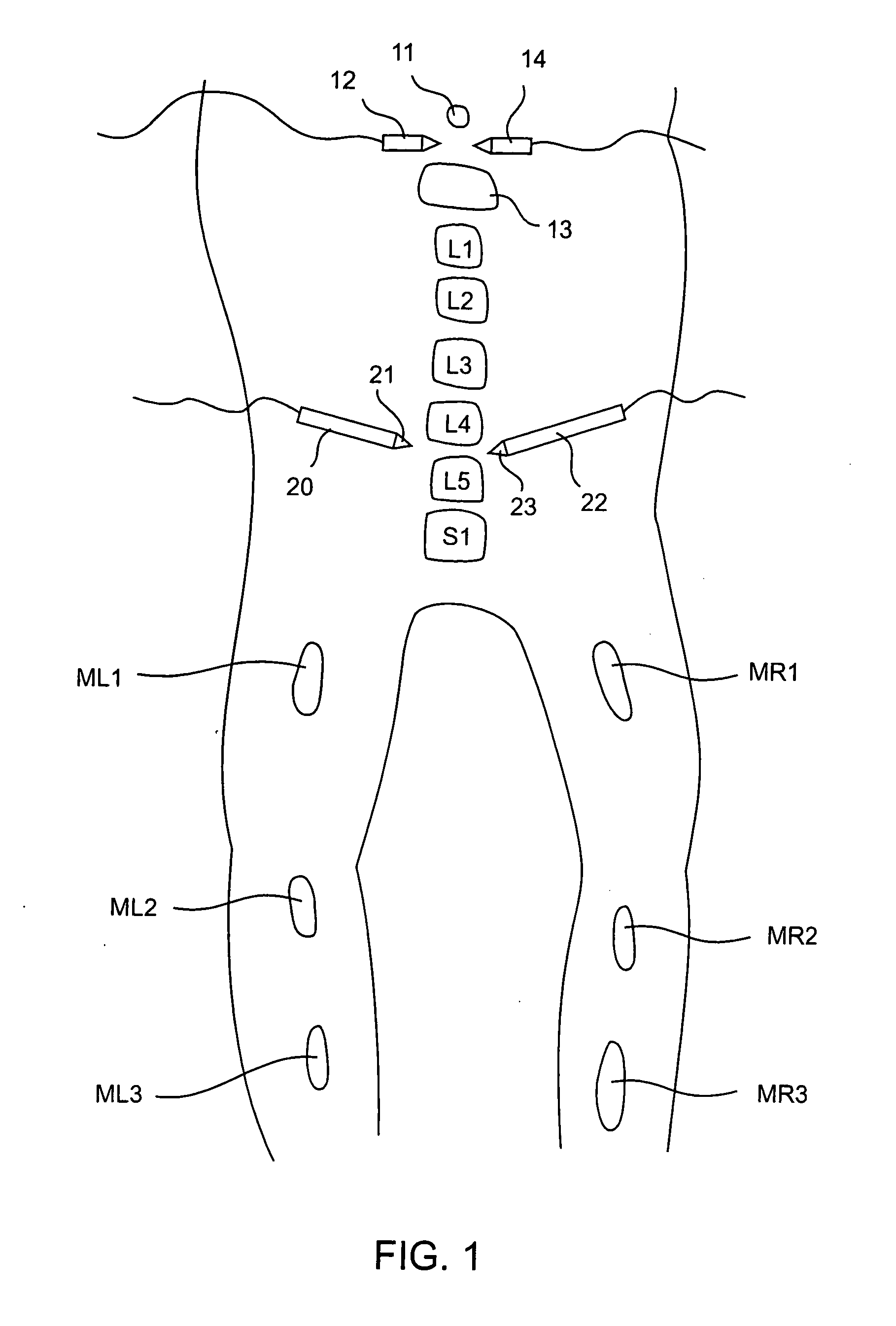
[0047] The present invention sets forth systems for detecting when a nerve is near or adjacent to an electrified surgical tool, probe, cannula, or other surgical instrument. The present invention also involves optional systems for simultaneously determining the “status” (e.g.: sensitivity) of a plurality of nerves.
[0048] As will be explained, the present system involves applying a signal with a current level to a probe near a nerve and determining whether an electromyographic “EMG” (i.e.: neuro-muscular) response for a muscle coupled to the nerve is present.
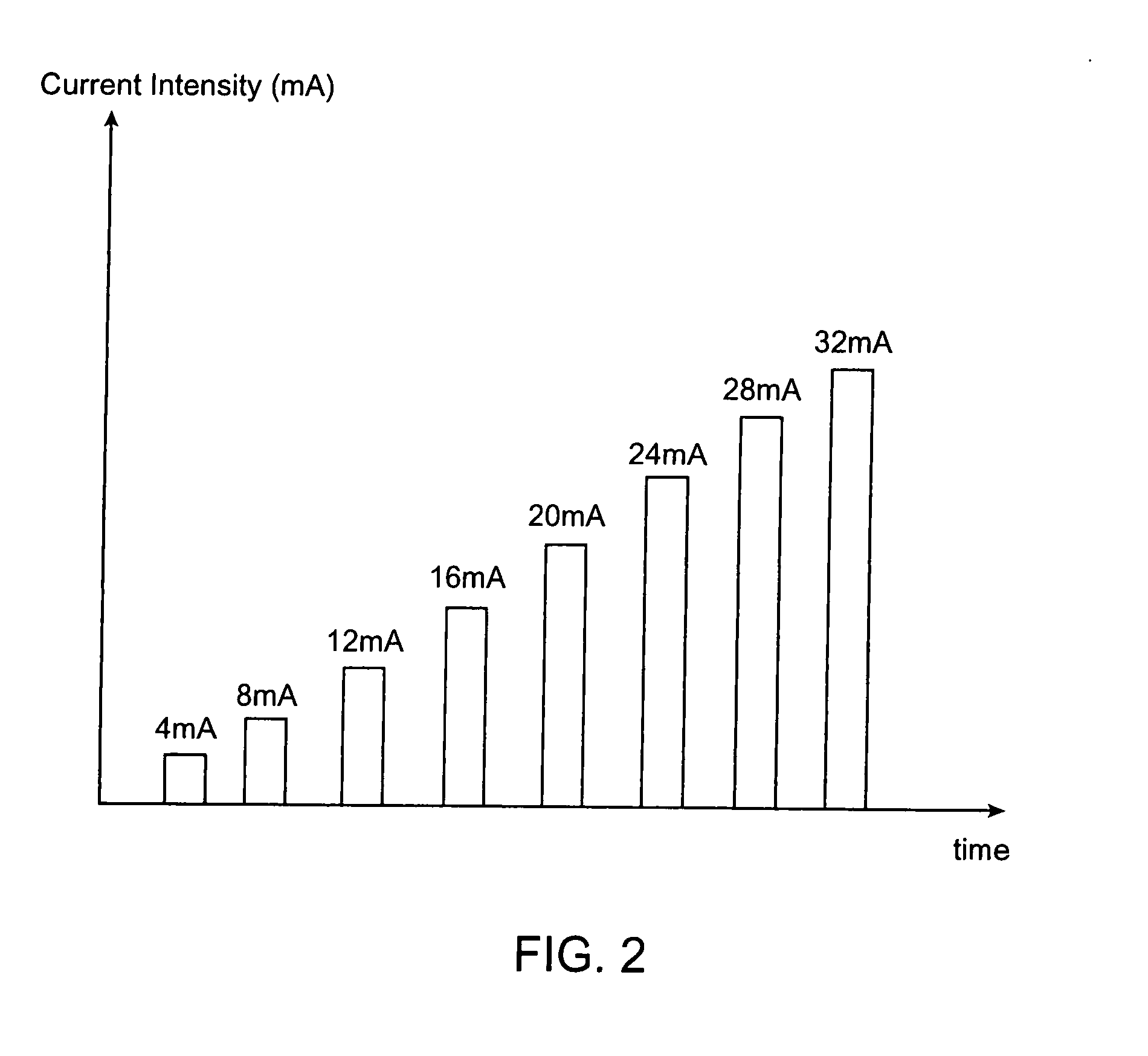
[0049] In preferred aspects, the present system applies a signal with a known current level (mA) to a “probe” (which could be midline probe, a cannula, a needle, etc.) Depending on the current level, distance to the nerve, and health of the nerve, an EMG may be detected in a muscle coupled to the nerve. In accordance with preferred aspects, an EMG response is determined to have been detected when the peak-to-peak response of th...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com