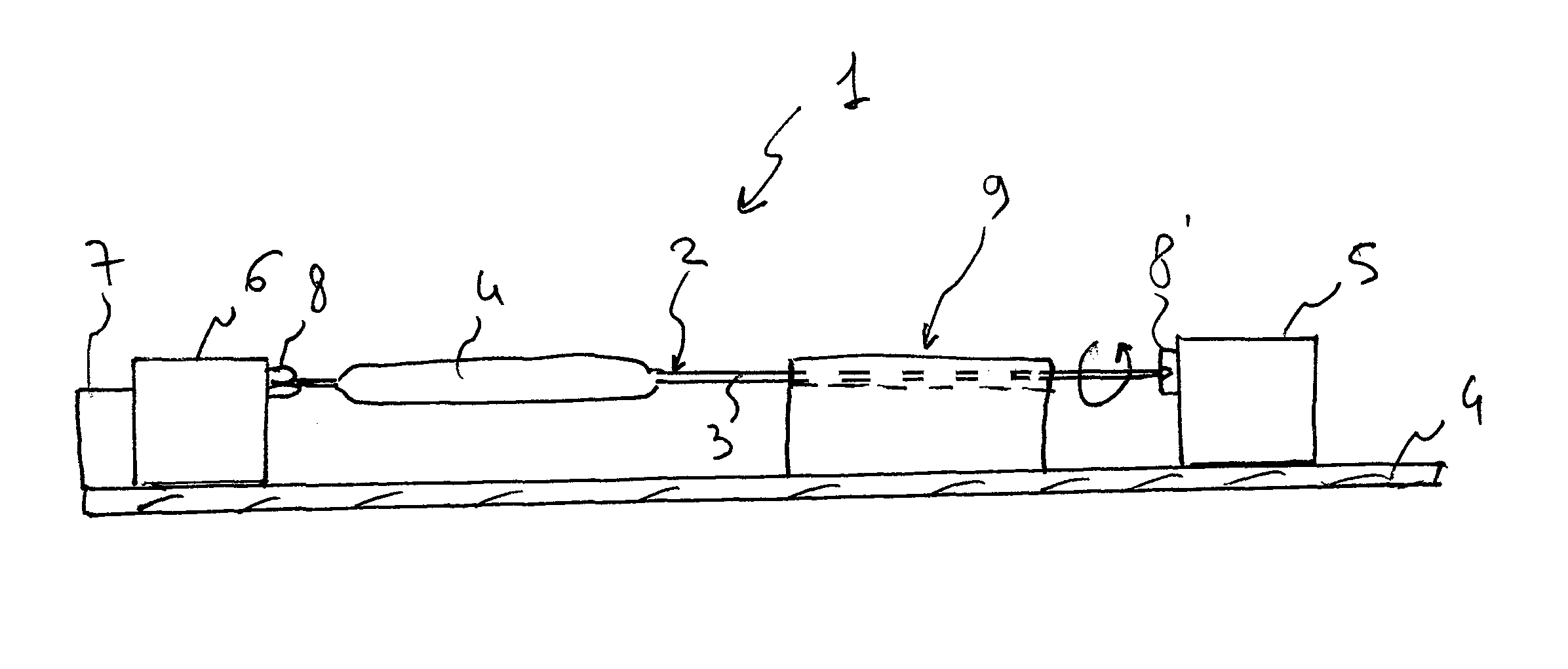
Drug-eluting medical device
a medical device and drug-eluting technology, applied in the direction of medical devices, dilators, catheters, etc., can solve the problems of incomplete intervention, obstruction, and restriction or obstruction
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
example 1a
Coating of Catheter Balloons with Crystalline Hydrated or Crystalline Hydrated Solvated Paclitaxel
[0102]Paclitaxel solutions have been prepared at a 50 mg / mL concentration in the following solvents:
[0103](1) 9:1 THF / water
[0104](2) 9:1 THF / water with addition of 15 mg / mL urea
[0105](3) 6.5:3.5 THF / water
[0106](4) Acetone / ethanol / water
[0107](5) Acetic acid (comparative solution)
[0108](6) Dichloromethane (comparative solution)
[0109]It shall be noted that paclitaxel in a crystalline hydrated or solvated hydrated form according to the invention is not obtained by crystallization from acetic acid. Instead, amorphous paclitaxel is obtained by precipitation from dichloromethane.
[0110]Some balloons—made of a polyamide-12+polyether-polyamide block copolymer compound (70% UBESTA® XPA9063+30% UBESTA® 3030XA) and in a folded condition—have been coated with paclitaxel by wetting the surface thereof with equal volumes of the solutions (1)-(6) by means of a Hamilton syringe, according to the previous...
example 1b
Coating of Catheter Balloons with Crystalline Hydrated or Crystalline Hydrated Solvated Paclitaxel (Coating in an Unfolded Condition)
[0113]The procedure of example 1A has been repeated using coating solution (2), by inflating first the folded balloons at 7 bar, then removing the pressurised air source and coating the inflated balloons by means of a Hamilton syringe. The coated balloons have then been re-folded after about 1 minute after the coating step, while the surface thereof was still wet.
[0114]The appearance of the coating was white, substantially homogeneous.
example 2
Assessment of Paclitaxel Adhesion on the Surface of the Catheter Balloons
[0115]The balloons prepared according to the example 1 have been subjected to some assessments, in order to determine the drug adhesion under the various conditions.
[0116]Test A
[0117]First, the dry adhesion has been assessed, which is useful to determine the paclitaxel loss which can occur in the production or handling steps of the balloon. Such determination has been carried out by dry expanding the balloon and shaking the inflated balloon within a tube.
[0118]The paclitaxel content in the tube was determined by HPLC / UV. The drug was taken up with ethanol, the tubes were closed and vigorously vortexed for at least 30 seconds, followed by a treatment in an ultrasound bath for 30 minutes. At least 70 μl of extract were injected into the HPLC, together with a paclitaxel standard solution (concentration of about 20 μg / mL). The results are reported in Table I.
[0119]Test B
[0120]Release of paclitaxel at the site of in...
PUM
| Property | Measurement | Unit |
|---|---|---|
| Temperature | aaaaa | aaaaa |
| Temperature | aaaaa | aaaaa |
| Temperature | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com