Methods, Systems and Devices for Non-Invasive Open Ventilation For Providing Ventilation Support
a technology of nasal interface and non-invasive ventilation, which is applied in the direction of mechanical equipment, valves, operating means/releasing devices, etc., can solve the problems of inability to provide patient comfort, nasal interfaces may generate undesirable noise, and performance may degrade, so as to reduce the work of breathing, increase airway pressure, and increase lung volume
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
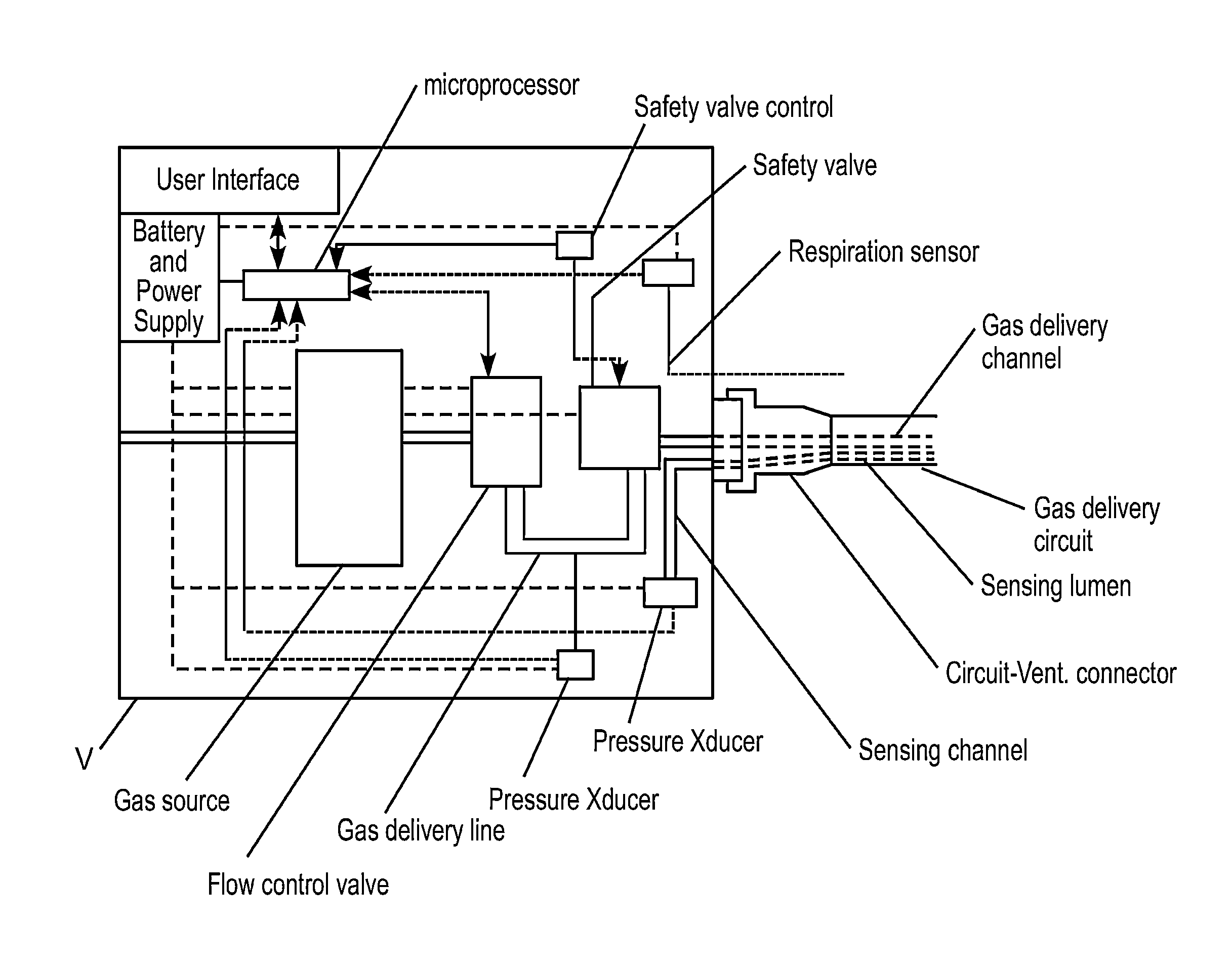
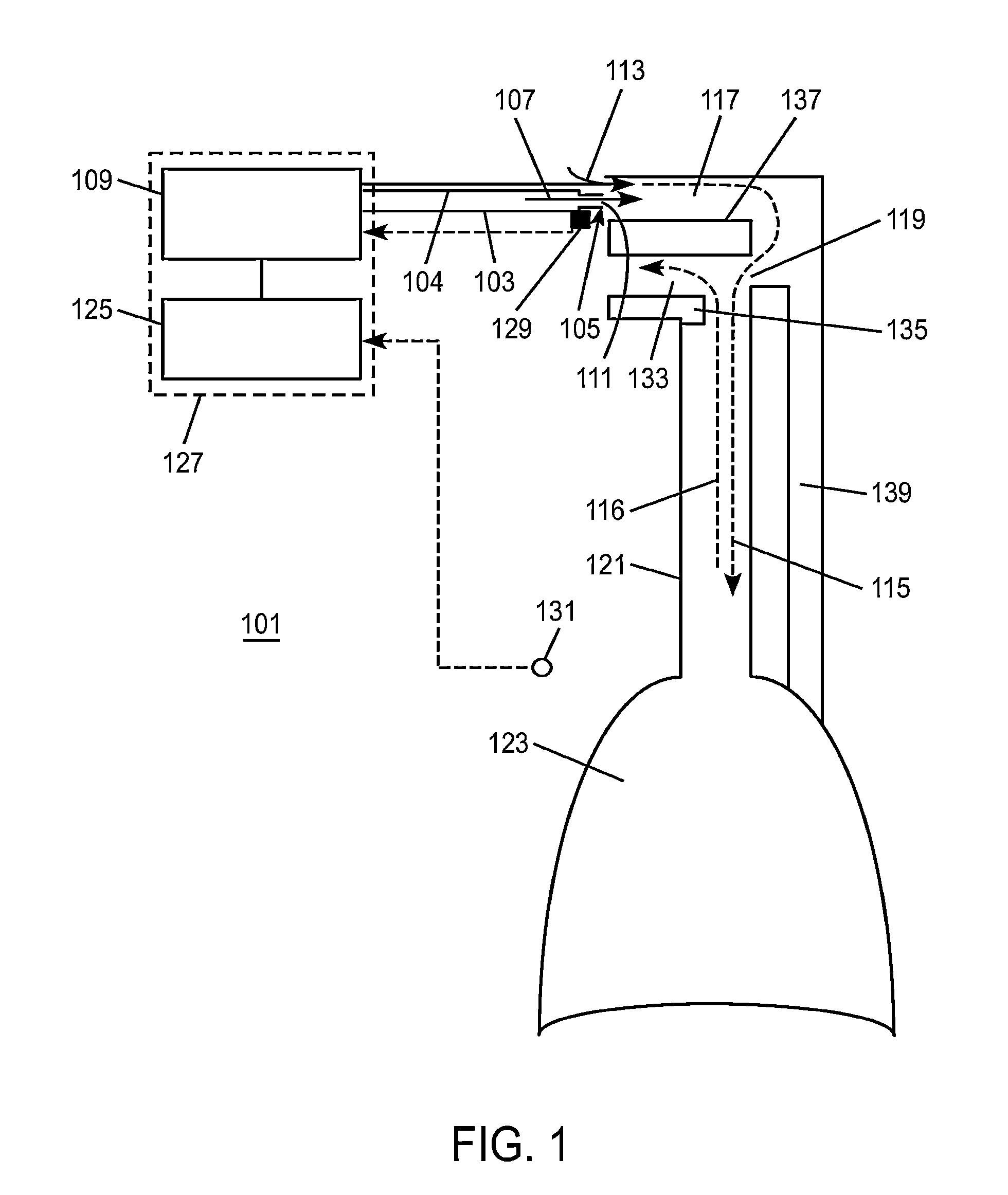
[0189]FIG. 1 is a schematic diagram showing an exemplary overall system 101 of an embodiment of the invention. A patient may be ventilated with non-invasive open ventilation (NIOV) using a ventilation gas delivery circuit 103, an airway pressure sensing line 104, and non-invasive open nasal interface (nasal interface) 105. The nasal interface 105 preferably does not seal against the patient's nose such as is typical with other ventilation interfaces, and rather leaves the nose open for the user to breathe normally and freely from the ambient surroundings. Ventilation gas 107 delivered from a ventilator 109 may travel through the gas delivery circuit 103 and out one or more gas exit ports 111 in the nasal interface 105. The ventilation gas 107 may exit at a speed that entrains ambient air 113, such that the combination of ventilation gas 107, entrained ambient air 113 and spontaneously inhaled air 115, if the patient is spontaneously breathing, is delivered to the patient's airways, ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com