Patents
Literature
31 results about "Lung pressure" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
It can lead to heart failure. Oxygenated blood is supplied to the rest of the body by the relevant pumping chamber of the heart. If hypertension, or high blood pressure, occurs near the lungs in a person's circulation, it is likely to be a progressive and serious condition.
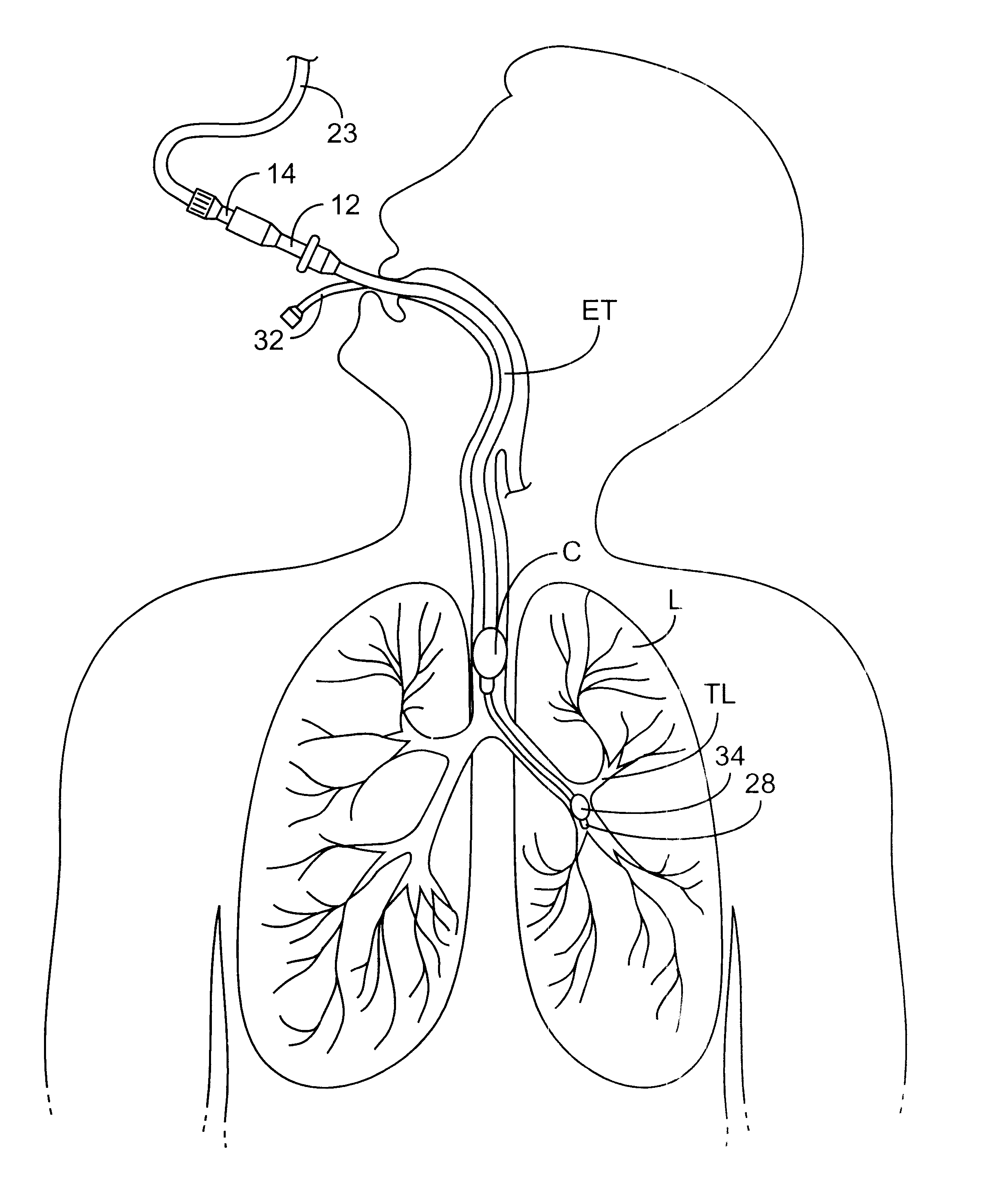
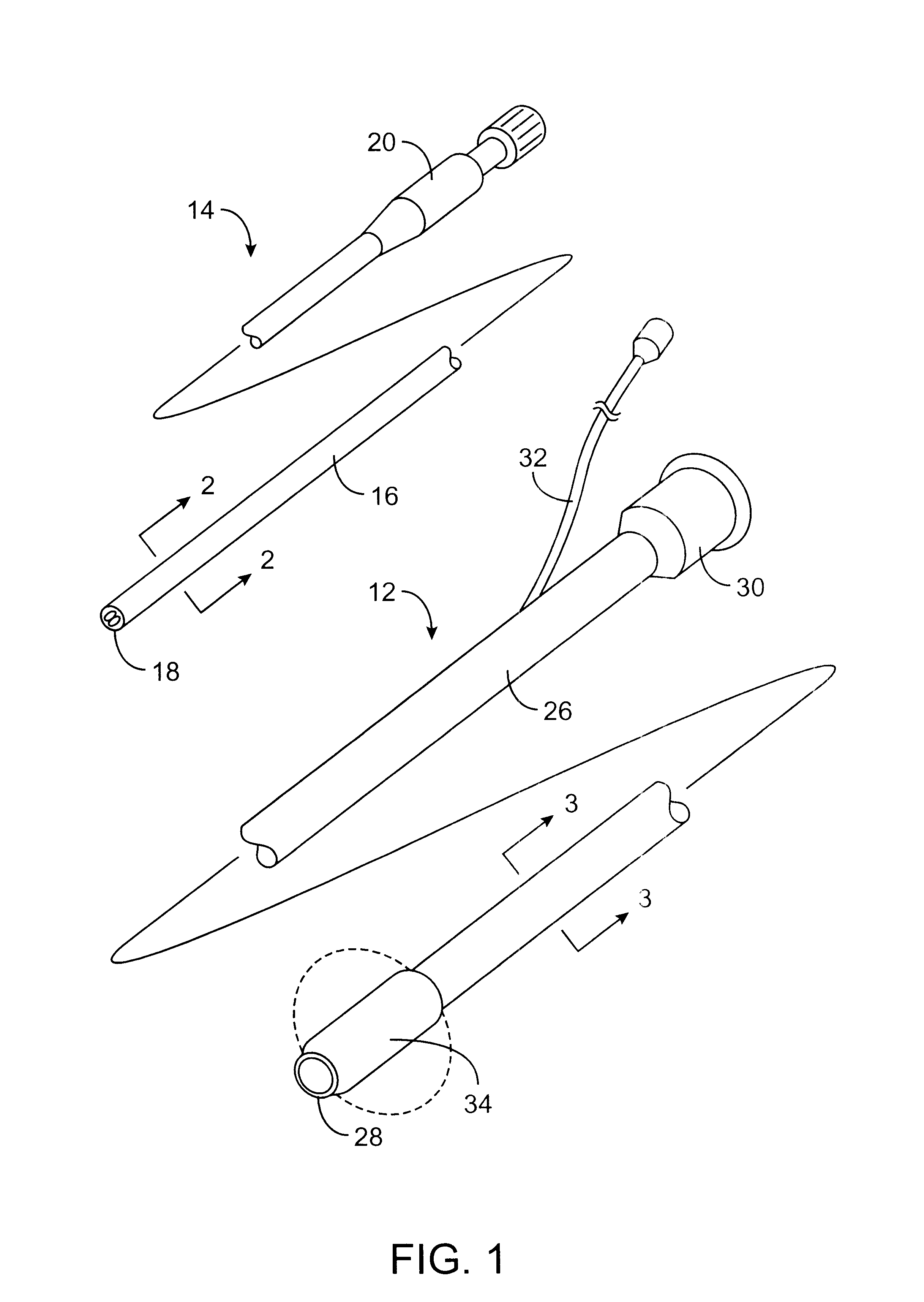
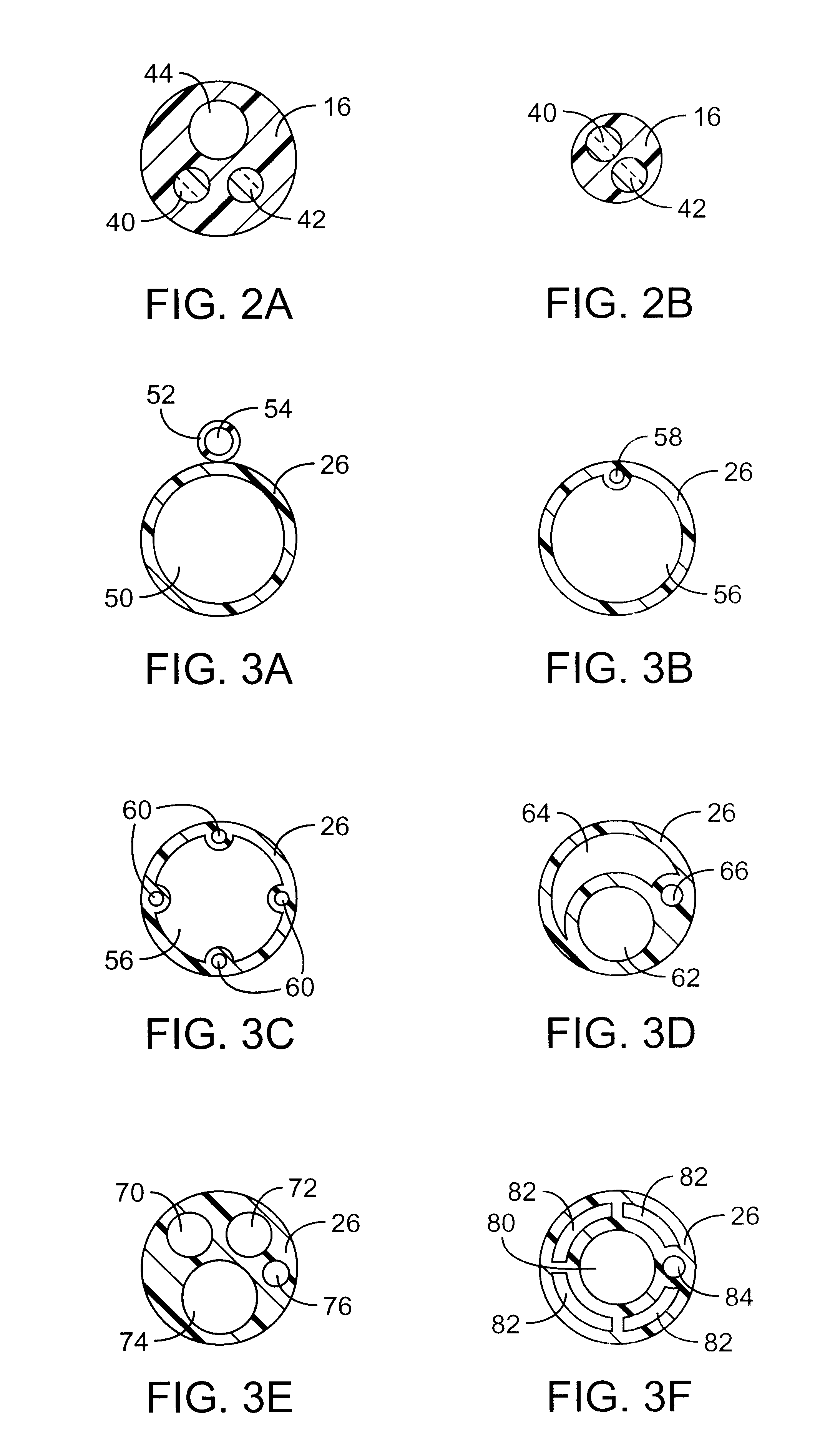
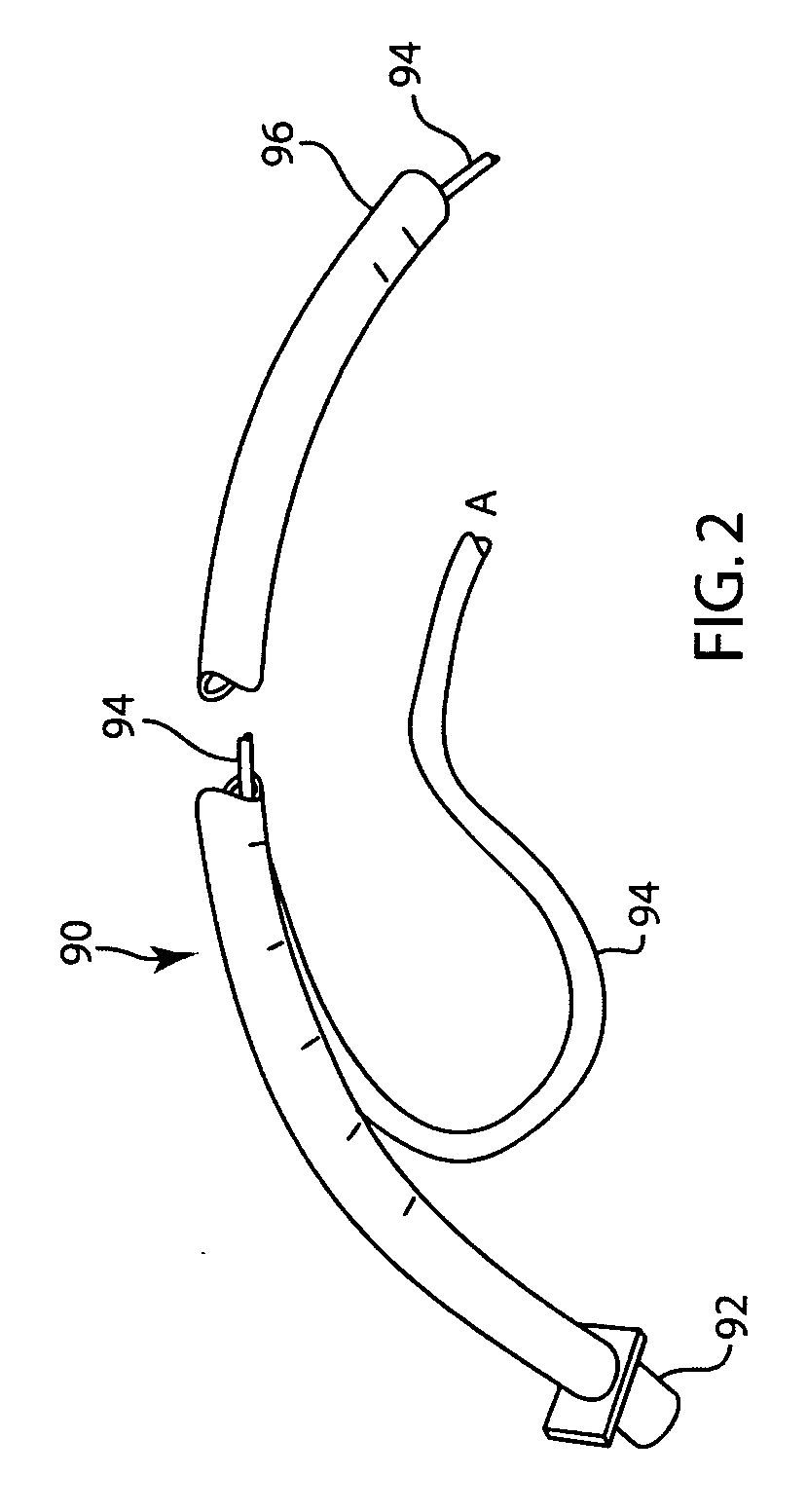
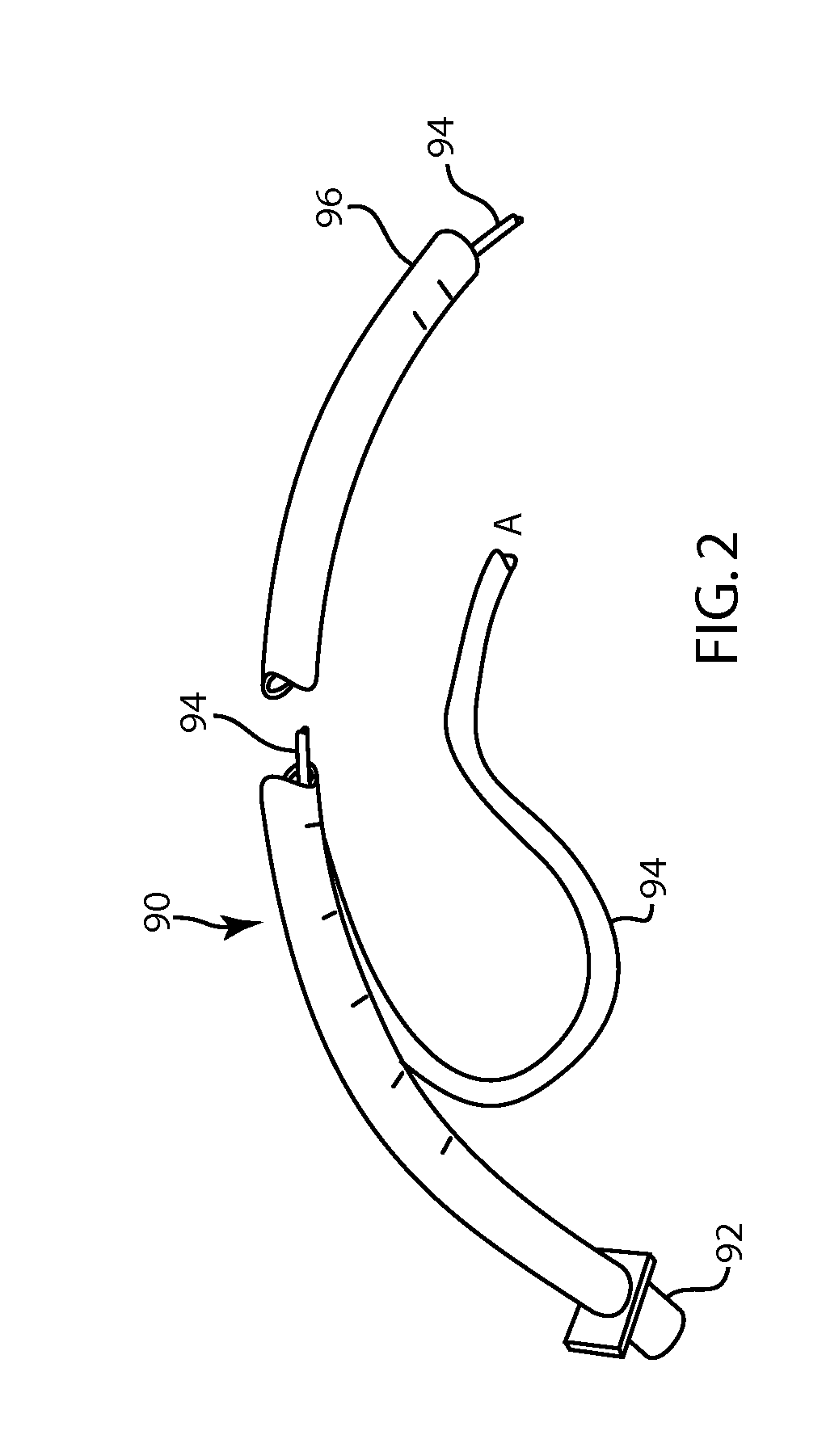
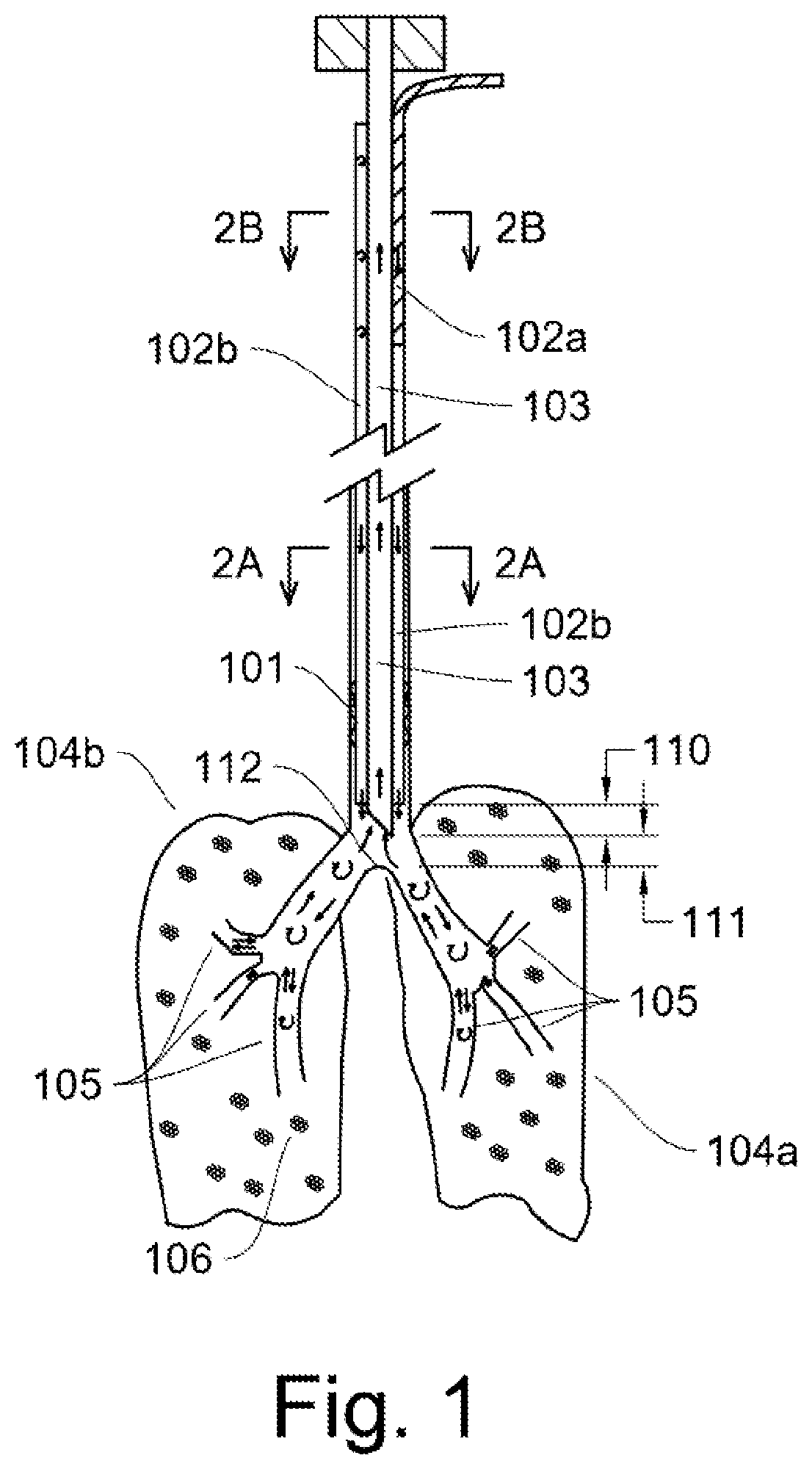
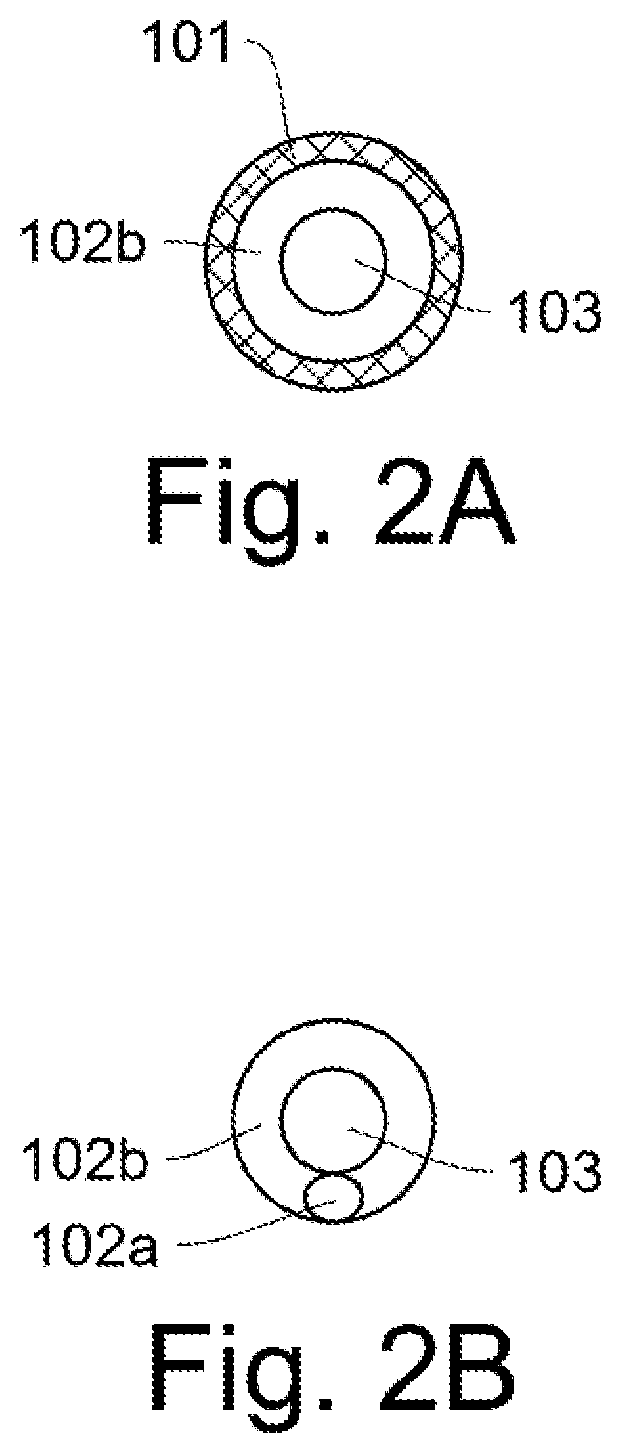
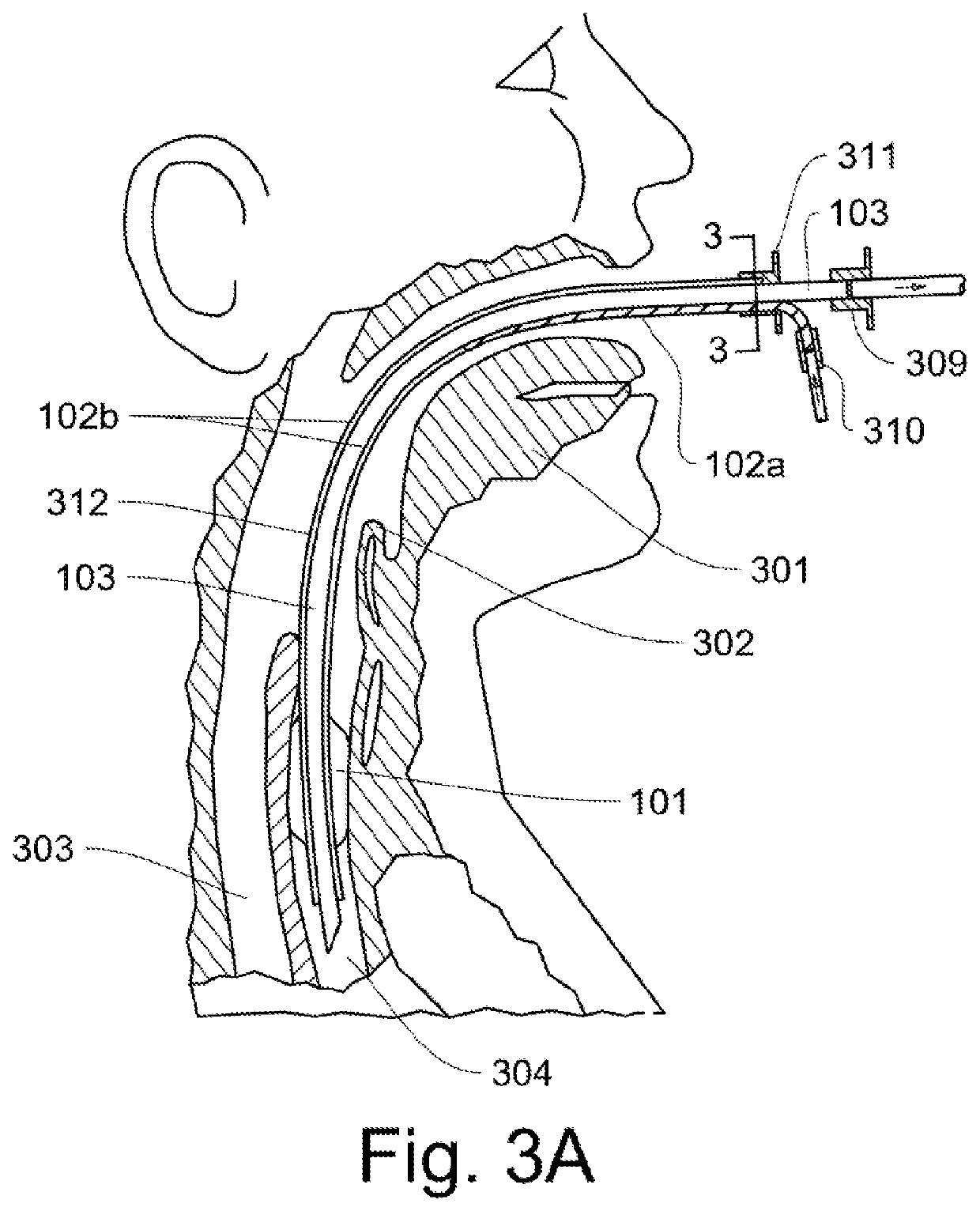
Sheath and method for reconfiguring lung viewing scope
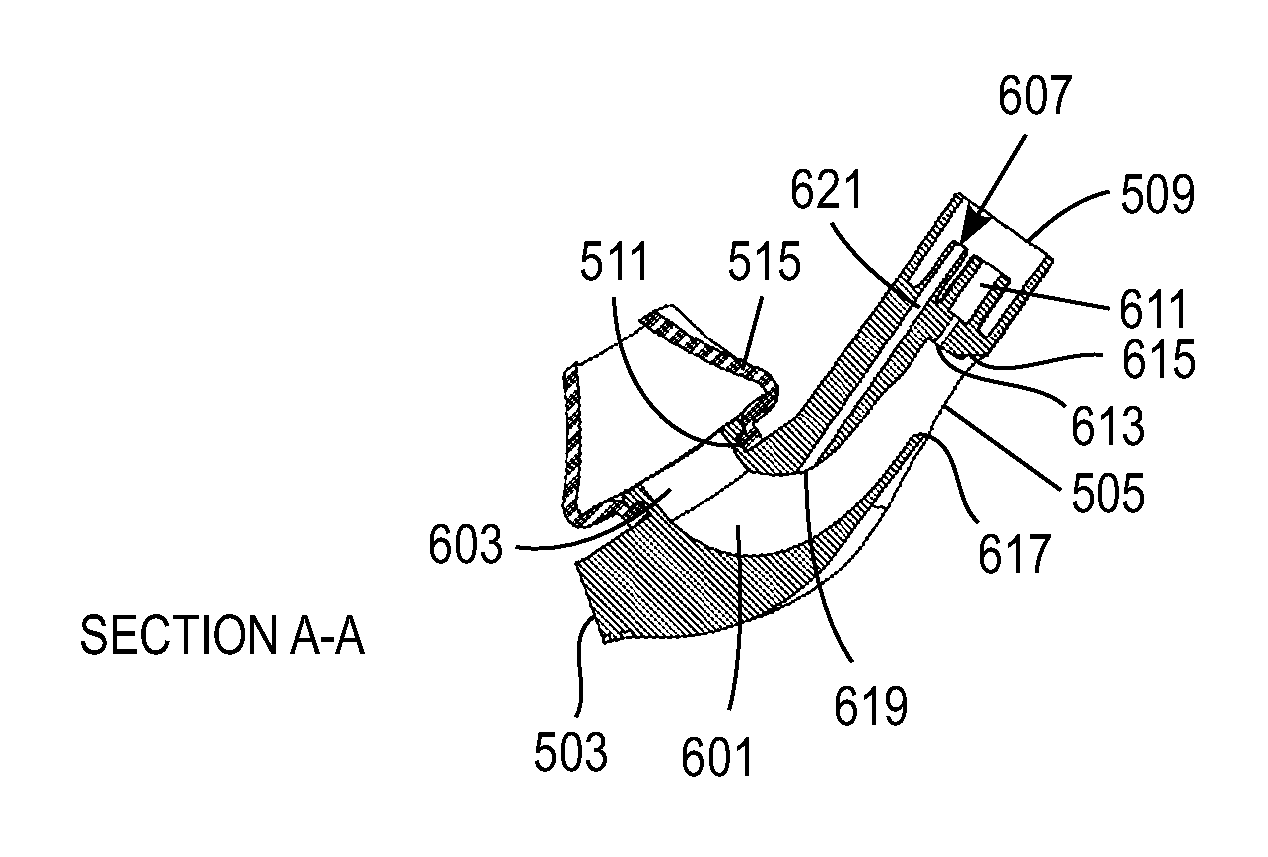
Apparatus, methods, and kits, are provided for use in combination with a conventional bronchoscope or other lung viewing scope. In particular, sheaths having an inflatable cuff at their distal end are provided to receive a viewing scope through a lumen thereof. The sheaths thus provide an inflatable cuff on a viewing scope assembly so that the scope can be used in procedures which require selective isolation of regions of a patient's lungs. In particular embodiments, the sheaths may include stop elements for properly positioning a viewing scope therein, pressure transducers for providing accurate lung pressure information during procedures, and the like. Methods for using and forming sheaths having inflatable cuffs are also described.
Owner:PULMONX
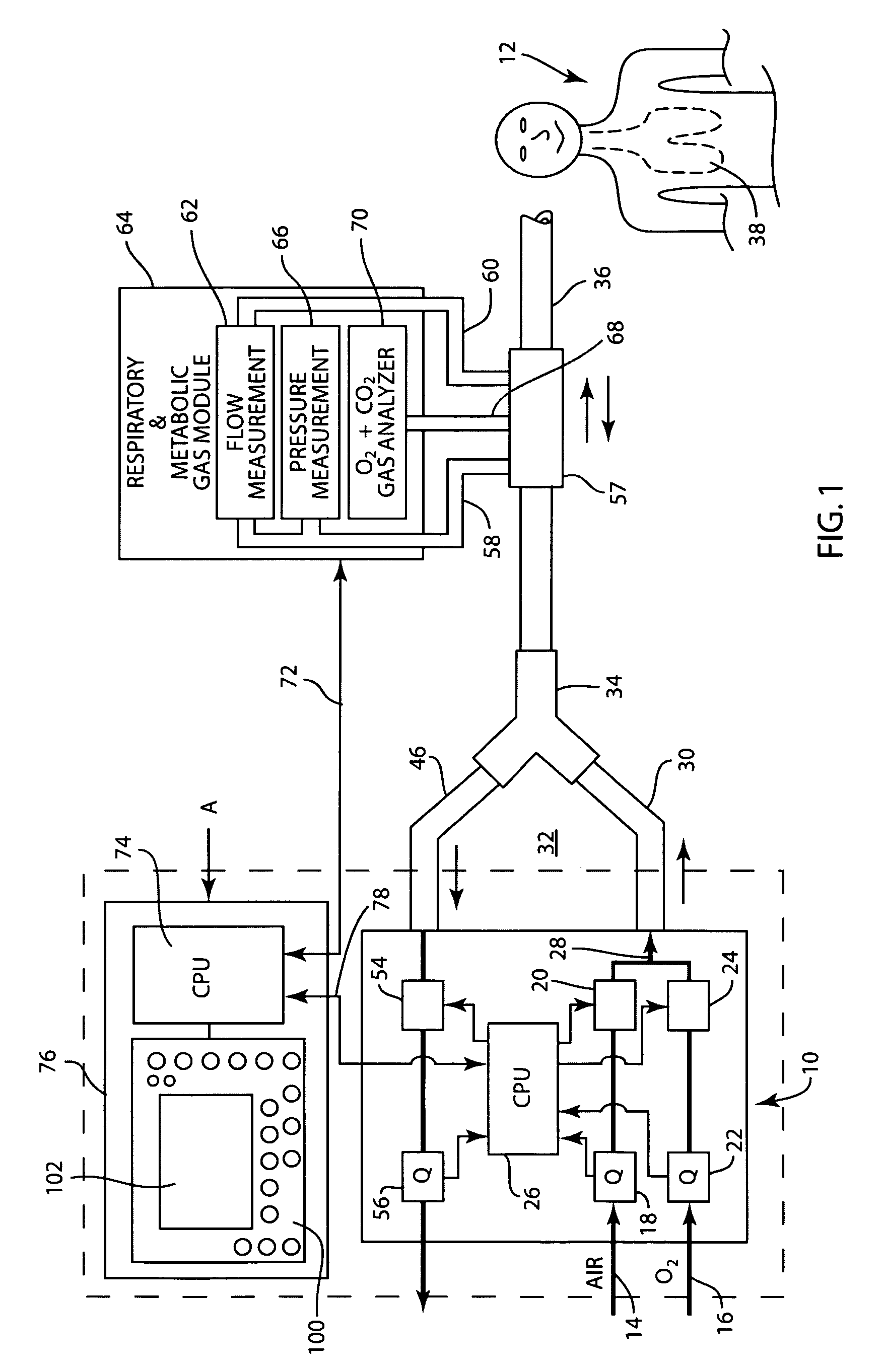
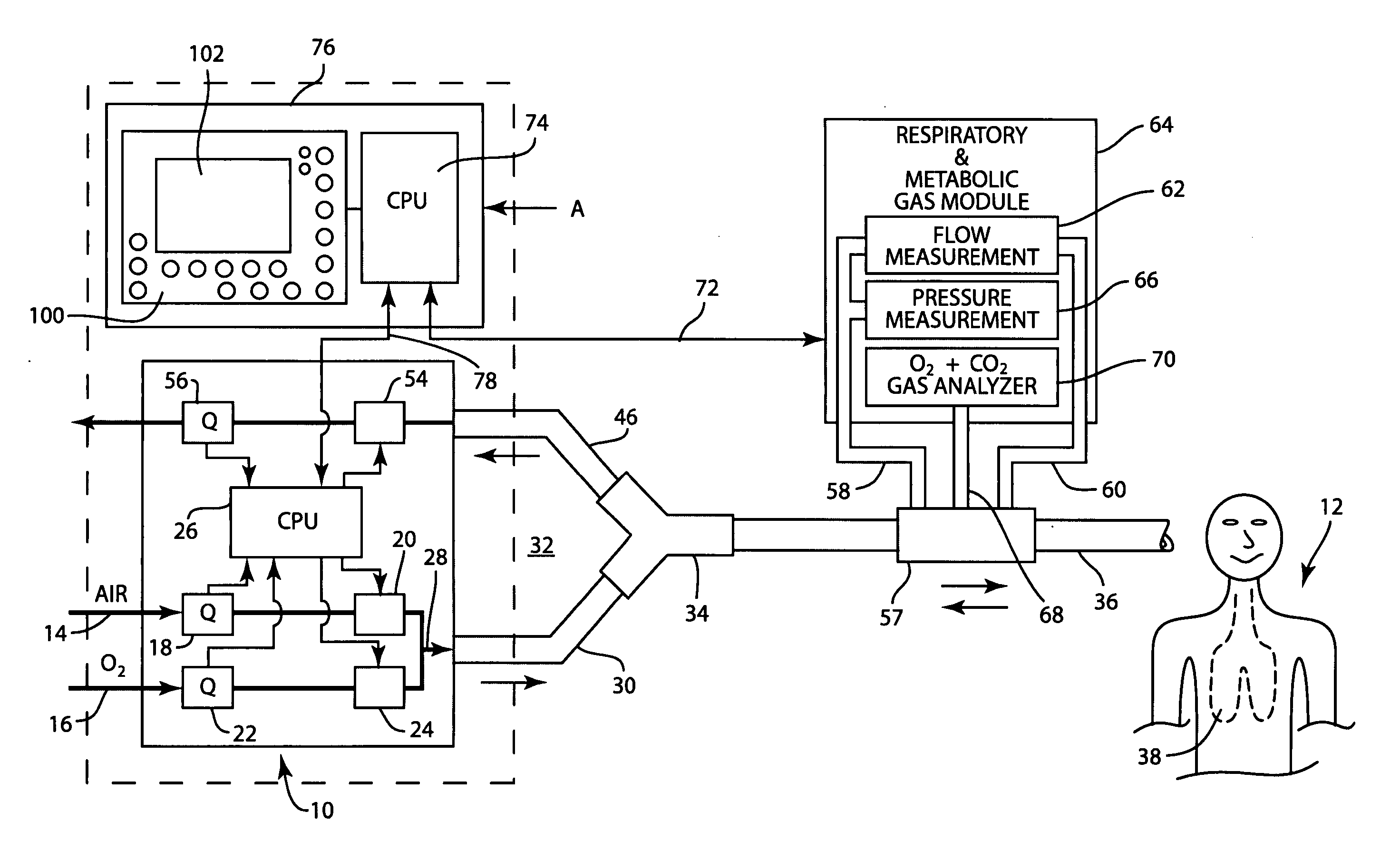
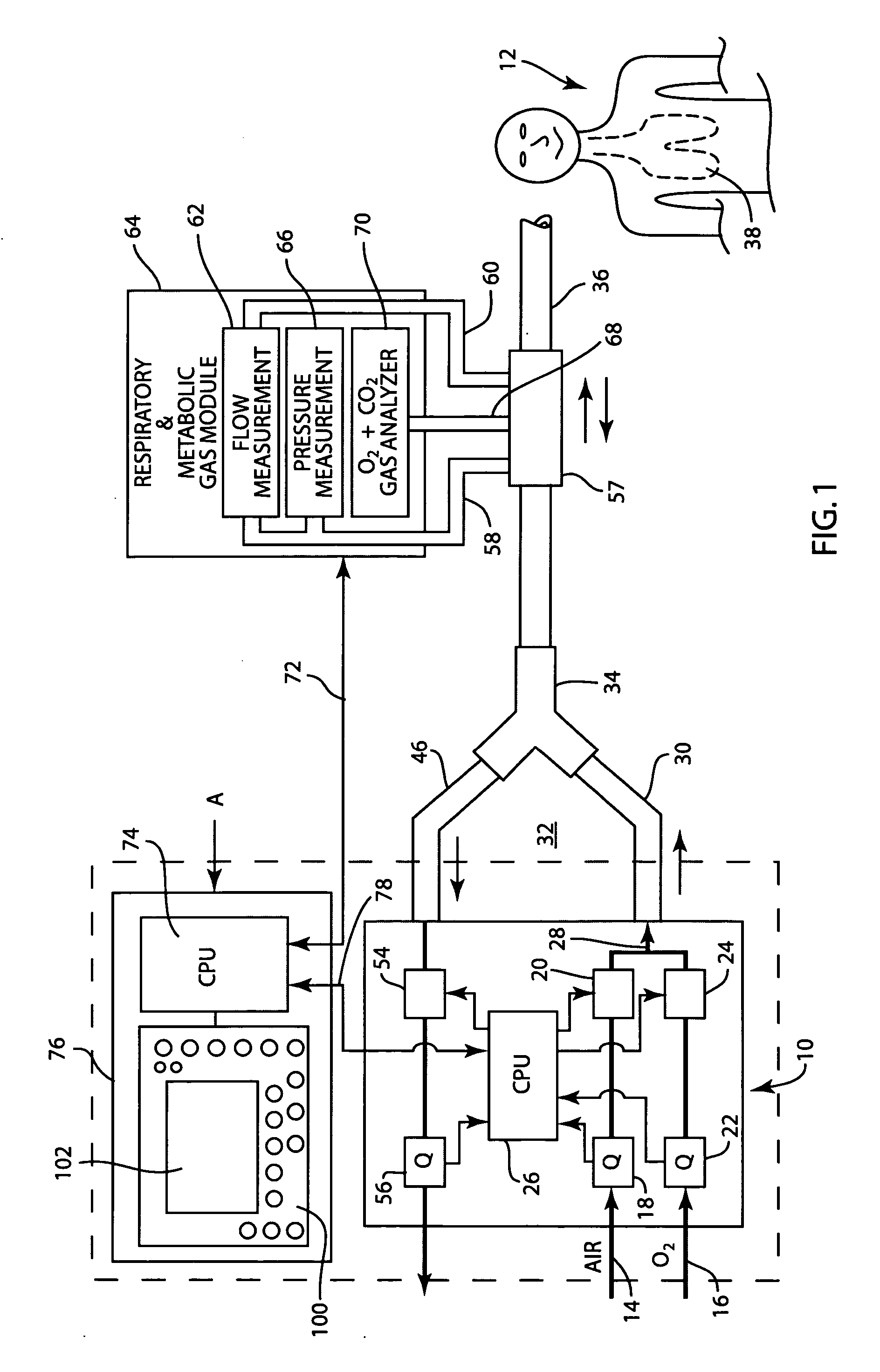
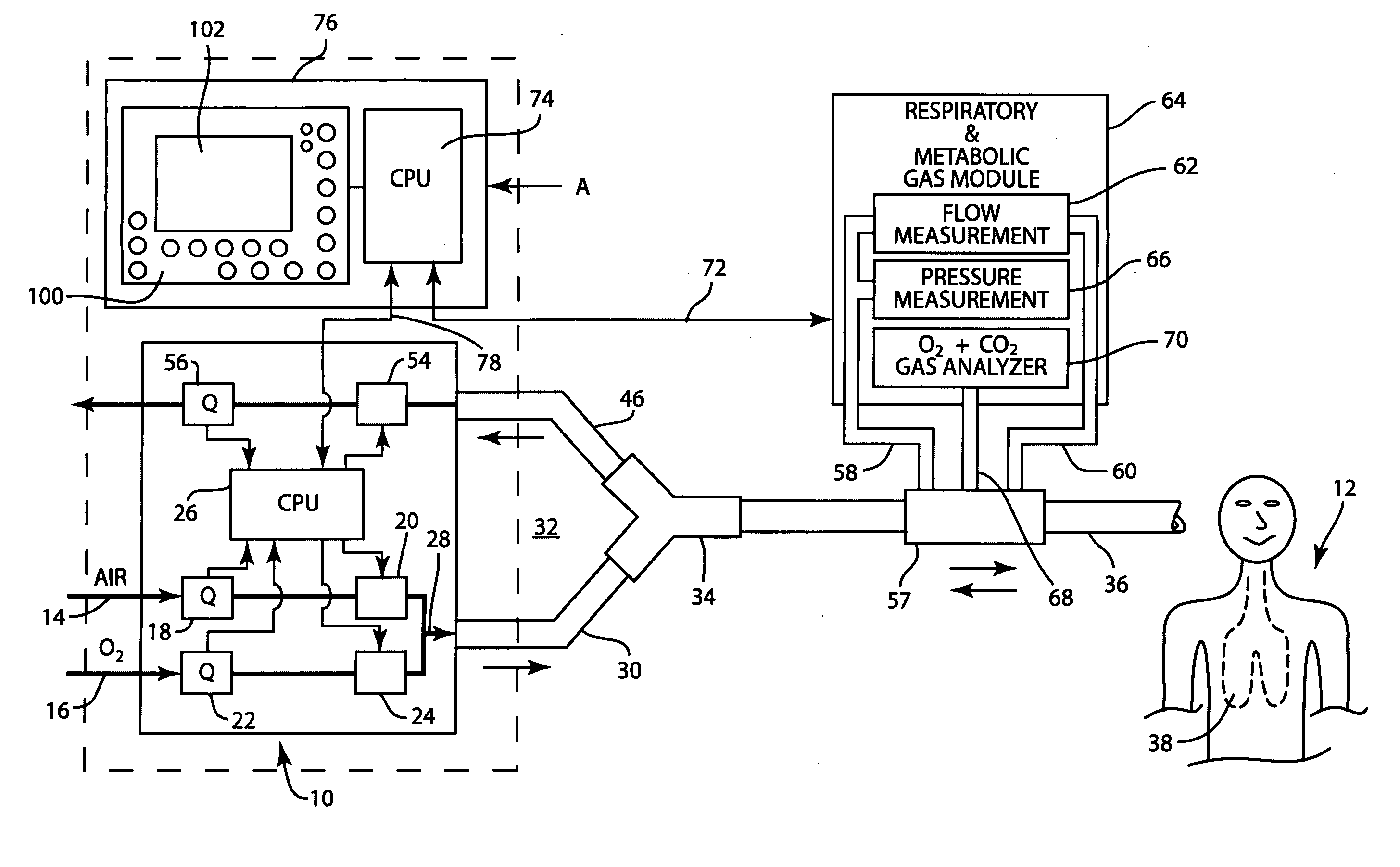
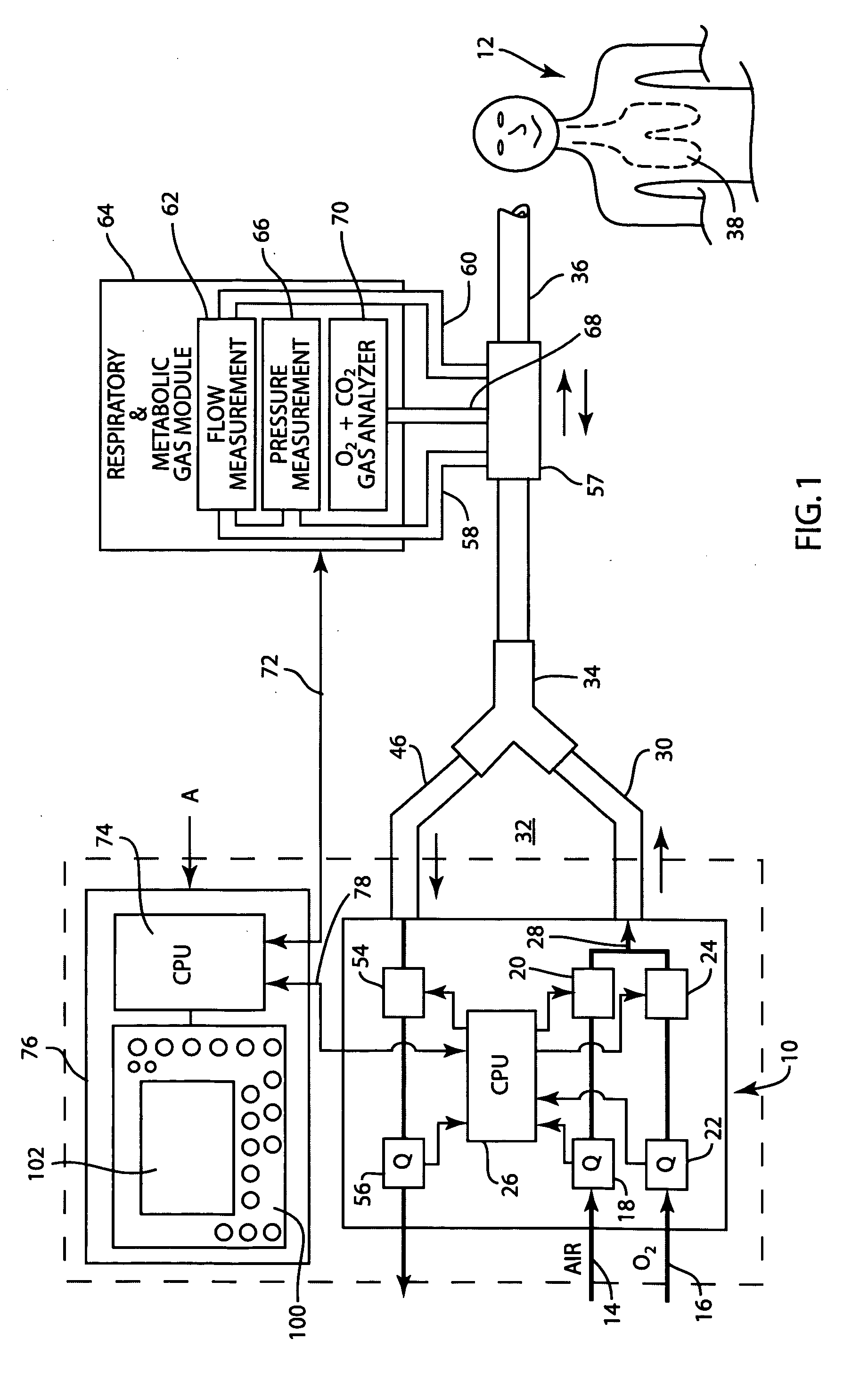
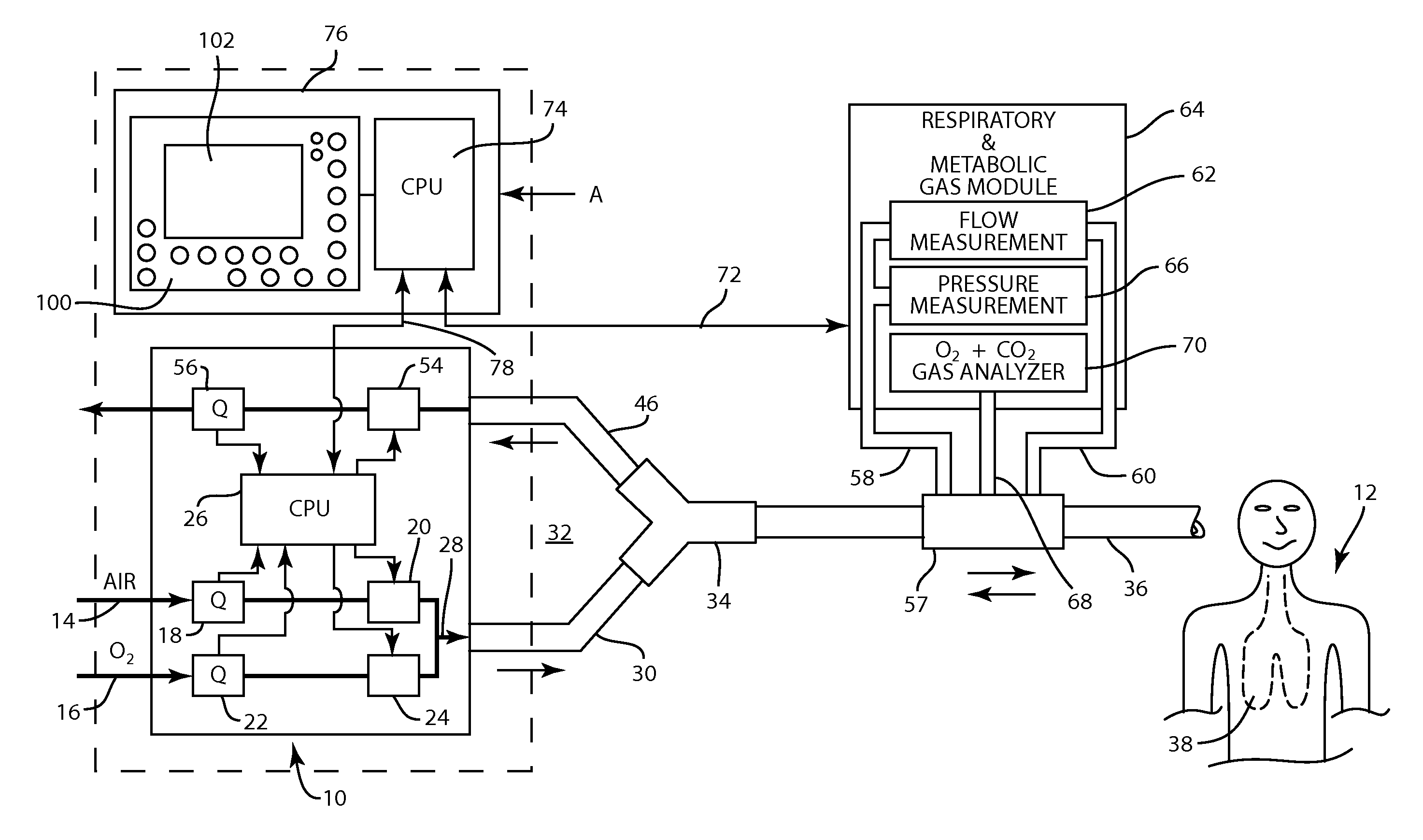
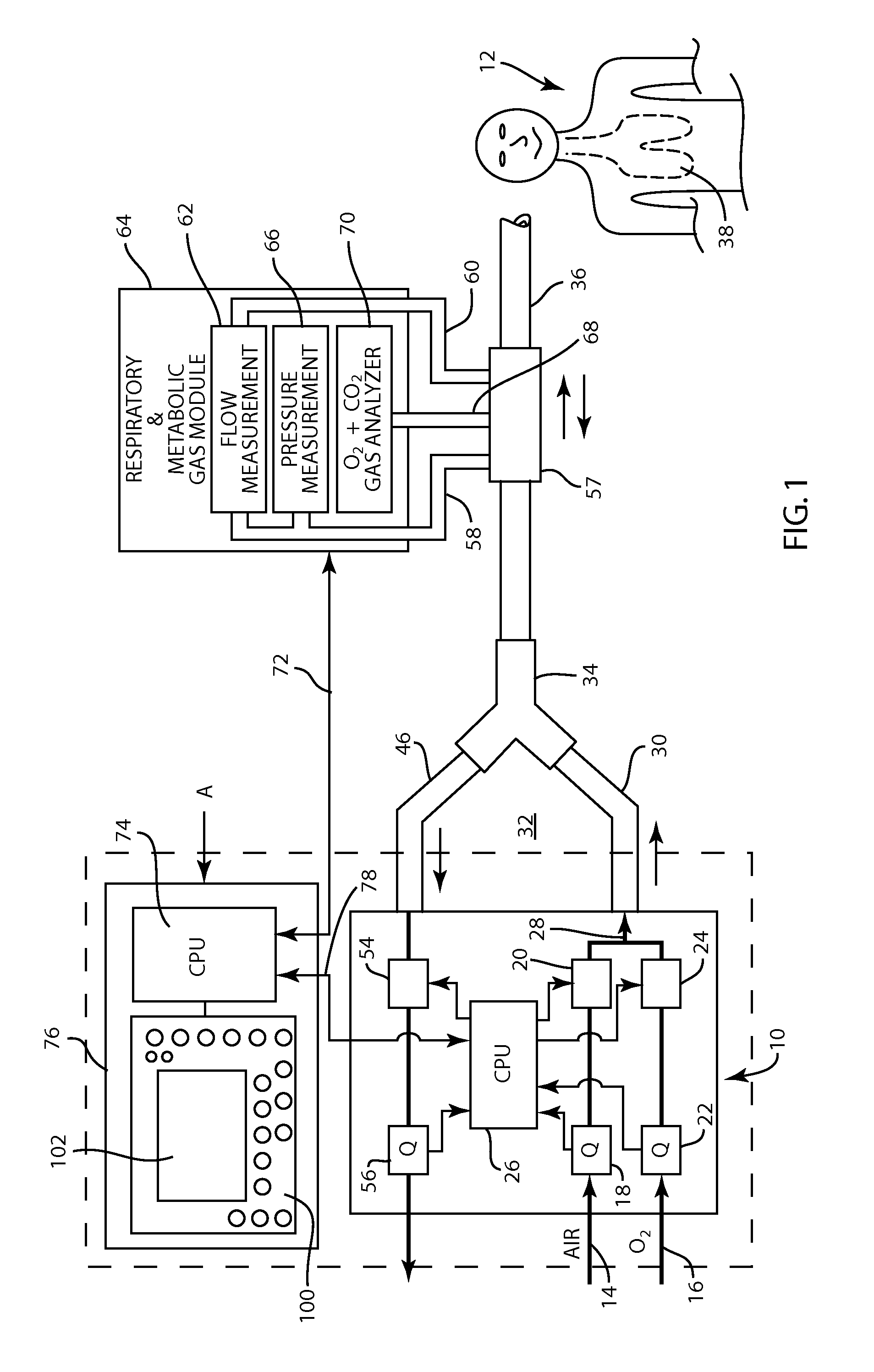
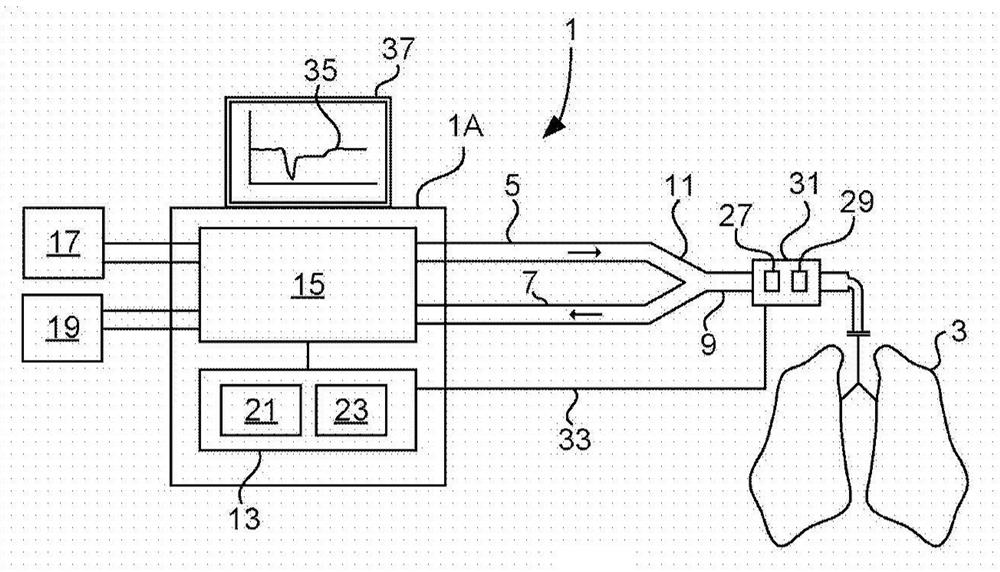
Method and apparatus for airway compensation control
ActiveUS20080091117A1Capacity remains stableRespiratorsOperating means/releasing devices for valvesForced expiratory vital capacityPulmonary compliance
A ventilator for ventilating a patient also assists a clinician in determining a suitable PEEP for the patient. For this purpose, a graph or tabular display of a series of different value PEEPs and corresponding functional residual capacities of the patient may be provided. Or, the relationship between lung compliance and a series of different values of PEEP may be provided. Or, the amount of the lung volume recruited / de-recruited at various levels of PEEP may be determined for use in selecting a desired PEEP. To this end, the functional residual capacity of the lungs is determined for a first PEEP level. The PEEP is then altered to a second level and a spirometry dynostatic curve of lung volume and pressure data is obtained. The lung volume on the dynostatic curve at a lung pressure corresponding to the first PEEP value is obtained. The difference between the functional residual capacity of the lungs at the first PEEP level and that determined from the dynostatic curve represents the lung volume recruited / de-recruited when changing between said first and second PEEPs.
Owner:GENERAL ELECTRIC CO
Apparatus and method for identifying optimal PEEP
InactiveUS20070062532A1Quickly and easily determineSure easyRespiratorsOperating means/releasing devices for valvesForced expiratory vital capacityRadiology
A ventilator for ventilating a patient also assists a clinician in determining a suitable PEEP for the patient. For this purpose, a graph or tabular display of a series of different value PEEPs and corresponding functional residual capacities of the patient may be provided. Or, the amount of the lung volume recruited / de-recruited at various levels of PEEP may be determined for use in selecting a desired PEEP. To this end, the functional residual capacity of the lungs is determined for a first PEEP level. The PEEP is then altered to a second level and a spirometry dynostatic curve of lung volume and pressure data is obtained. The lung volume on the dynostatic curve at a lung pressure corresponding to the first PEEP value is obtained. The difference between the functional residual capacity of the lungs at the first PEEP level and that determined from the dynostatic curve represents the lung volume recruited / de-recruited when changing between said first and second PEEPs.
Owner:GENERAL ELECTRIC CO
Apparatus and method for identifying FRC and PEEP characteristics
InactiveUS20070062533A1Quickly and easily determineSure easyRespiratorsOperating means/releasing devices for valvesForced expiratory vital capacityPulmonary compliance
A ventilator for ventilating a patient also assists a clinician in determining a suitable PEEP for the patient. For this purpose, a graph or tabular display of a series of different value PEEPs and corresponding functional residual capacities of the patient may be provided. Or, the relationship between lung compliance and a series of different values of PEEP may be provided. Or, the amount of the lung volume recruited / de-recruited at various levels of PEEP may be determined for use in selecting a desired PEEP. To this end, the functional residual capacity of the lungs is determined for a first PEEP level. The PEEP is then altered to a second level and a spirometry dynostatic curve of lung volume and pressure data is obtained. The lung volume on the dynostatic curve at a lung pressure corresponding to the first PEEP value is obtained. The difference between the functional residual capacity of the lungs at the first PEEP level and that determined from the dynostatic curve represents the lung volume recruited / de-recruited when changing between said first and second PEEPs.
Owner:GENERAL ELECTRIC CO
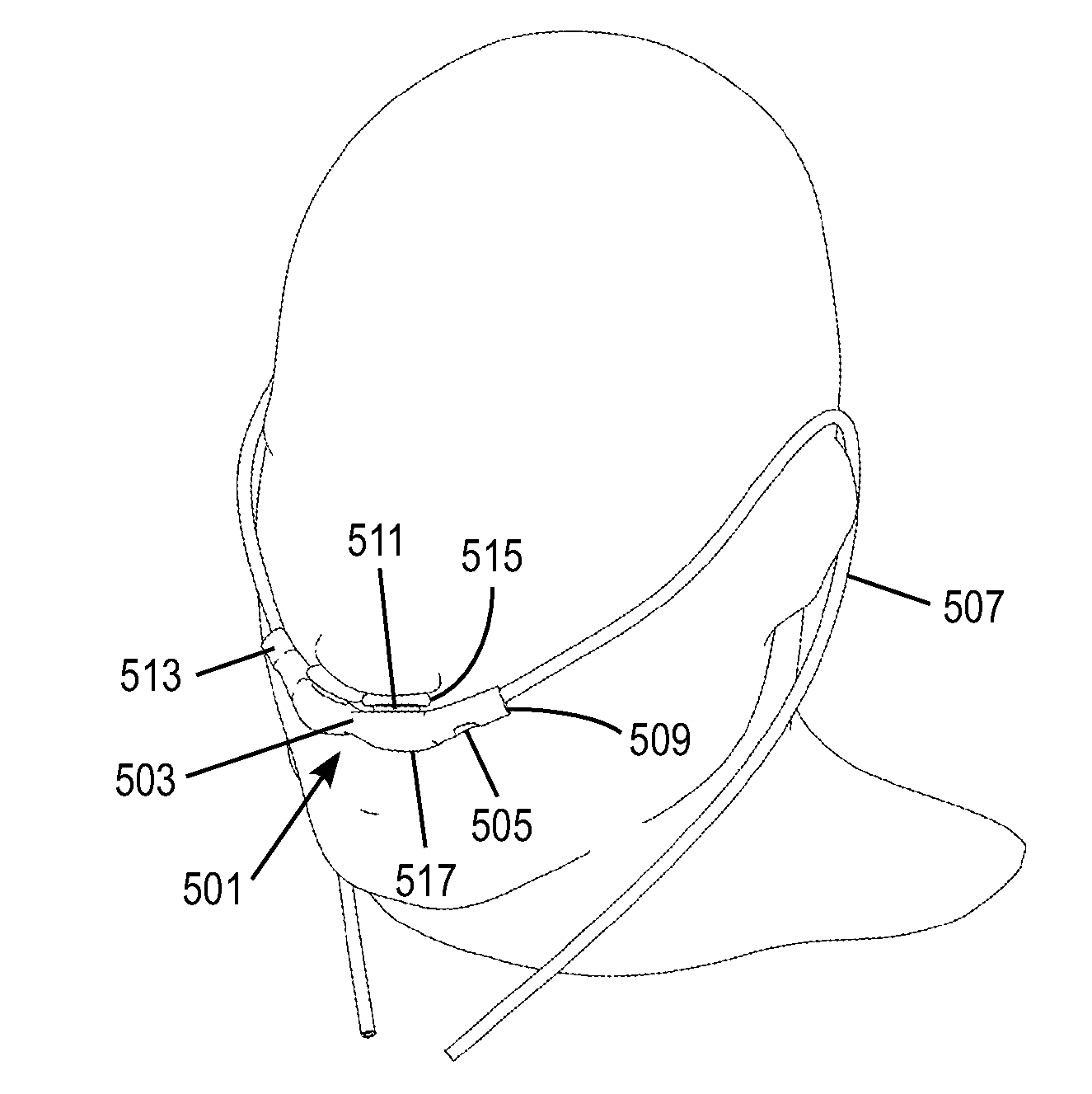
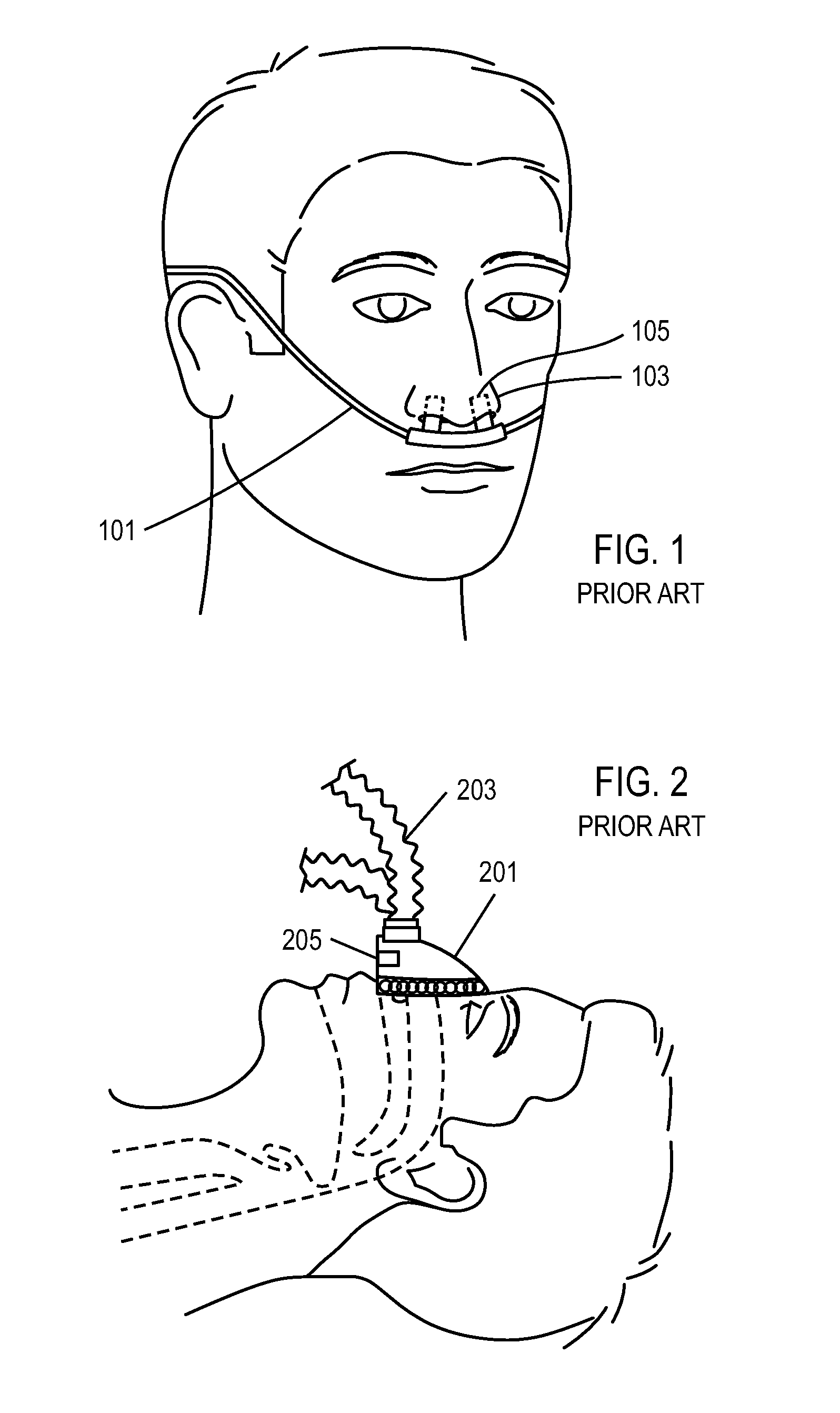
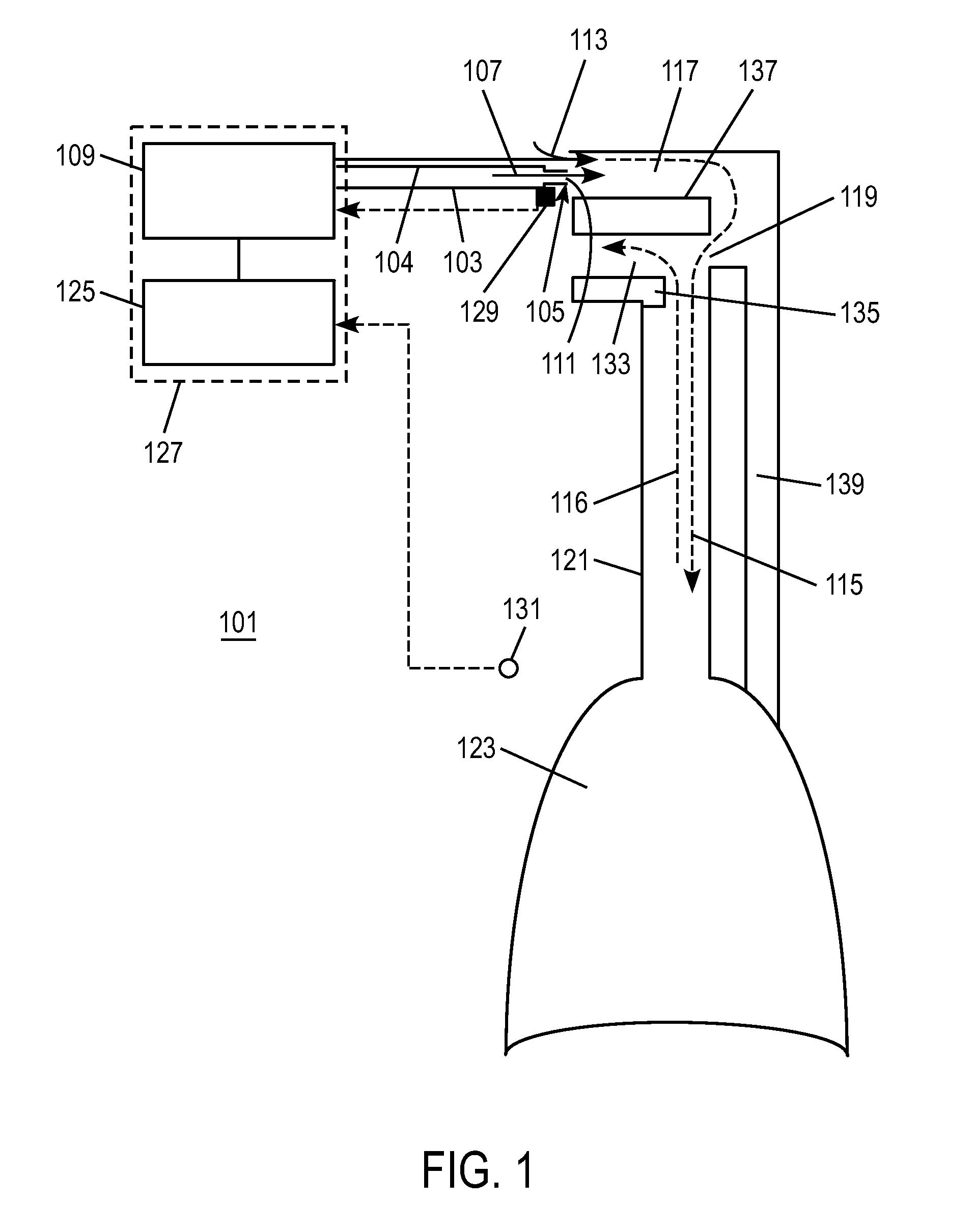
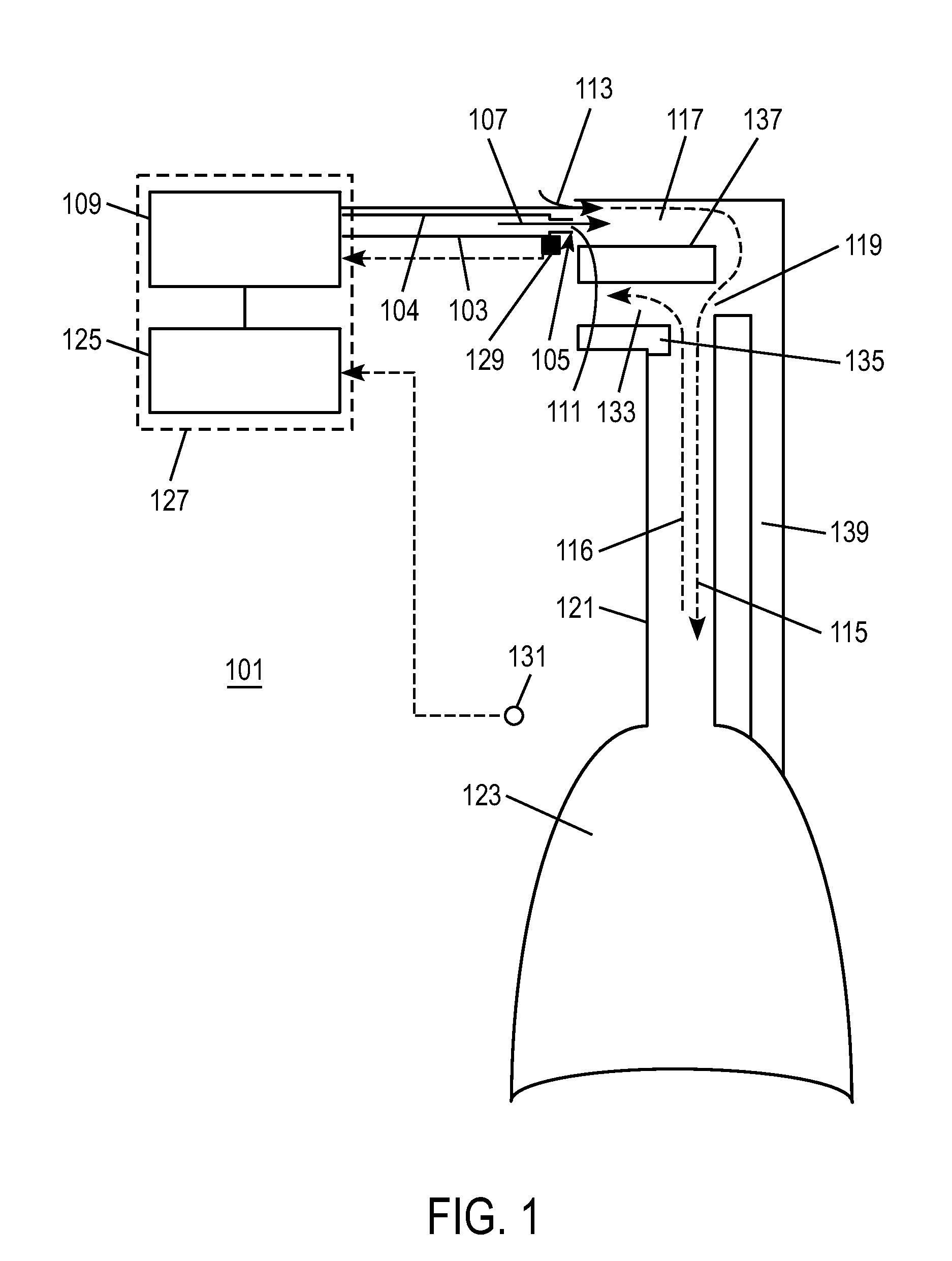
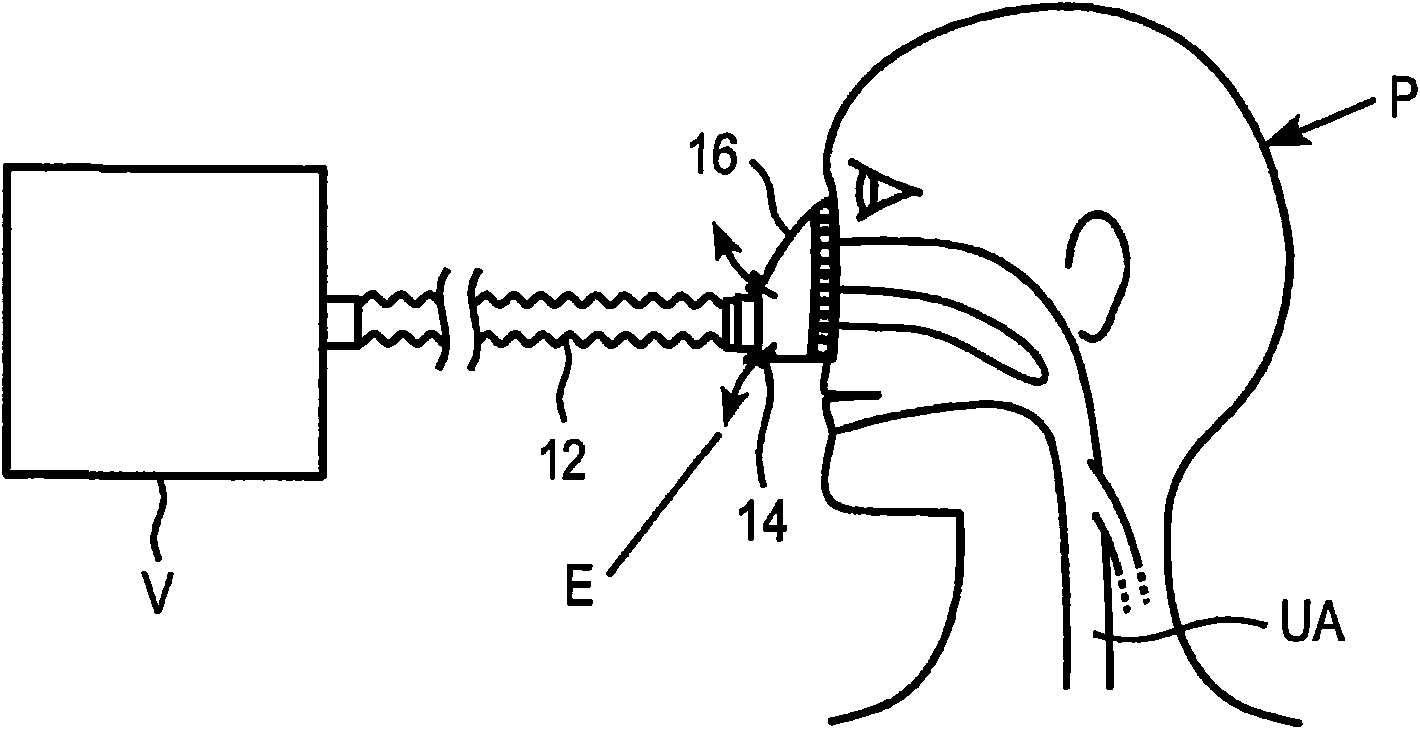
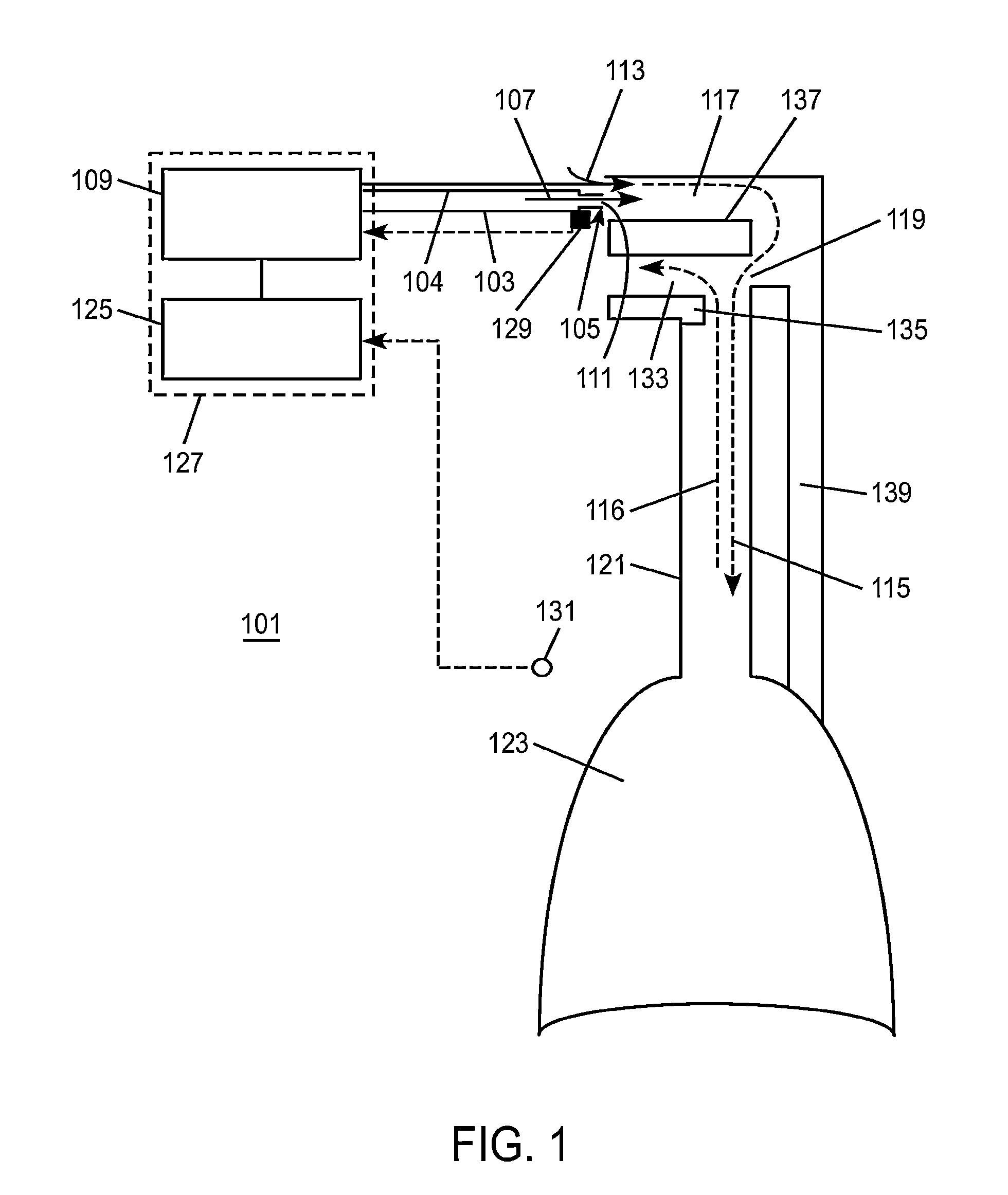
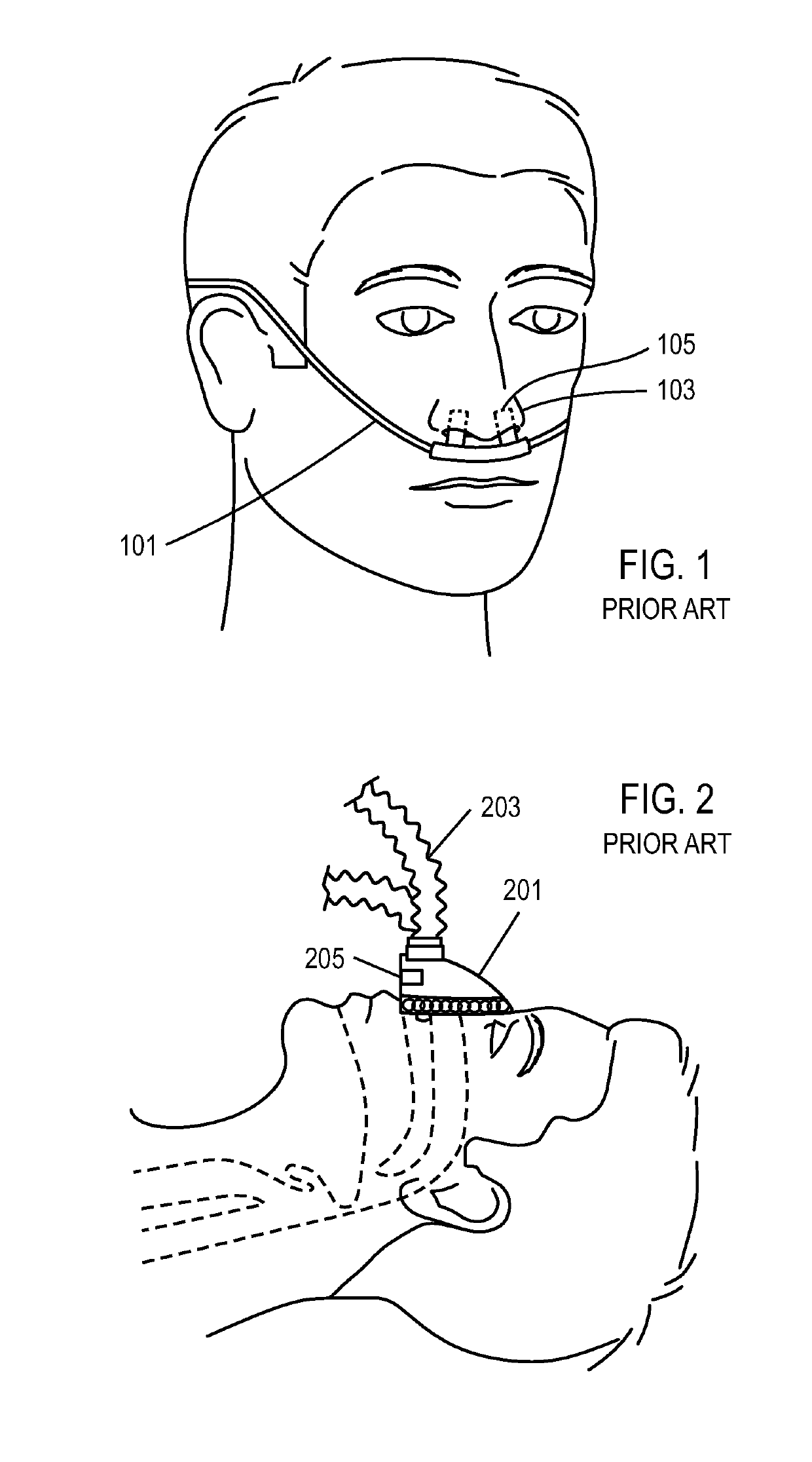
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
ActiveUS20110214676A1Avoid airway obstructionRespiratorsMedical devicesGas delivery sourceAirway pressures
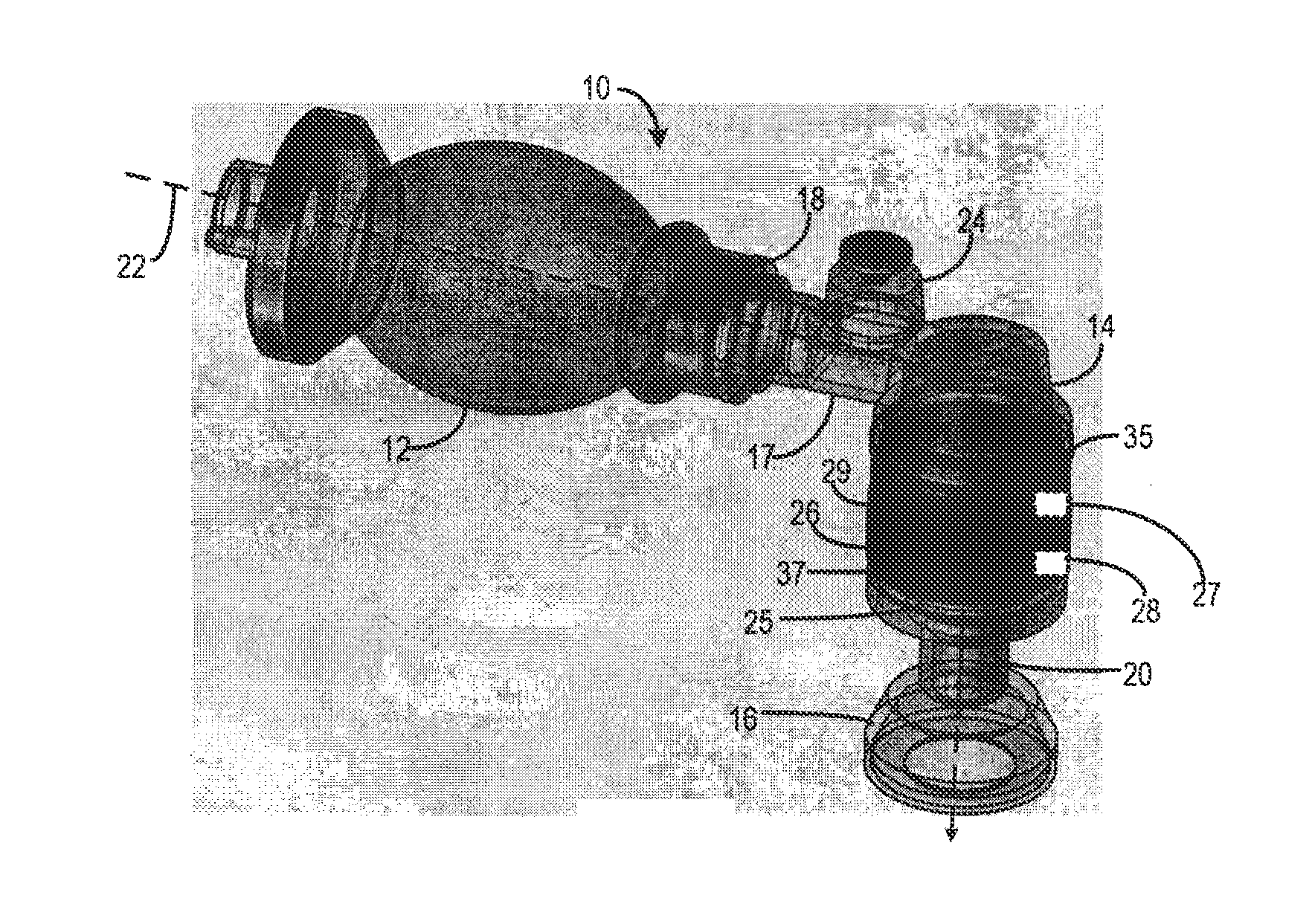
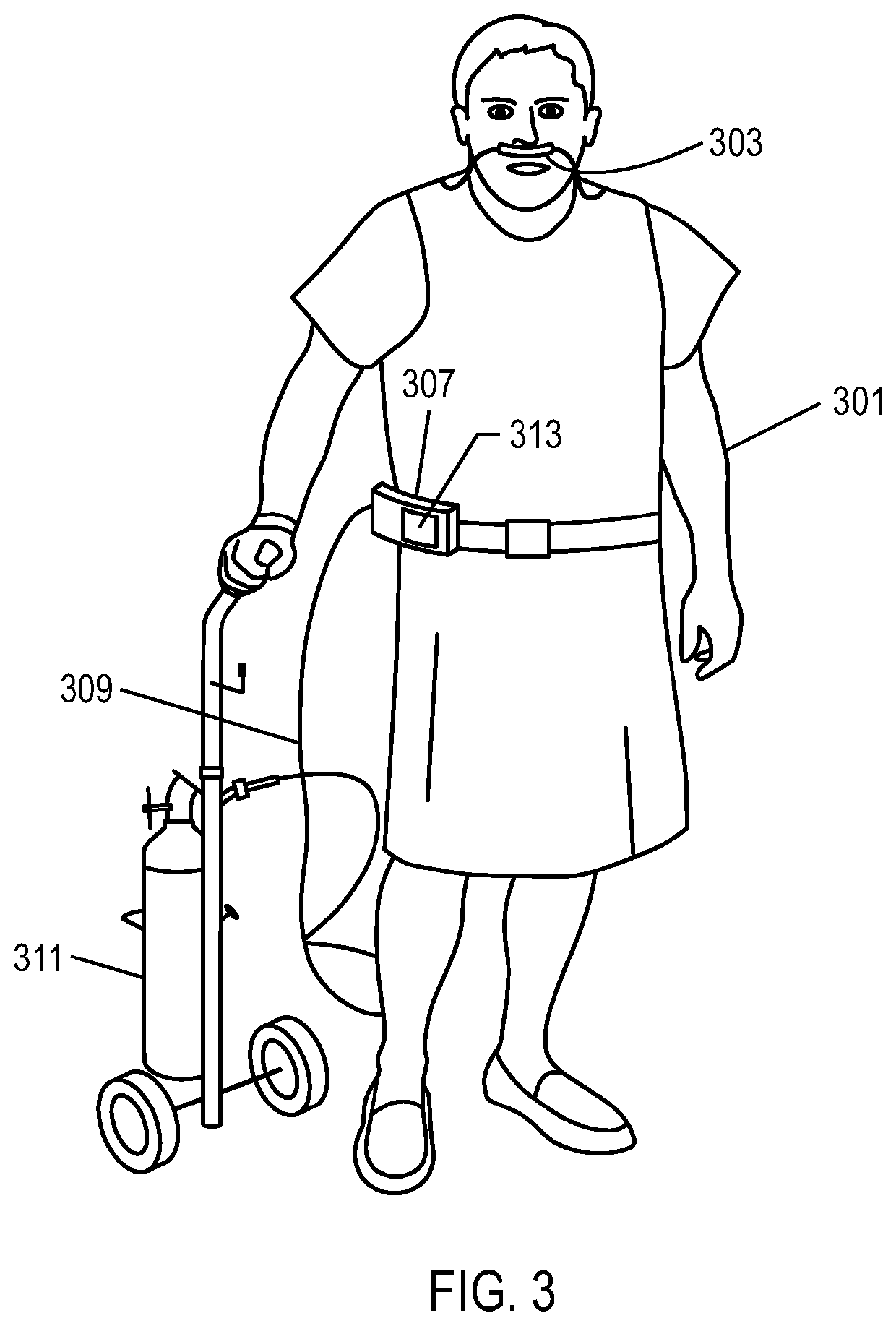
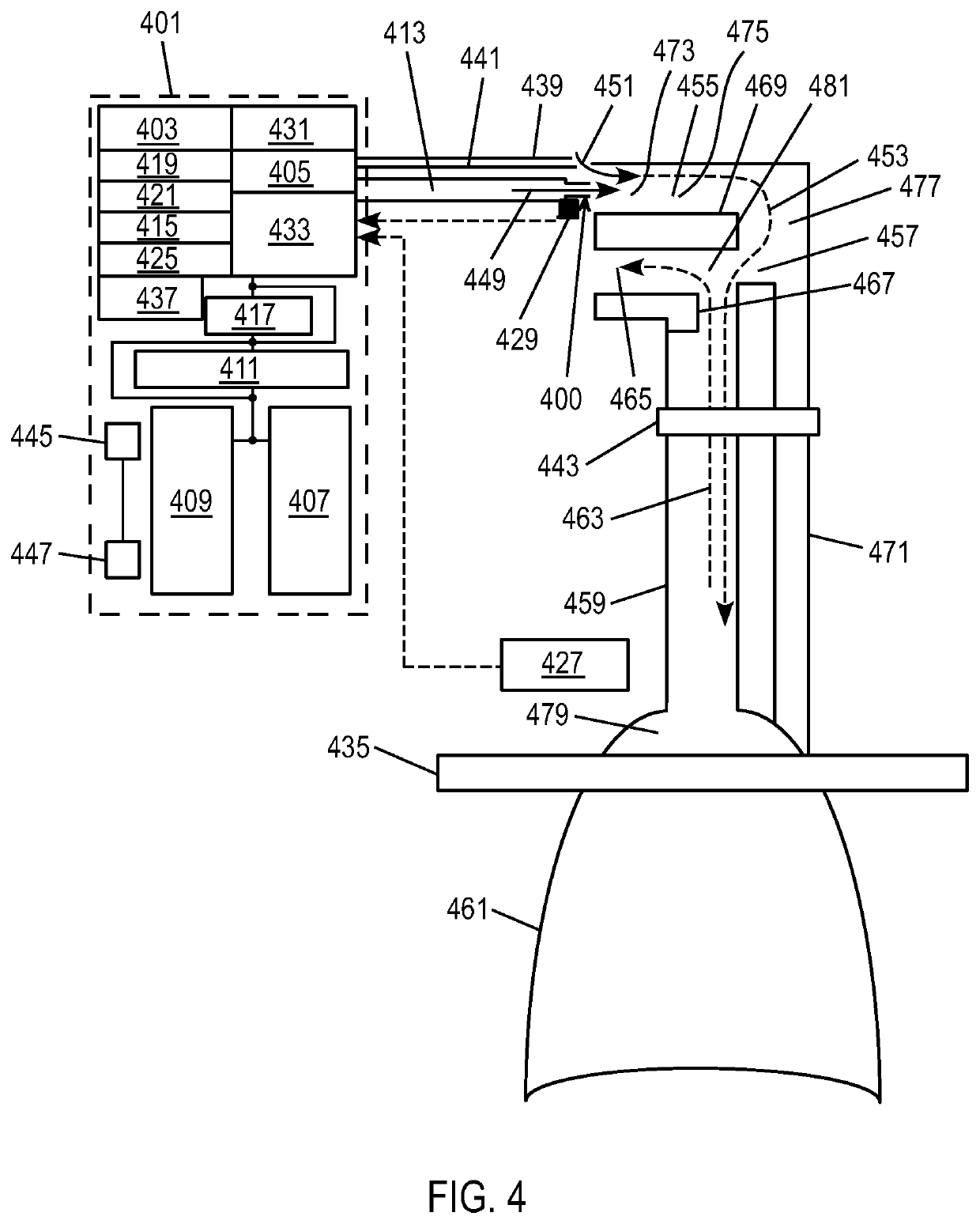
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
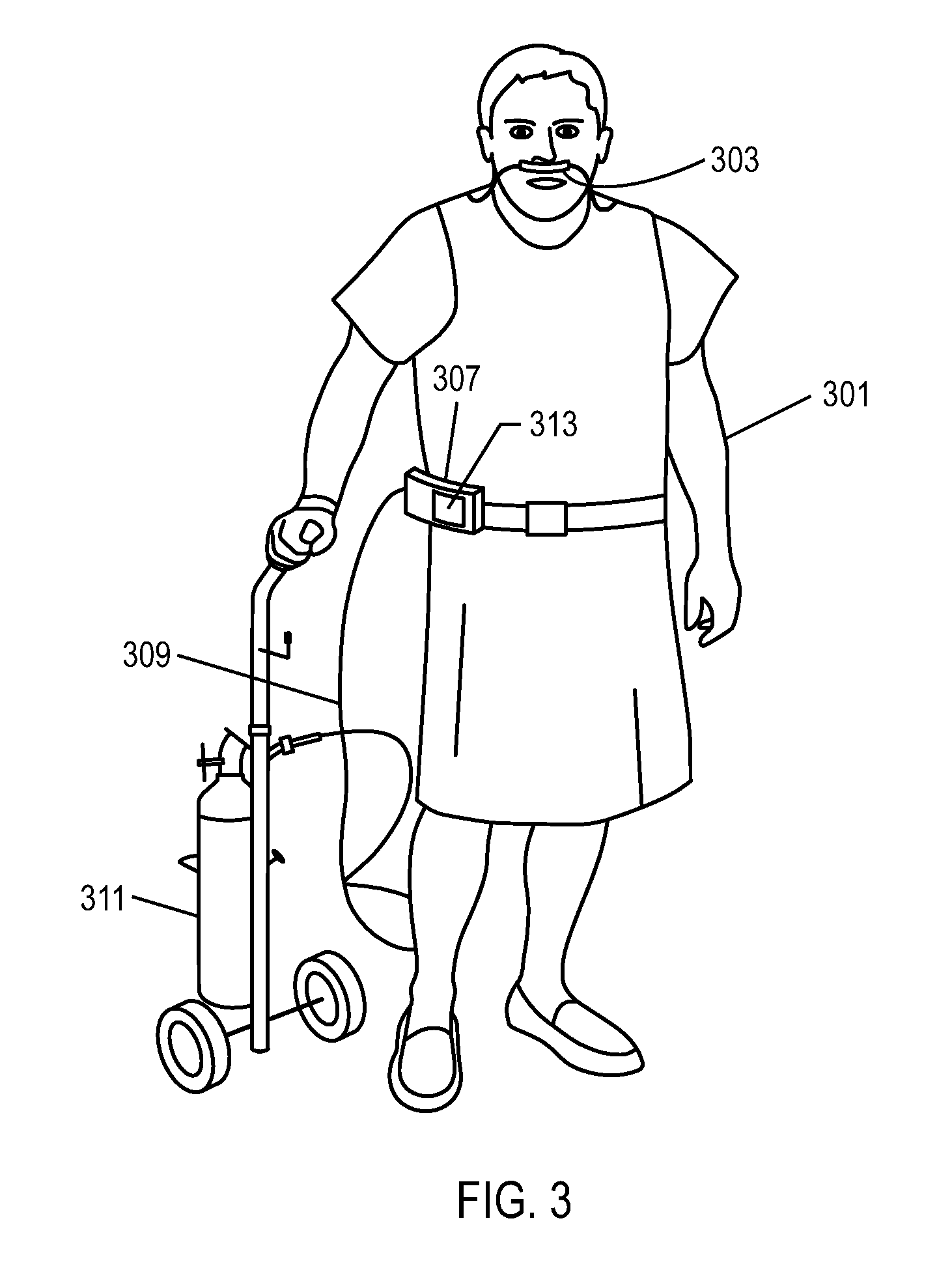
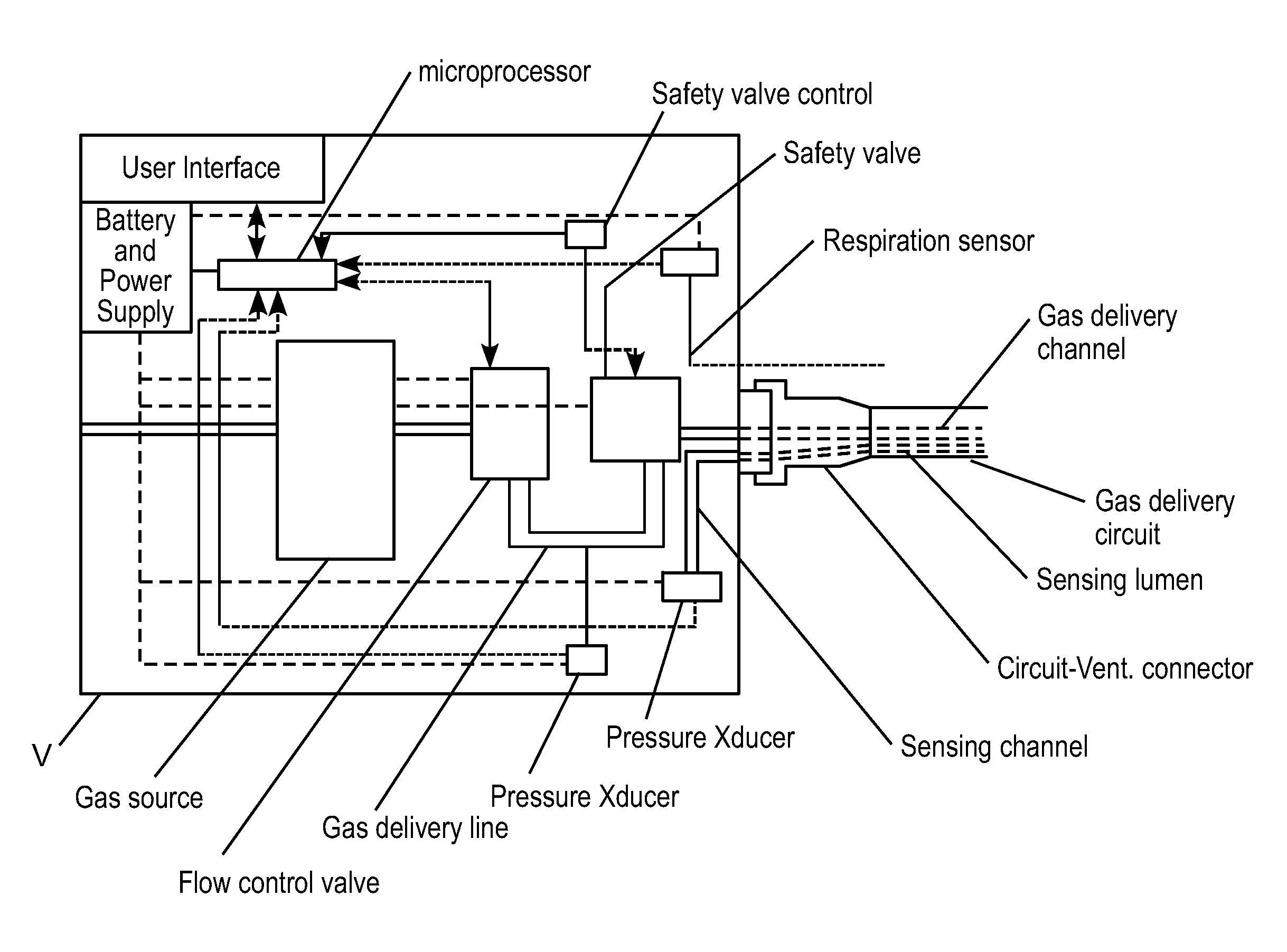
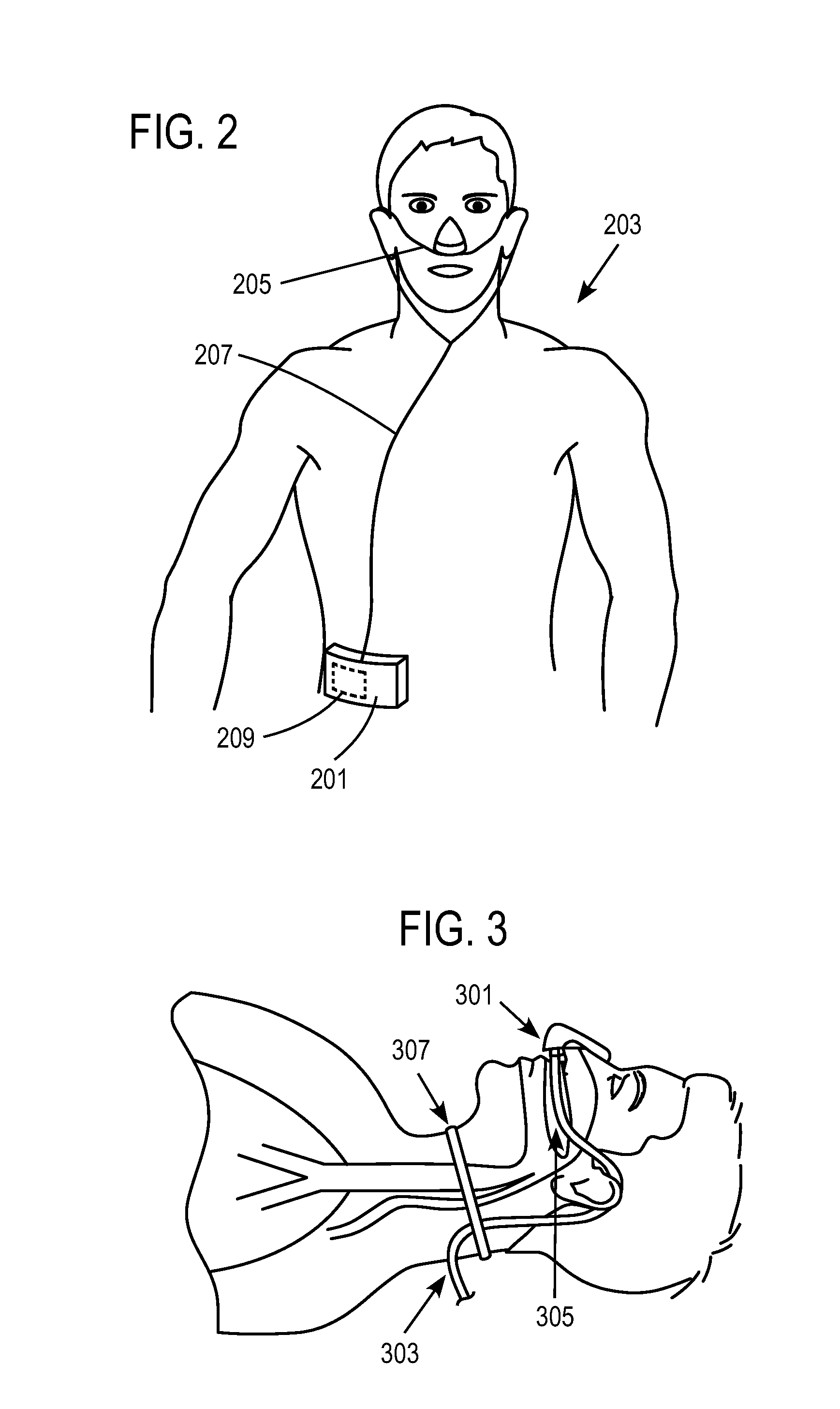
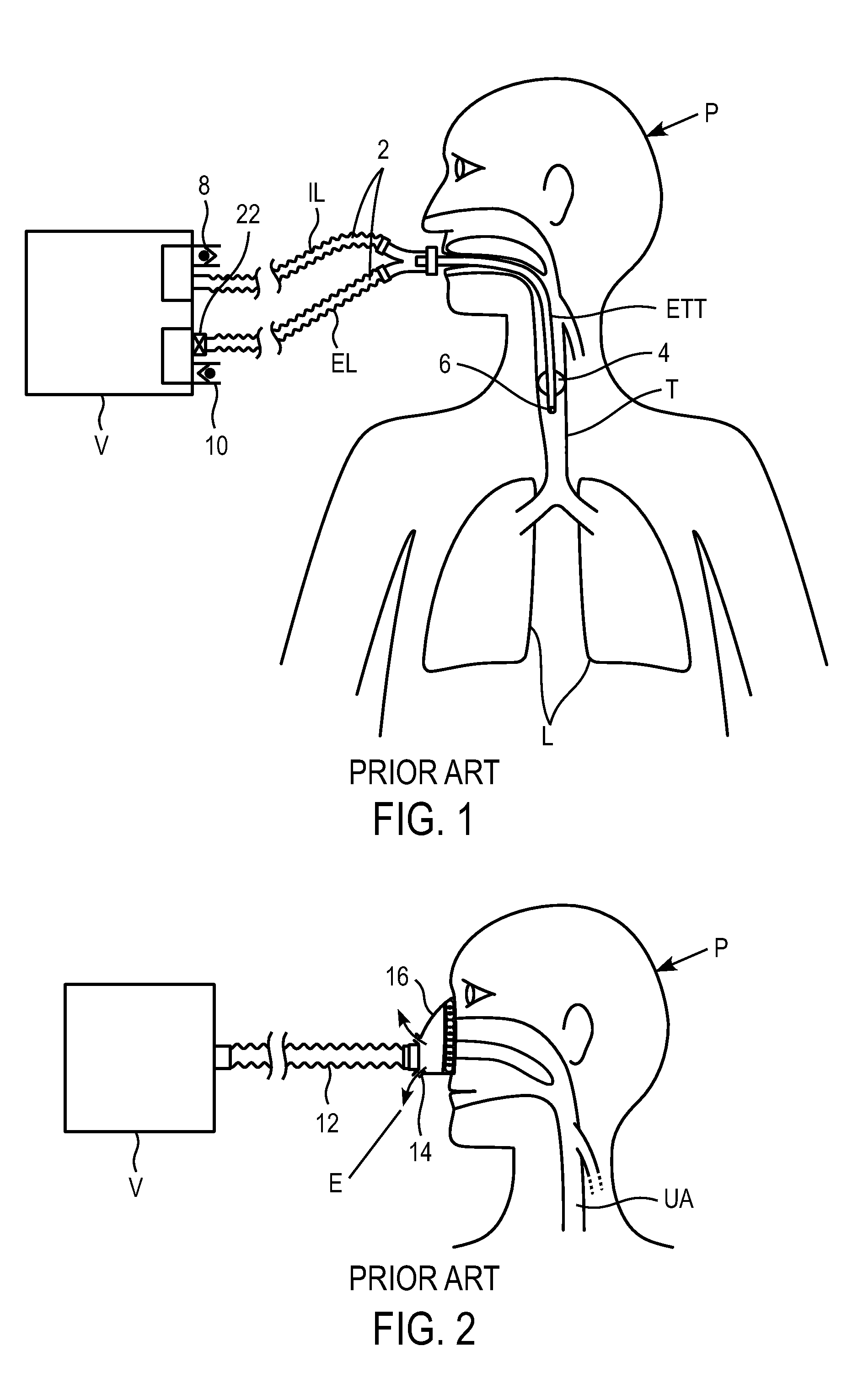
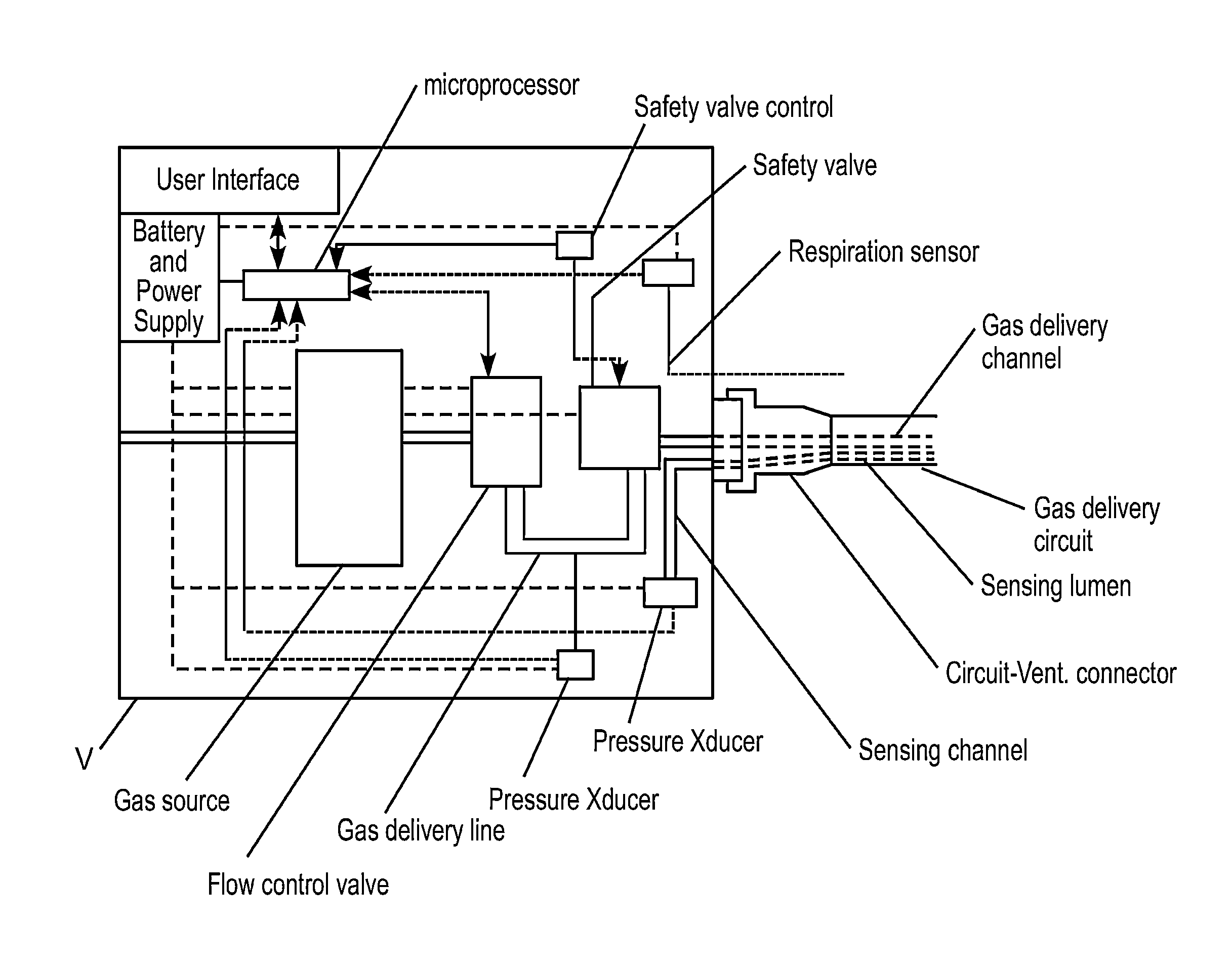
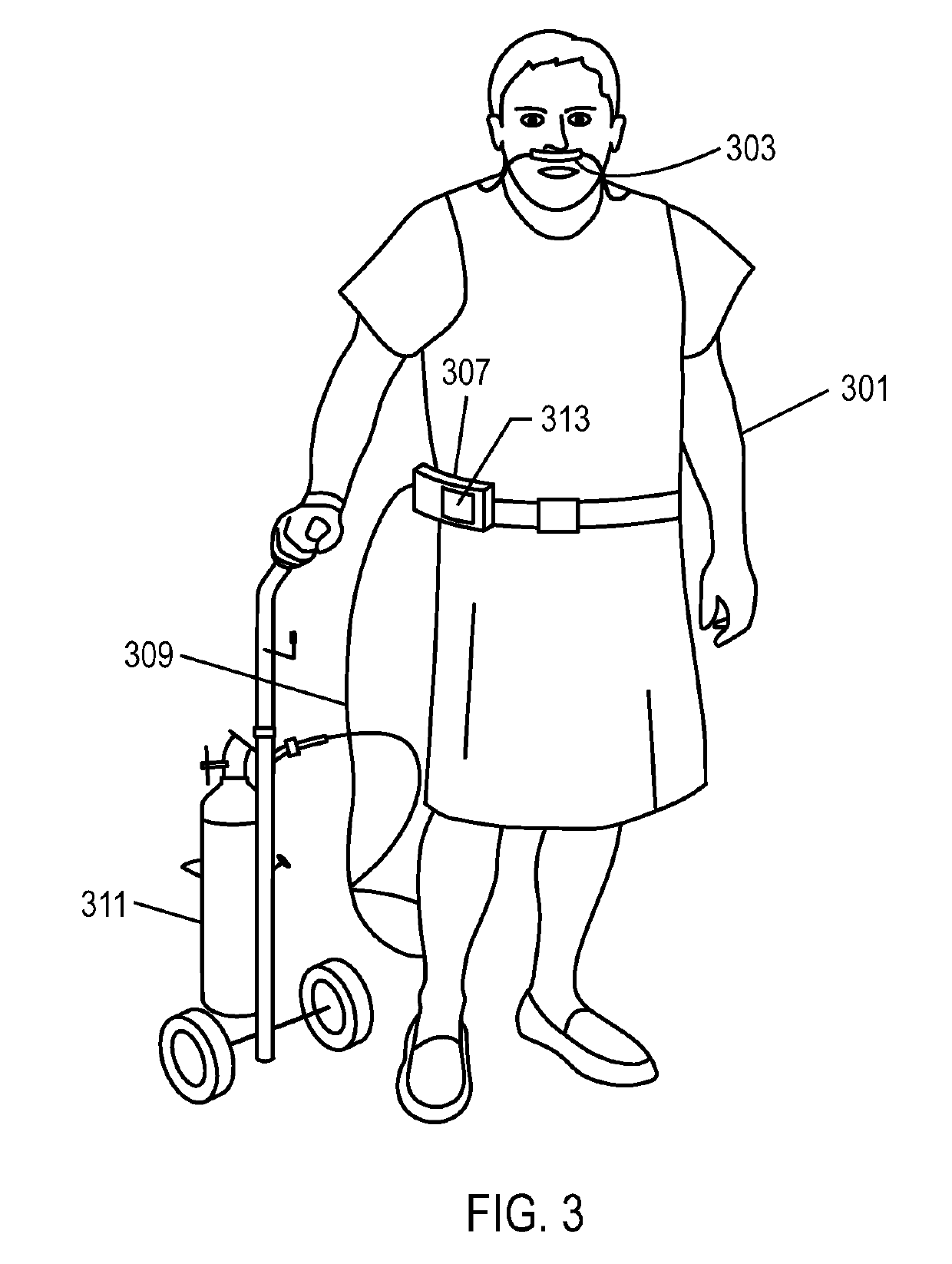
Methods, systems and devices for non-invasive open ventilation for providing ventilation support
ActiveUS20100252041A1Work lessIncrease airway pressureRespiratorsOperating means/releasing devices for valvesLung volumesNon invasive
A system for providing ventilation support to a patient may include a ventilator, a control unit, a gas delivery circuit with a proximal end in fluid communication with the ventilator and a distal end in fluid communication with a nasal interface, and a nasal interface. The nasal interface may include at least one jet nozzle at the distal end of the gas delivery circuit; and at least one spontaneous respiration sensor for detecting respiration in communication with the control unit. The system may be open to ambient. The control unit may receive signals from the at least one spontaneous respiration sensor and determine gas delivery requirements. The ventilator may deliver gas at a velocity to entrain ambient air and increase lung volume or lung pressure above spontaneously breathing levels to assist in work of breathing, and deliver ventilation gas in a cyclical delivery pattern synchronized with a spontaneous breathing pattern.
Owner:BREATHE TECHNOLOGIES INC
Methods, systems and devices for non-invasive open ventilation with gas delivery nozzles in free space
ActiveUS20100252039A1Work lessIncrease airway pressureRespiratorsOperating means/releasing devices for valvesNoseLung volumes
A non-invasive ventilation system may include an interface. The interface may include at least one gas delivery jet nozzle adapted to be positioned in free space and aligned to directly deliver ventilation gas into an entrance of a nose. The at least one gas delivery jet nozzle may be connected to a pressurized gas supply. The ventilation gas may entrain ambient air to elevate lung pressure, elevate lung volume, decrease the work of breathing or increase airway pressure, and wherein the ventilation gas is delivered in synchrony with phases of breathing. A support for the at least one gas delivery jet nozzle may be provided. A breath sensor may be in close proximity to the entrance of the nose. A patient may spontaneous breathe ambient air through the nose without being impeded by the interface.
Owner:BREATHE TECHNOLOGIES INC
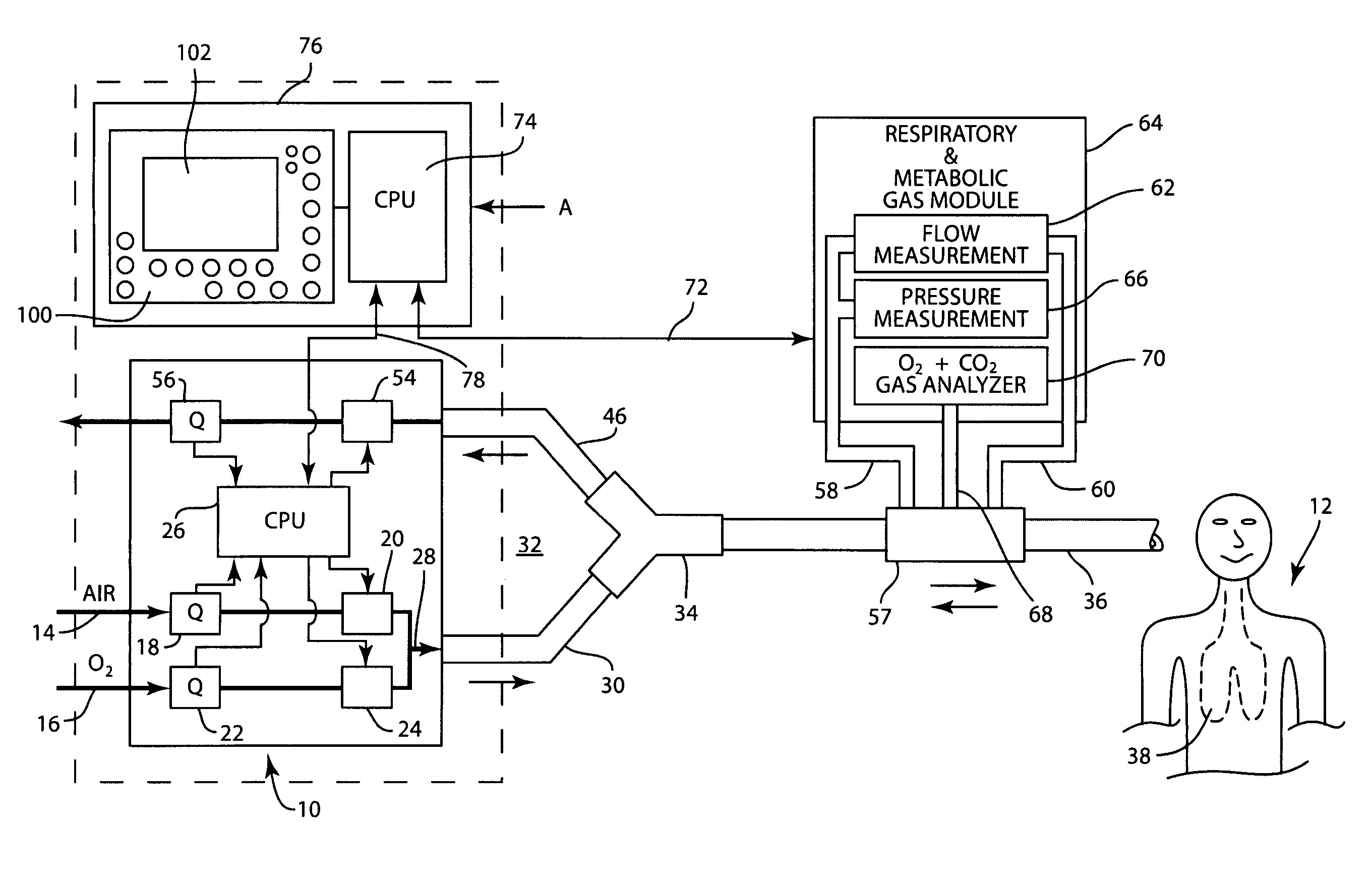
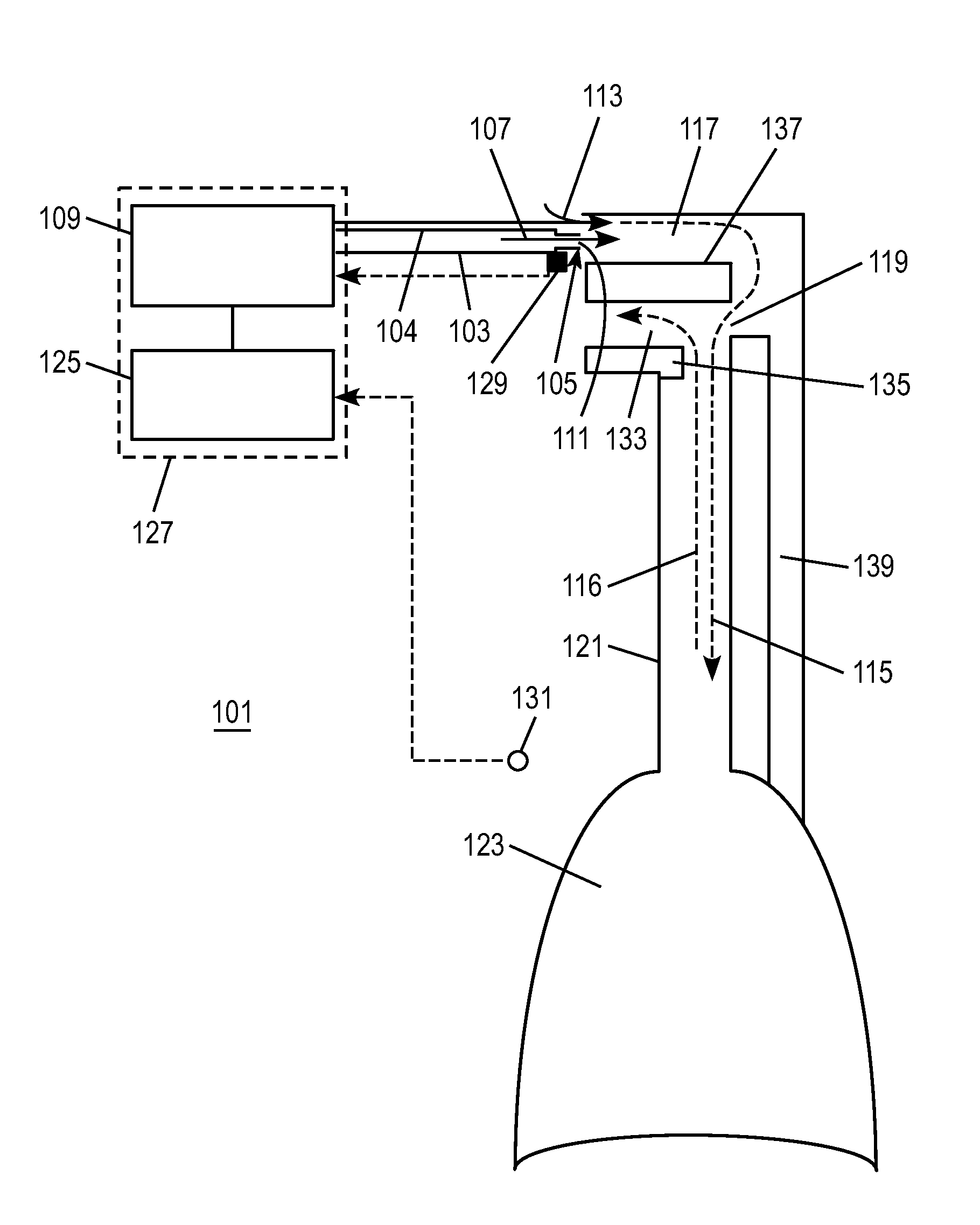
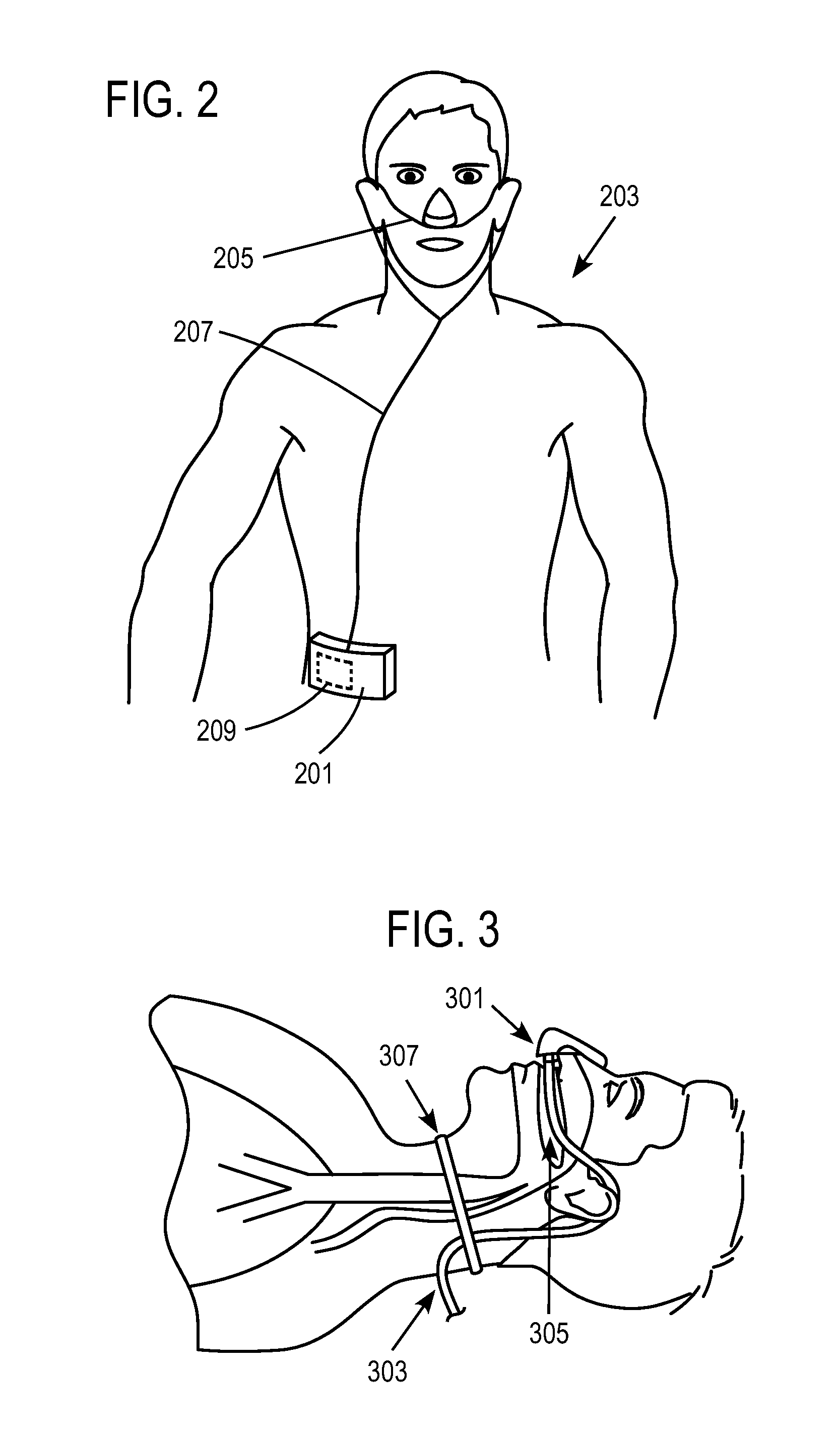
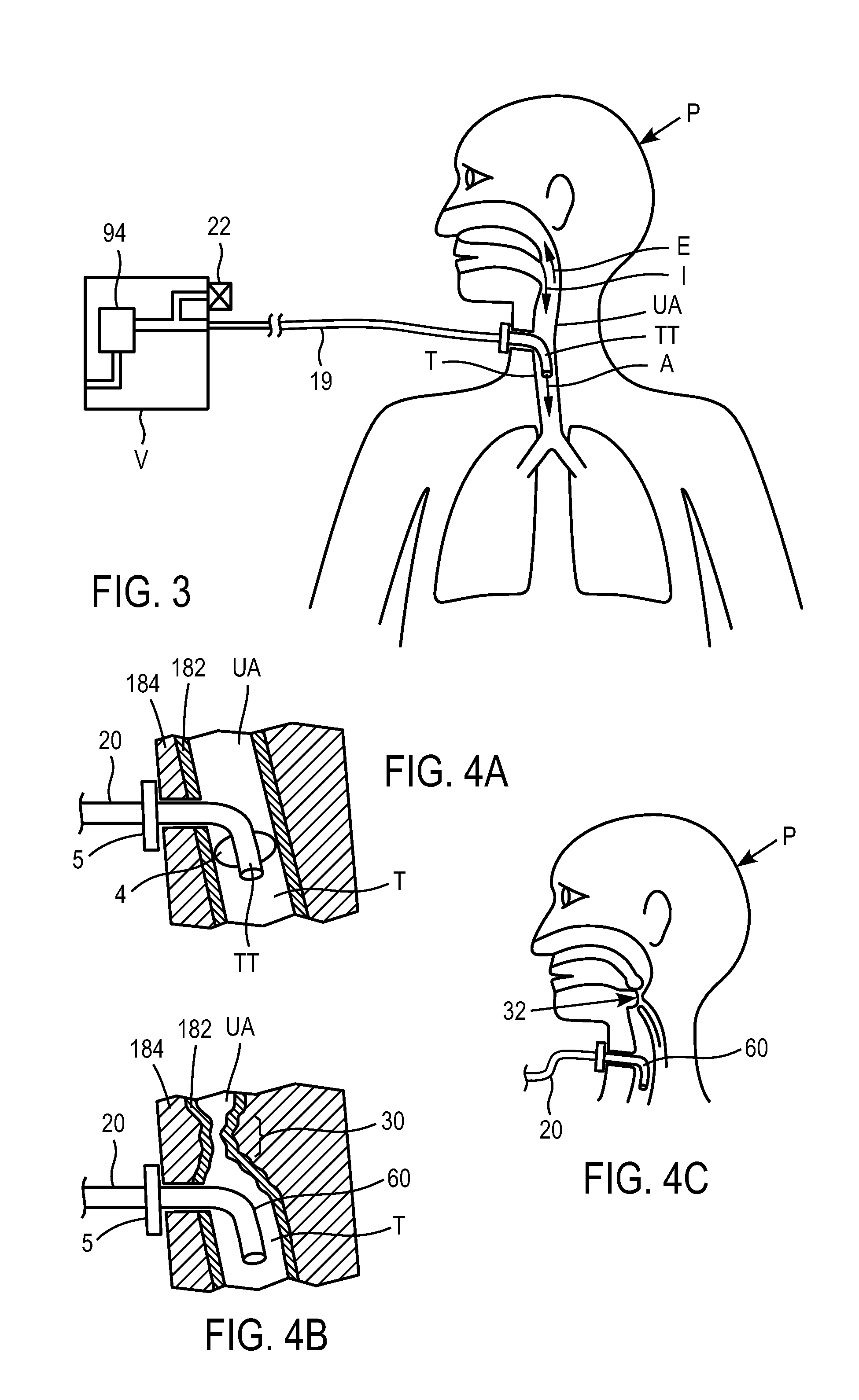
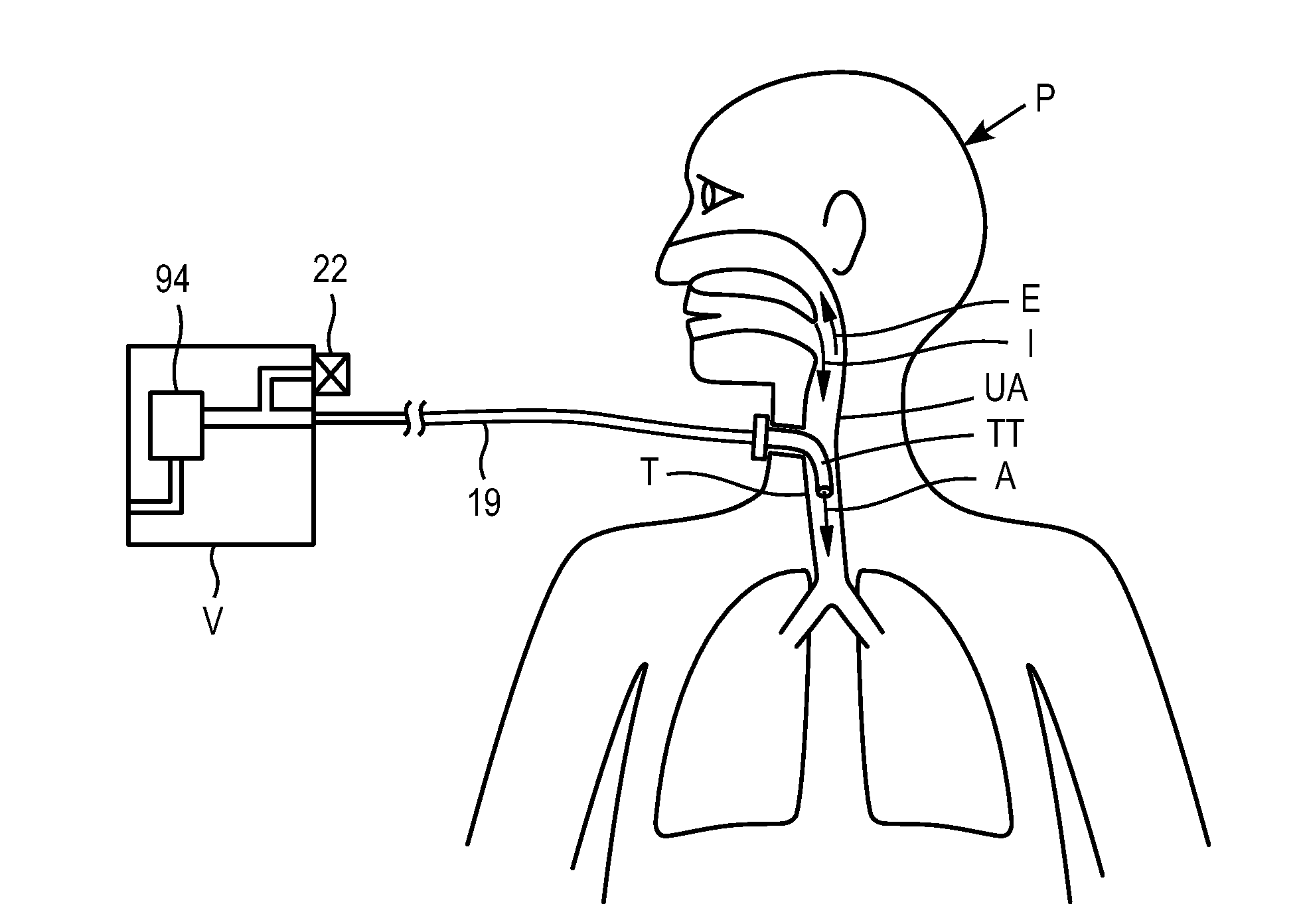
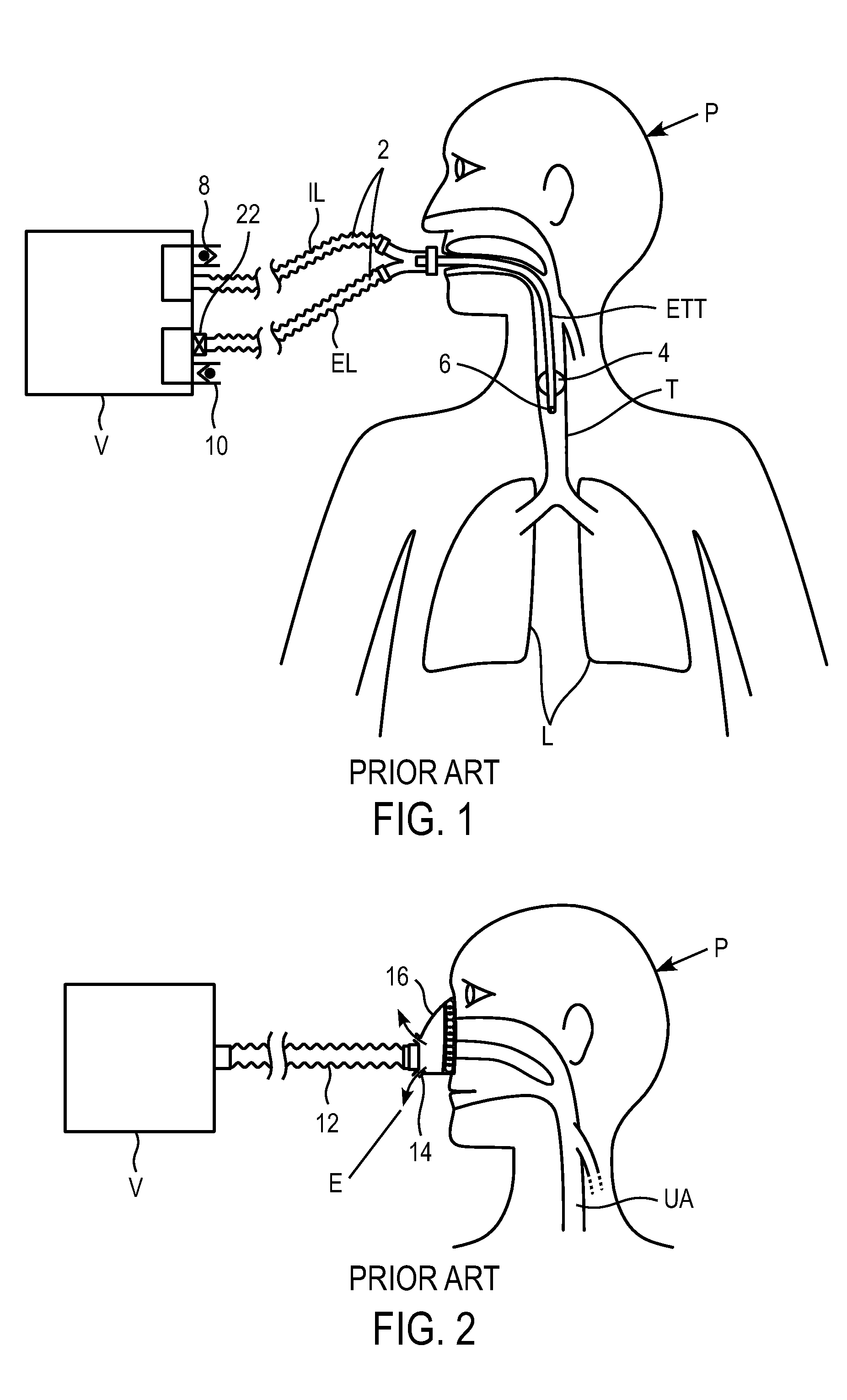
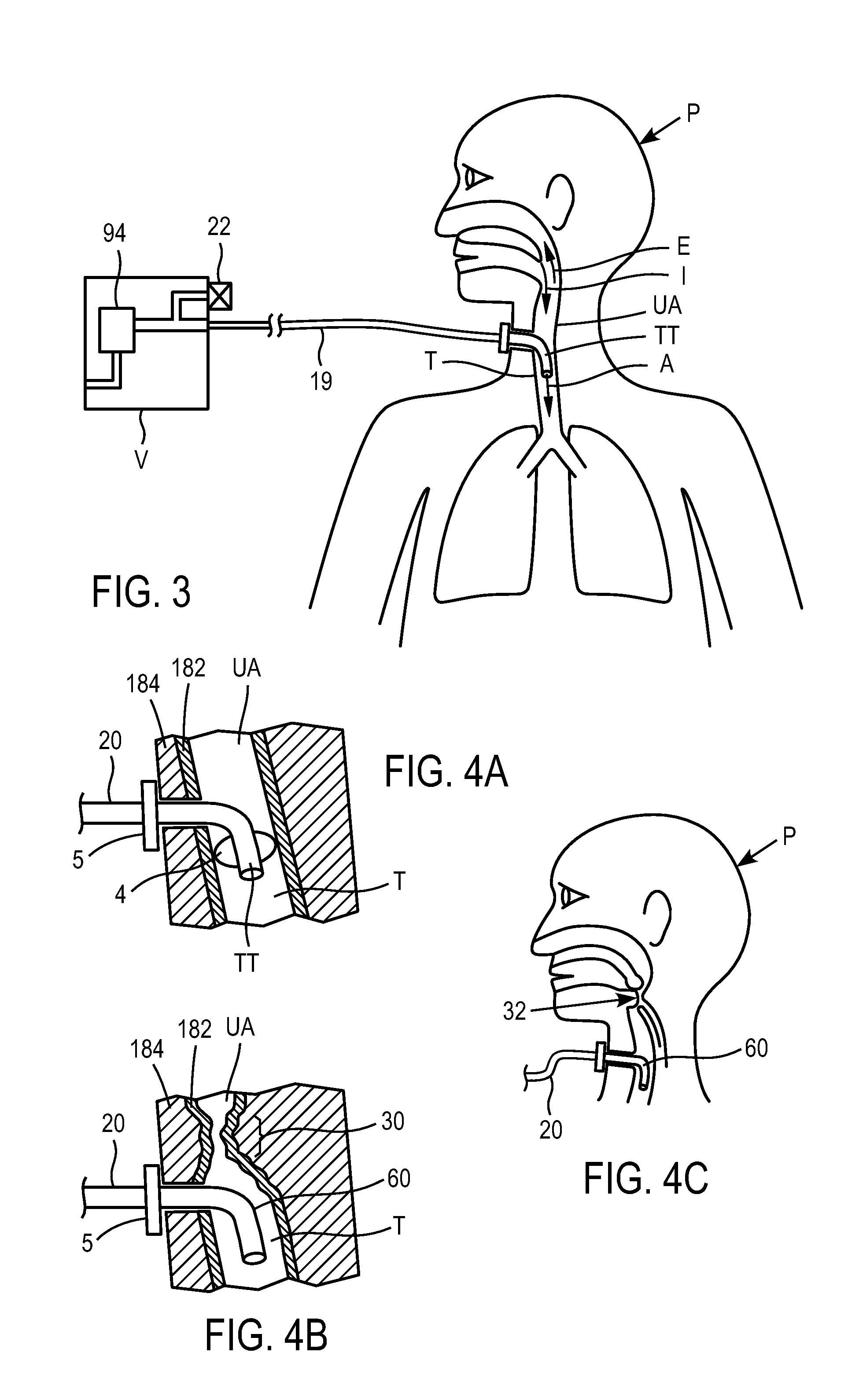
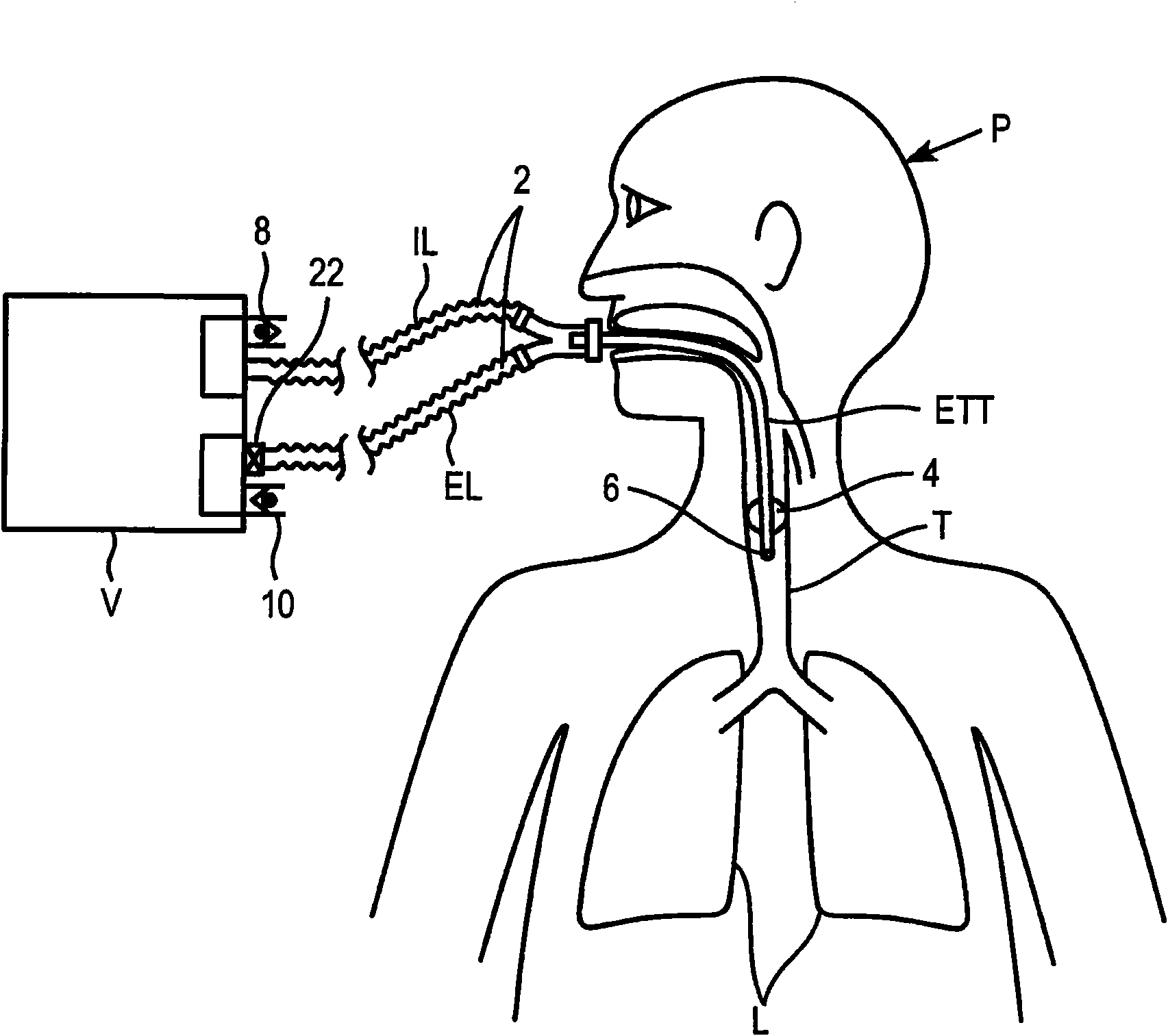
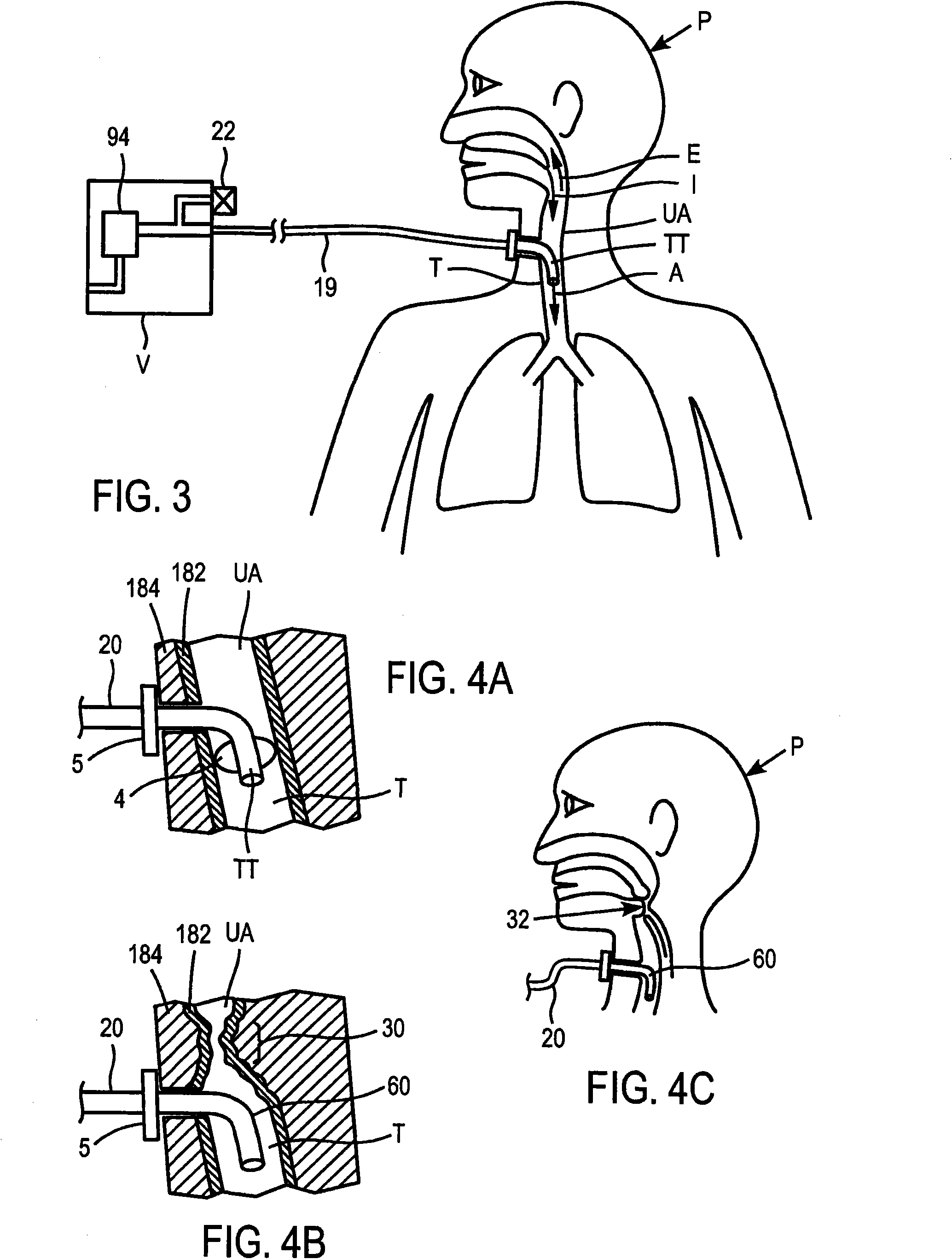
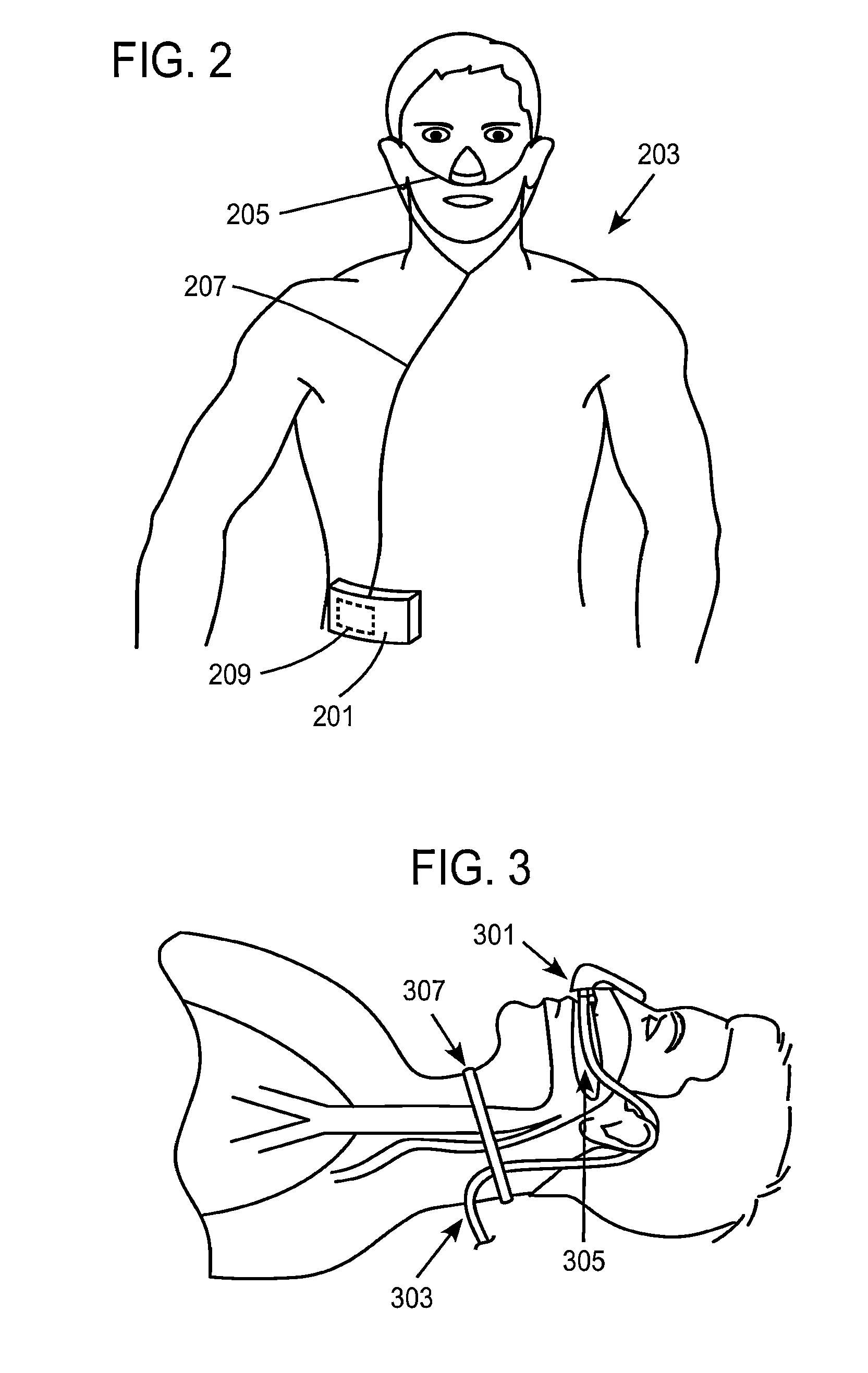
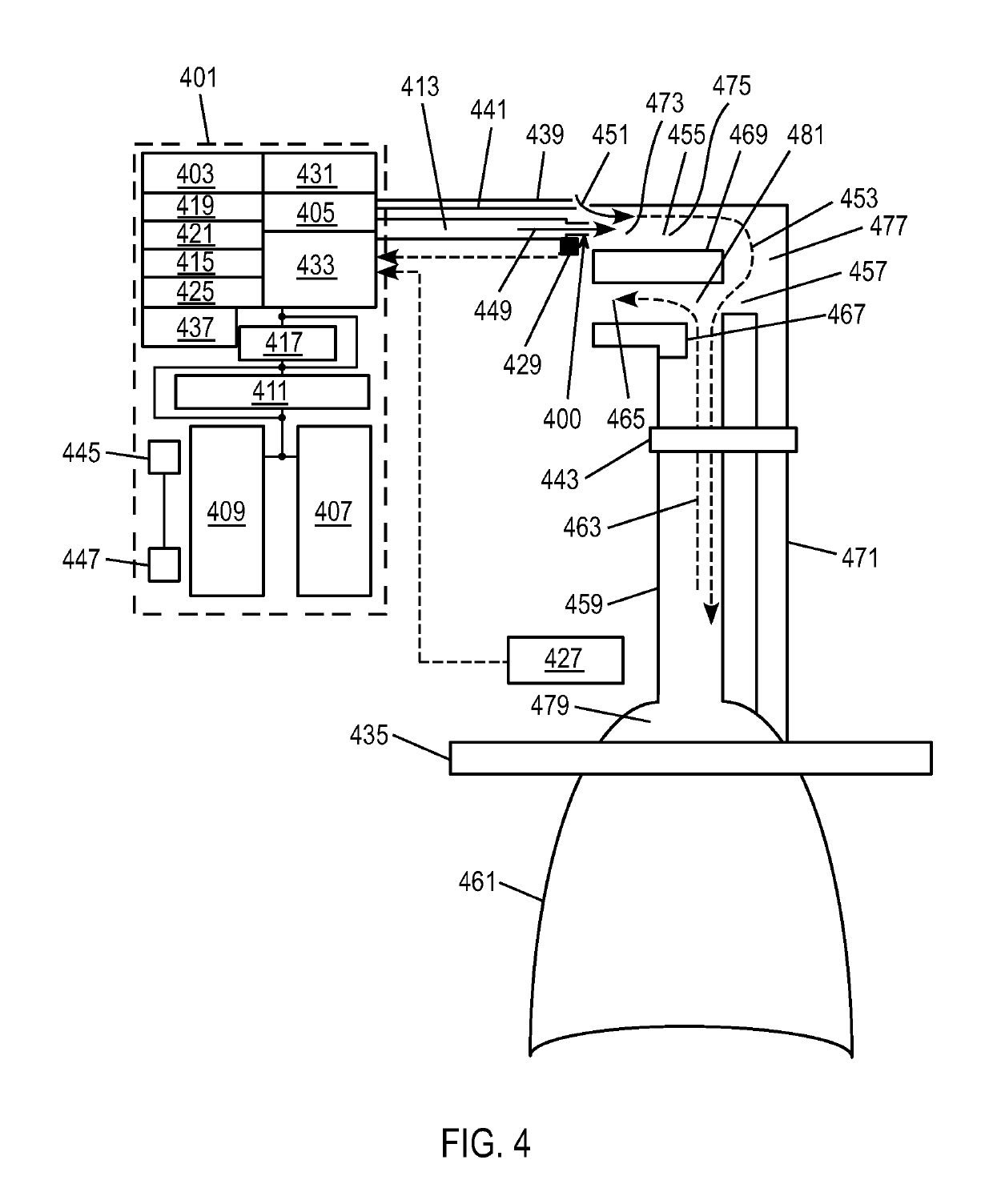
Methods and devices for providing inspiratory and expiratory flow relief during ventilation therapy
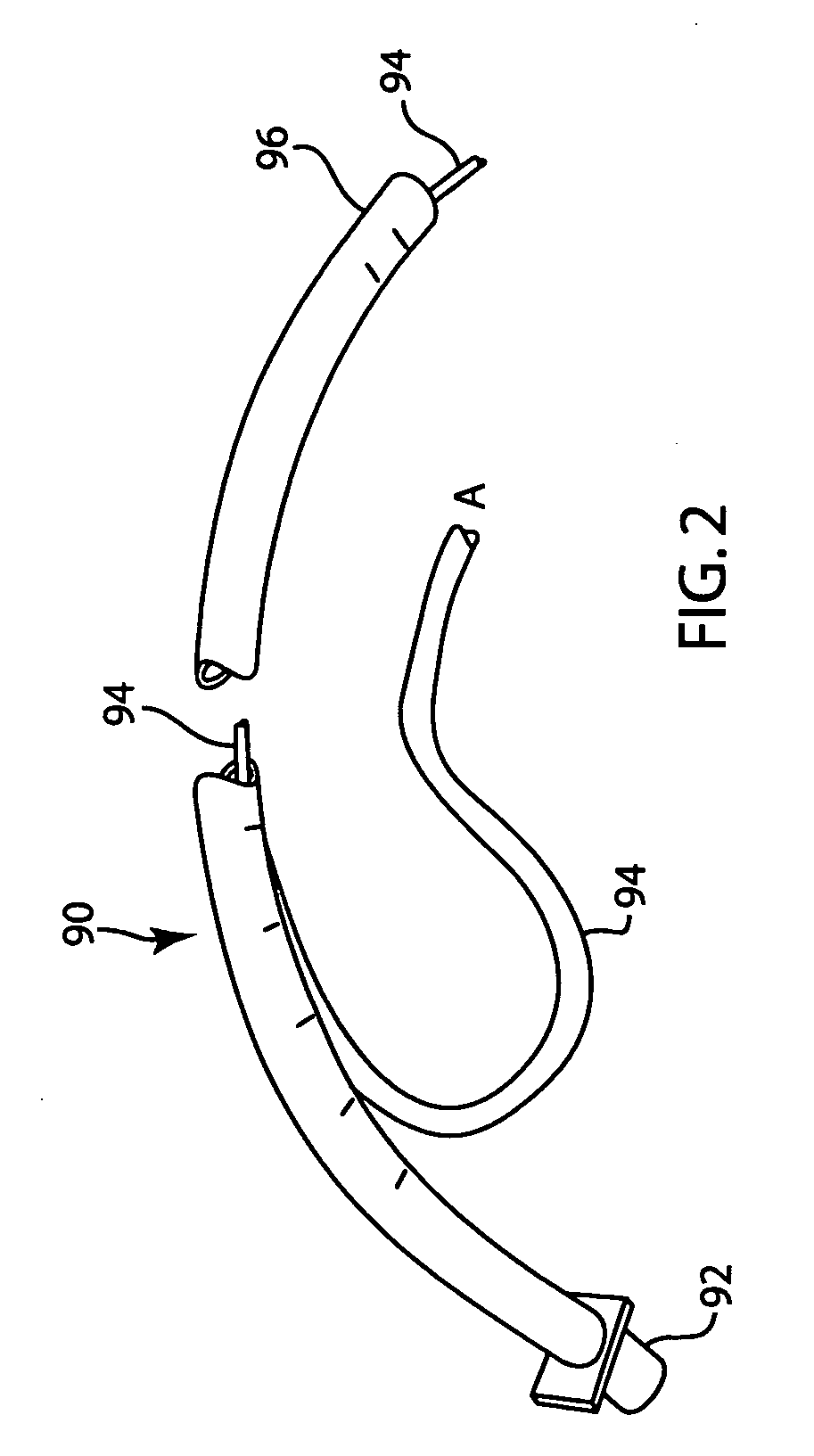
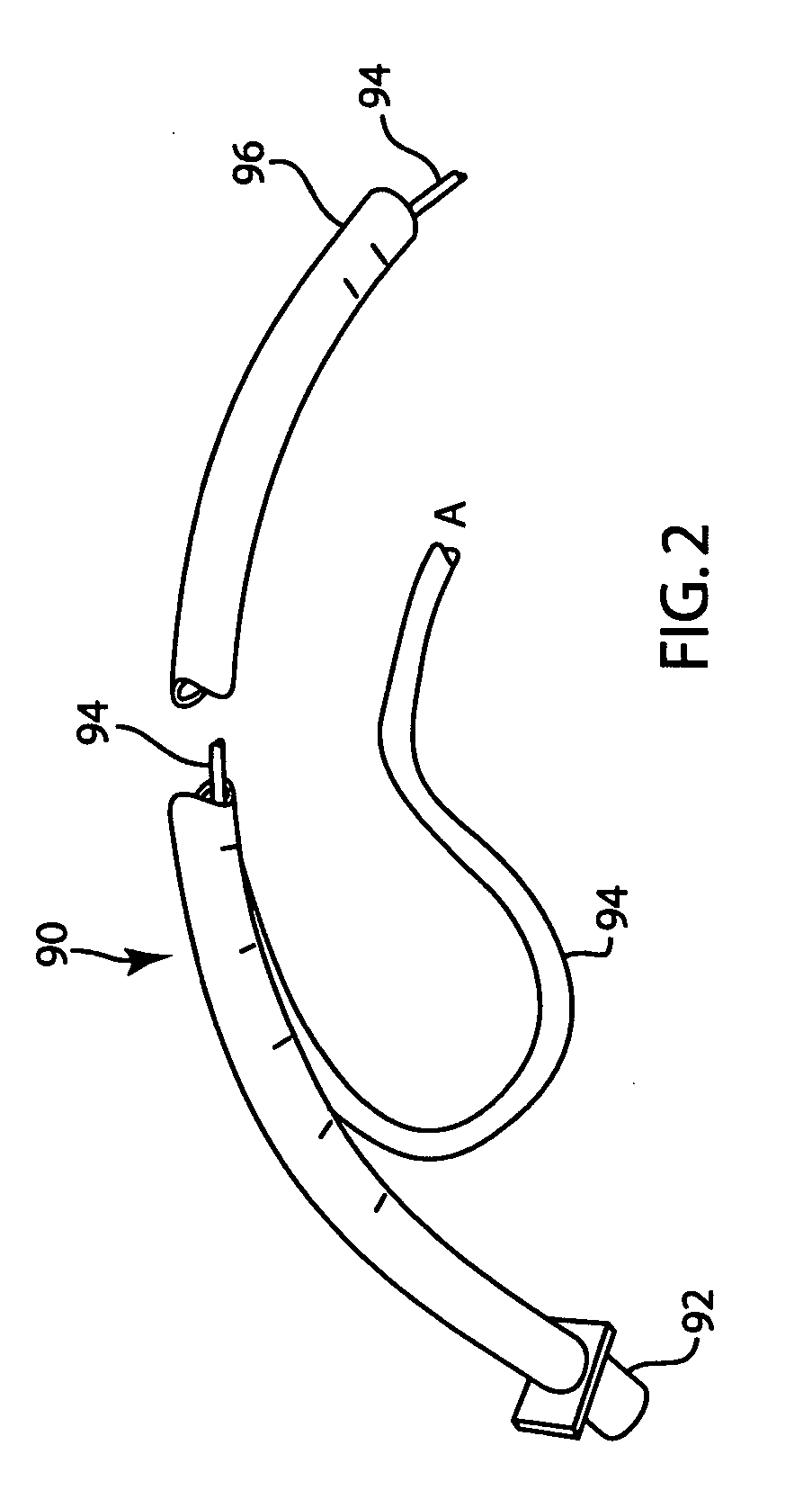
ActiveUS20090151724A1Breathe freelyUndesirable pressureRespiratorsOperating means/releasing devices for valvesRespiratory supportAirway pressures
Respiratory support and / or controlled mechanical ventilation of a patient are provided. A ventilation apparatus may include a ventilator, a transtracheal prosthesis, and a respiratory relief device. The transtracheal prostheses and ventilation catheter may be arranged such that the patient can breathe freely through the upper airway and / or the tracheal prostheses. Respiratory sensors may measure a breathing rate, lung pressure, airway pressure, or a combination thereof. Pulses of gas may be provided to the patient through the ventilation catheter during inspiration. The pulses may have a first volume while the patient breathes normal and a second volume when the sensors detect a cessation of breathing or reduction in breathing volume. The second volume may be provided at 1-5 times the normal breathing rate, with a volume 25-500% times the first volume, or both.
Owner:BREATHE TECHNOLOGIES INC
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
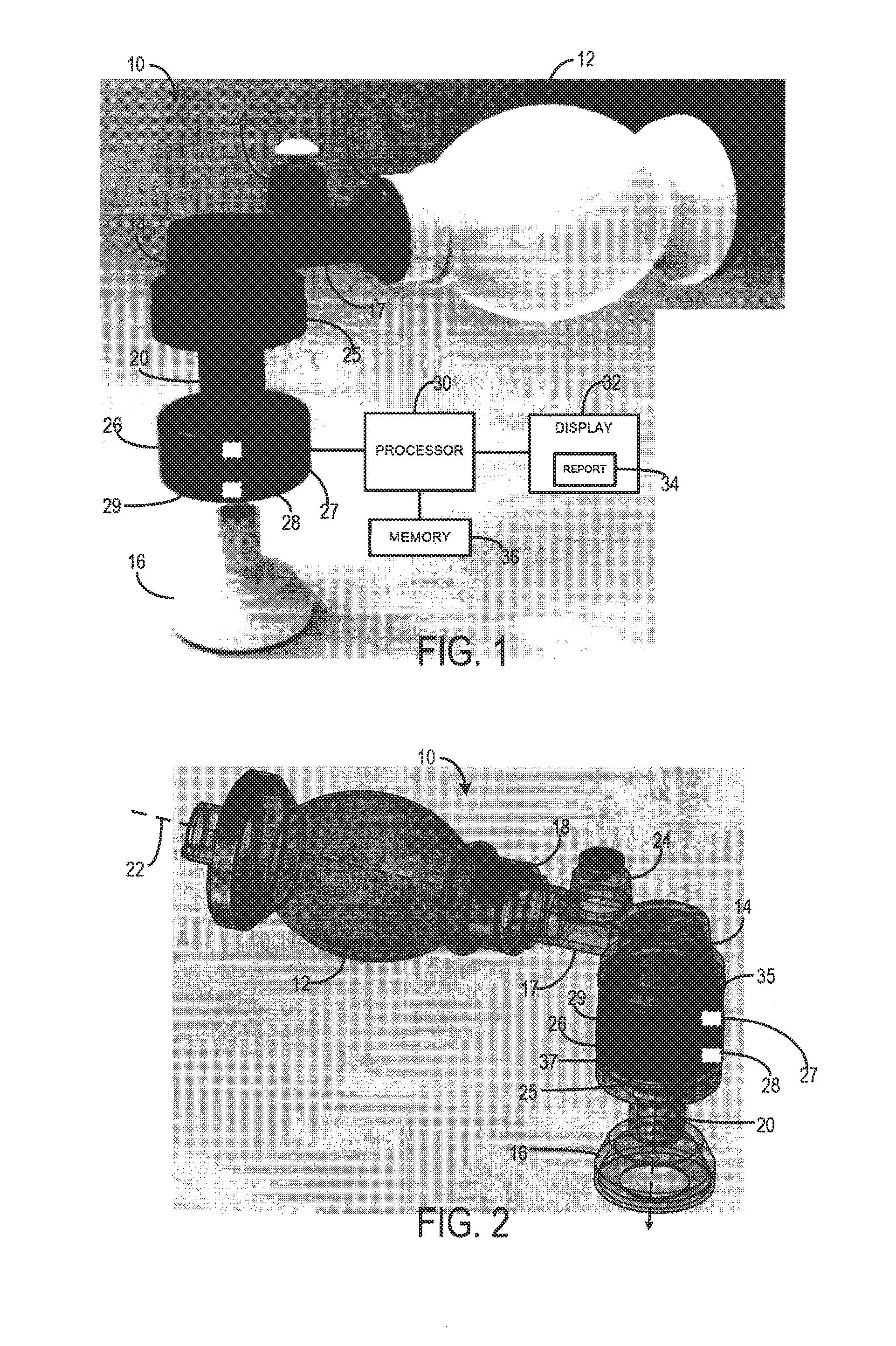
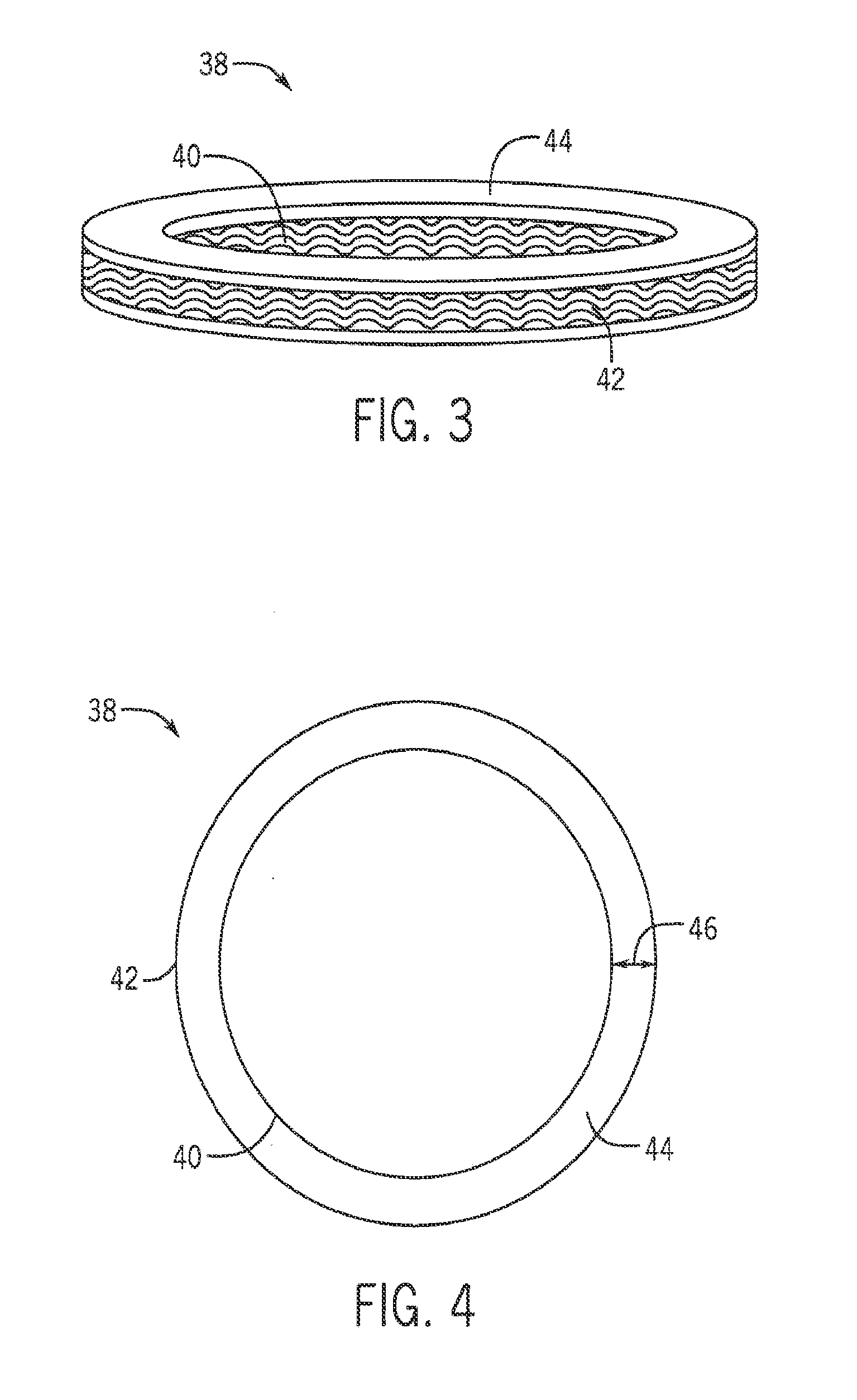
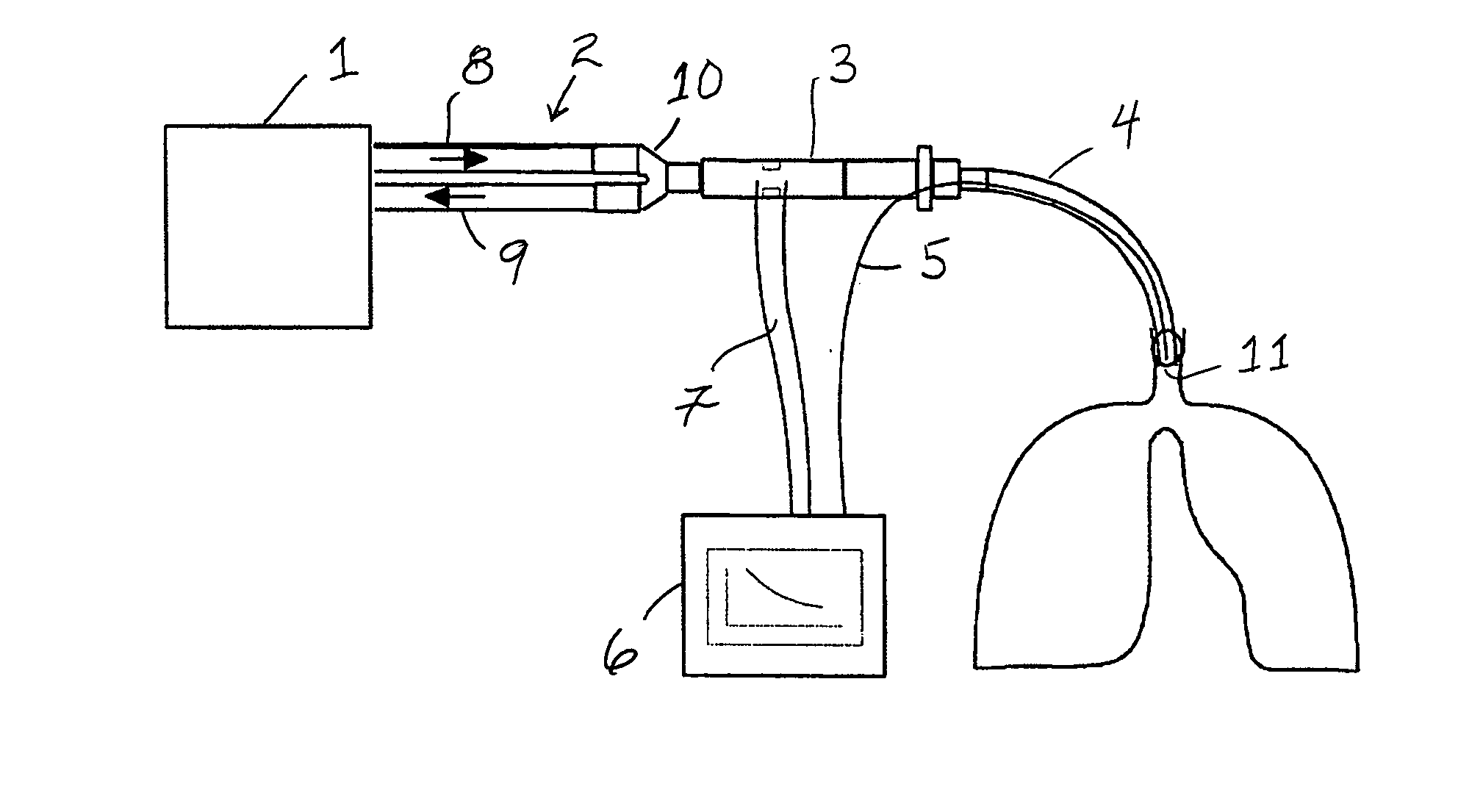
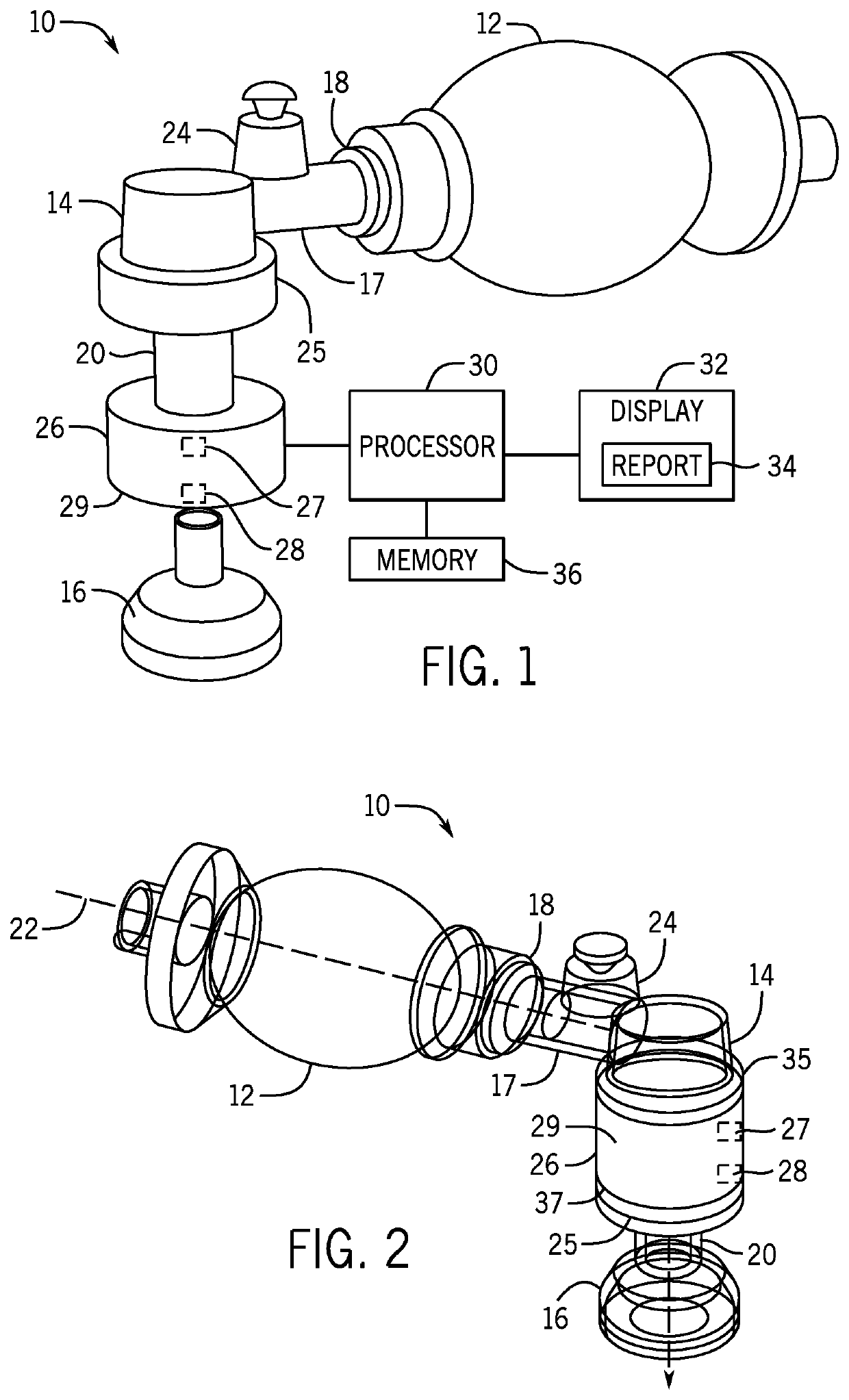
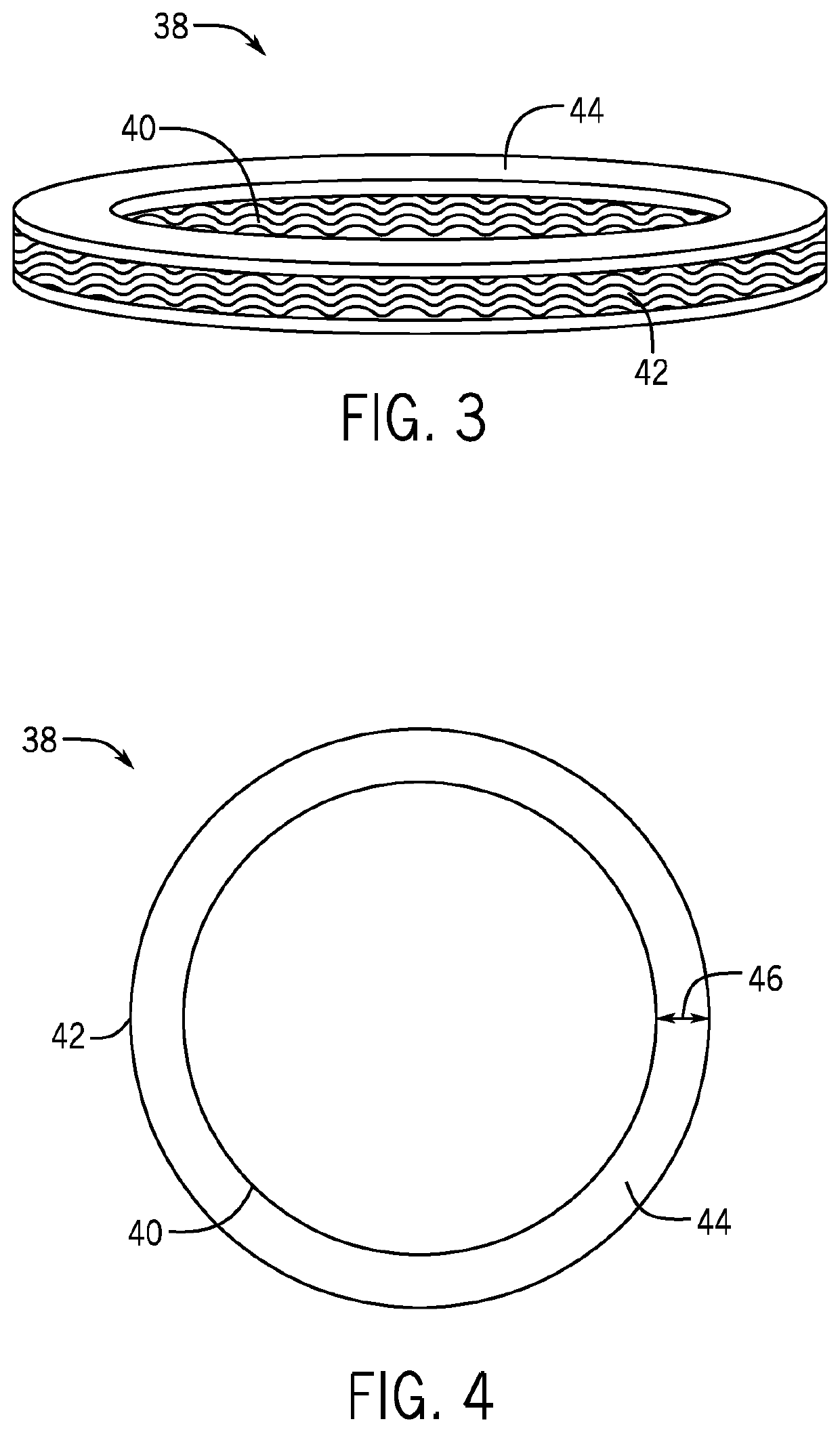
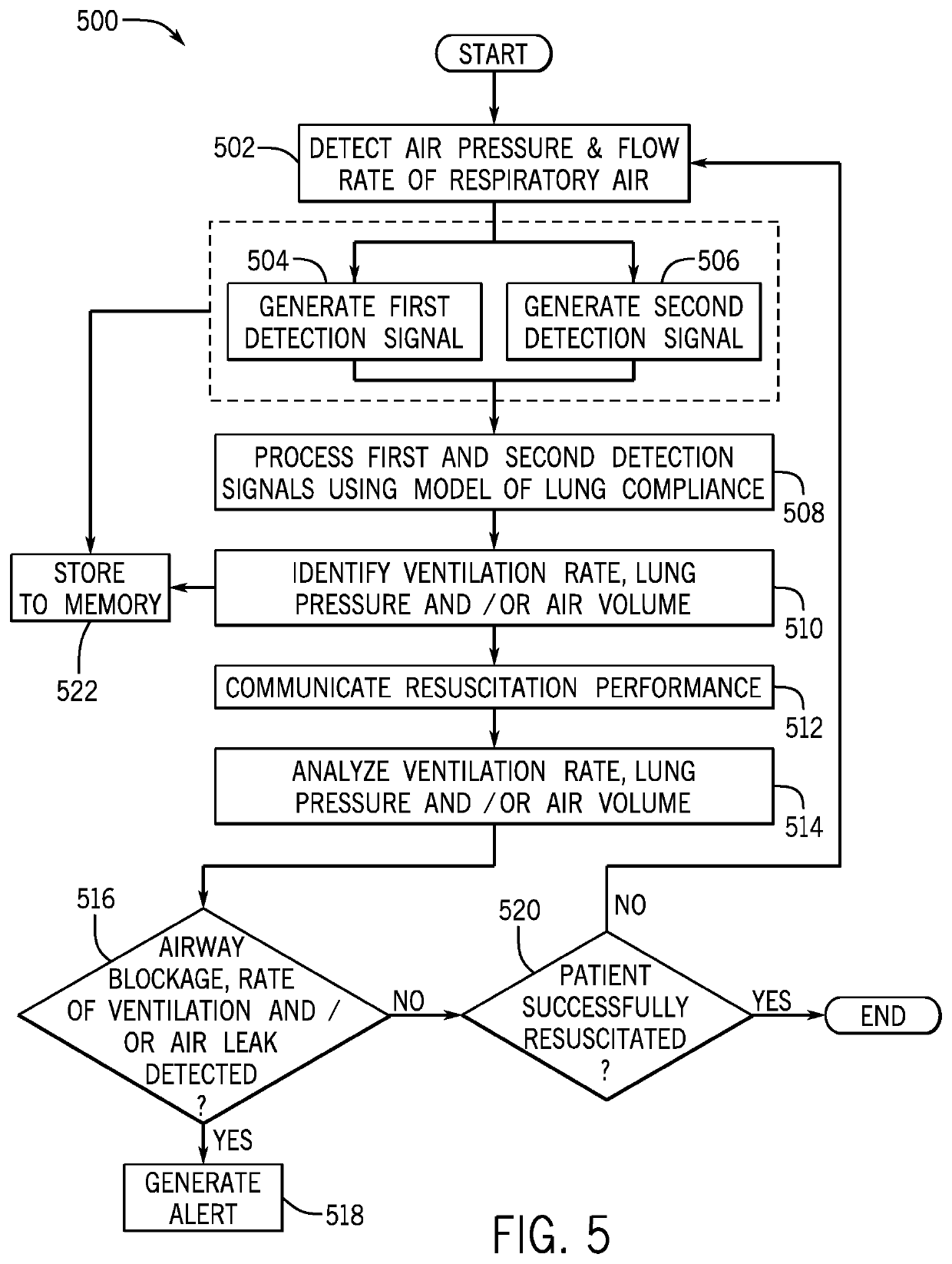
System and method for monitoring resuscitation or respiratory mechanics of a patient
ActiveUS20150283342A1Overcomes drawbackTracheal tubesRespiratory device testingAir volumeLung pressure
A system and method for monitoring resuscitation and respiratory mechanics of a patient is provided. A pressure sensor detects air pressure within an air-flow path of a resuscitator and generates a first detection signal in response thereto. A flow-rate sensor detects the flow-rate within the air-flow path and generates a second detection signal In response thereto. A processor receives and processes the first and second detection signals using an algorithm to identify a ventilation rate, a lung pressure, and an air volume corresponding to the respiratory air. A report is generated of real-time feedback about respiration of the patient that includes the ventilation rate, lung pressure, and air volume.
Owner:THE GENERAL HOSPITAL CORP
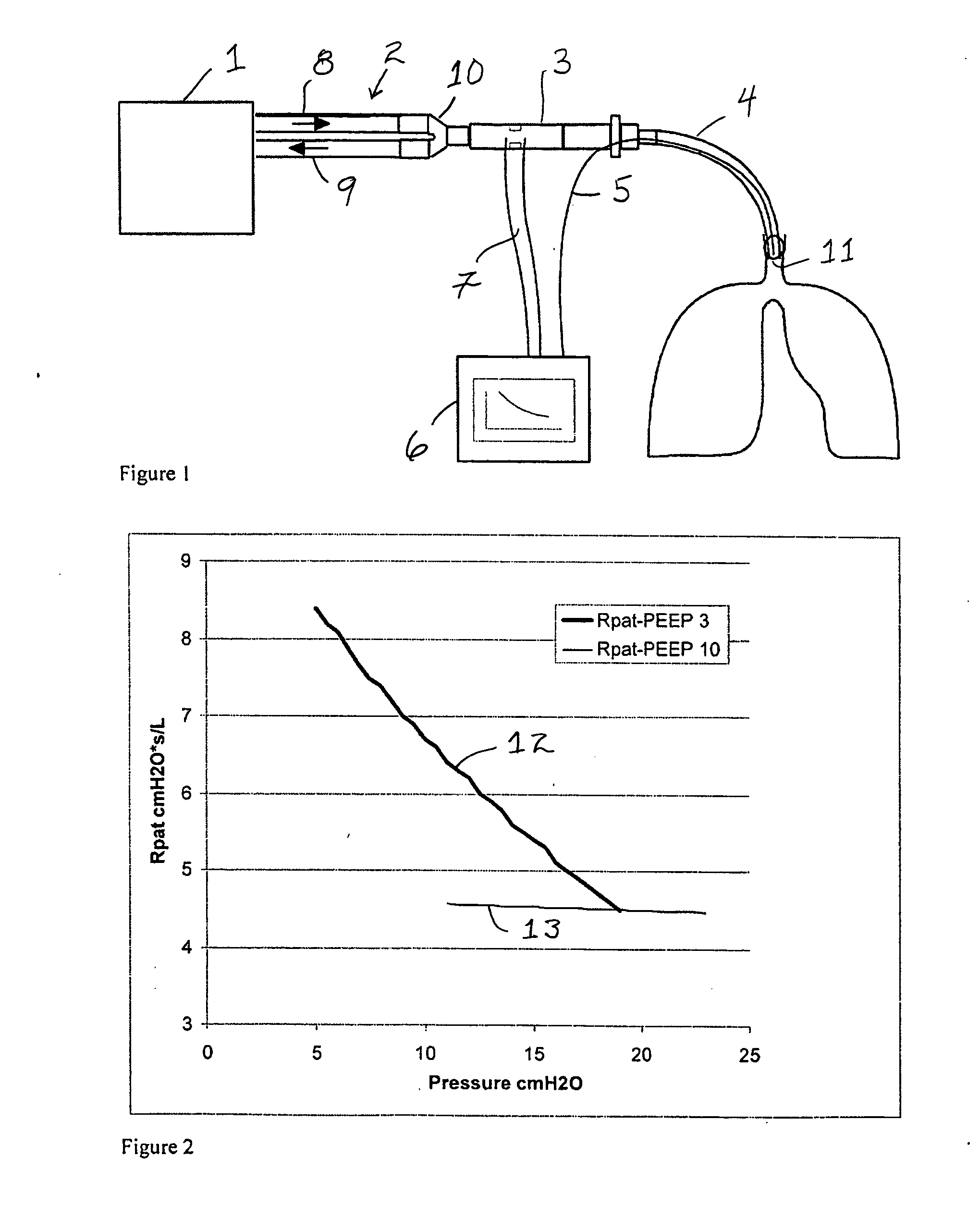
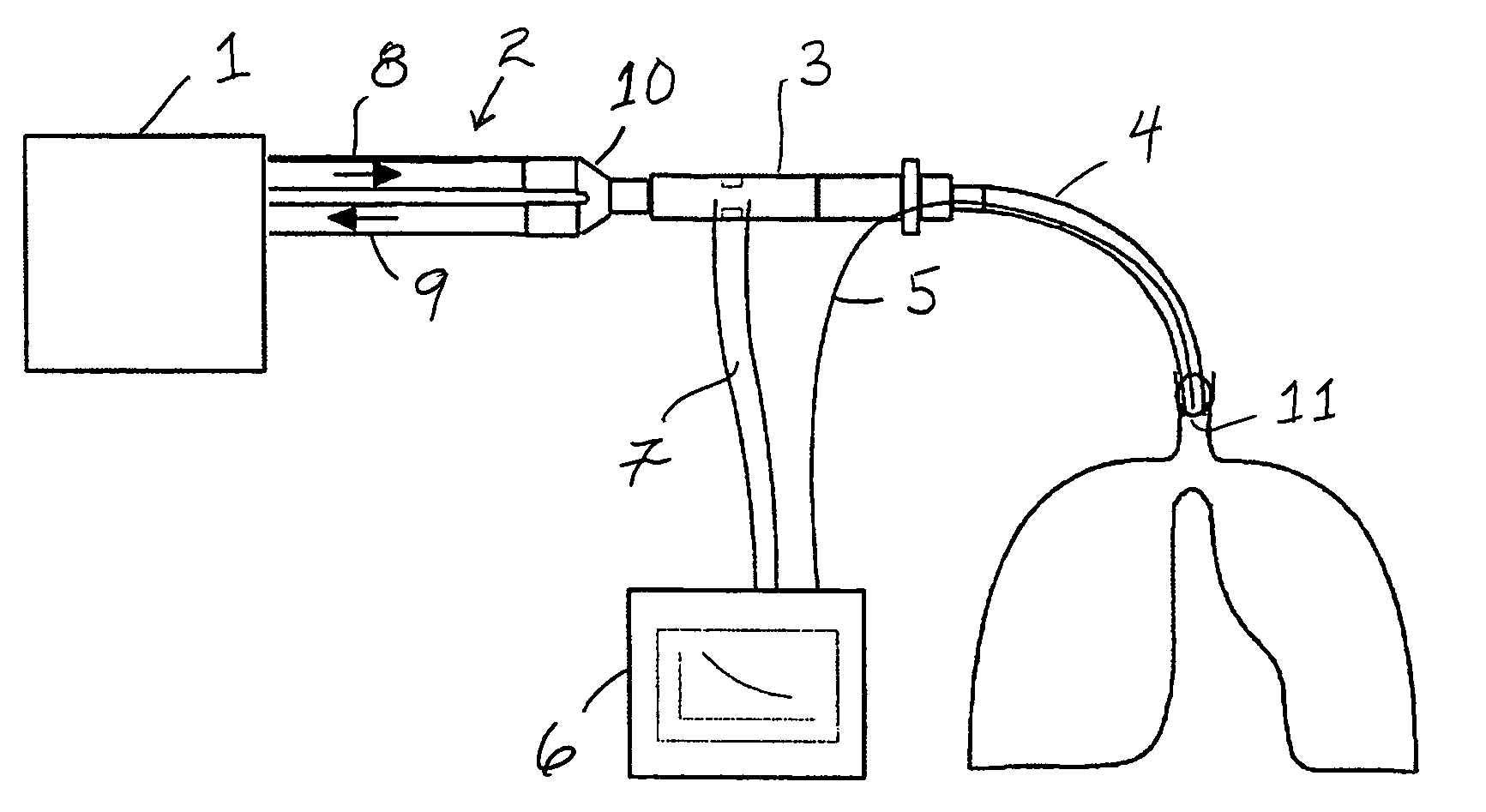
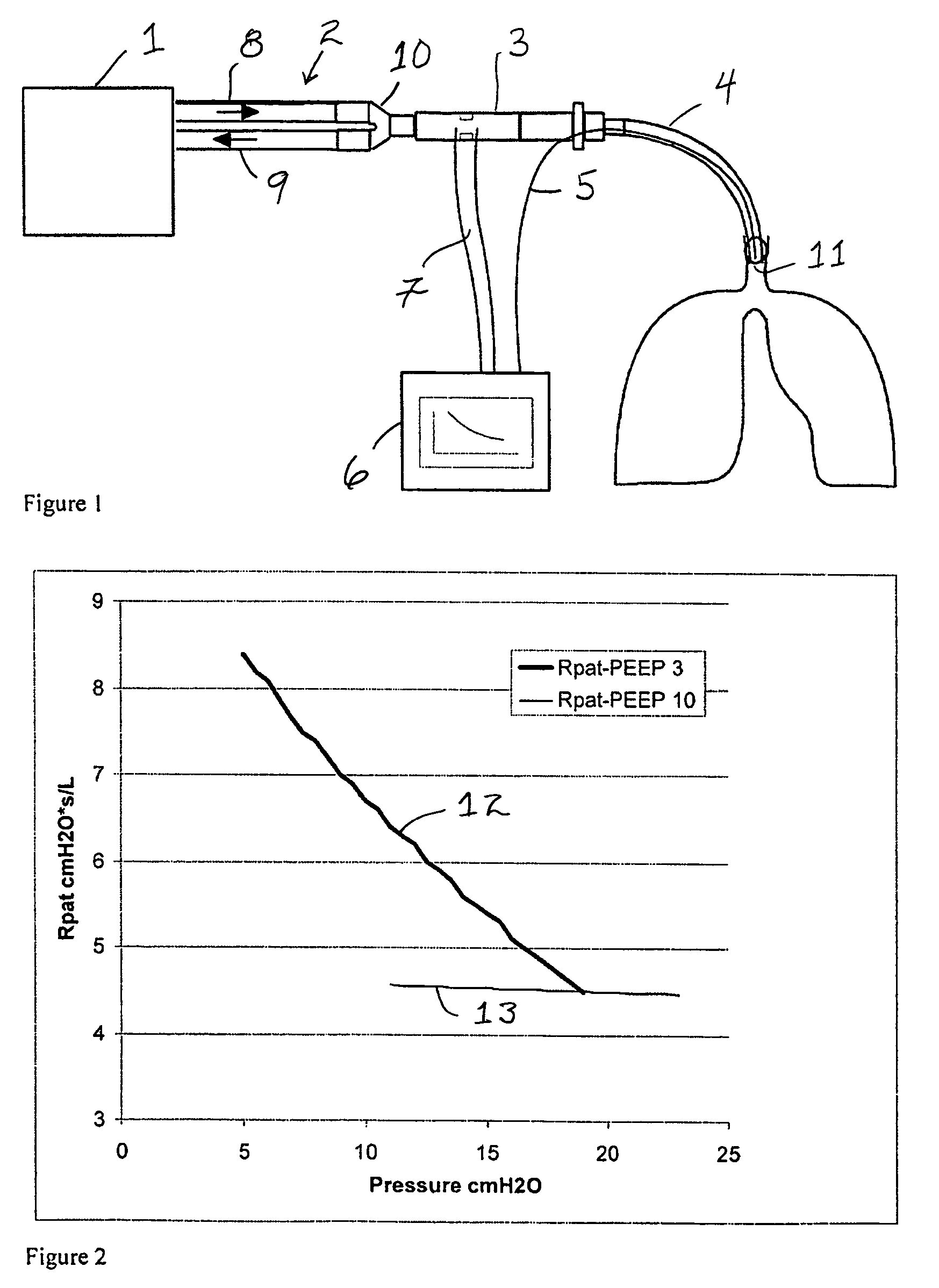
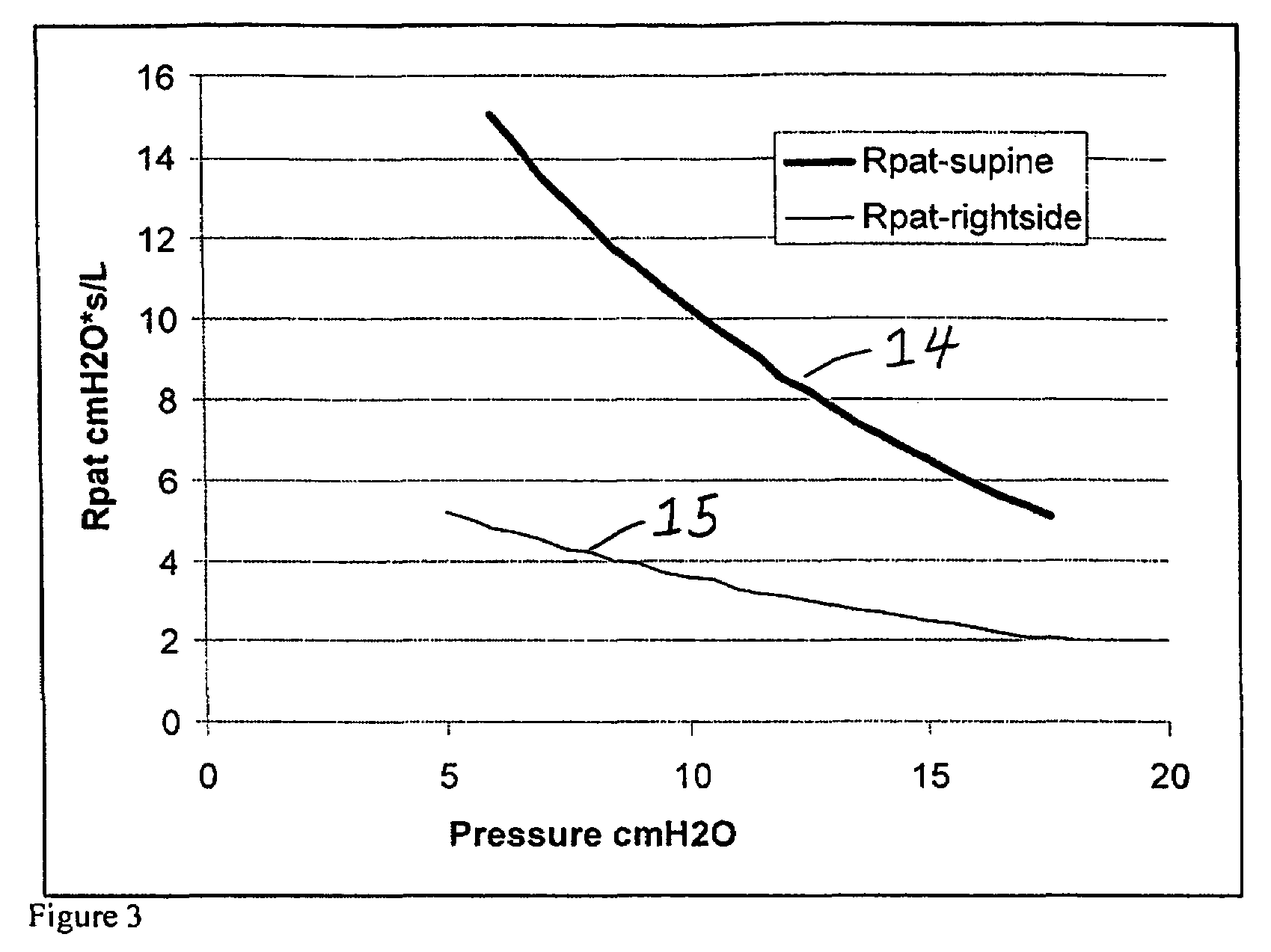
Method for monitoring lung collapse
InactiveUS20070062528A1Maximizes volume rangeWide rangeTracheal tubesOperating means/releasing devices for valvesLung CollapseLung pressure
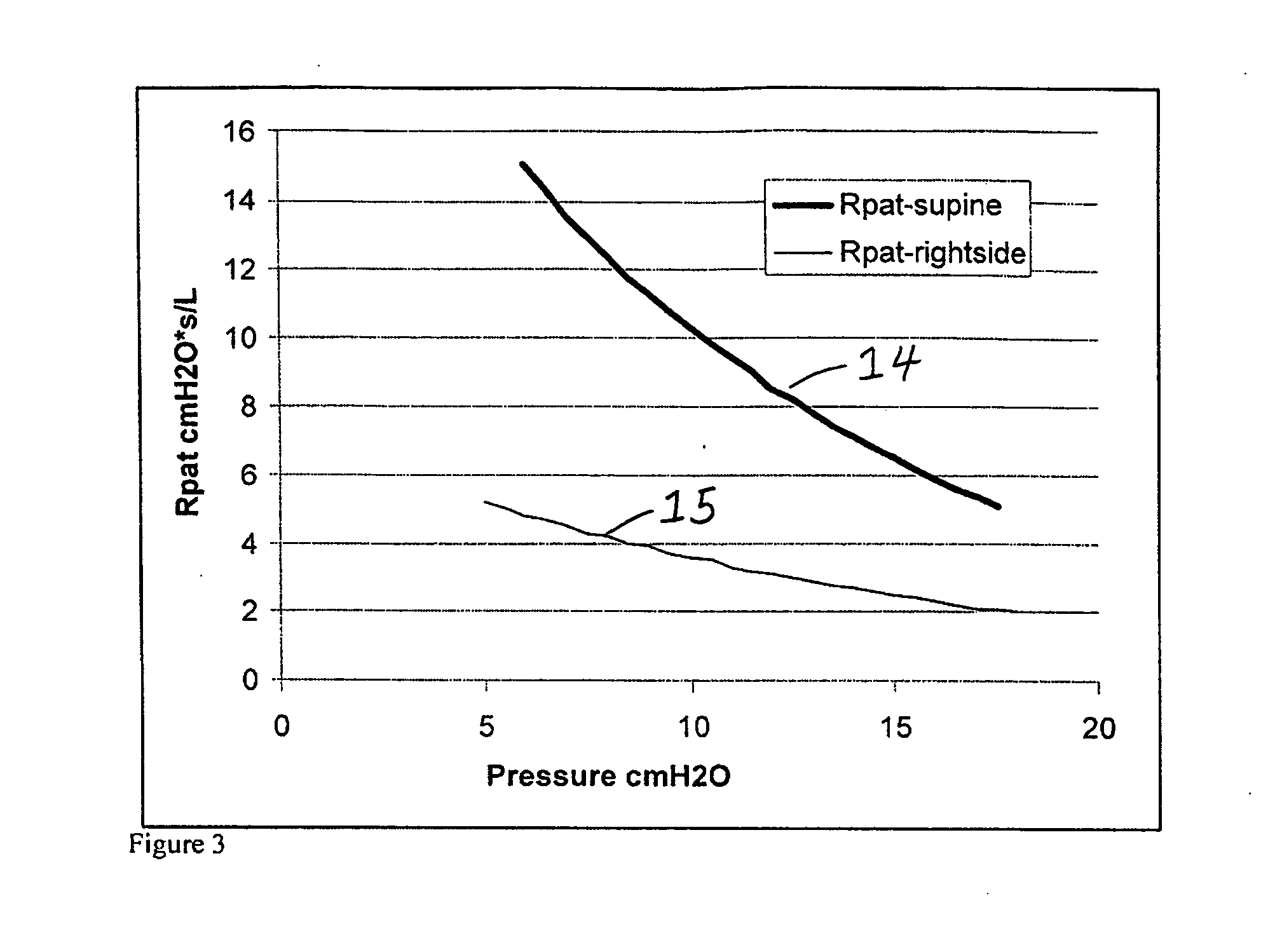
A method for measuring lung collapse and for providing information regarding recruitment and successfulness of actions taken to recruit the lung is provided. Alveolar- and proximal pressures are determined at different lung pressures or volumes. Patient airway resistance is calculated combining these measurements with flow measurement. Plotting the resistance against the lung pressure or volume gives a within-breath distribution of the resistance. Increase of this resistance at end-expiration volume or pressure indicates lung collapse.
Owner:GENERAL ELECTRIC CO
Apparatus and Method for Identifying FRC and PEEP Characteristics
ActiveUS20120055476A1RespiratorsOperating means/releasing devices for valvesForced expiratory vital capacityPressure data
A patient ventilator for assisting a clinician in determining a suitable PEEP for the patient. The amount of the lung volume recruited / de-recruited at various levels of PEEP may be determined for use in selecting a desired PEEP. To this end, the functional residual capacity of the lungs is determined for a first PEEP level. The PEEP is then altered to a second level and a spirometry dynostatic curve of lung volume and pressure data is obtained. The lung volume on the dynostatic curve at a lung pressure corresponding to the first PEEP value is obtained. The difference between the functional residual capacity of the lungs at the first PEEP level and that determined from the dynostatic curve represents the lung volume recruited / de-recruited when changing between said first and second PEEPs.
Owner:GENERAL ELECTRIC CO
Methods and devices for providing inspiratory and expiratory flow relief during ventilation therapy
ActiveUS8567399B2Breathe freelyRespiratorsOperating means/releasing devices for valvesCatheterRespiratory support
Respiratory support and / or controlled mechanical ventilation of a patient are provided. A ventilation apparatus may include a ventilator, a transtracheal prosthesis, and a respiratory relief device. The transtracheal prostheses and ventilation catheter may be arranged such that the patient can breathe freely through the upper airway and / or the tracheal prostheses. Respiratory sensors may measure a breathing rate, lung pressure, airway pressure, or a combination thereof. Pulses of gas may be provided to the patient through the ventilation catheter during inspiration. The pulses may have a first volume while the patient breathes normal and a second volume when the sensors detect a cessation of breathing or reduction in breathing volume. The second volume may be provided at 1-5 times the normal breathing rate, with a volume 25-500% times the first volume, or both.
Owner:BREATHE TECHNOLOGIES INC
Methods and devices for providing inspiratory and expiratory flow relief during ventilation therapy
Respiratory support and / or controlled mechanical ventilation of a patient are provided. A ventilation apparatus may include a ventilator, a transtracheal prosthesis, and a respiratory relief device. The transtracheal prostheses and ventilation catheter may be arranged such that the patient can breathe freely through the upper airway and / or the tracheal prostheses. Respiratory sensors may measure a breathing rate, lung pressure, airway pressure, or a combination thereof. Pulses of gas may be provided to the patient through the ventilation catheter during inspiration. The pulses may have a first volume while the patient breathes normal and a second volume when the sensors detect a cessation of breathing or reduction in breathing volume. The second volume may be provided at 1 - 5 times the normal breathing rate, with a volume 25 - 500% times the first volume, or both.
Owner:BREATHE TECHNOLOGIES INC
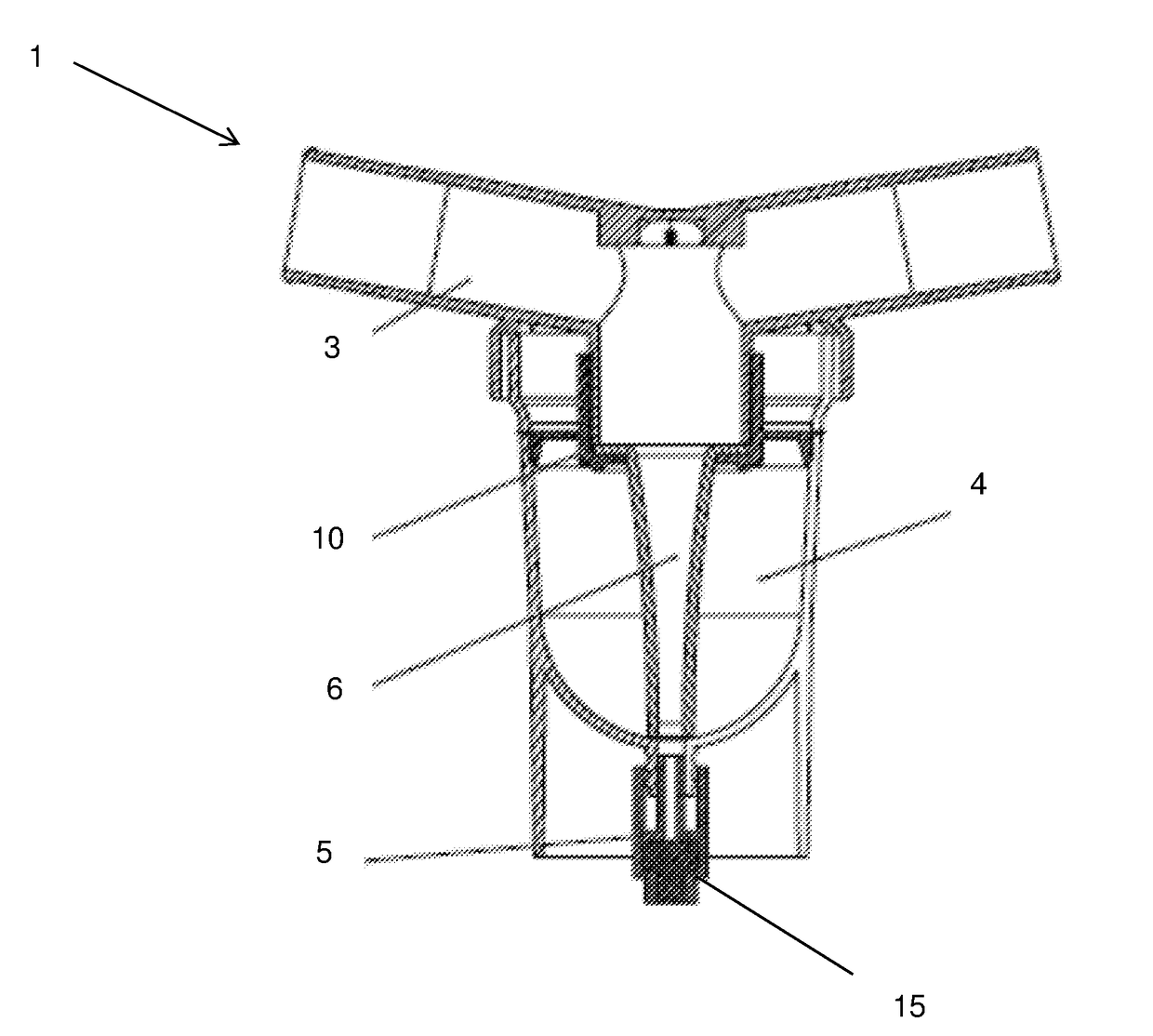
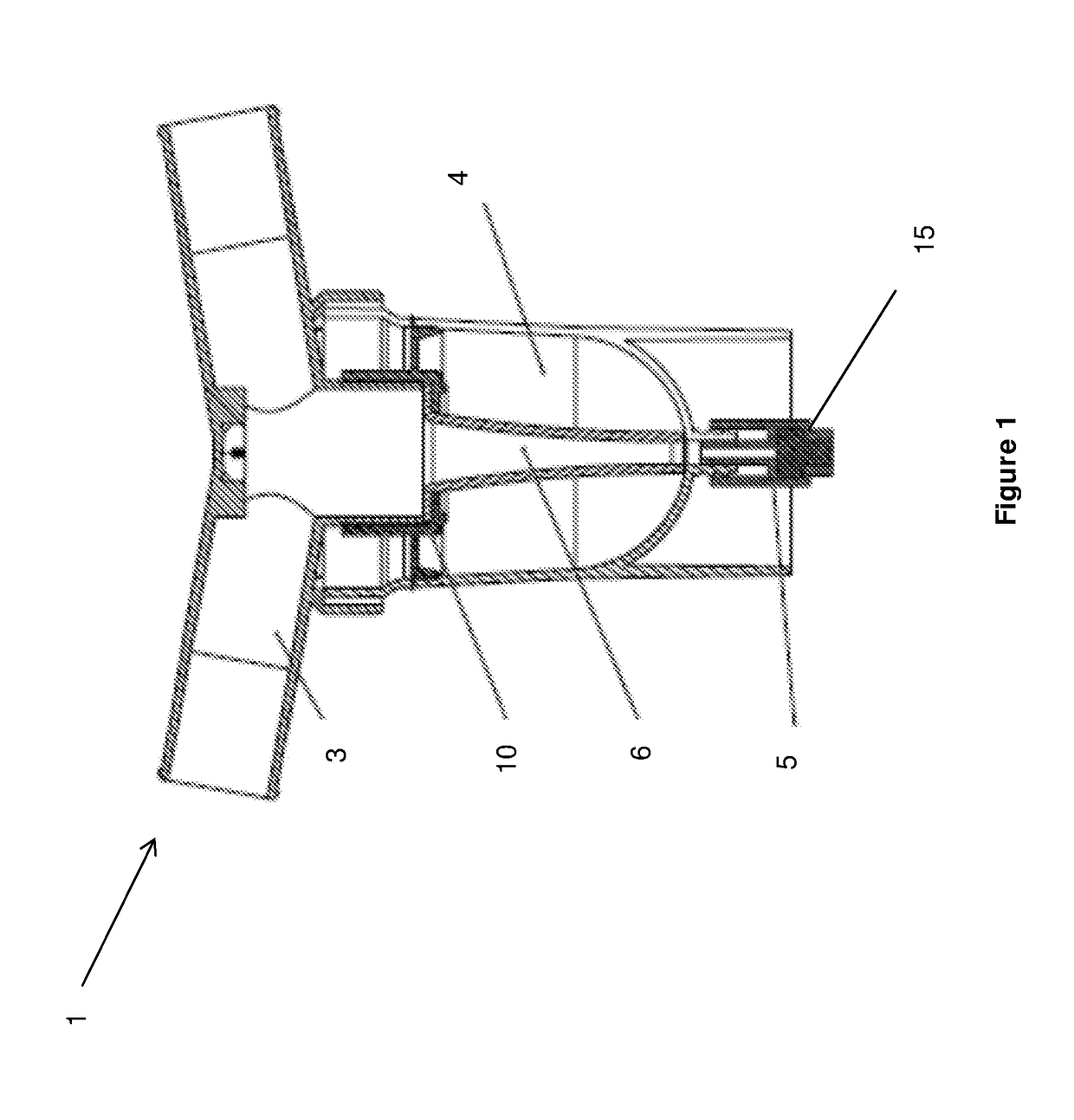
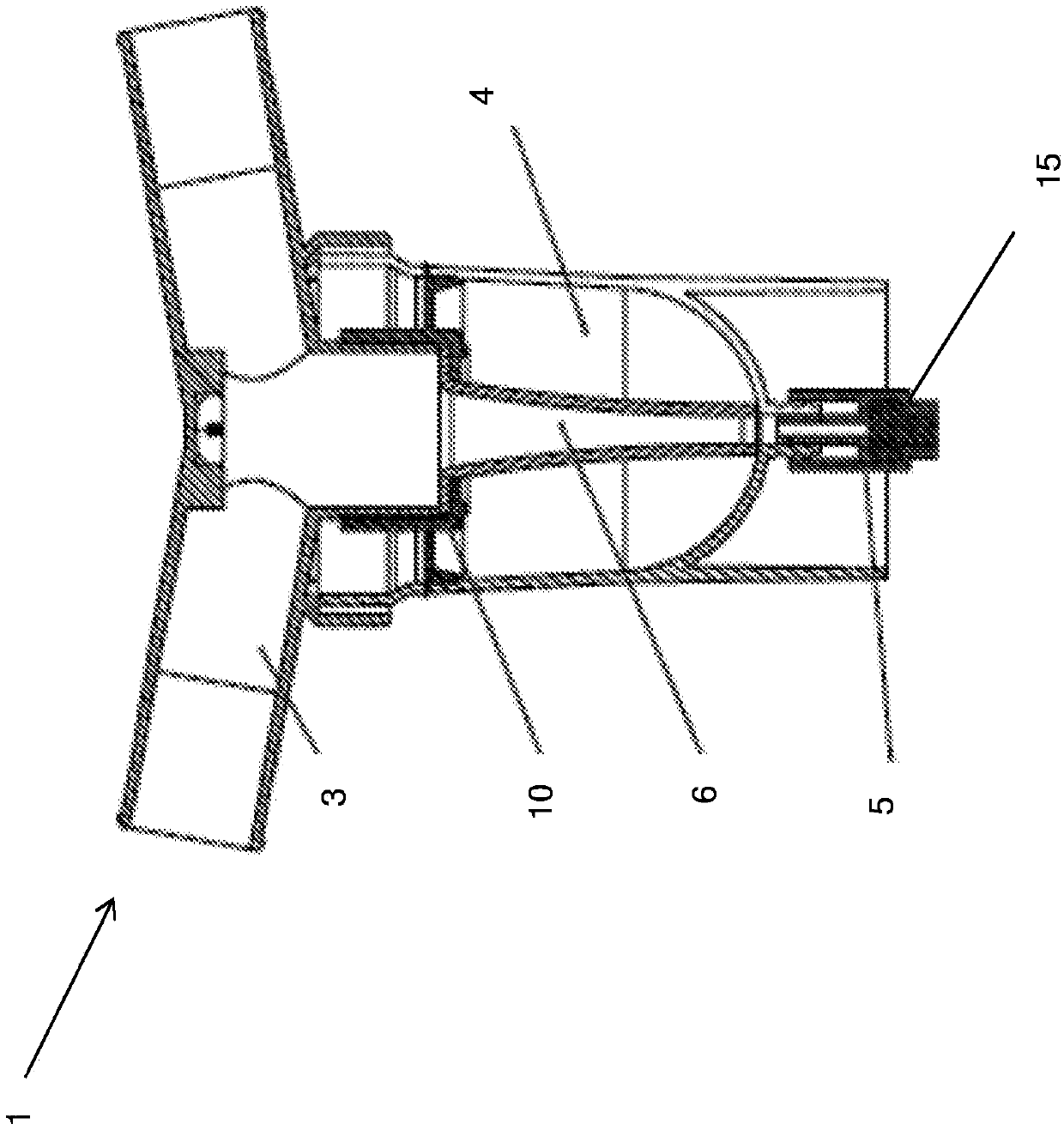
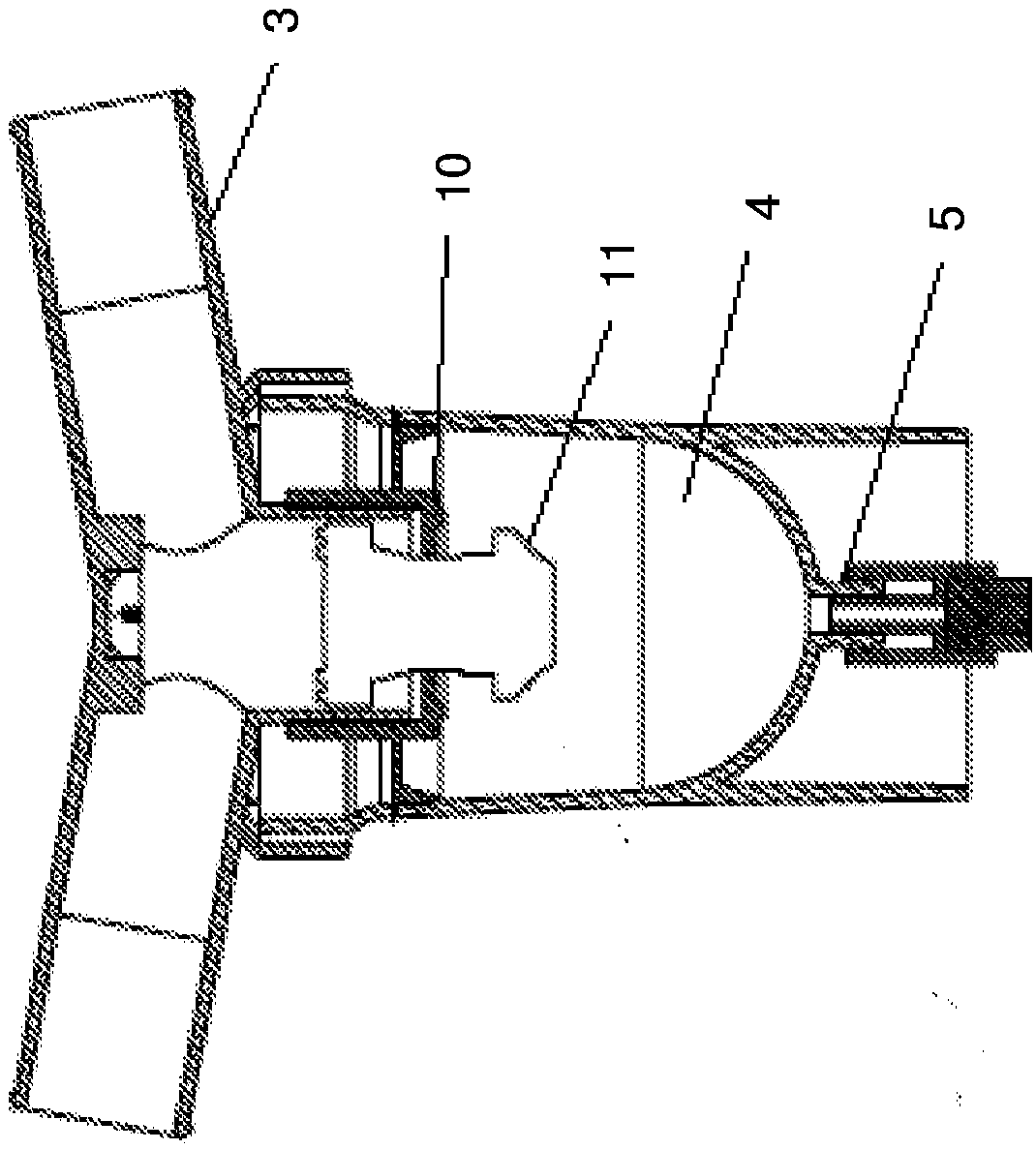
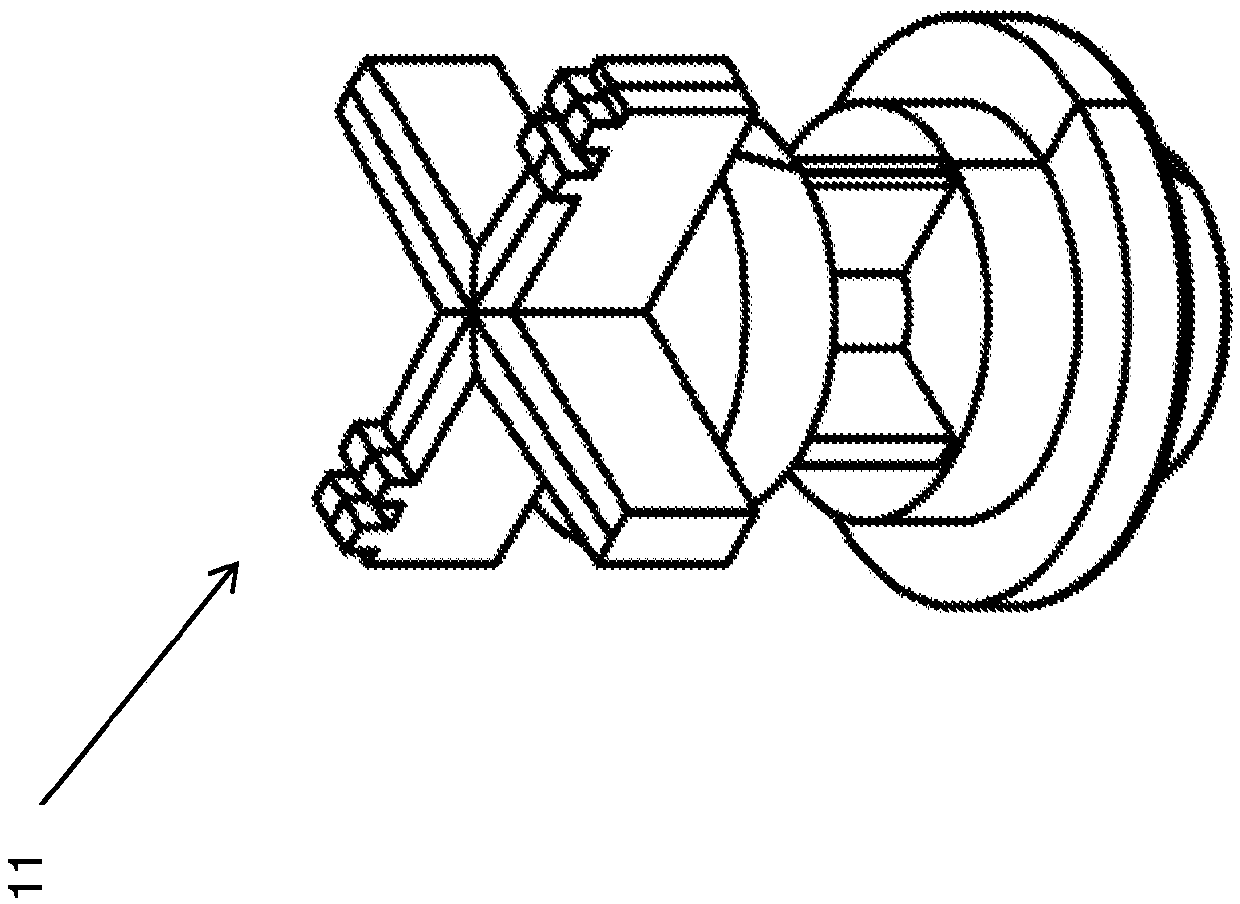
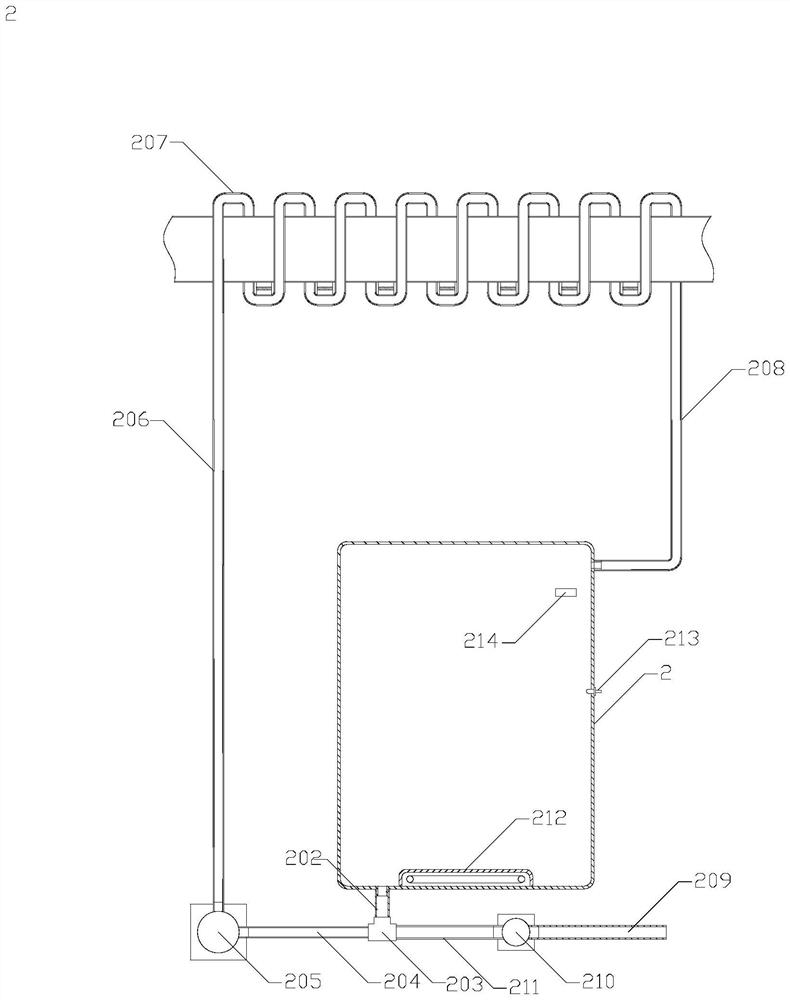
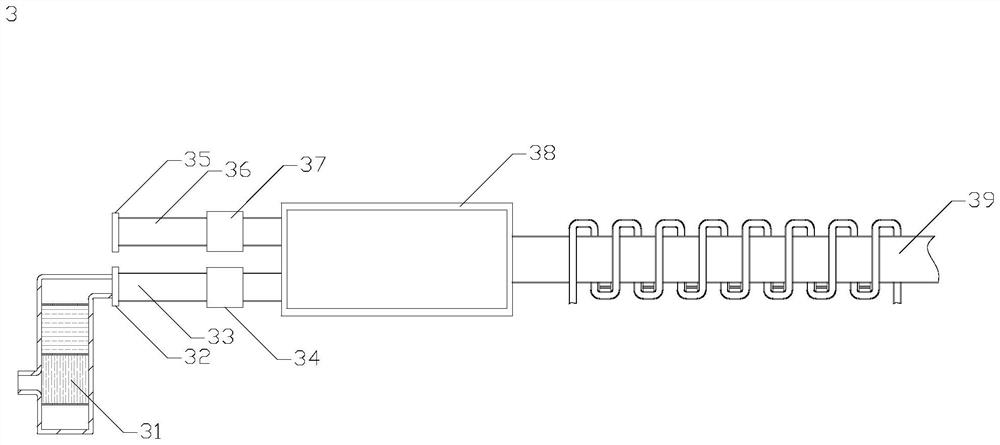
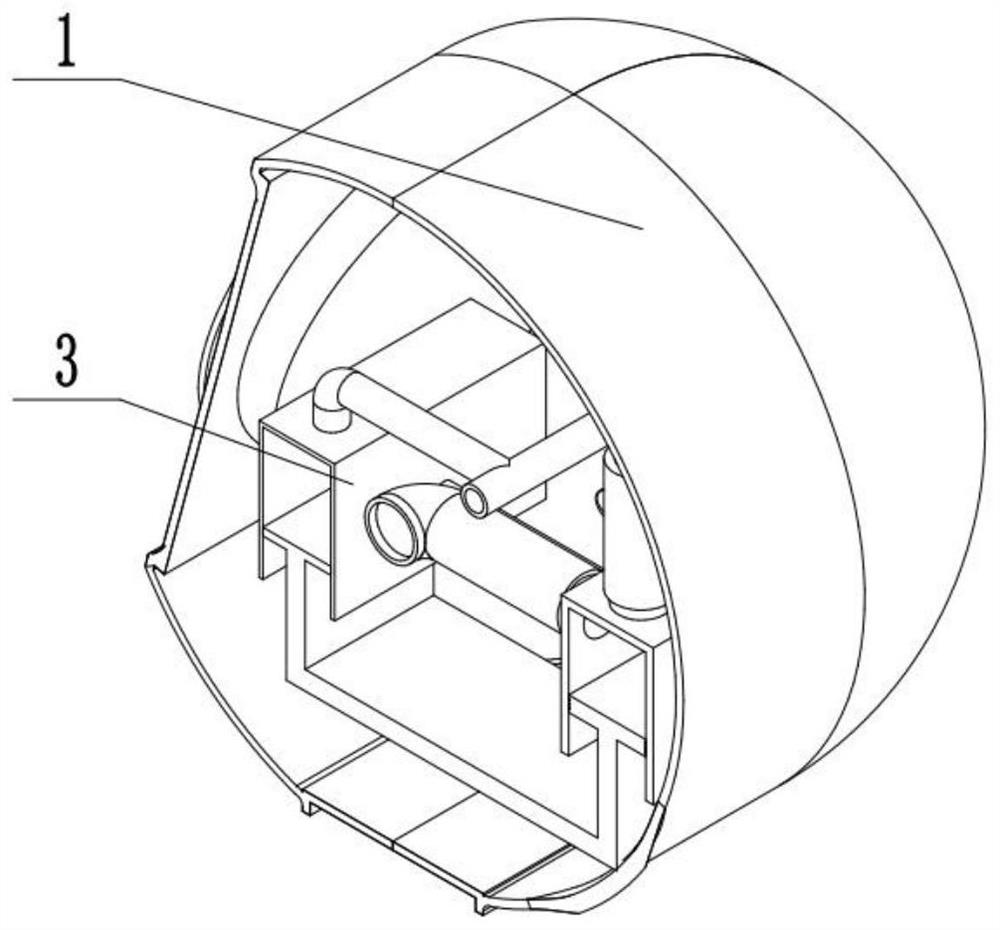
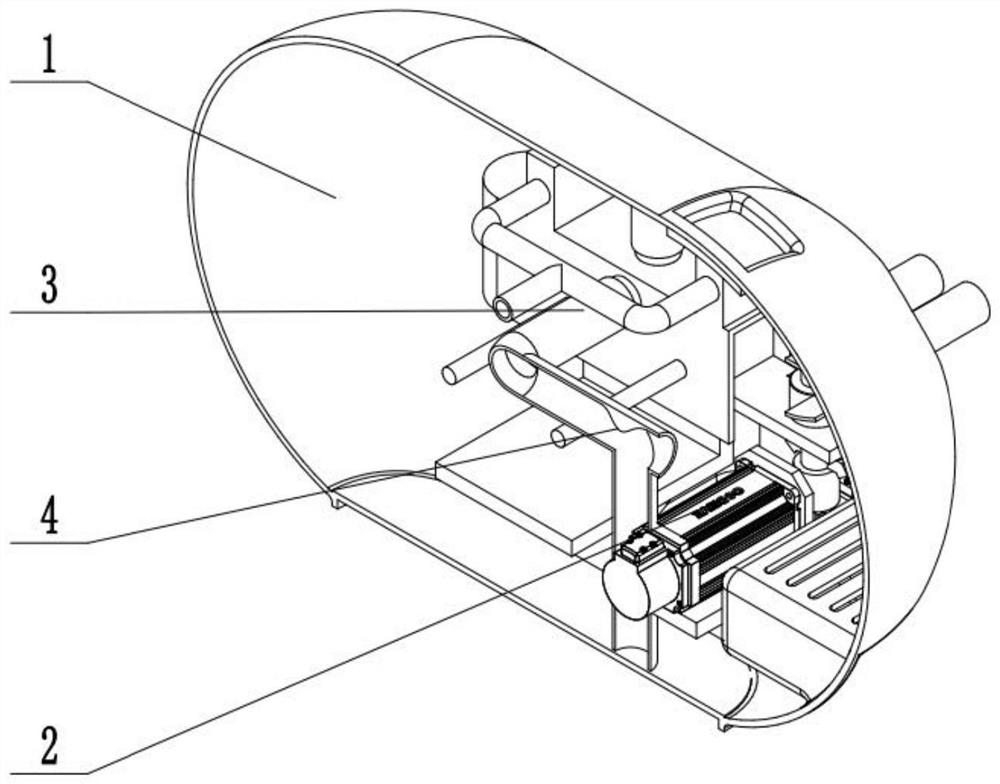
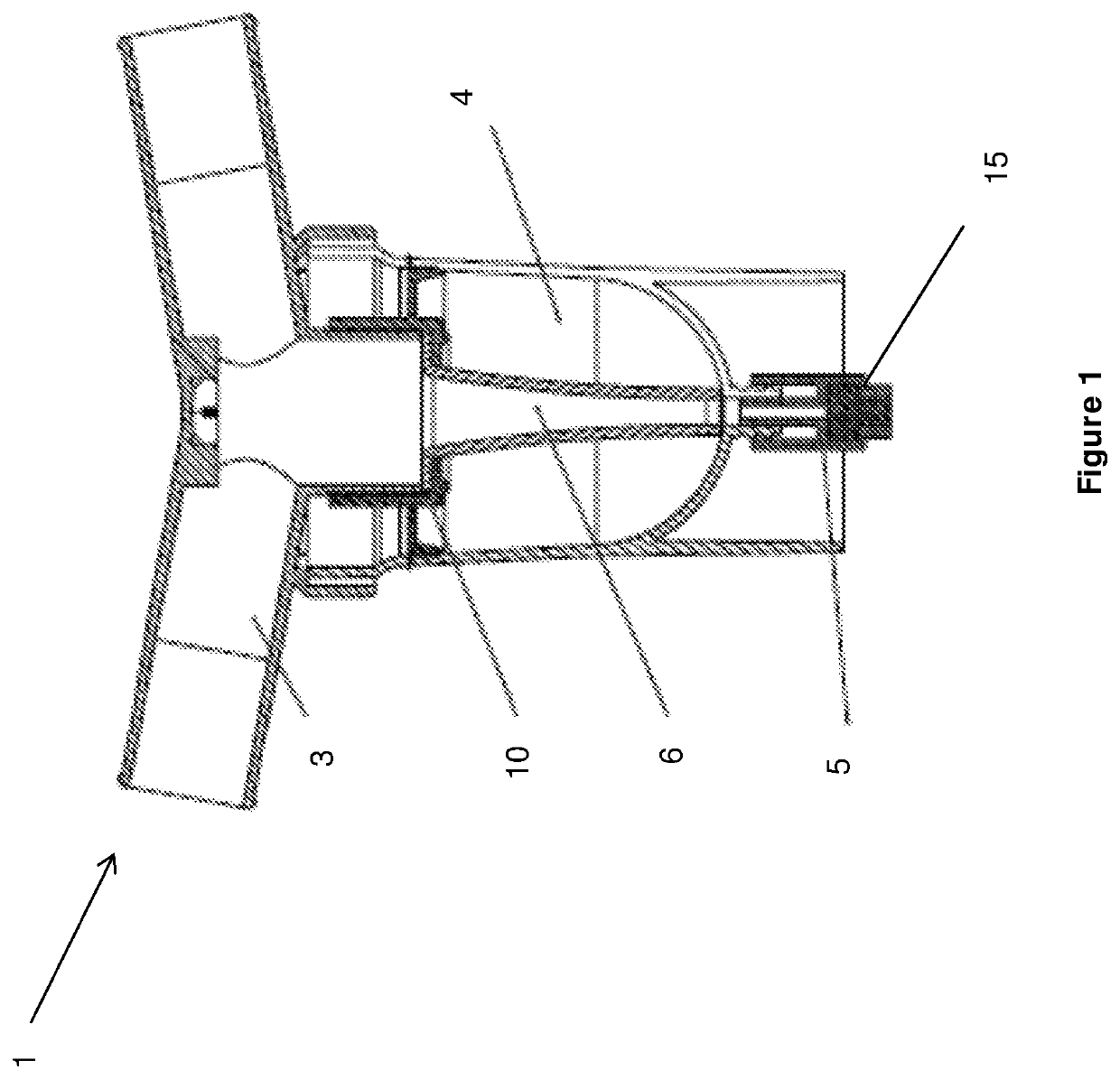
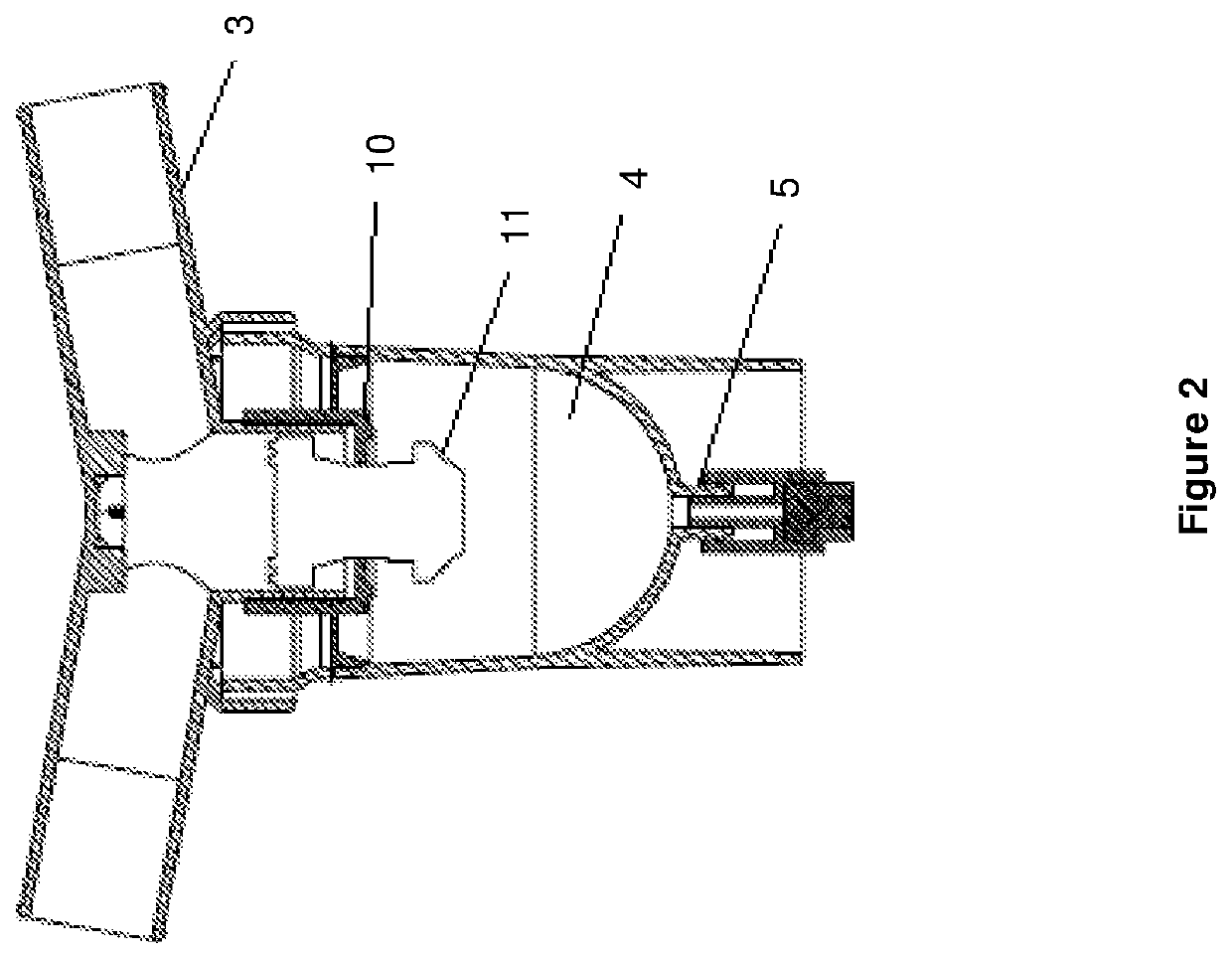
Coaxial and double lumen breathing circuit systems having a lung pressure measurement port and closed system water trap which can be drained with an enjector
ActiveUS20180221615A1Eliminate resistanceOvercome riskRespiratorsMedical devicesWater trapEngineering
The invention relates to providing novel functions to the double lumen breathing circuits and coaxial breathing circuits which at present do not comprise water traps, by adding a closed system water trap designed to have an inkwell shape and a lung pressure measurement port to said circuits wherein the fluid collected in the bottle section can be discharged without having to open the bottle by means of a drainage luer port located at the base of the bottle and a needleless apparatus that has been inserted into the port, and an injector.
Owner:SEVINCLI ATILLA +2
Methods, Systems and Devices for Non-Invasive Open Ventilation For Providing Ventilation Support
ActiveUS20130255683A2Work lessIncrease pressureRespiratorsOperating means/releasing devices for valvesLung volumesNon invasive
A system for providing ventilation support to a patient may include a ventilator, a control unit, a gas delivery circuit with a proximal end in fluid communication with the ventilator and a distal end in fluid communication with a nasal interface, and a nasal interface. The nasal interface may include at least one jet nozzle at the distal end of the gas delivery circuit; and at least one spontaneous respiration sensor for detecting respiration in communication with the control unit. The system may be open to ambient. The control unit may receive signals from the at least one spontaneous respiration sensor and determine gas delivery requirements. The ventilator may deliver gas at a velocity to entrain ambient air and increase lung volume or lung pressure above spontaneously breathing levels to assist in work of breathing, and deliver ventilation gas in a cyclical delivery pattern synchronized with a spontaneous breathing pattern.
Owner:BREATHE TECHNOLOGIES INC
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
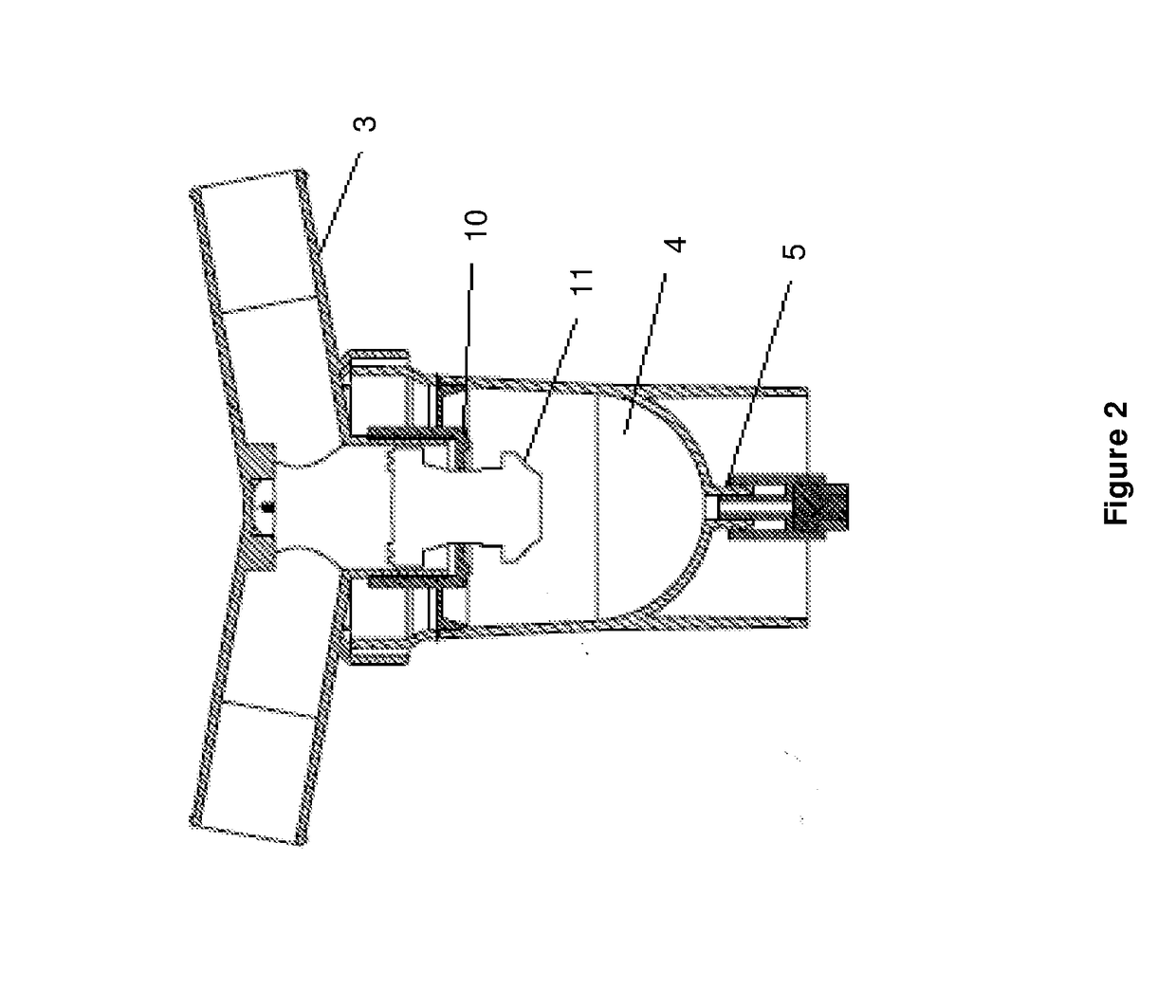
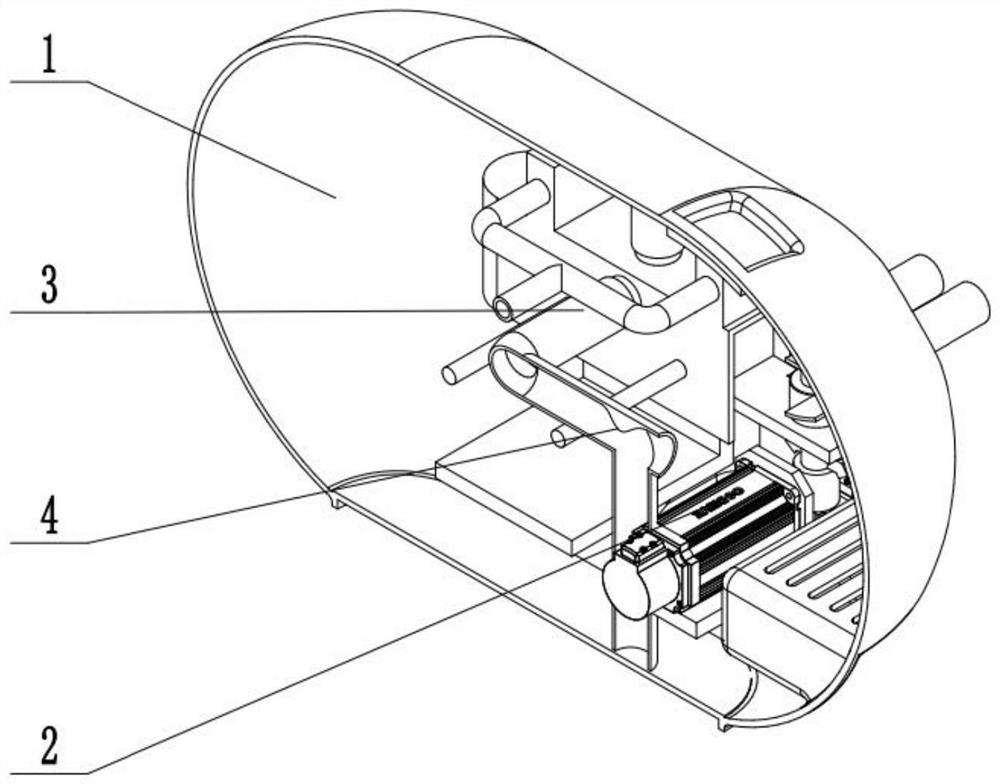
Coaxial and double lumen breathing circuit systems having a lung pressure measurement port and closed system water trap which can be drained with an enjector
Double lumen breathing circuits and coaxial breathing circuits which at present do not comprise water traps, by adding a closed system water trap (1, 2) designed to have an inkwell shape (6) and a lung pressure measurement port (9) to said circuits wherein the fluid collected in the bottle section (4) can be discharged without having to open the bottle by means of a drainage luer port (5) locatedat the base of the bottle and a needleless apparatus (15) that has been inserted into the port, and an injector.
Owner:MEDITRA MEDICAL SUPPLIES IND & BUSINESS MANAGEMENT INC +1
System and method for monitoring resuscitation or respiratory mechanics of a patient
A system and method for monitoring resuscitation and respiratory mechanics of a patient is provided. A pressure sensor detects air pressure within an air-flow path of a resuscitator and generates a first detection signal in response thereto. A flow-rate sensor detects the flow-rate within the air-flow path and generates a second detection signal In response thereto. A processor receives and processes the first and second detection signals using an algorithm to identify a ventilation rate, a lung pressure, and an air volume corresponding to the respiratory air. A report is generated of real-time feedback about respiration of the patient that includes the ventilation rate, lung pressure, and air volume.
Owner:THE GENERAL HOSPITAL CORP
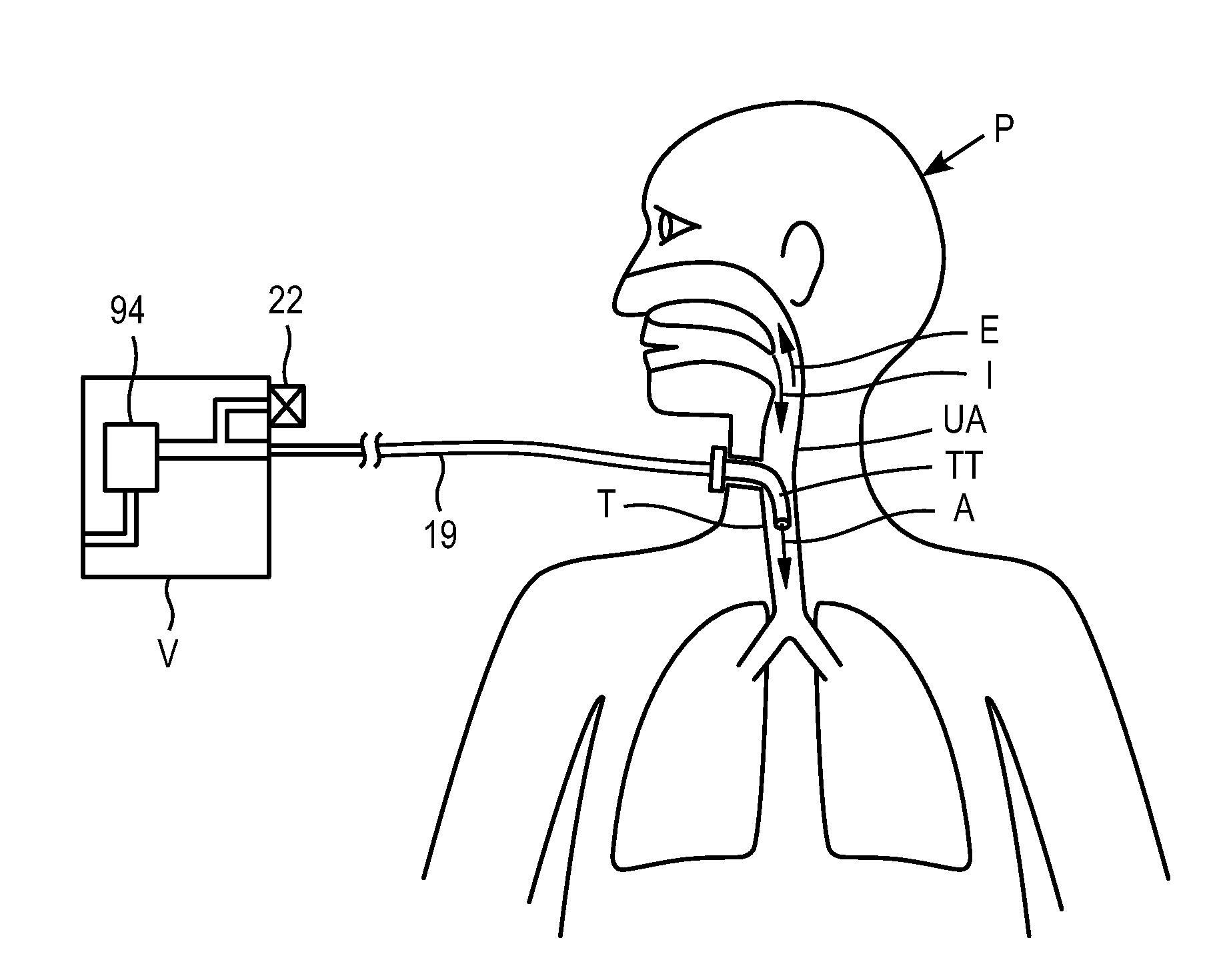
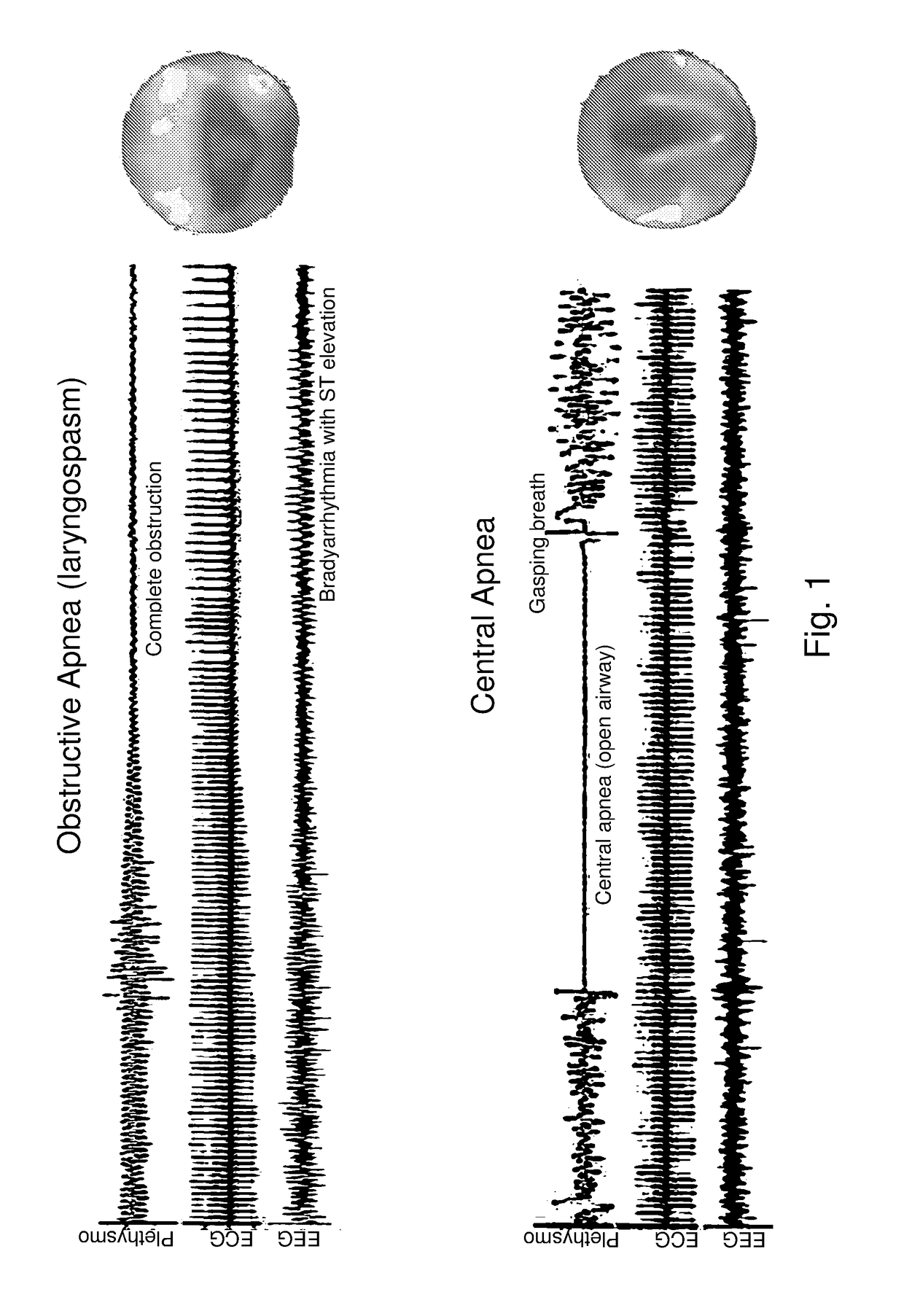
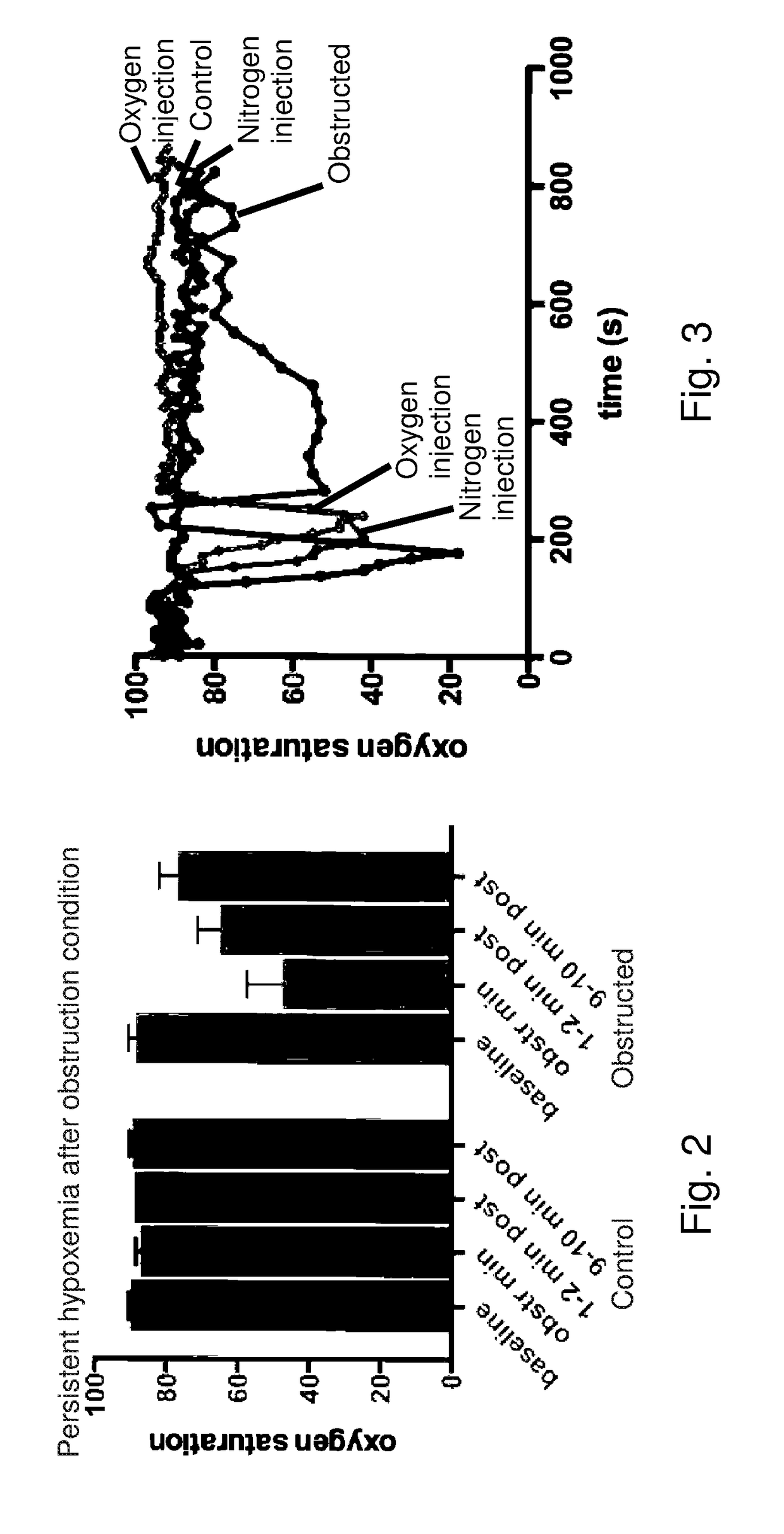
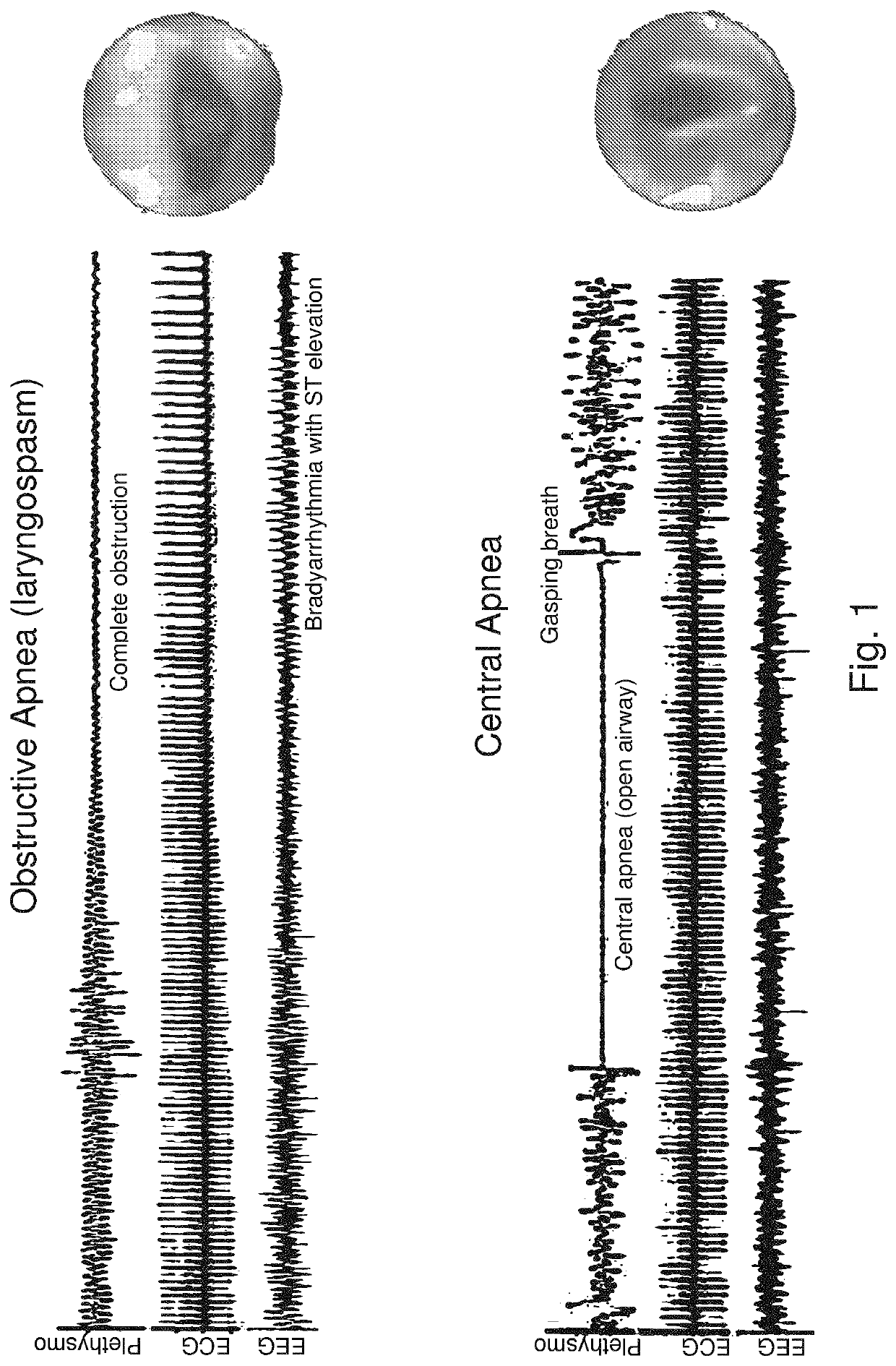
Acute pulmonary pressurization device and method of use
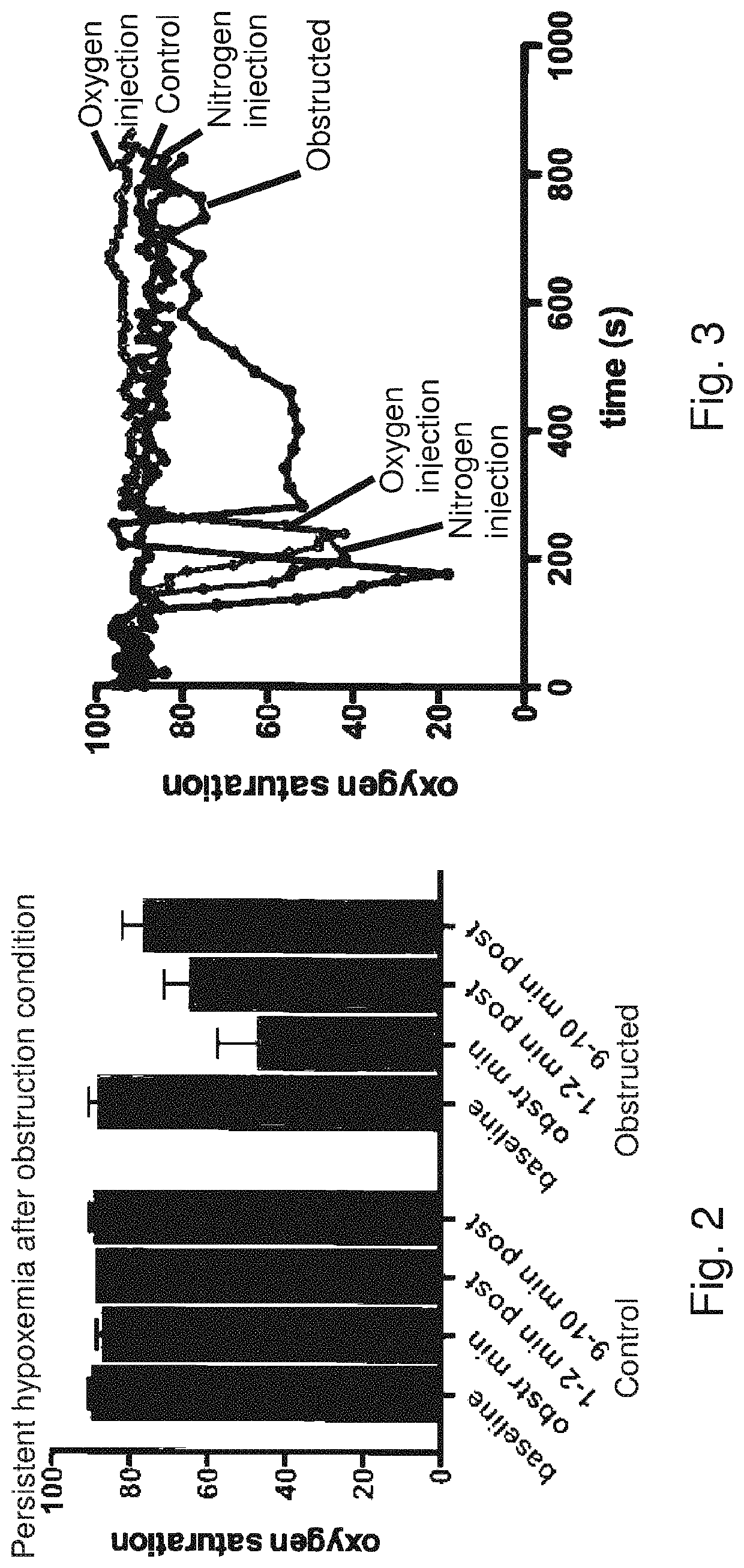
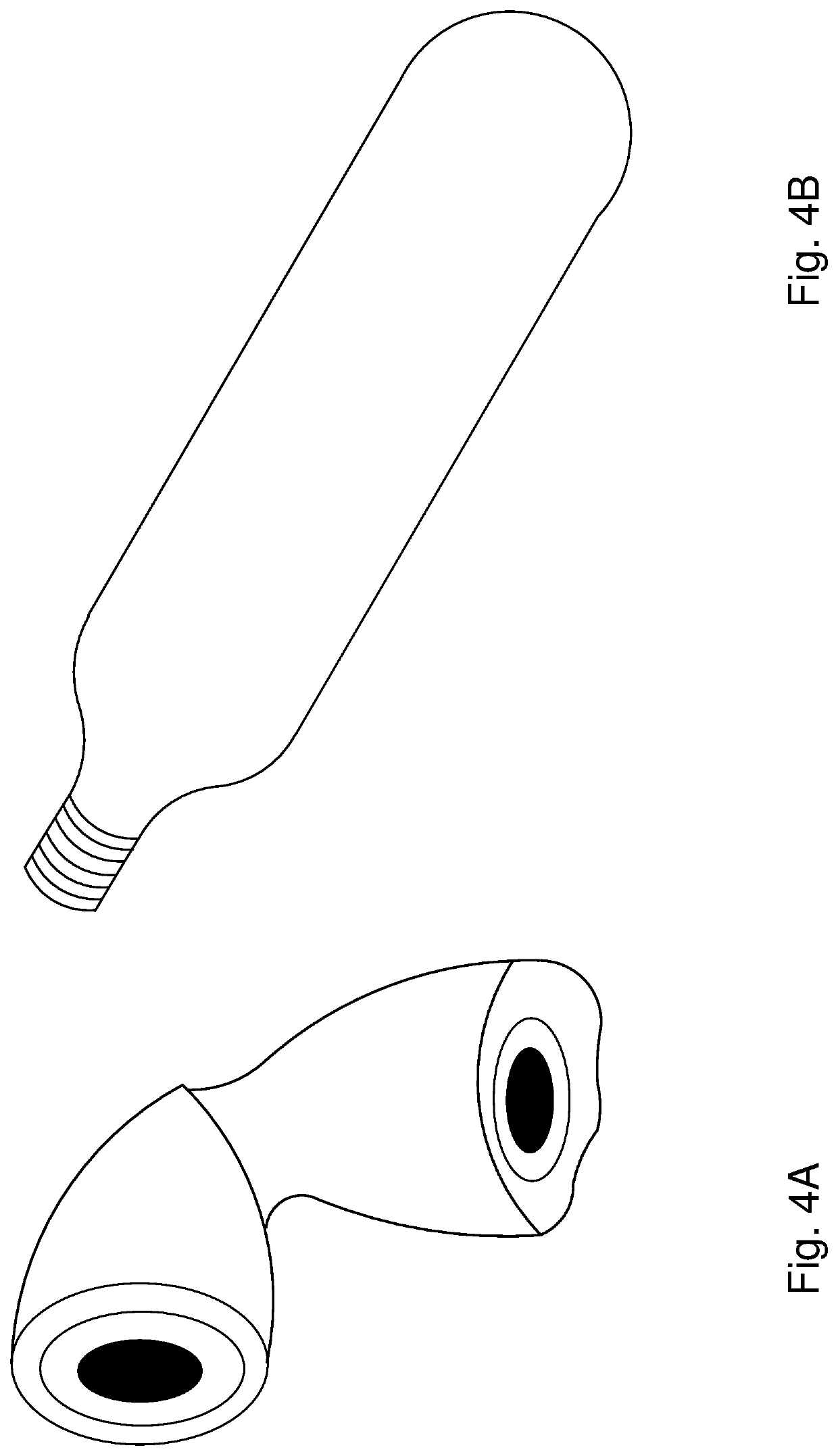
ActiveUS20180326171A1Supporting oxygen saturation levelAlleviating negative pulmonary pressureTracheal tubesMedical devicesLaryngospasmToxic gas
A system and method for relief of negative lung pressure during acute laryngospasm or upper airway obstruction, providing a non-toxic gas cartridge capable of supplying between 0.5-5 liters of gas during a procedure, a valve adapted to commence and stop gas release, and a trans-cricothyroid cartilage inflation needle for acutely relieving the negative pressure in the chest. The needle may also be used to insert a guidewire to assist in endotracheal tube insertion.
Owner:THE RES FOUND OF STATE UNIV OF NEW YORK
Patient Ventilator Control Using Constant Flow and Breathing Triggers
ActiveUS20210402119A1Avoid difficultyTracheal tubesMedical devicesPhysical medicine and rehabilitationLung alveolus
The embodied invention is a new inspiration / expiration ventilator flow design, with a constant inspiration flow and intermittent-concurrent expiratory flow based on lung pressure setpoints. This mode is possible by using a new dual lumen tube inserted into a patient Trachea. Additionally, the control provides support for patient initiated breathing which is initiated by a lung pressure drop. This control provides continuous and gentle recruitment of lung alveoli.
Owner:LEVERED IMPACT LLC
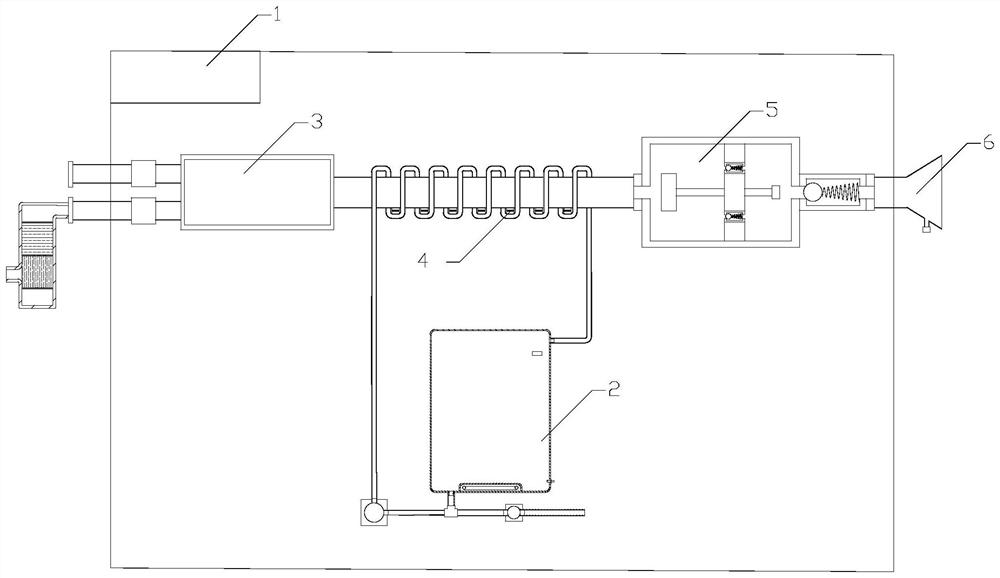
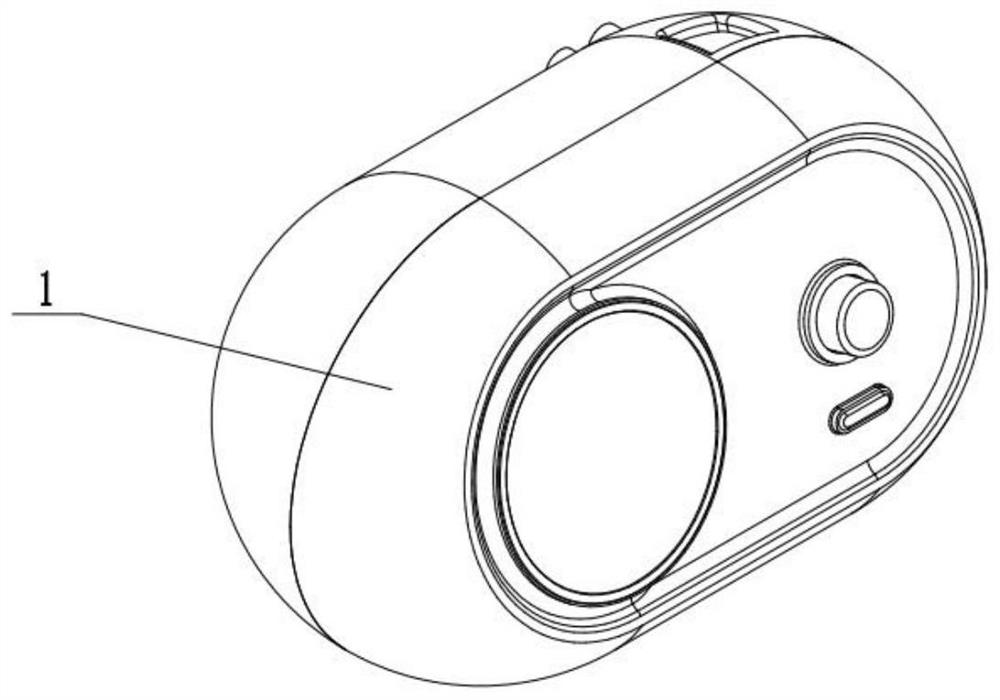
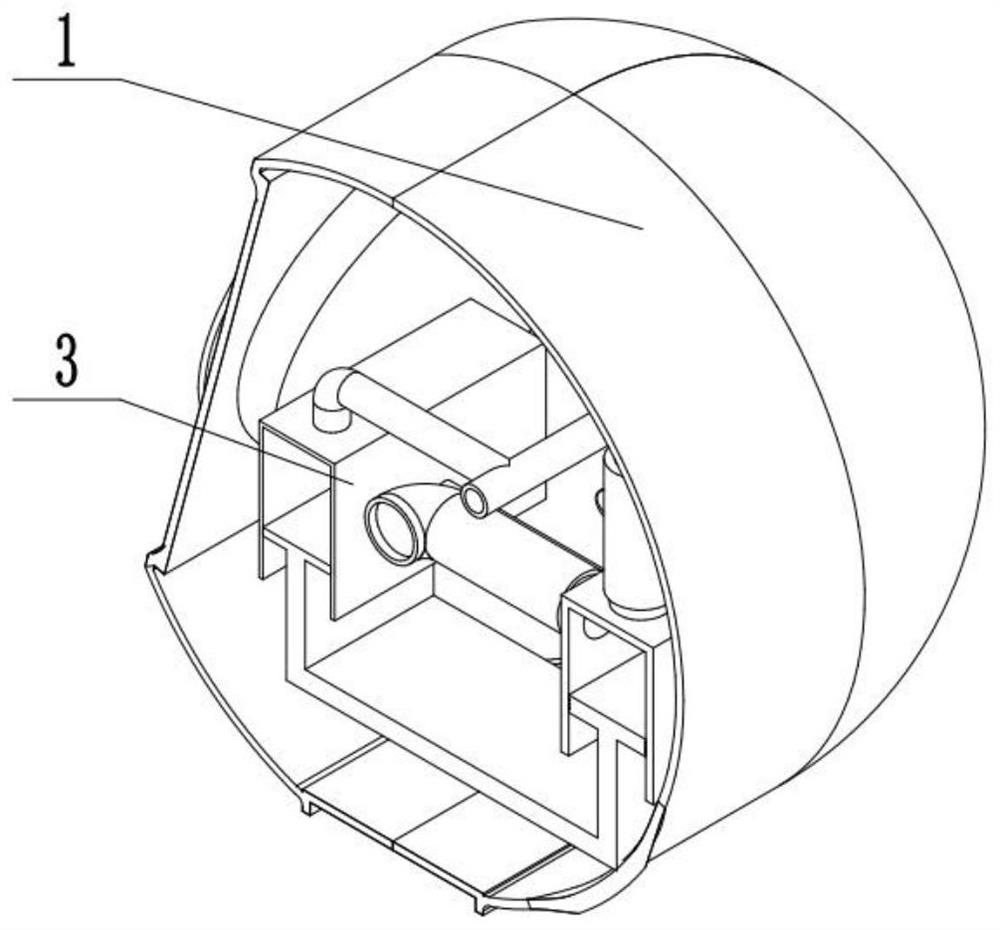
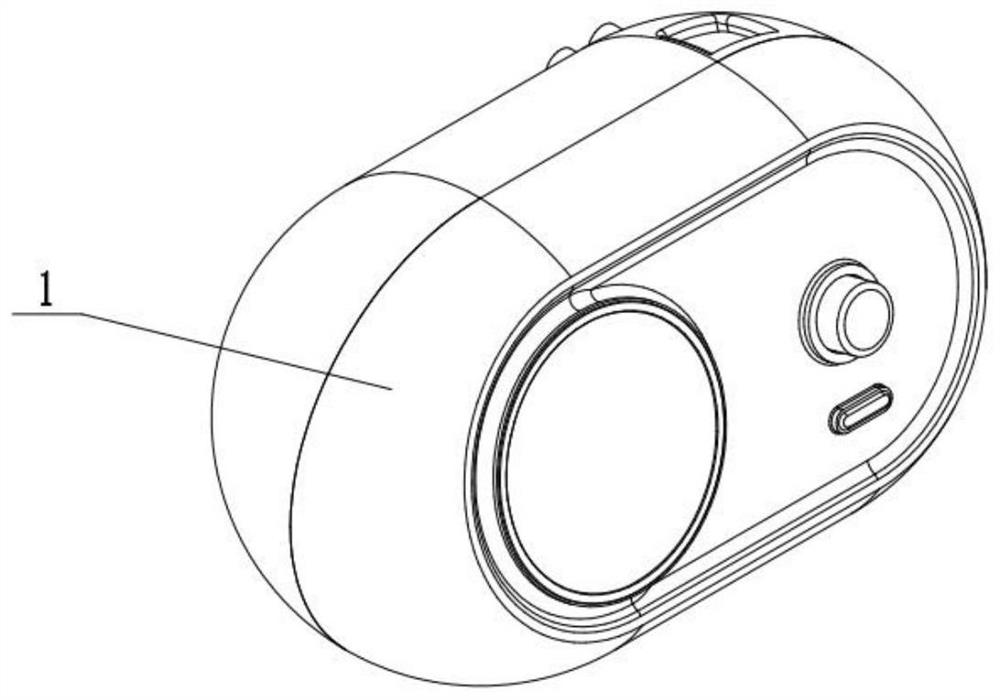
Medical breathing machine with humidifying and warming functions and working method thereof
PendingCN114366965AImprove user experienceImprove uniformityRespiratorsElectrocardiographyPhysical medicine and rehabilitationOxygen tank
The invention relates to a medical breathing machine with humidifying and warming functions. The medical breathing machine comprises a controller, a humidifying and warming mechanism, an air and oxygen mixing mechanism, a frequency coordination device, an oxygen tank, an air compressor and a mask. Gas is heated through hot water in the spiral pipe, so that the heating uniformity of the gas to be introduced is improved, and the use experience of a respirator user is improved; the air-oxygen mixing proportion can be conveniently adjusted by adjusting the opening degrees of the first flow adjusting valve and the second flow adjusting valve, and the convenience of debugging and using the breathing machine is improved; reciprocating sliding of the sliding block can be simply controlled through the motor, the breathing frequency can be controlled by controlling the positive and negative rotation switching frequency of the motor, the pressure of gas to be introduced can be adjusted according to the lung pressure of a user by controlling the sliding block pushing amount, and the use convenience degree of the breathing machine is improved. And by arranging the waterproof breathable film, the use safety and reliability are improved under the condition that the gas humidification effect is guaranteed.
Owner:肖强
A ventilator with return air treatment
ActiveCN113813483BGuaranteed fixed pressureAchieving assisted breathingRespiratorsEngineeringEmergency medicine
The invention relates to a medical related equipment, more specifically a ventilator with return air treatment, which solves the problem that the current mechanically controlled ventilator cannot adjust the oxygen supply amount according to the specific situation of the patient, and some patients have respiratory diseases If the ventilator is used without treatment, it will cause pollution to the oxygen supply part inside the ventilator. The oxygen adjustment device is installed and fixed on the shell, the breathing control device is installed and fixed on the shell, and the treatment pipeline is installed and fixed on the shell. The shell is equipped with other devices, the oxygen volume adjustment device controls and adjusts the oxygen intake according to the needs of the patient, the breathing control device realizes automatic control of breathing action, and the processing pipeline controls and processes the exhaled gas of the patient to realize adjustable oxygen intake and ensure that the patient's lung pressure is fixed to achieve the functions of assisting breathing and processing the return air.
Owner:深圳市大方牙科技有限公司
Breathing machine with return air treatment function
ActiveCN113813483AGuaranteed fixed pressureAchieving assisted breathingRespiratorsEngineeringRespiratory disease
The invention relates to medical related equipment, in particular to a breathing machine with an air return treatment function, and solves the problems that an existing mechanically-controlled breathing machine can not adjust a fed oxygen supply amount according to the specific conditions of patients, in addition, parts of patients have respiratory diseases, when the breathing machine is adopted without treatment, an oxygen supply part in the breathing machine is polluted. An oxygen amount adjusting device, a breathing control device and a treatment pipeline are mounted and fixed on a shell; other devices are mounted through the shell; the oxygen amount adjusting device controls and adjusts an oxygen feeding amount according to the requirements of a patient; the breathing control device automatically controls breathing actions; and the treatment pipeline controls and processes air exhaled by the patient. By use of the breathing machine, the oxygen feeding amount can be adjusted, and the lung pressure of the patient is guaranteed to be fixed, and therefore, the functions of assisting in breathing and processing return air can be achieved.
Owner:深圳市大方牙科技有限公司
Method for monitoring lung collapse
InactiveUS7699789B2Reduce tensionMaximize rangeTracheal tubesRespiratory organ evaluationLung CollapseLung pressure
A method for measuring lung collapse and for providing information regarding recruitment and successfulness of actions taken to recruit the lung is provided. Alveolar- and proximal pressures are determined at different lung pressures or volumes. Patient airway resistance is calculated combining these measurements with flow measurement. Plotting the resistance against the lung pressure or volume gives a within-breath distribution of the resistance. Increase of this resistance at end-expiration volume or pressure indicates lung collapse.
Owner:GENERAL ELECTRIC CO
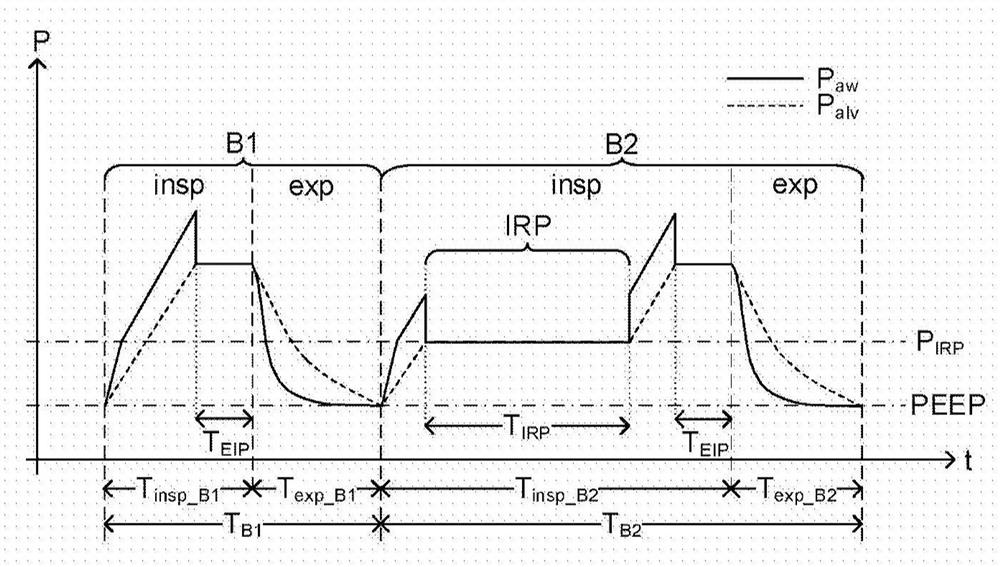
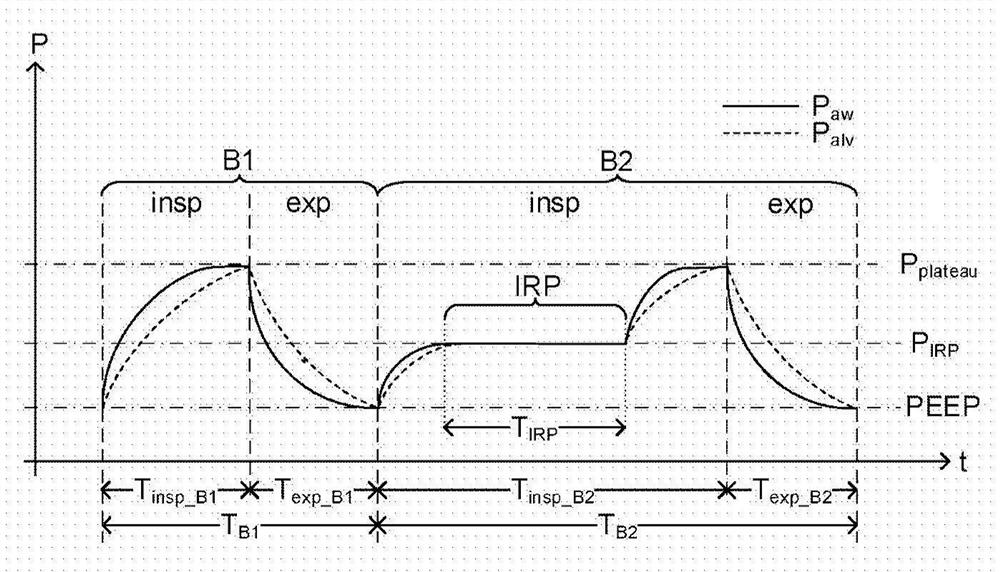
Ventilation pattern for hemodynamic parameter determination during mechanical ventilation
PendingCN112261964AImprove securityReduced risk of collapsed lungs (atelectasis)RespiratorsMedical devicesBlood flowPhysical therapy
A method for changing the effective ventilation of a mechanically ventilated subject (3) to enable or carry out non-invasive determination of hemodynamic parameters is disclosed. The method comprisesa step of ventilating the subject using a ventilation pattern comprising at least one phase of increased ventilation and at least one phase of decreased ventilation, wherein the phase of decreased ventilation comprises at least one prolonged breath (B2; B2', B2'', B2''') including a respiratory pause (IRP). The respiratory pause is initiated when the lung pressure (Palv) of the subject is betweena minimum lung pressure and a maximum lung pressure of the subject during the prolonged breath.
Owner:MAQUET CRITICAL CARE
Coaxial and double lumen breathing circuit systems having a lung pressure measurement port and closed system water trap which can be drained with an enjector
ActiveUS11395896B2Resistance against the air flow is eliminatedOvercome riskRespiratorsMedical devicesWater trapSurgery
The invention relates to providing novel functions to the double lumen breathing circuits and coaxial breathing circuits which at present do not comprise water traps, by adding a closed system water trap designed to have an inkwell shape and a lung pressure measurement port to said circuits wherein the fluid collected in the bottle section can be discharged without having to open the bottle by means of a drainage luer port located at the base of the bottle and a needleless apparatus that has been inserted into the port, and an injector.
Owner:SEVINCLI ATILLA +2
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
Acute pulmonary pressurization device and method of use
ActiveUS11033702B2Negative pressureReduce negative pressureTracheal tubesMedical devicesLaryngospasmToxic gas
A system and method for relief of negative lung pressure during acute laryngospasm or upper airway obstruction, providing a non-toxic gas cartridge capable of supplying between 0.5-5 liters of gas during a procedure, a valve adapted to commence and stop gas release, and a trans-cricothyroid cartilage inflation needle for acutely relieving the negative pressure in the chest. The needle may also be used to insert a guidewire to assist in endotracheal tube insertion.
Owner:THE RES FOUND OF STATE UNIV OF NEW YORK
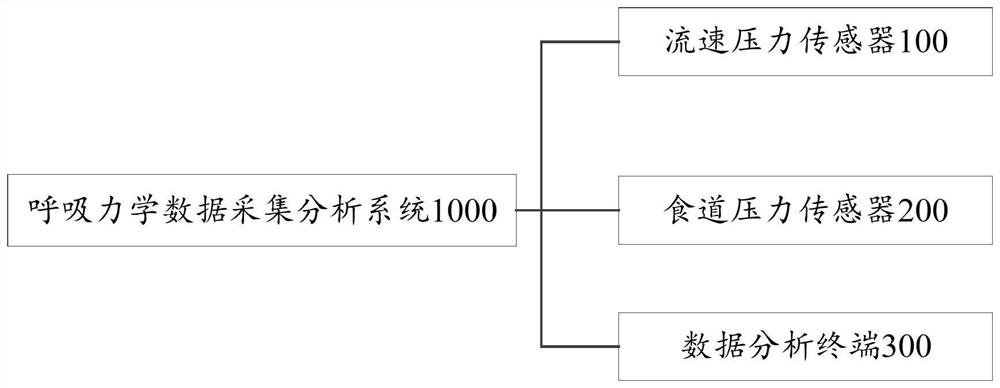
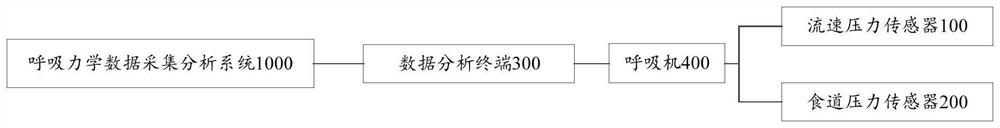
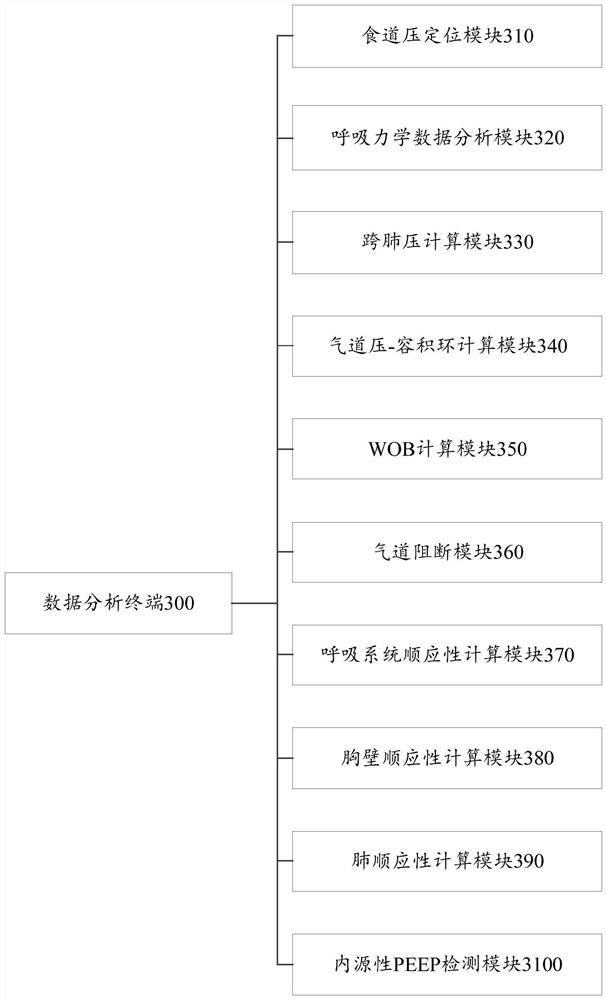
Respiratory mechanics data acquisition and analysis method and system based on esophageal pressure monitoring
The invention relates to a respiratory mechanics data acquisition and analysis method and system, and the system comprises a flow velocity pressure sensor, an esophagus pressure sensor and a data analysis terminal. The data analysis terminal comprises at least one of the following modules: an esophageal pressure positioning module, a respiratory mechanics data analysis module, a cross-lung pressure calculation module, an airway pressure-volume ring calculation module, a WOB calculation module, an airway blocking module, a respiratory system compliance calculation module, a chest wall compliance calculation module, a lung compliance calculation module and an endogenous PEEP detection module. According to the technical scheme, the flow velocity, airway pressure and esophageal pressure data acquisition and analysis equipment provided by the invention synchronously acquires related data of respiratory mechanics with high resolution, and performs real-time or offline analysis on the data.
Owner:BEIJING TIANTAN HOSPITAL AFFILIATED TO CAPITAL MEDICAL UNIV
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com