Patents
Literature
70 results about "Non-invasive ventilation" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
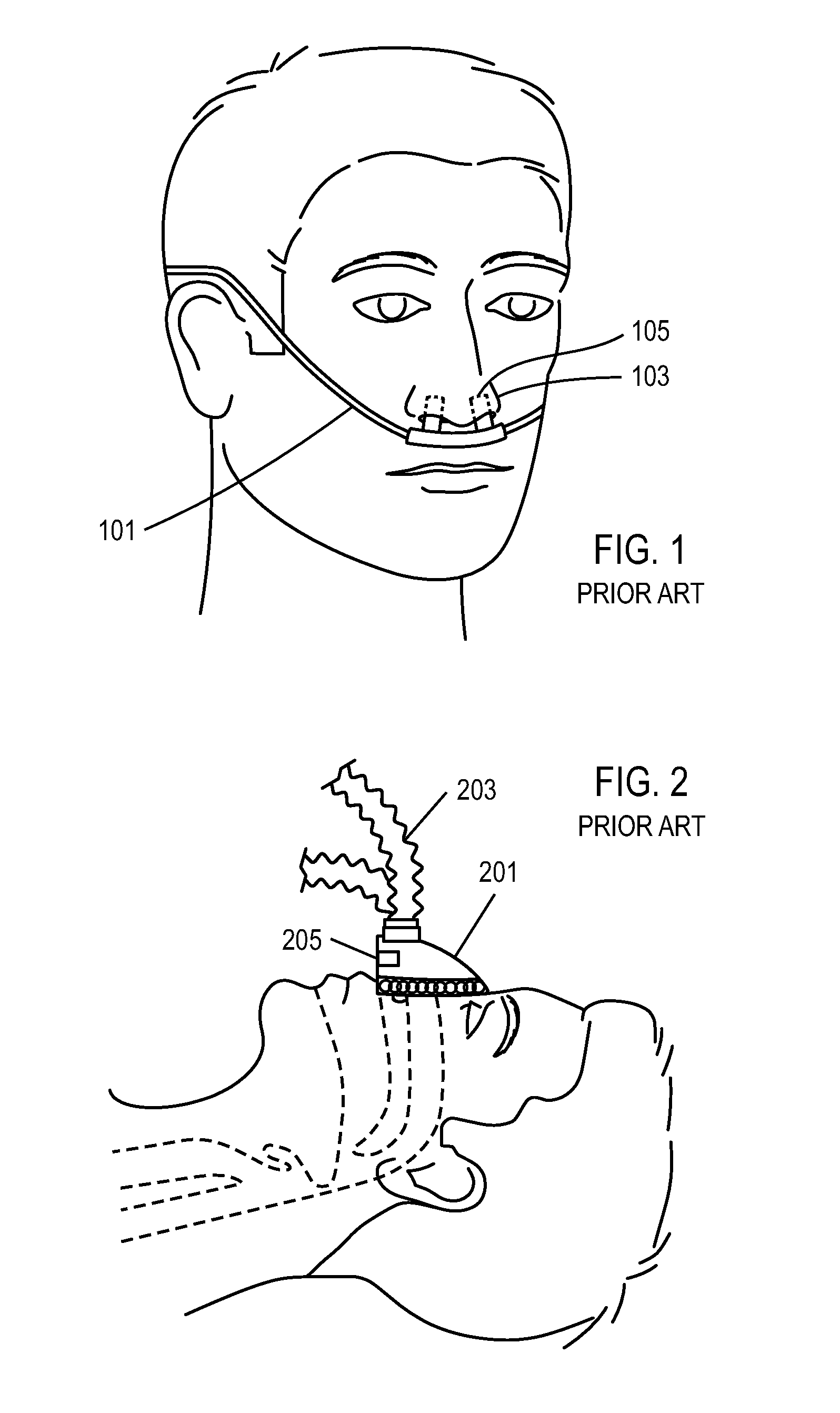
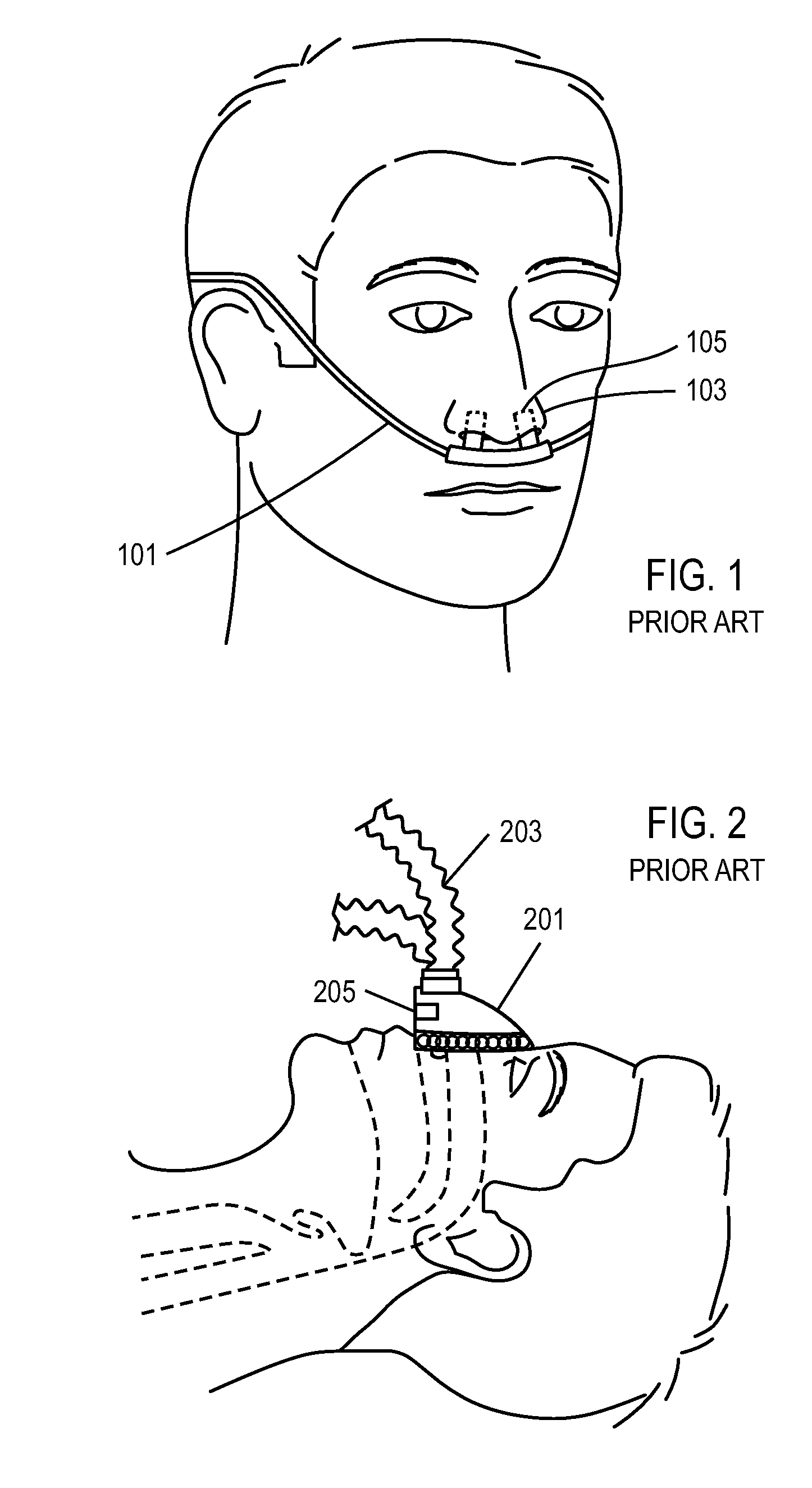
Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask or nasal mask. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face, but without a need for tracheal intubation (a tube through the mouth into the windpipe). While there are similarities with regards to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.
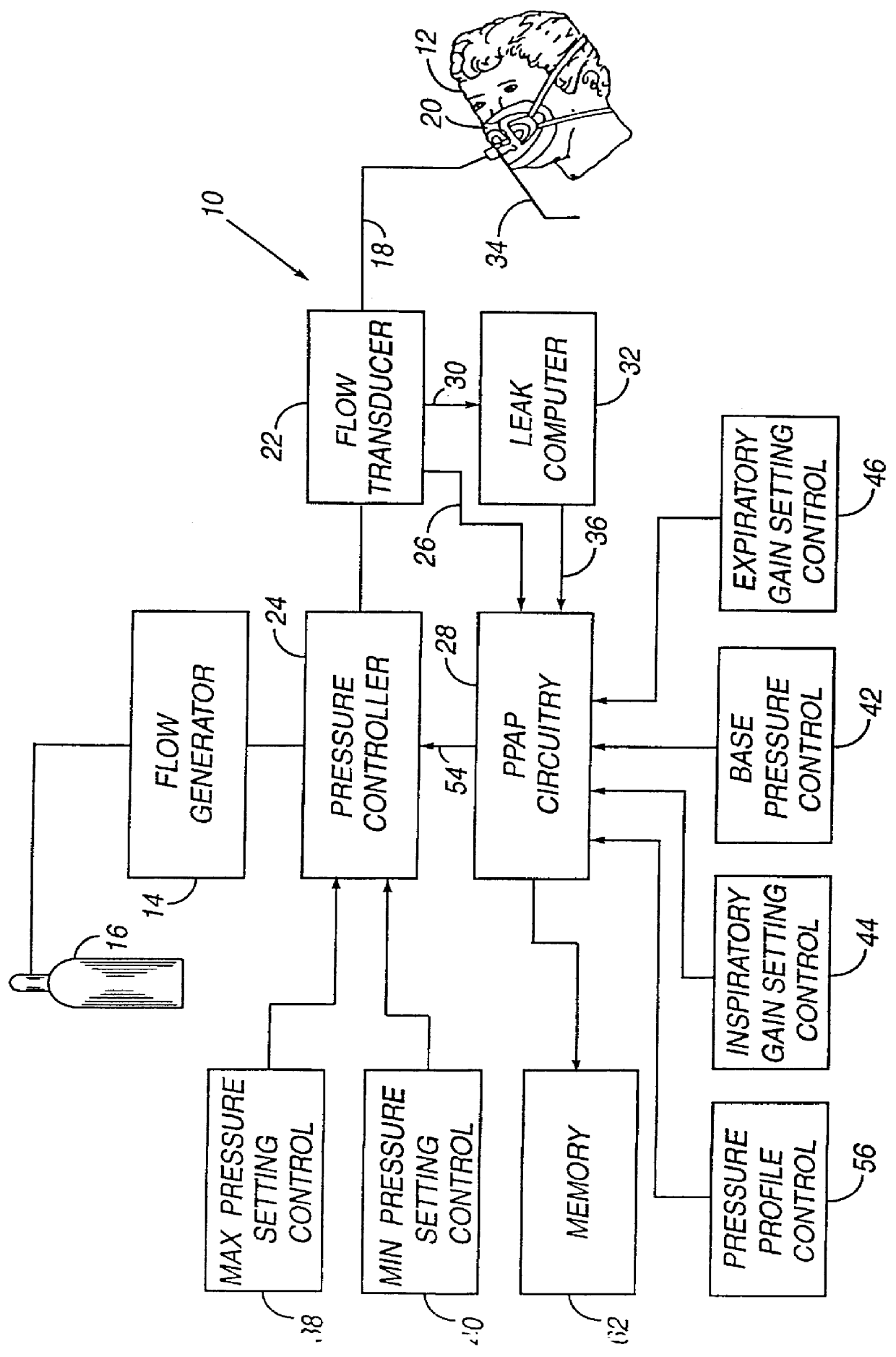
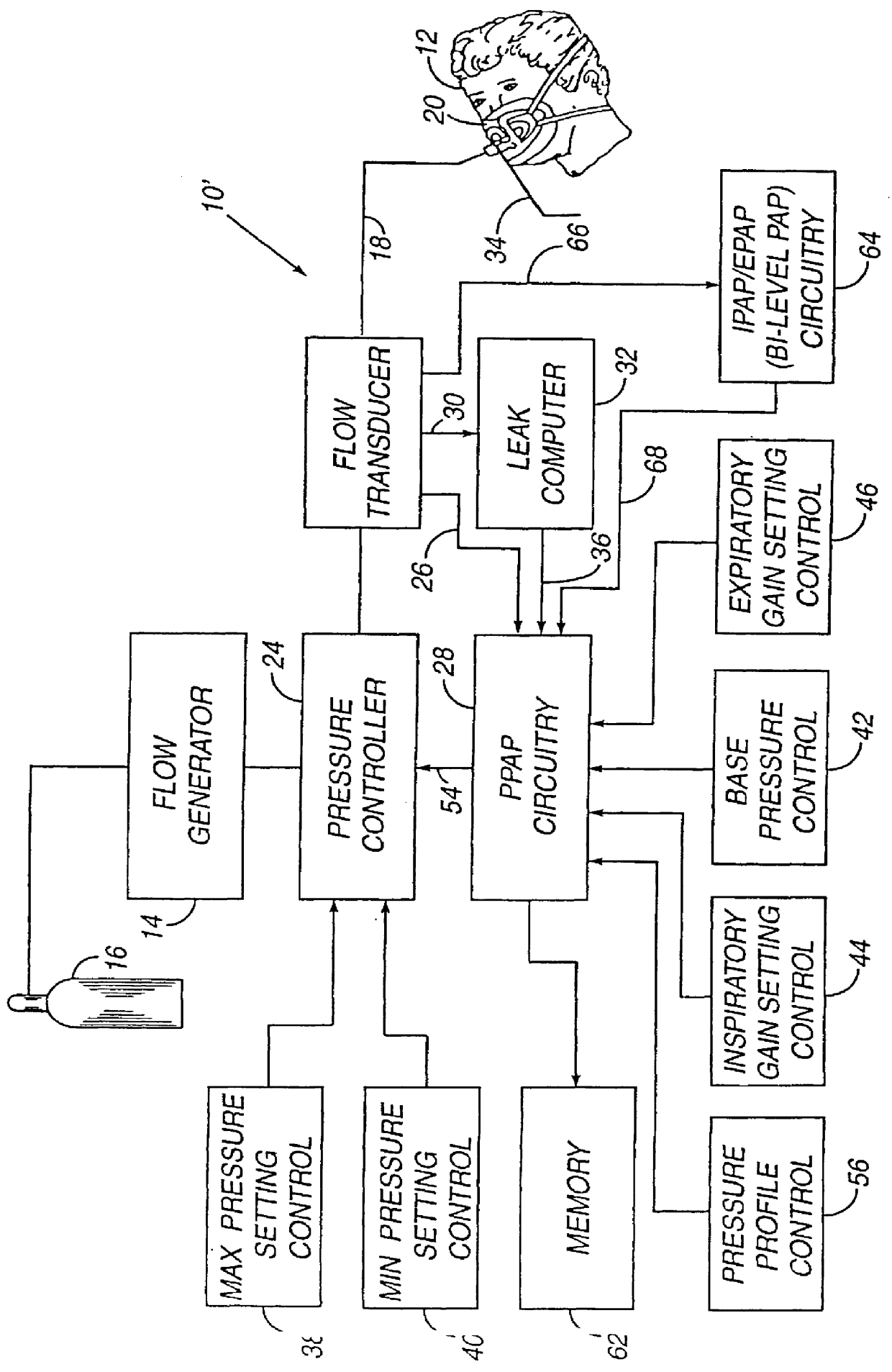
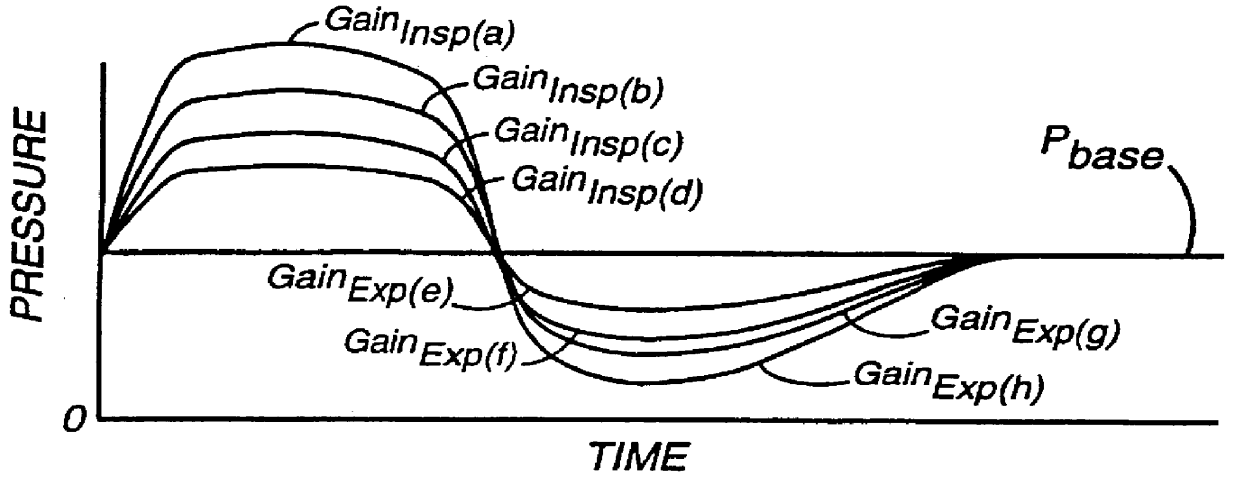
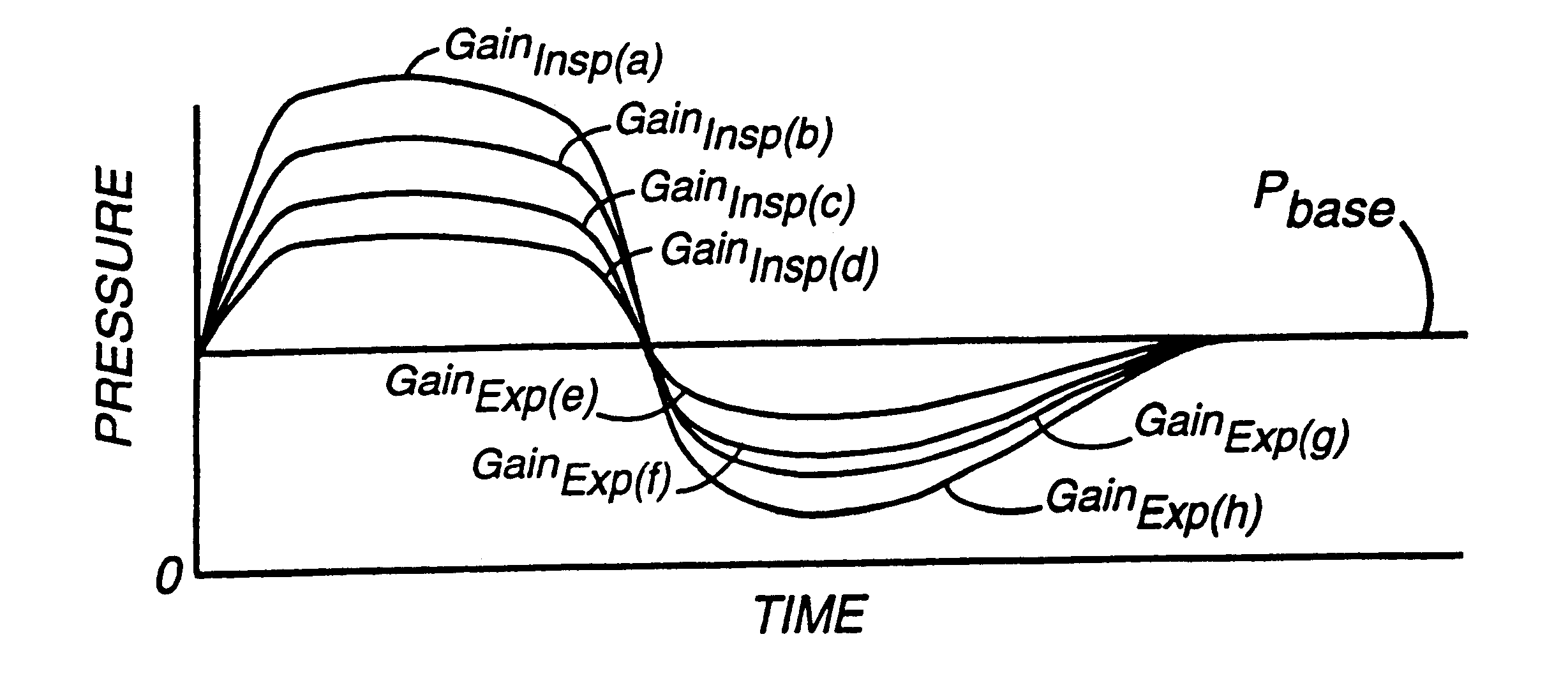
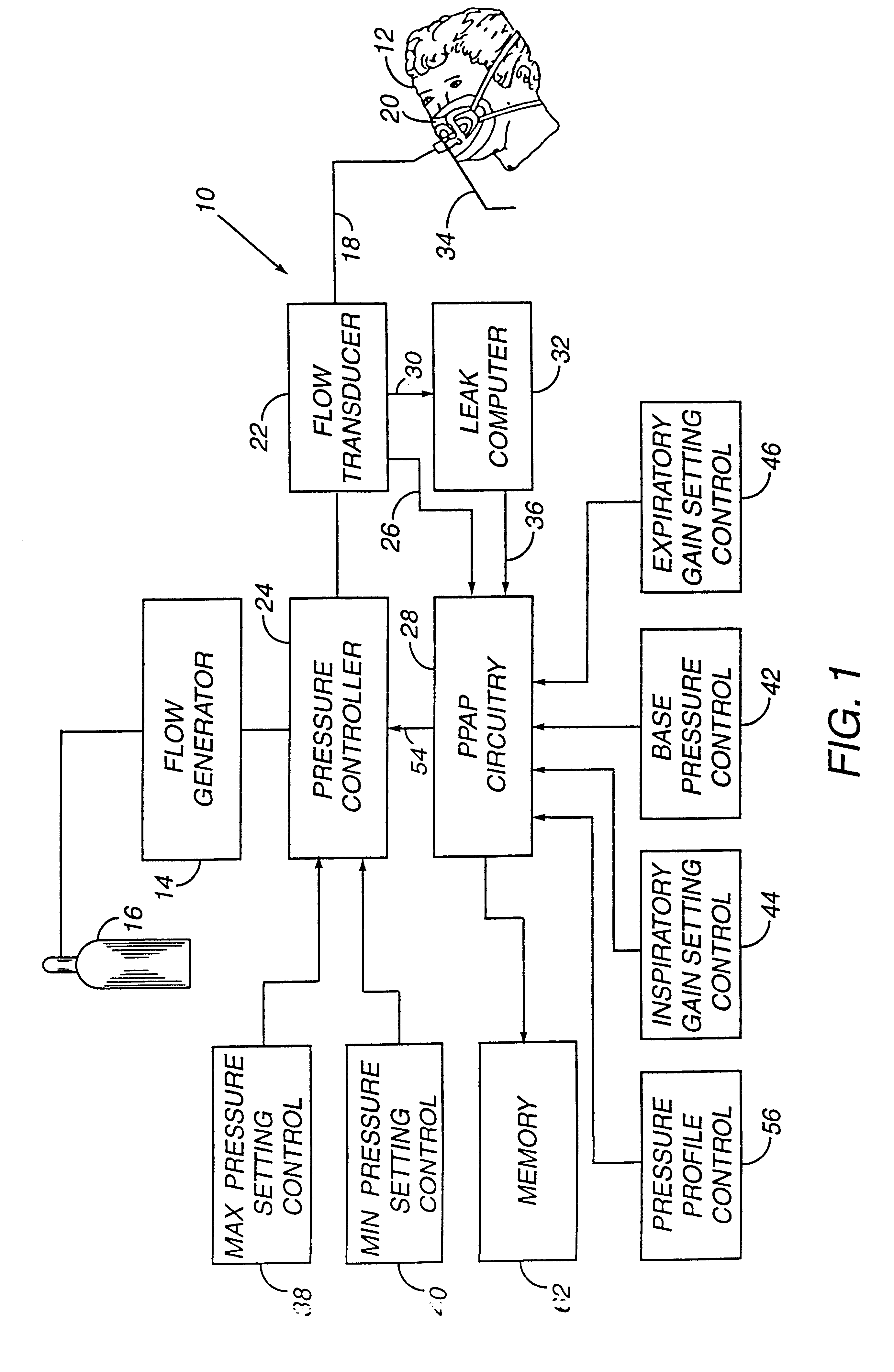
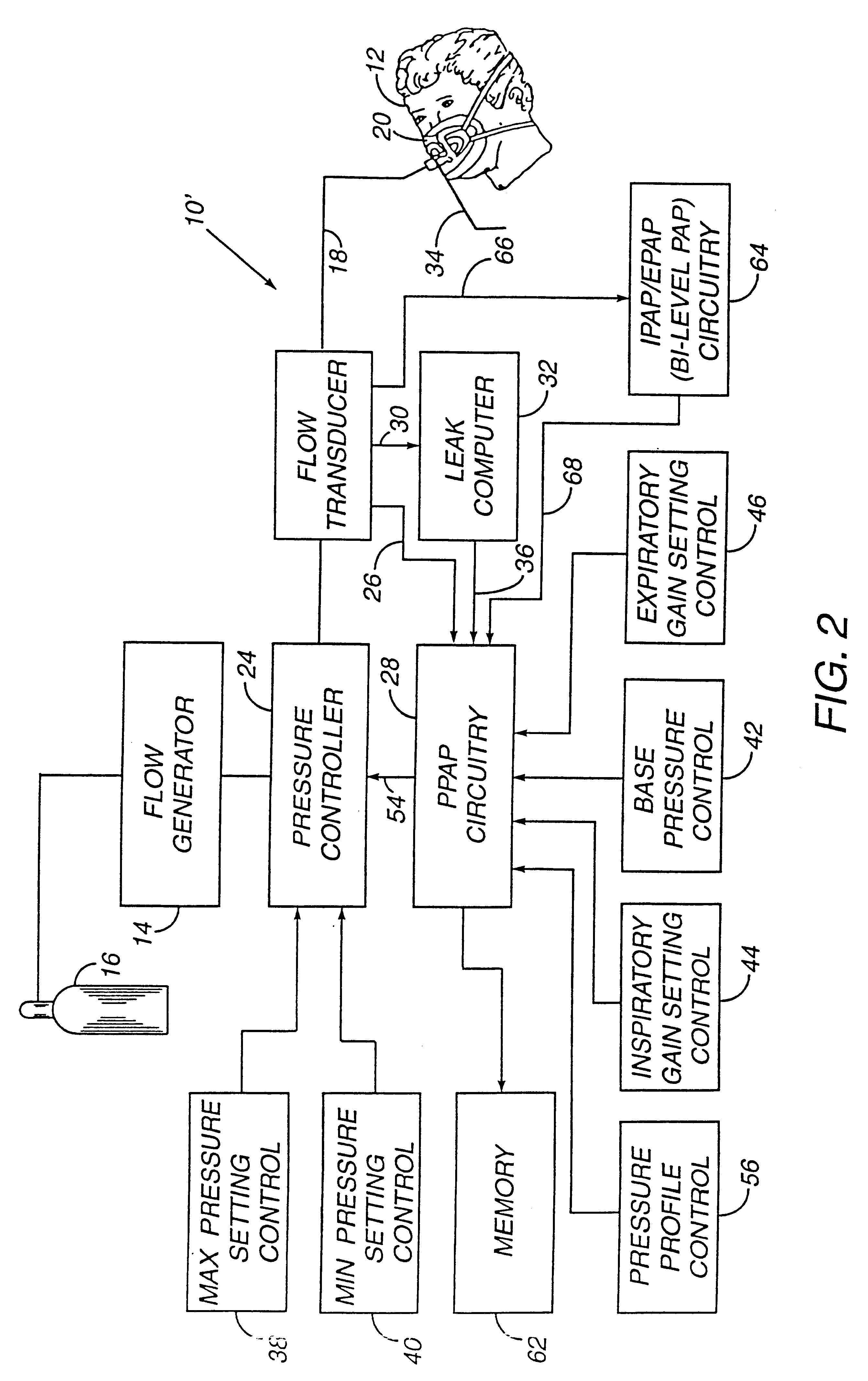
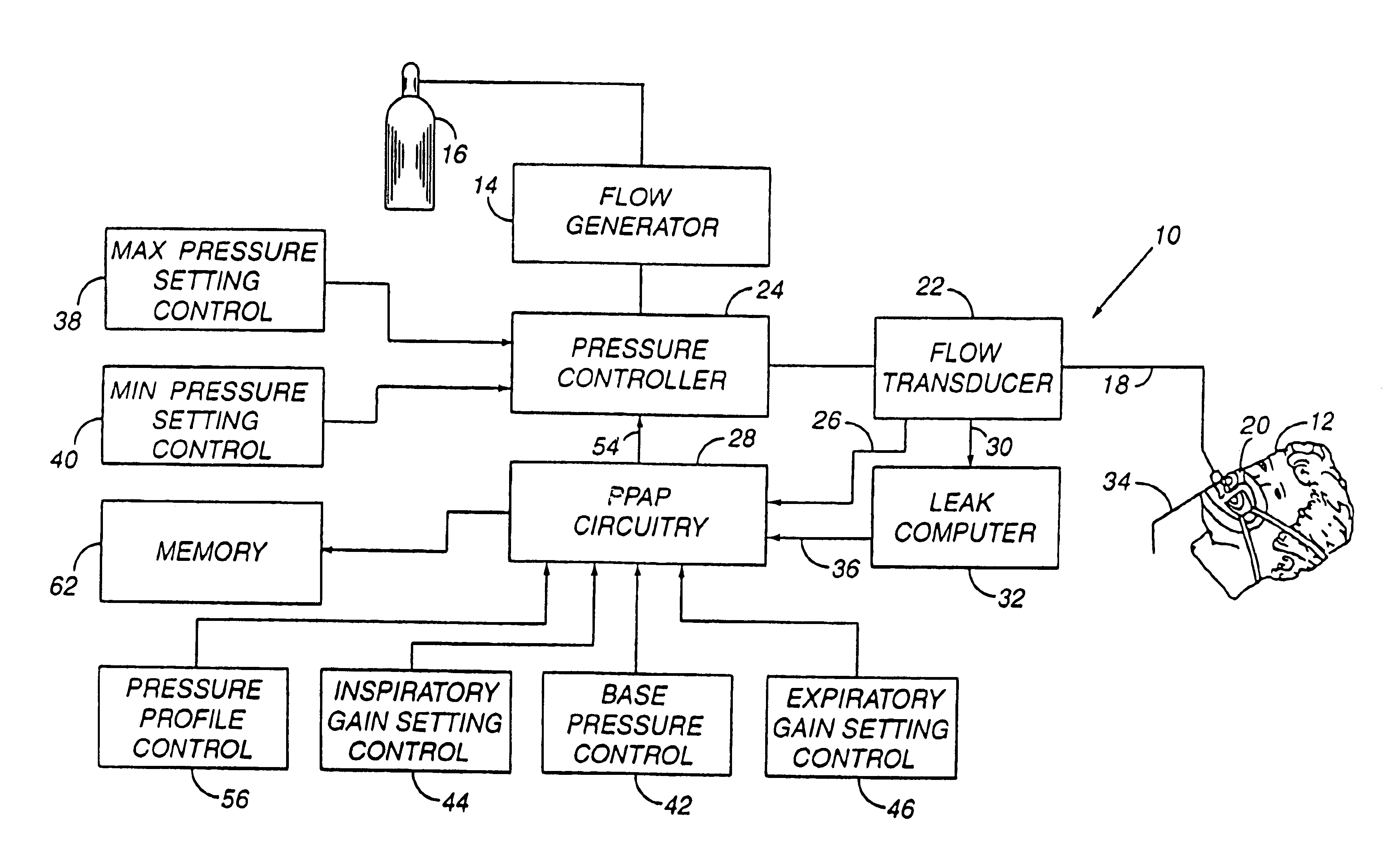
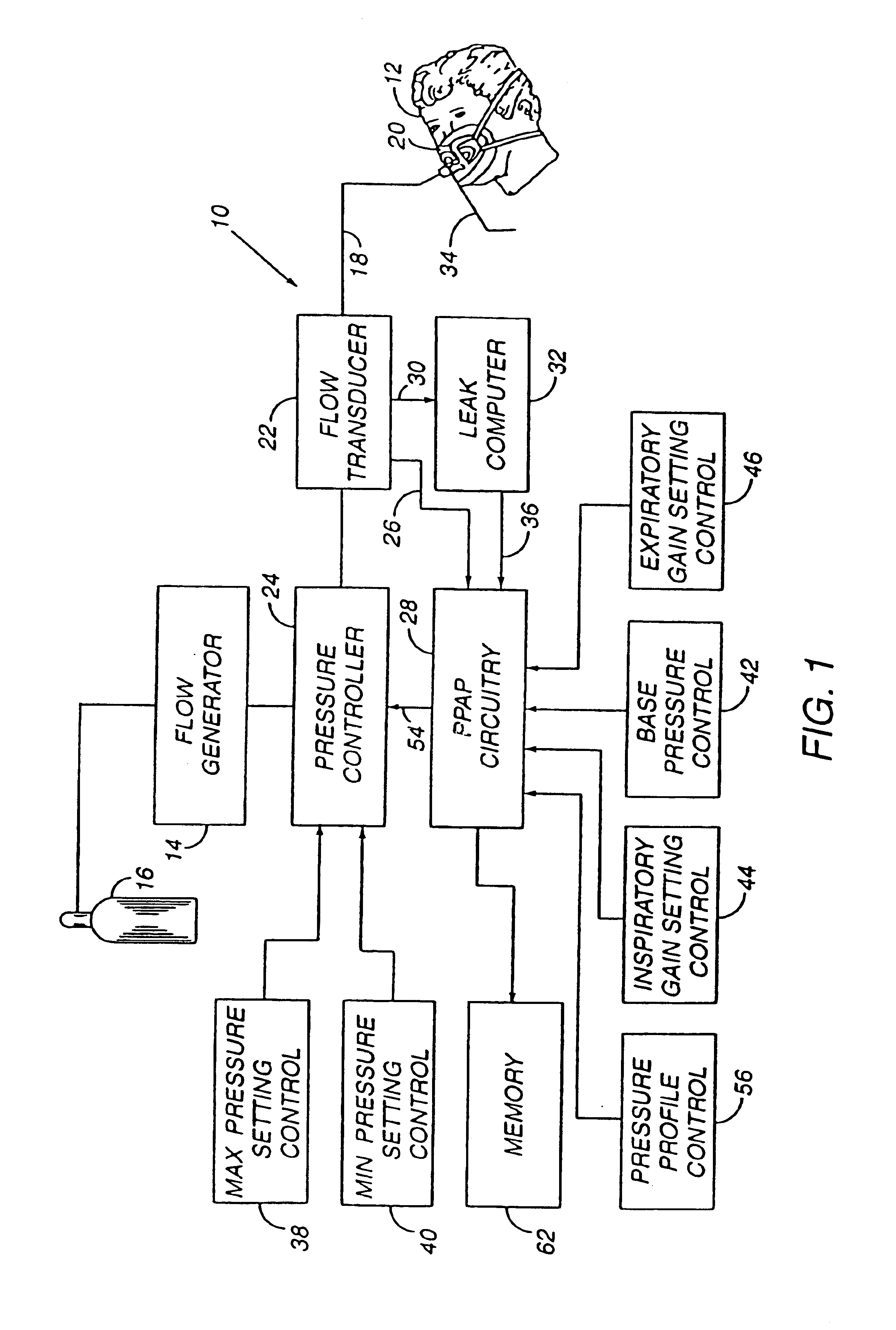
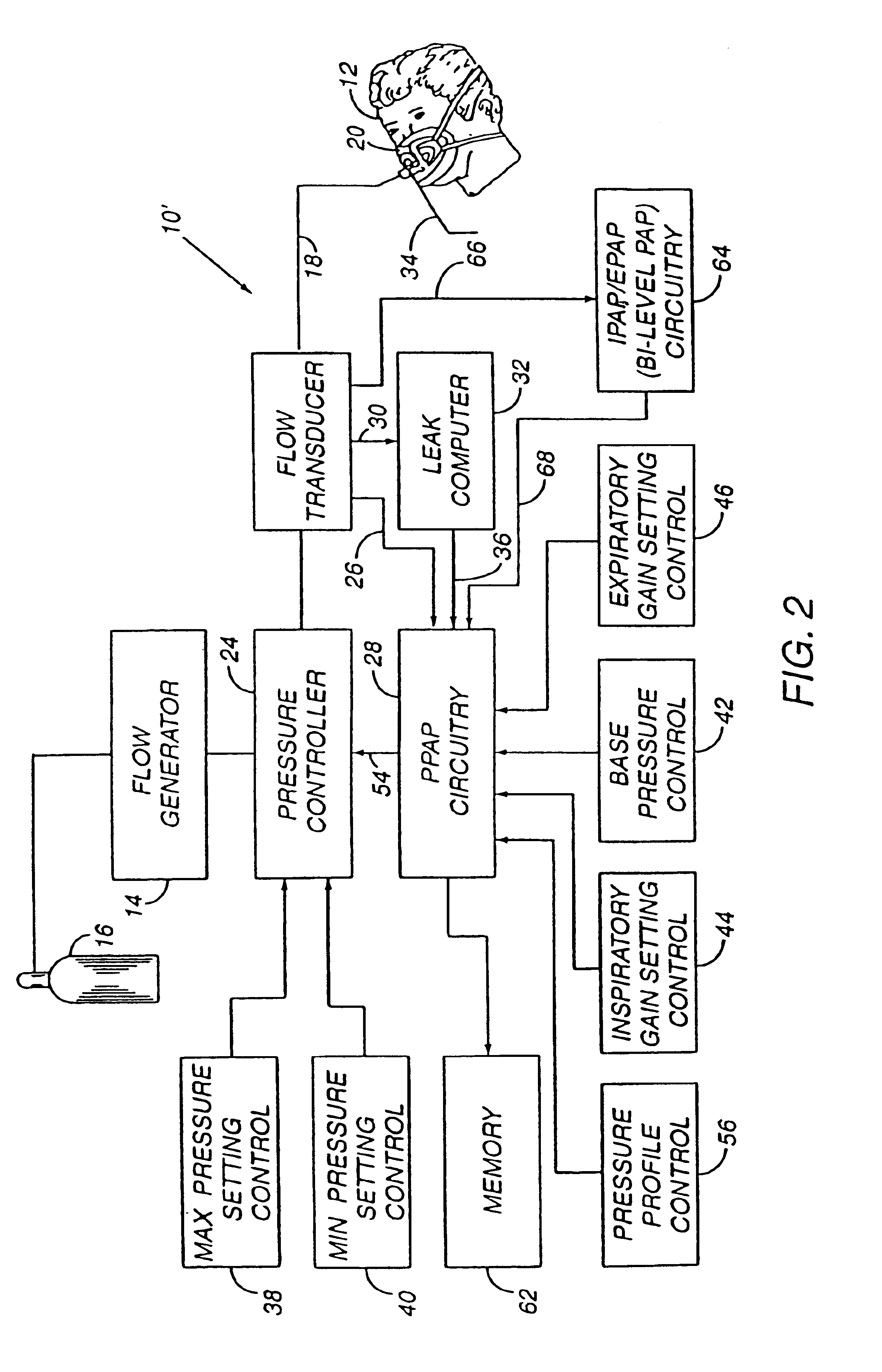
Method and apparatus for providing positive airway pressure to a patient
InactiveUS6105575AReduce cardiac preloadEasily detecting exhalationRespiratorsOperating means/releasing devices for valvesMedical disorderPositive pressure
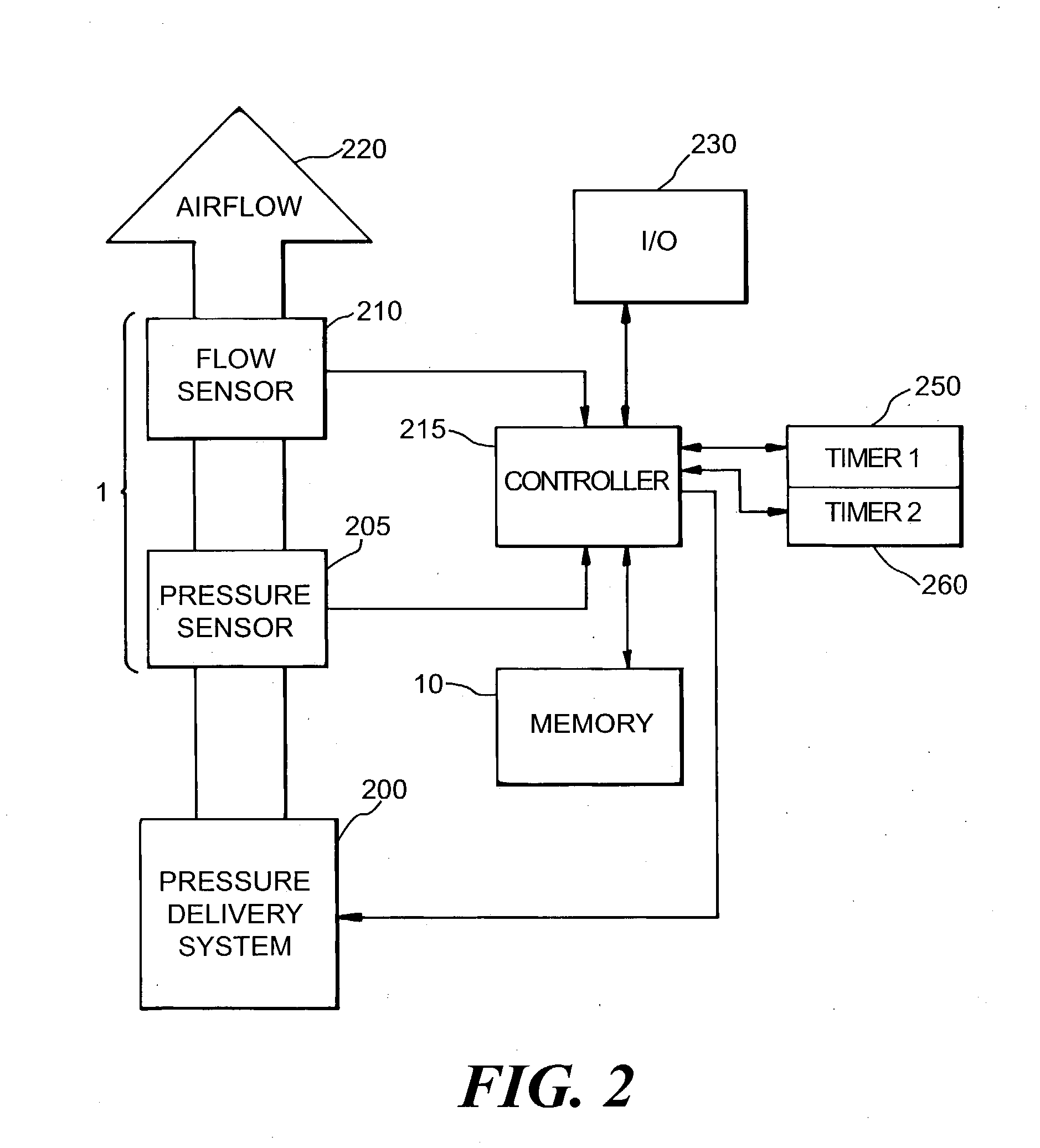
A system including methods and apparatus for treatment of a medical disorder such as obstructive sleep apnea or congestive heart failure. The system involves applying separate and independent gains to flow rates of pressurized gas delivered to a patient during inspiratory and expiratory phases of a respiratory cycle to deliver the pressurized gas in proportion to the respective gains during inspiration and expiration. A base pressure may be applied in addition to the gain-modified pressures and an elevated pressure profile may be employed to assist or control inspiration. The system may be fully automated responsive to feedback provided by a flow sensor that determines the estimated patient flow rate. A leak computer can be included to instantaneously calculate gas leakage from the system. The system may be utilized in connection with conventional continuous positive airway pressure (bi-level PAP) equipment to effect various beneficial treatment applications.
Owner:RIC INVESTMENTS LLC
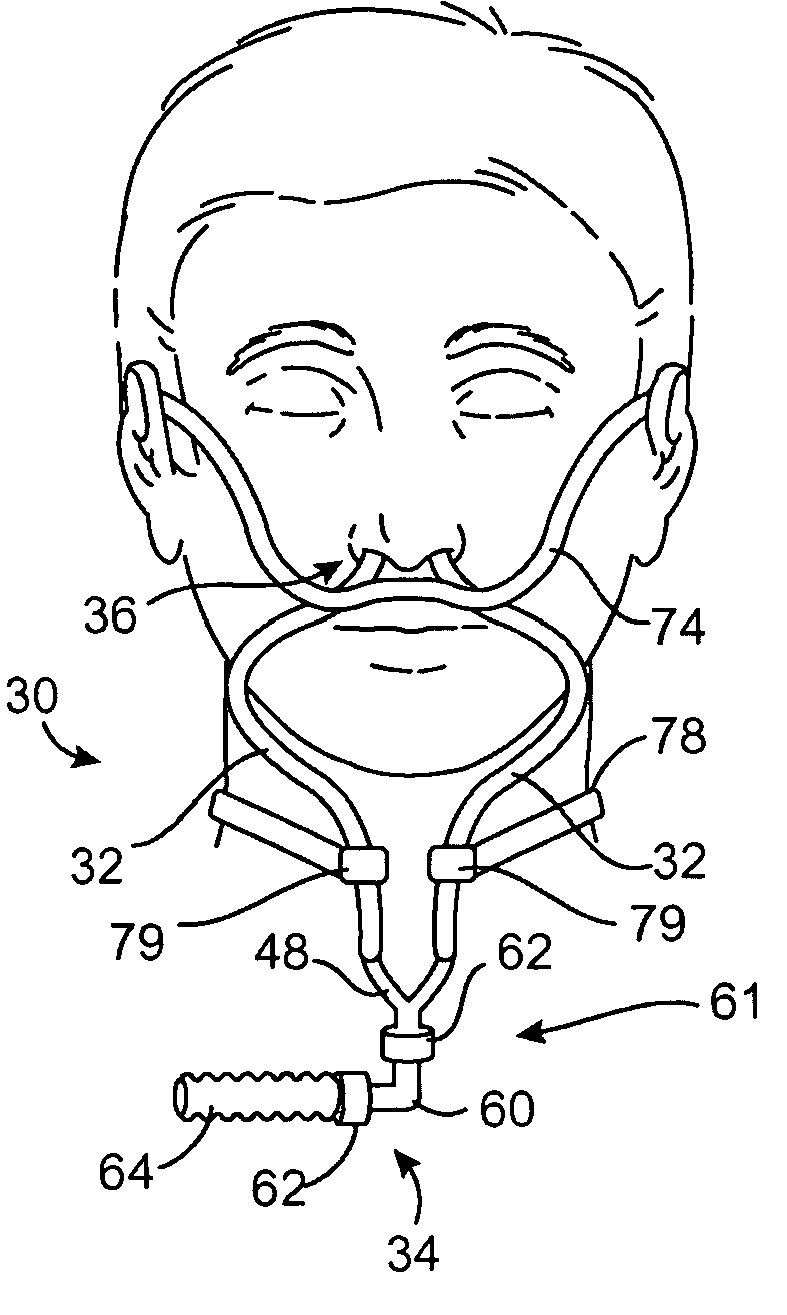
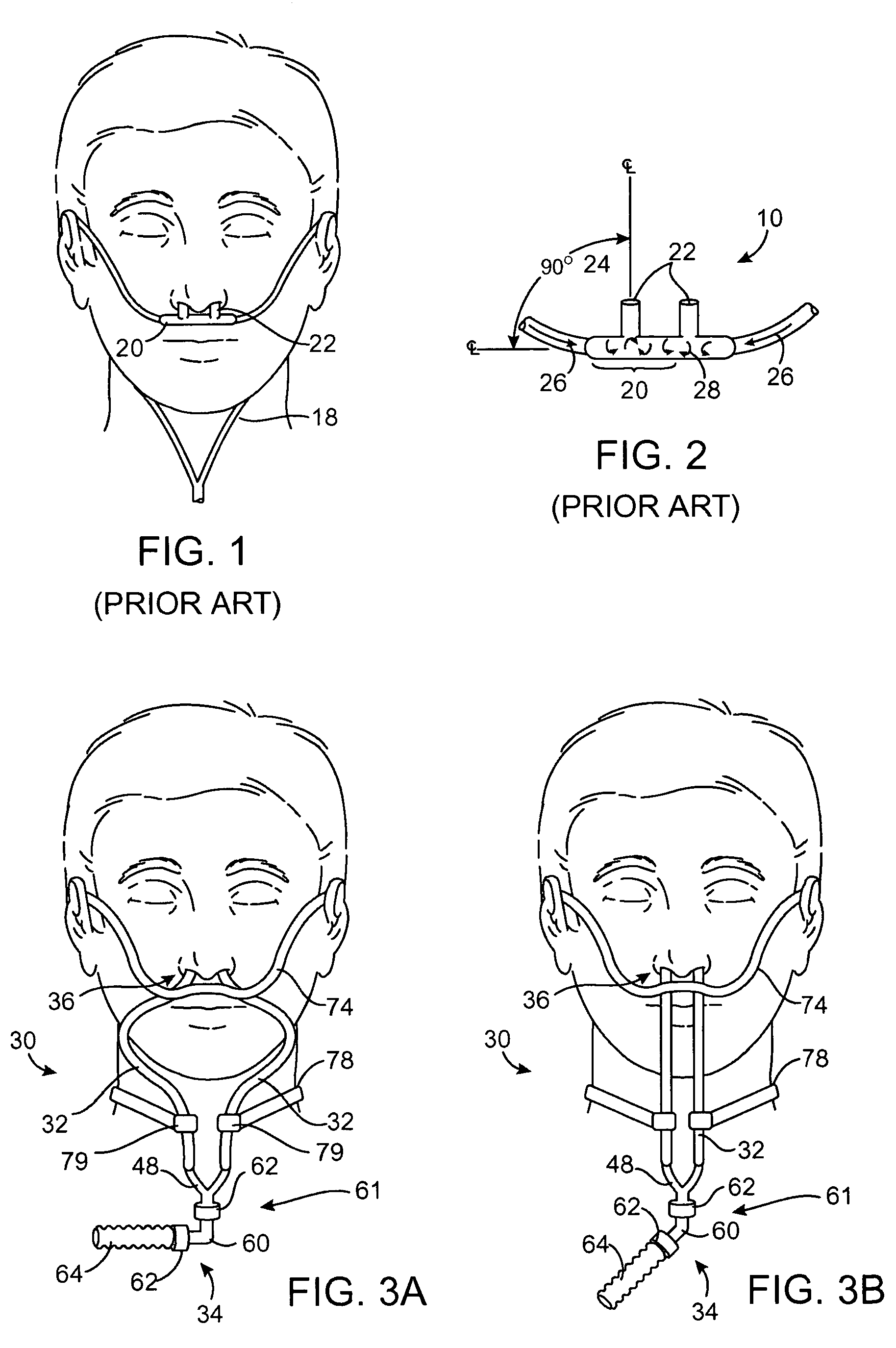
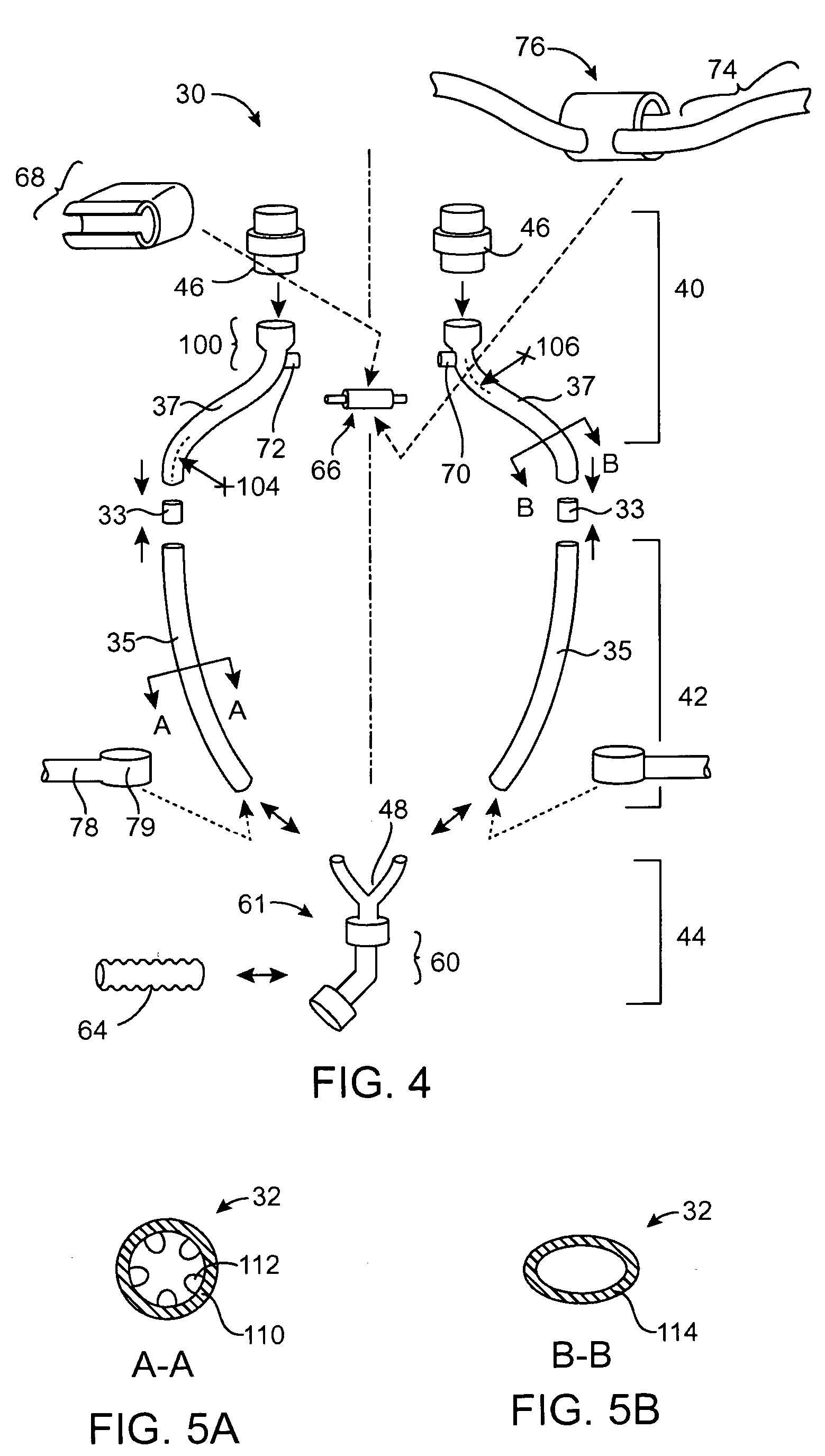
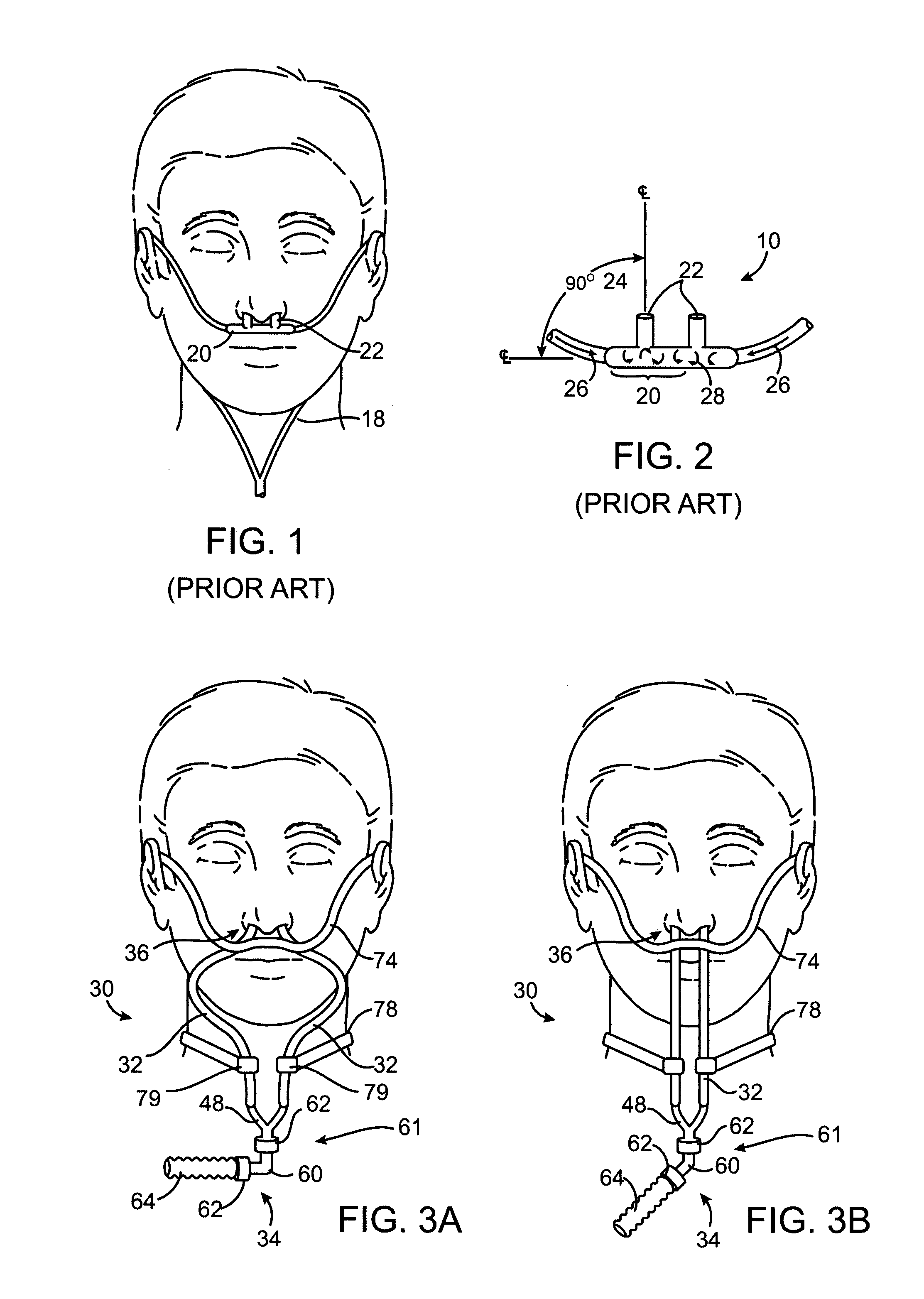
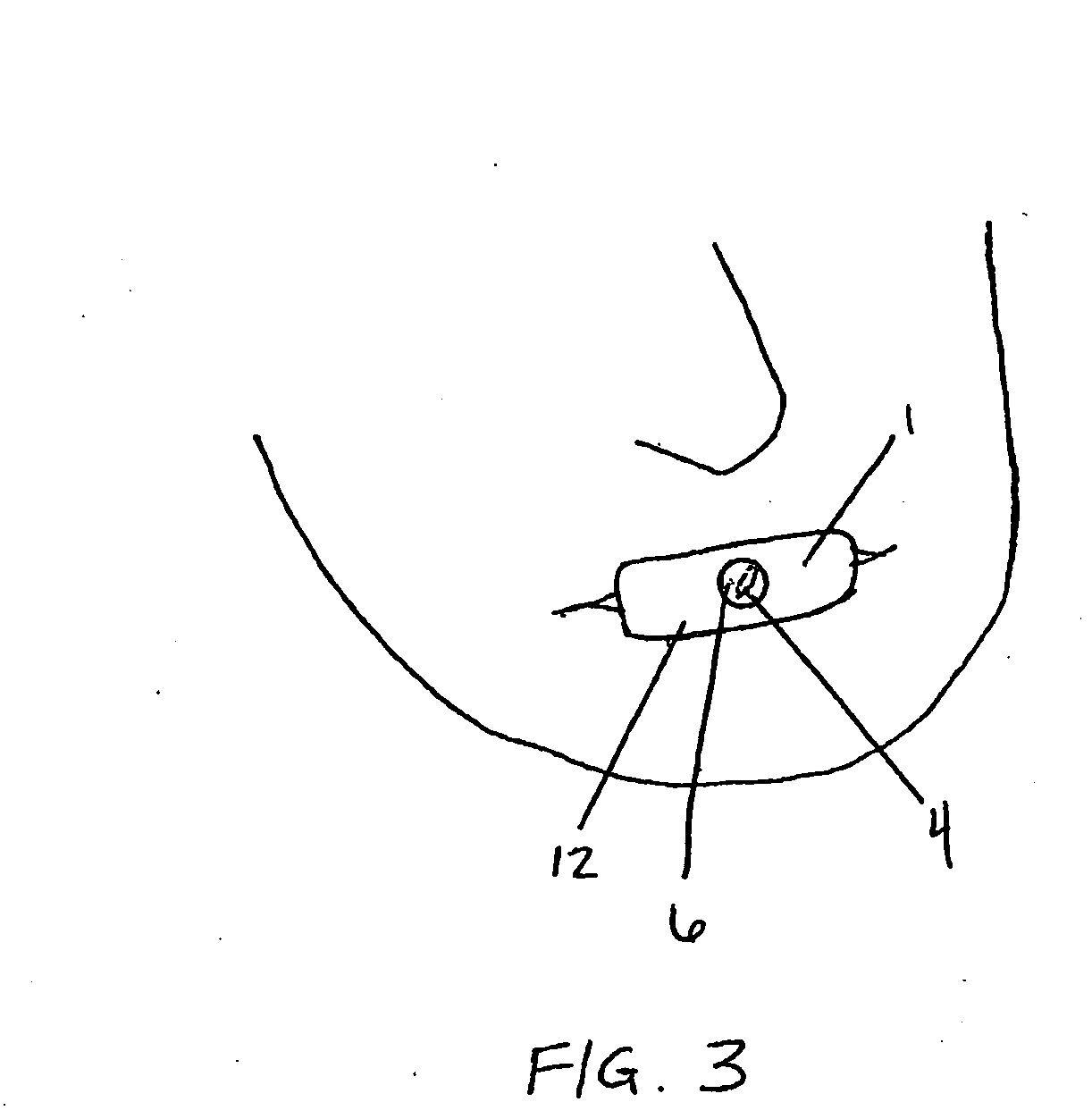
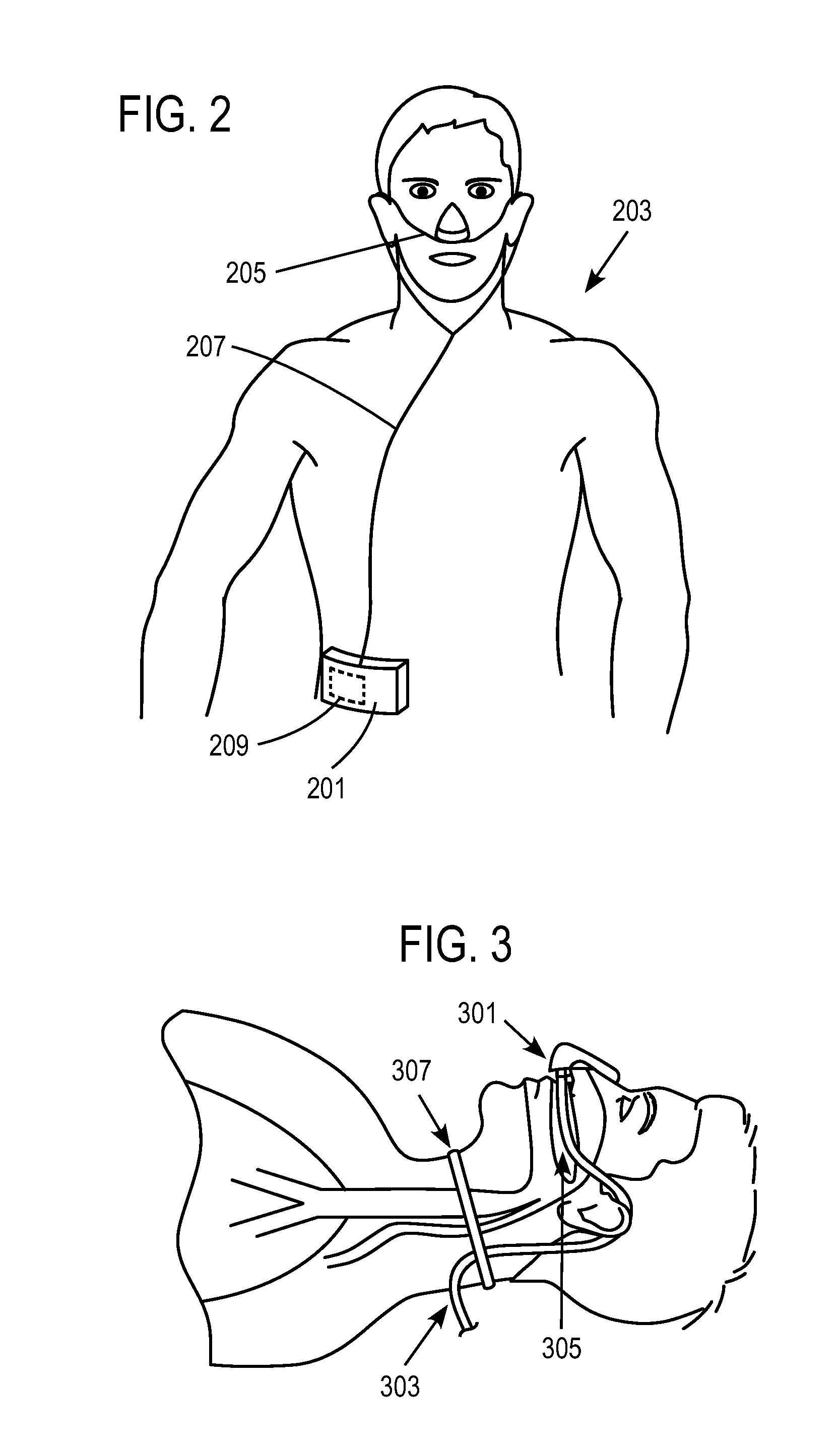
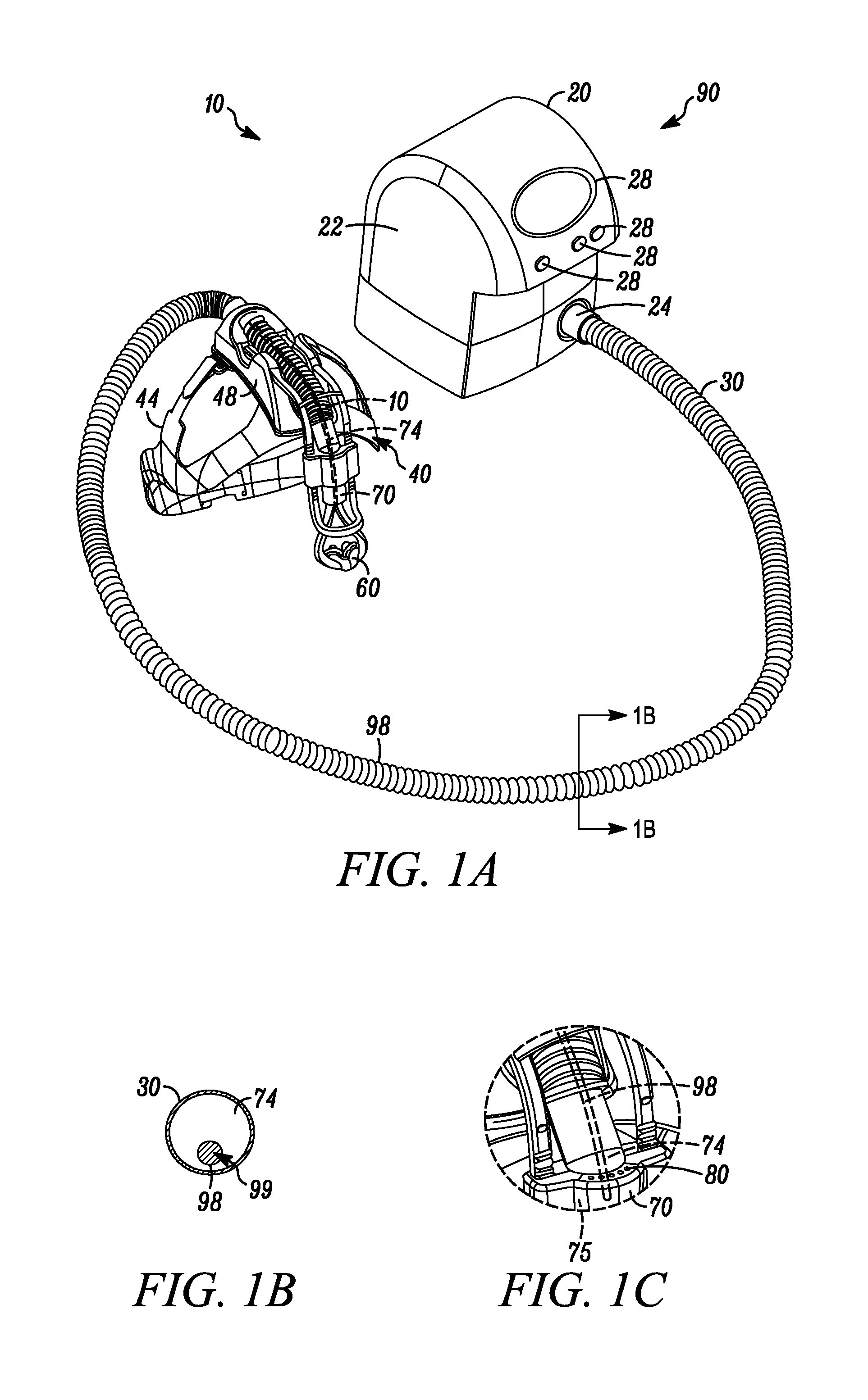
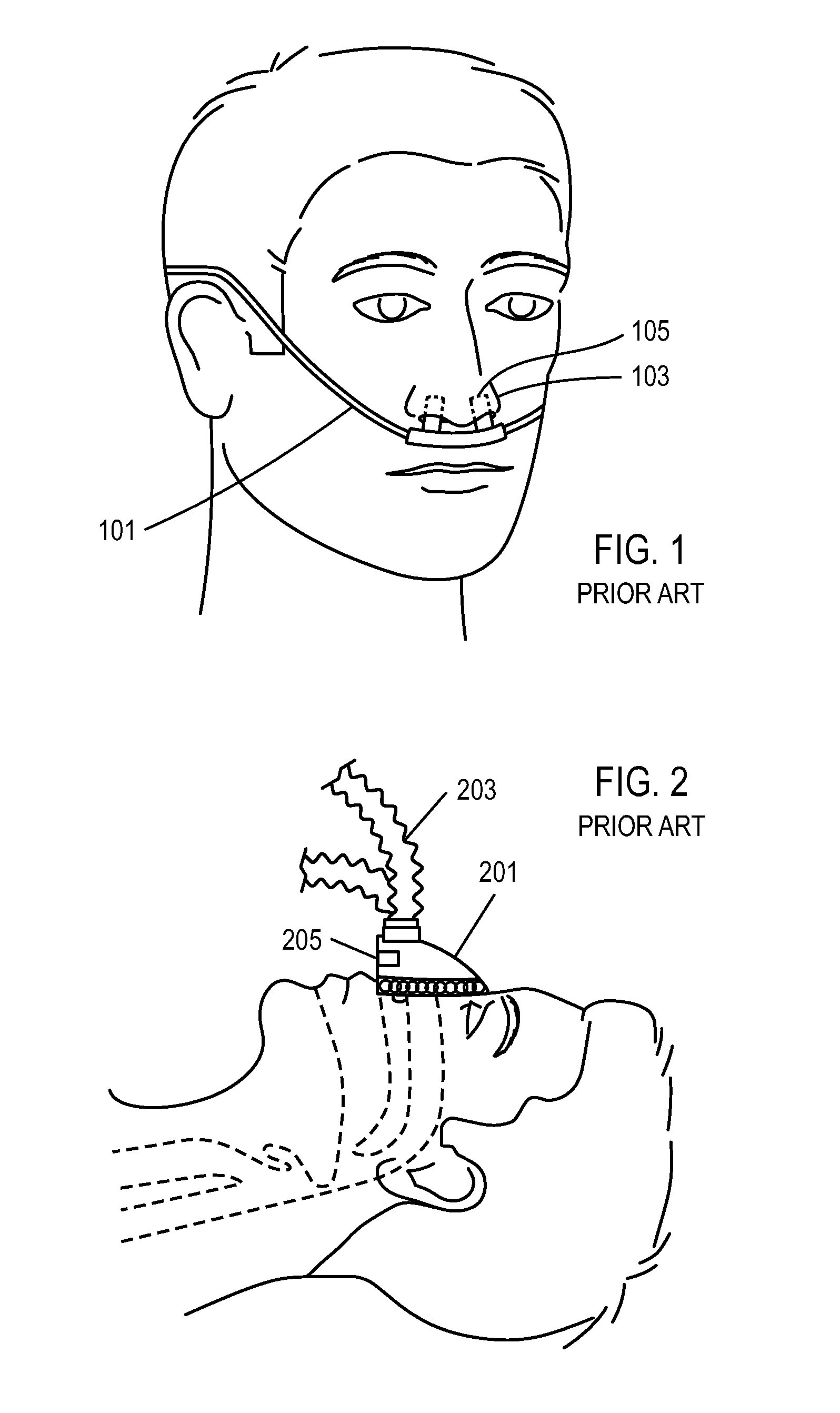
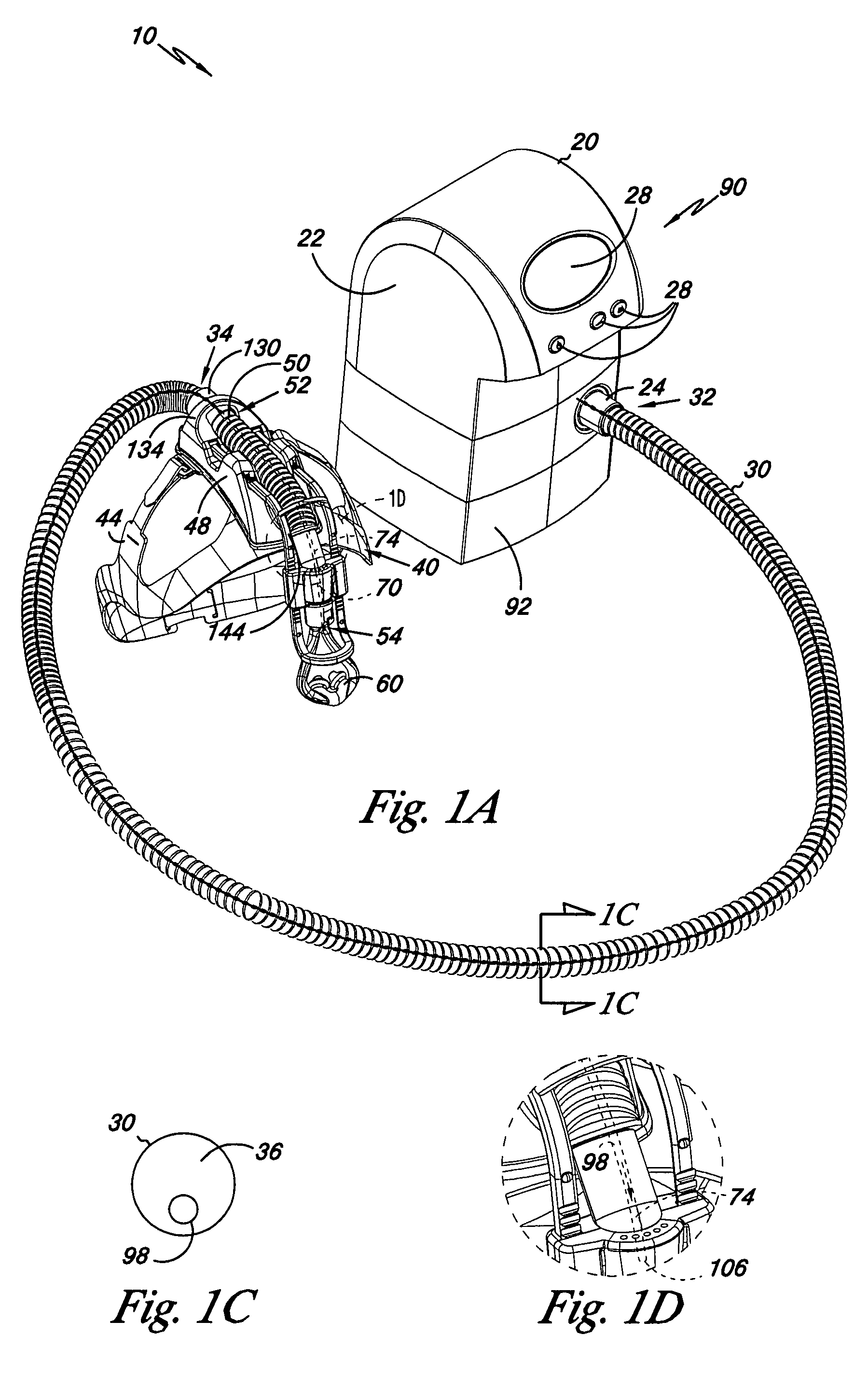
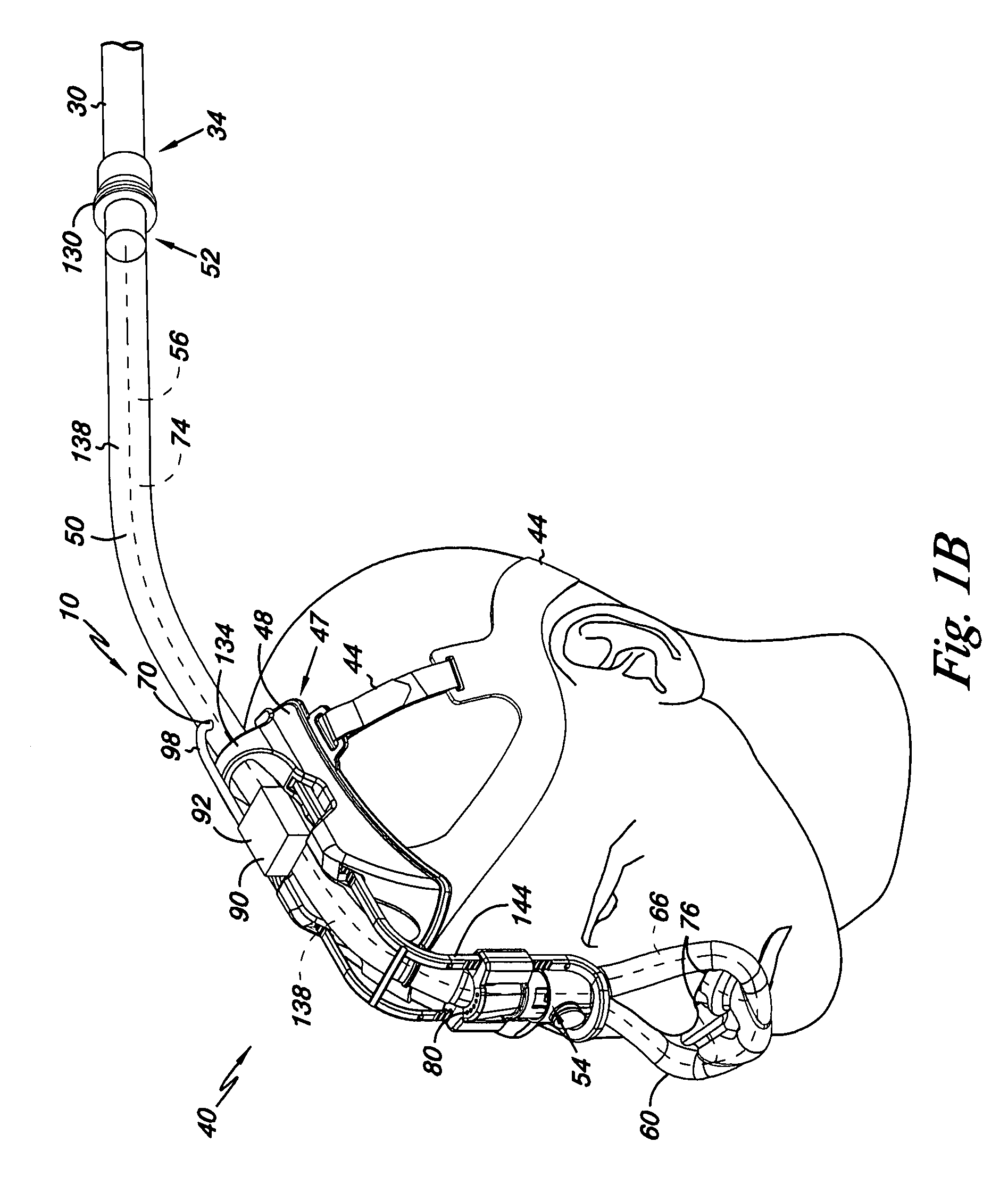
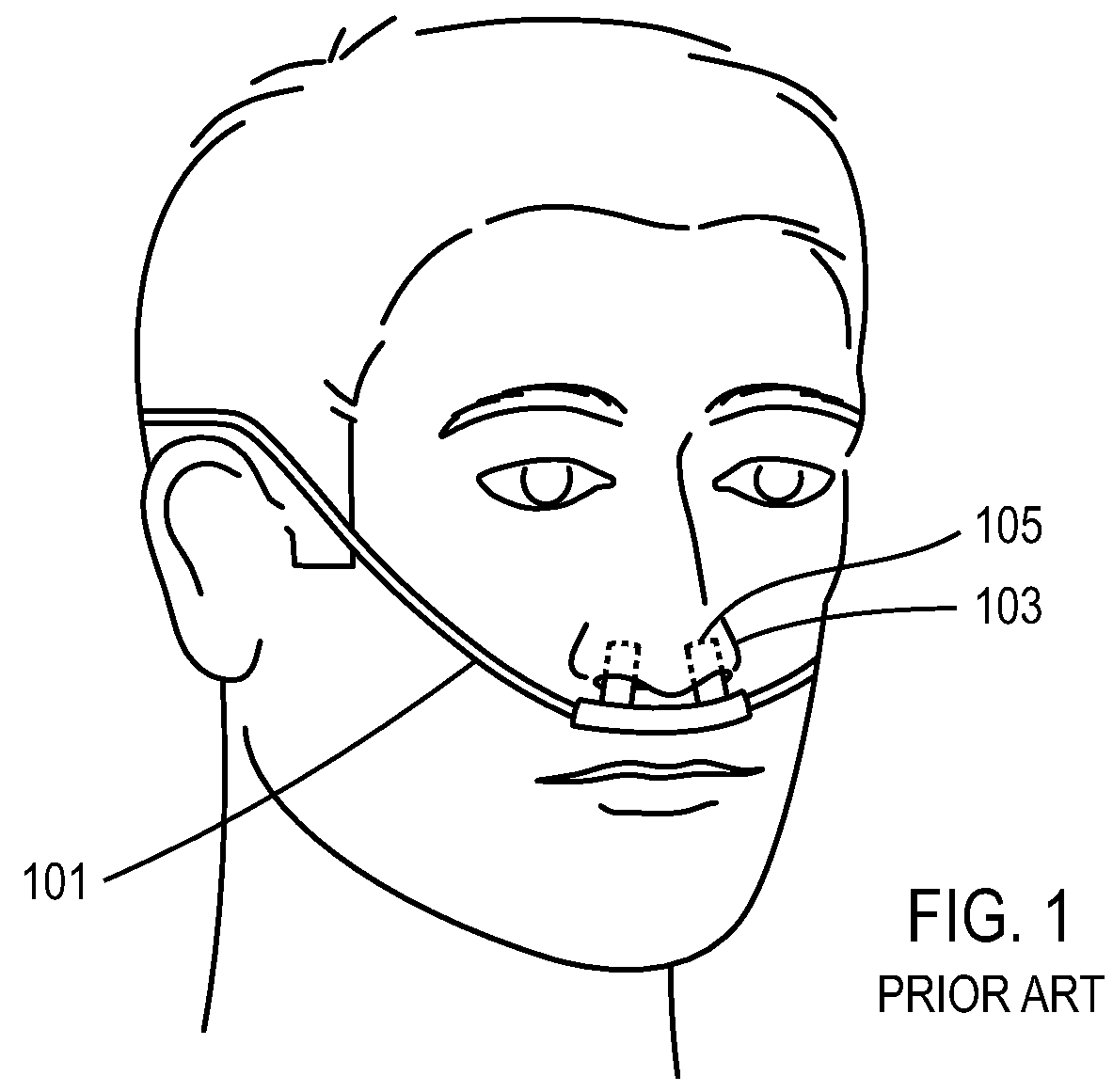
Method and device for non-invasive ventilation with nasal interface
ActiveUS20050066976A1Noise minimizationMinimize resistancePhysical therapyBreathing filtersNasal cavityNostril
A nasal ventilation interface including a pair of tubes configured to deliver a ventilation gas. The tubes are attachable at a first end to a ventilation gas supply hose and engageable at a second end with a person's nostril. A coupler is configured to align the pair of tubes with the person's nostrils, wherein each tube has an absence of pneumatic interconnection with the other tube.
Owner:MENLOLIFE
Method and apparatus for providing positive airway pressure to a patient
InactiveUS6609517B1Reduce cardiac preloadEasily detecting exhalationRespiratorsOperating means/releasing devices for valvesMedical disorderPositive pressure
A system including methods and apparatus for treatment of a medical disorder such as obstructive sleep apnea or congestive heart failure. The system involves applying separate and independent gains to flow rates of pressurized gas delivered to a patient during inspiratory and expiratory phases of a respiratory cycle to deliver the pressurized gas in proportion to the respective gains during inspiration and expiration. A base pressure may be applied in addition to the gain-modified pressures and an elevated pressure profile may be employed to assist or control inspiration. The system may be fully automated responsive to feedback provided by a flow sensor that determines the estimated patient flow rate. A leak computer can be included to instantaneously calculate gas leakage from the system. The system may be utilized in connection with conventional continuous positive airway pressure (bi-level PAP) equipment to effect various beneficial treatment applications.
Owner:RIC INVESTMENTS LLC
Method and apparatus for providing positive airway pressure to a patient
InactiveUS6932084B2Easily detecting exhalationDecrease in EPAPRespiratorsOperating means/releasing devices for valvesMedical disorderPositive pressure
A system including methods and apparatus for treatment of a medical disorder such as obstructive sleep apnea or congestive heart failure. The system involves applying a gain to flow rate of pressurized gas delivered to a patient during inspiratory and / or expiratory phases of a respiratory cycle to deliver the pressurized gas in proportion to the respective gains during inspiration and / or expiration. A base pressure may be applied in addition to the gain-modified pressures and an elevated pressure profile may be employed to assist or control inspiration. The system may be fully automated responsive to feedback provided by a flow sensor that determines the estimated patient flow rate. A leak computer can be included to instantaneously calculate gas leakage from the system. The system may be utilized in connection with conventional continuous positive airway pressure treatments, such as CPAP or bi-level positive airway pressure equipment to effect various beneficial treatment applications.
Owner:RIC INVESTMENTS LLC
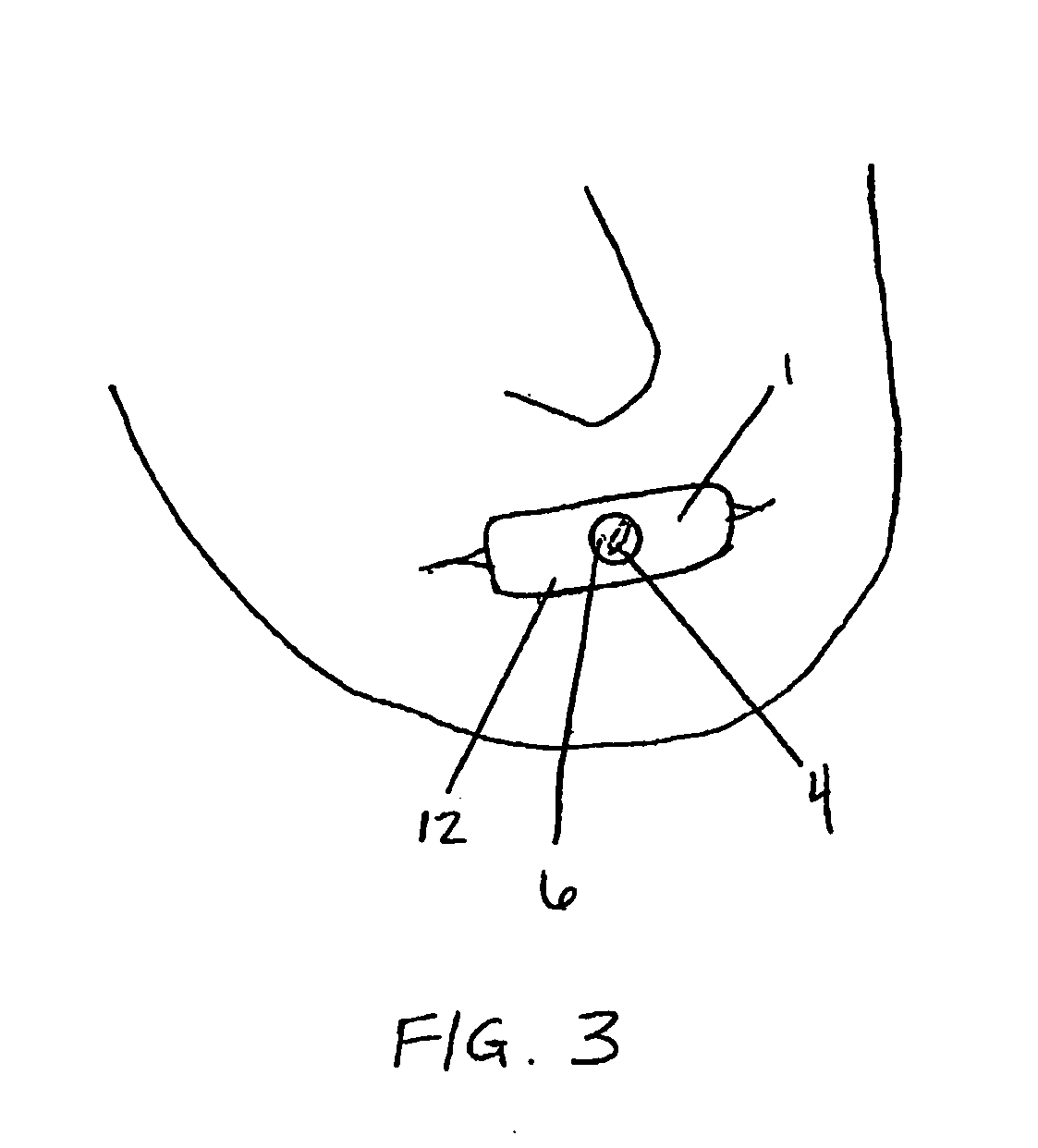
Method and device for non-invasive ventilation with nasal interface
ActiveUS7406966B2Retain comfortNoise minimizationPhysical therapyBreathing filtersNasal cavityNostril
A nasal ventilation interface including a pair of tubes configured to deliver a ventilation gas. The tubes are attachable at a first end to a ventilation gas supply hose and engageable at a second end with a person's nostril. A coupler is configured to align the pair of tubes with the person's nostrils, wherein each tube has an absence of pneumatic interconnection with the other tube.
Owner:MENLOLIFE
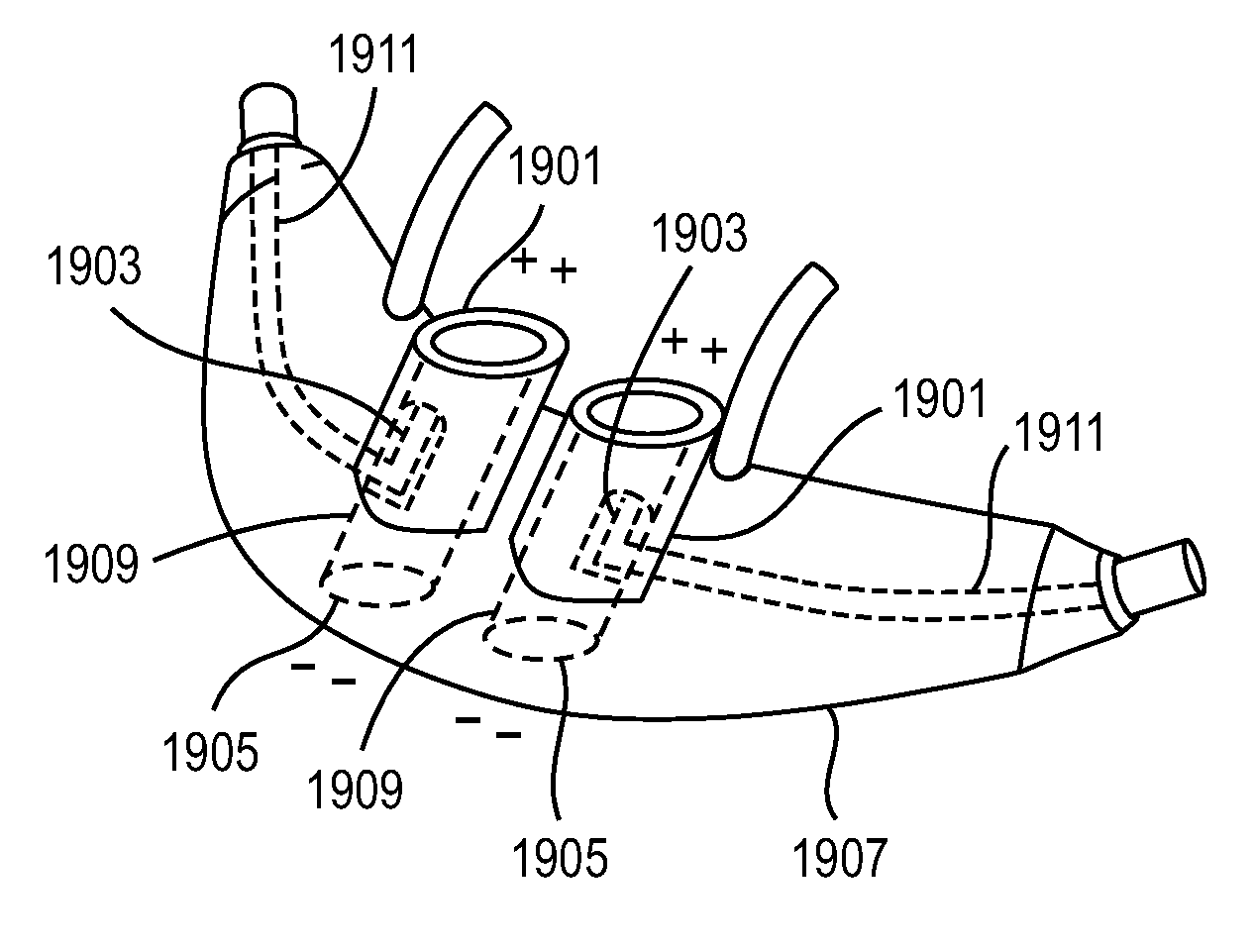
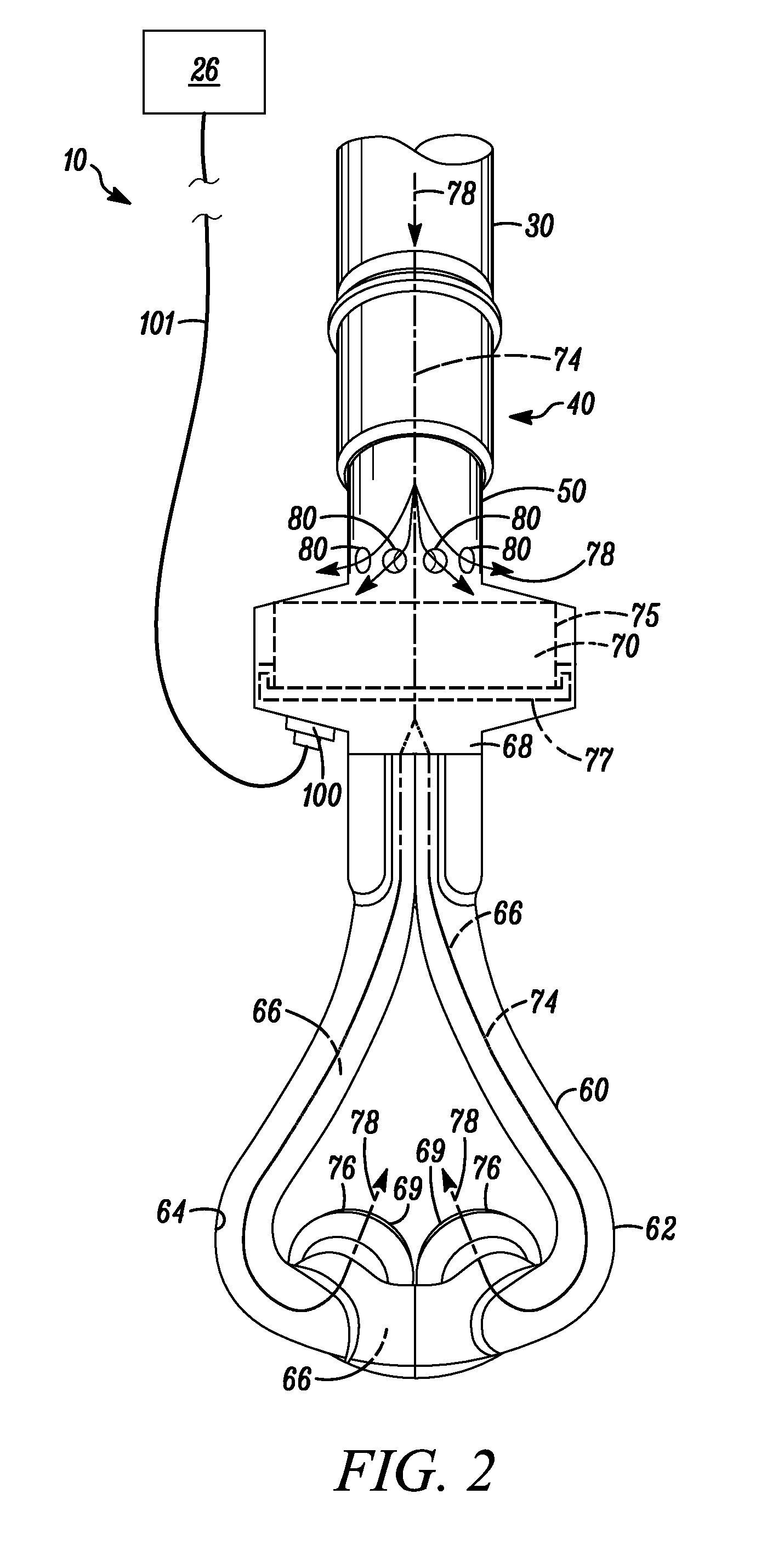
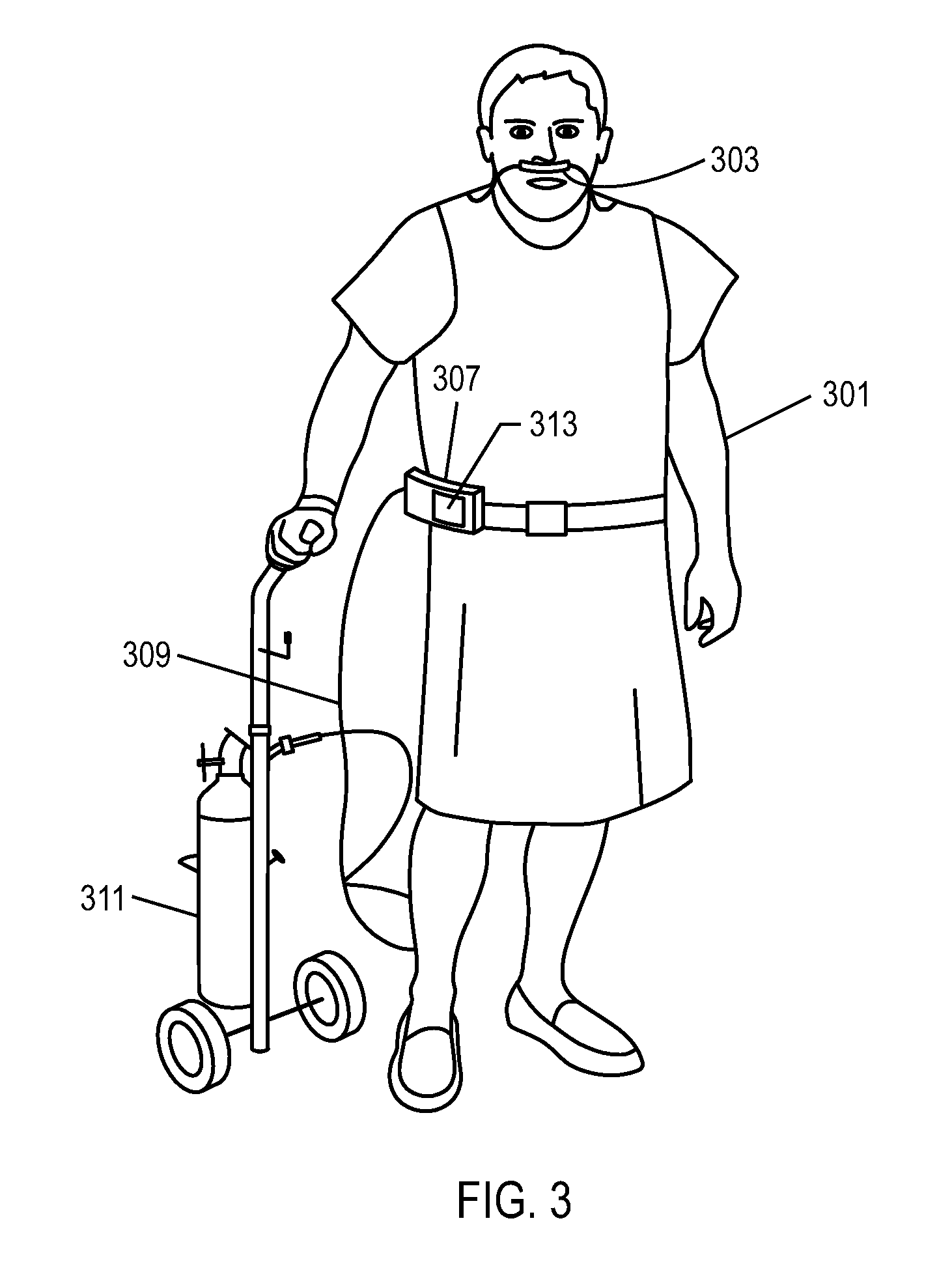
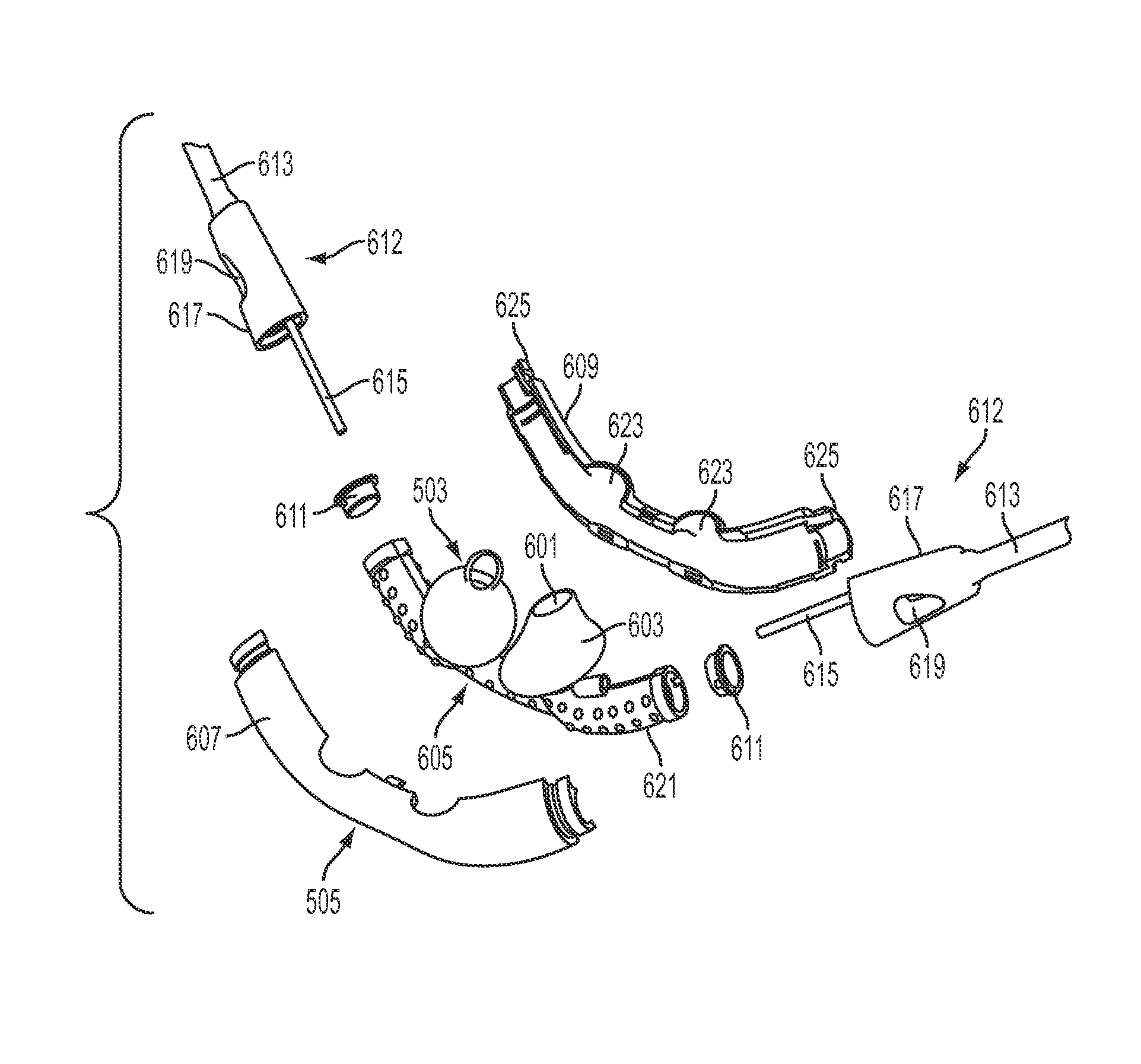
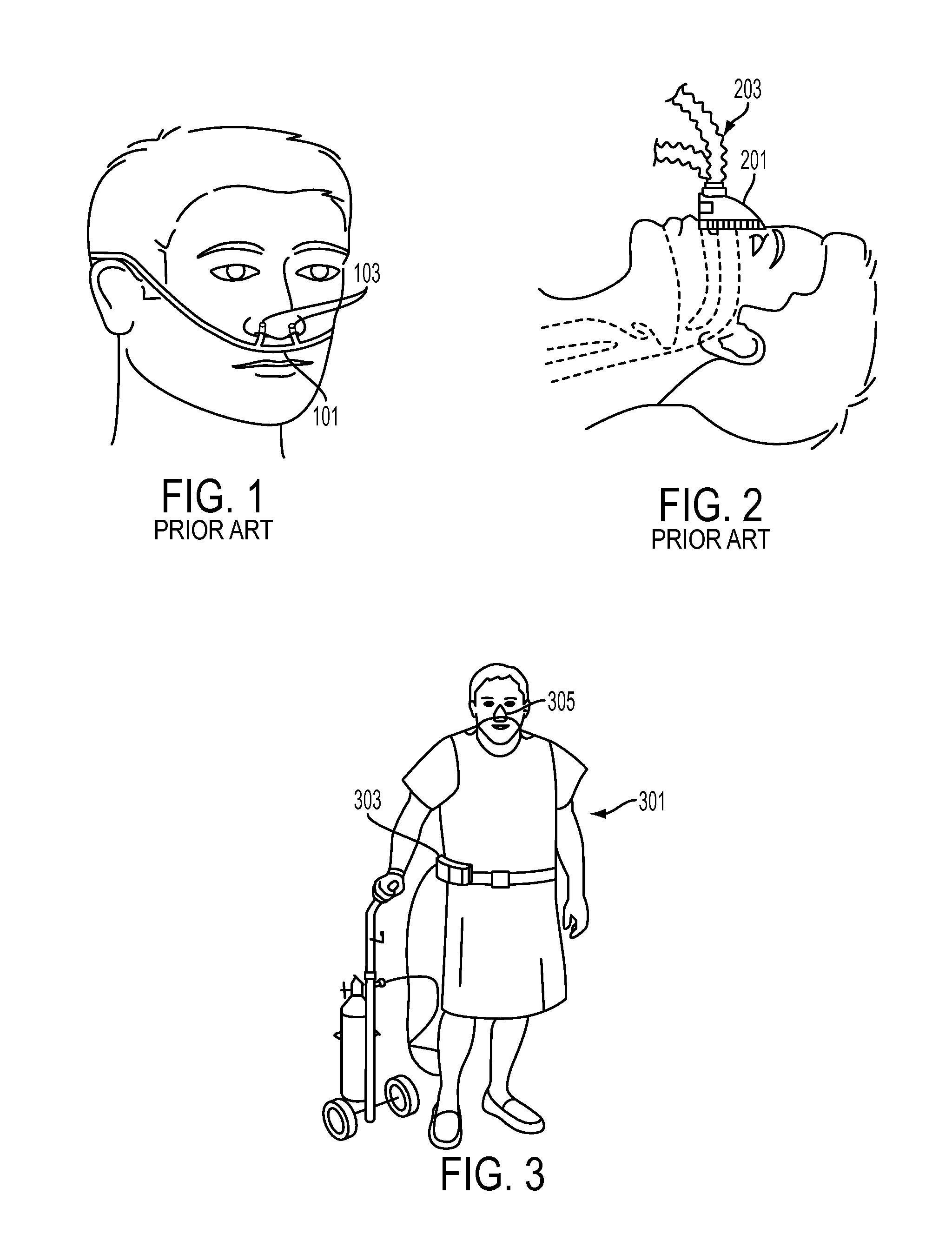
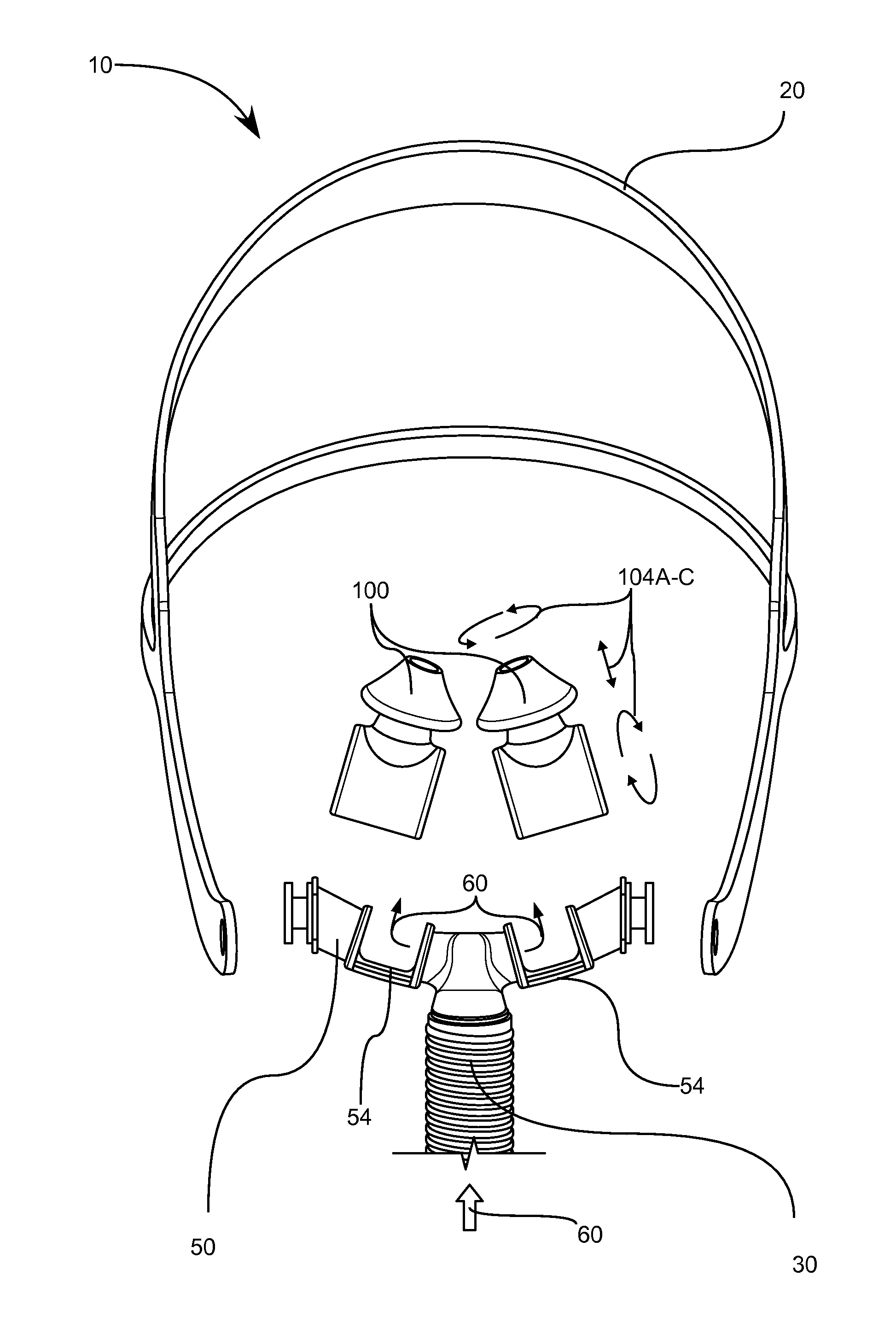
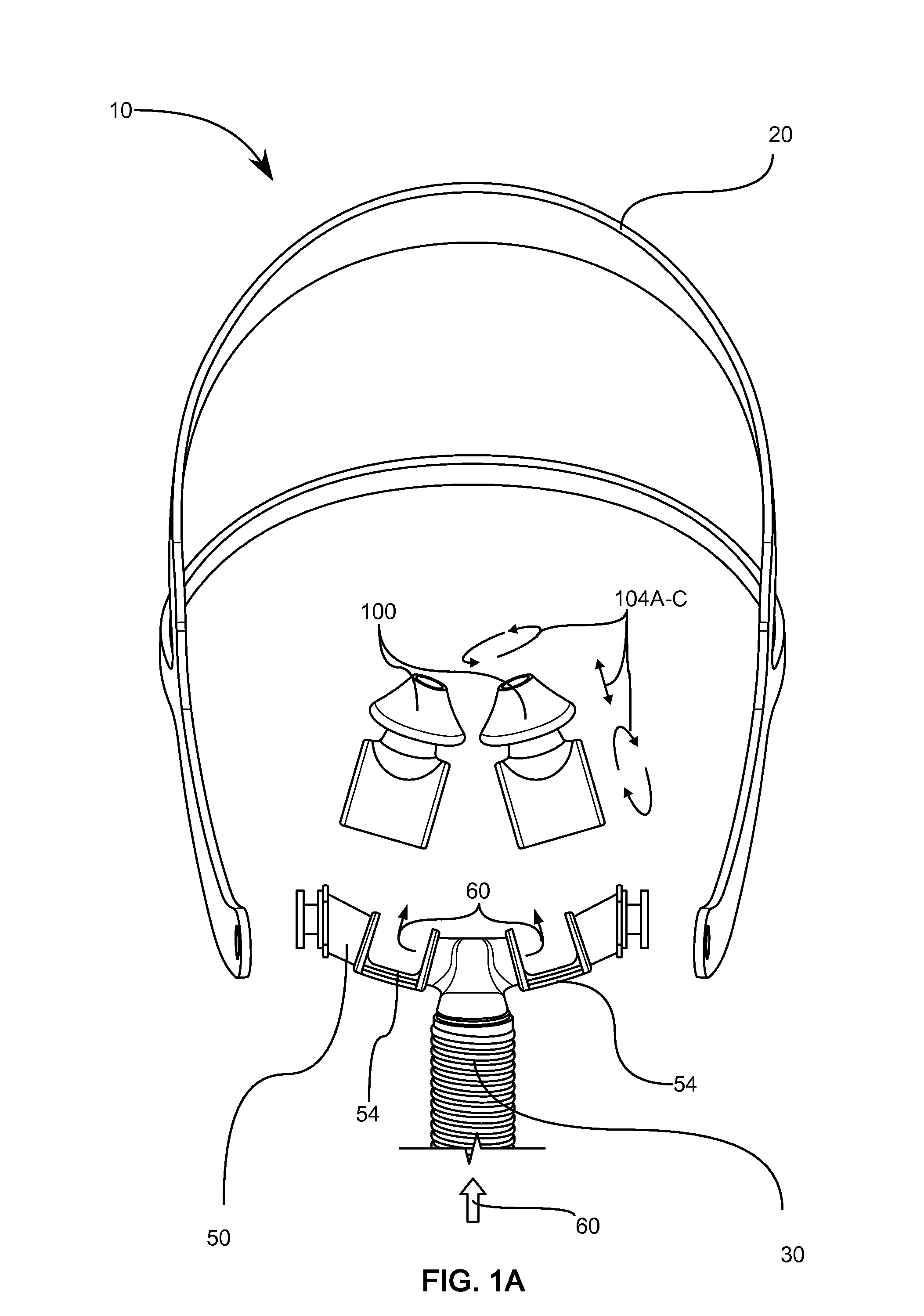
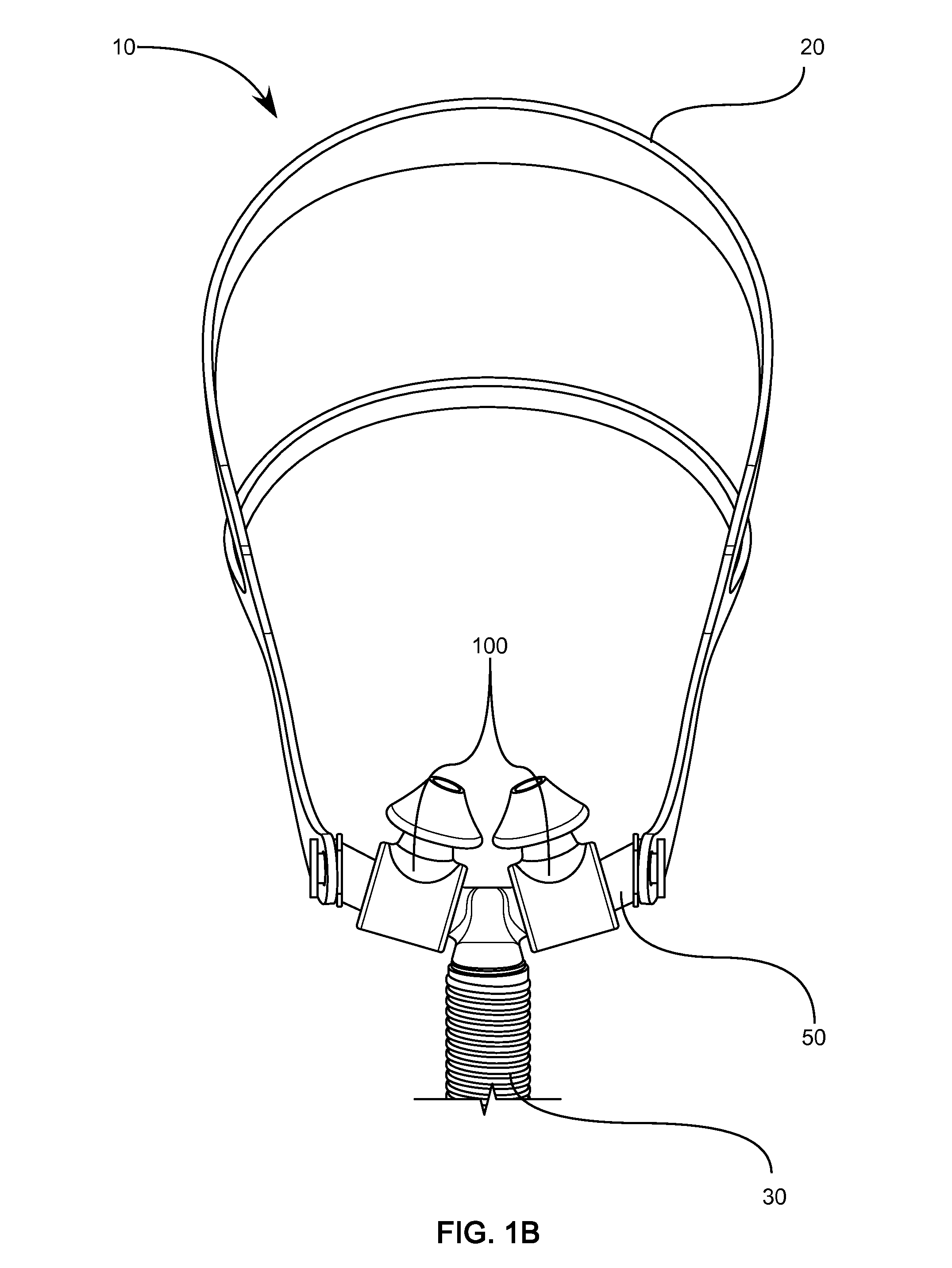
Methods, systems and devices for non-invasive open ventilation with gas delivery nozzles within nasal pillows
ActiveUS20100252037A1Work lessIncrease airway pressureRespiratorsOperating means/releasing devices for valvesNostrilNon invasive
A non-invasive ventilation system may include a nasal interface. The nasal interface may include a left outer tube with a left distal end adapted to impinge a left nostril, at least one left opening in the left distal end in pneumatic communication with the left nostril, and a left proximal end of the left outer tube in fluid communication with ambient air. The left proximal end of the left outer tube may curve laterally away from a midline of a face. A right outer tube may be similarly provided. One or more left jet nozzles may direct ventilation gas into the left outer tube, and one or more right jet nozzles may direct ventilation gas into the right outer tube. The jet nozzles may be in fluid communication with the pressurized gas supply.
Owner:BREATHE TECHNOLOGIES INC
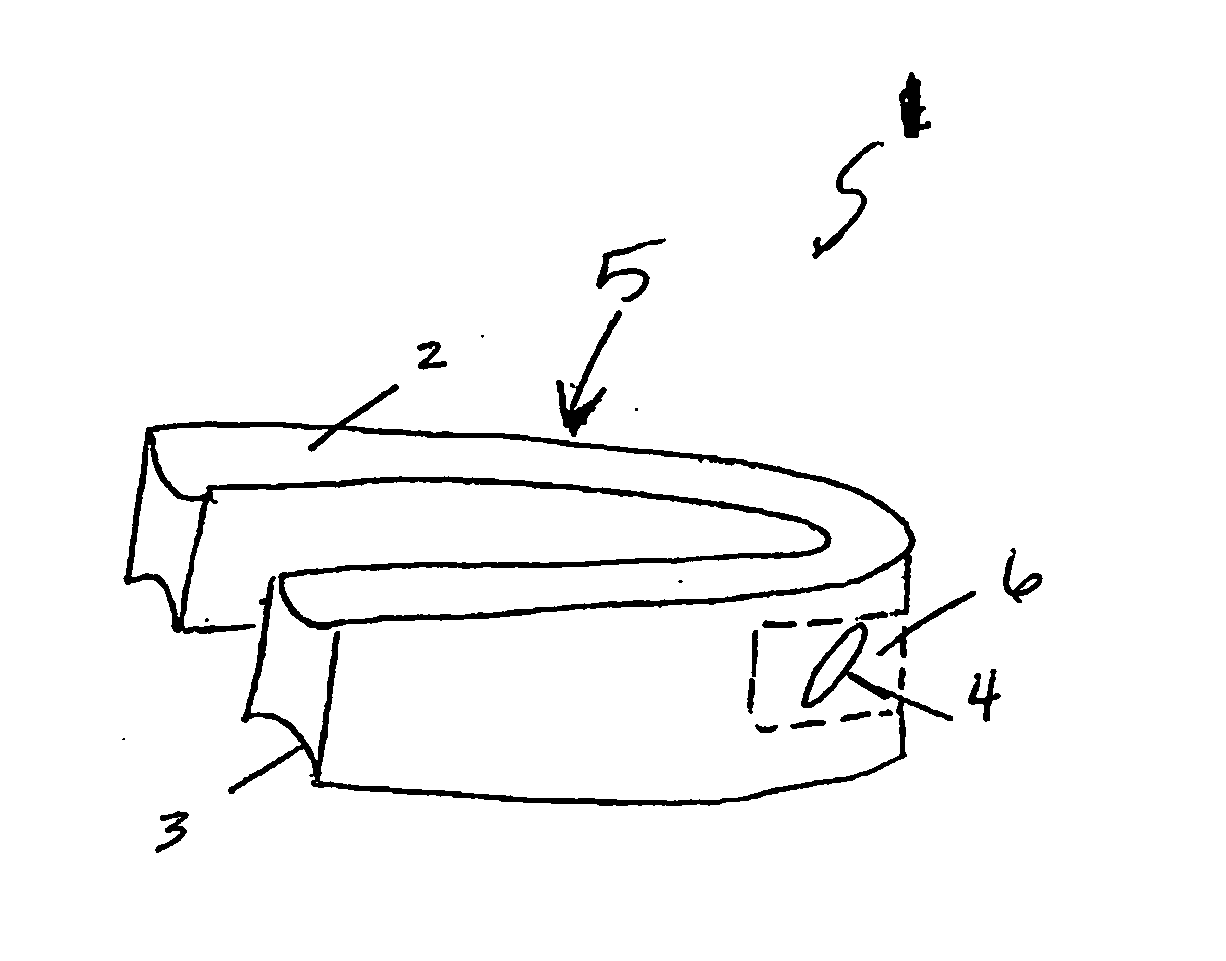
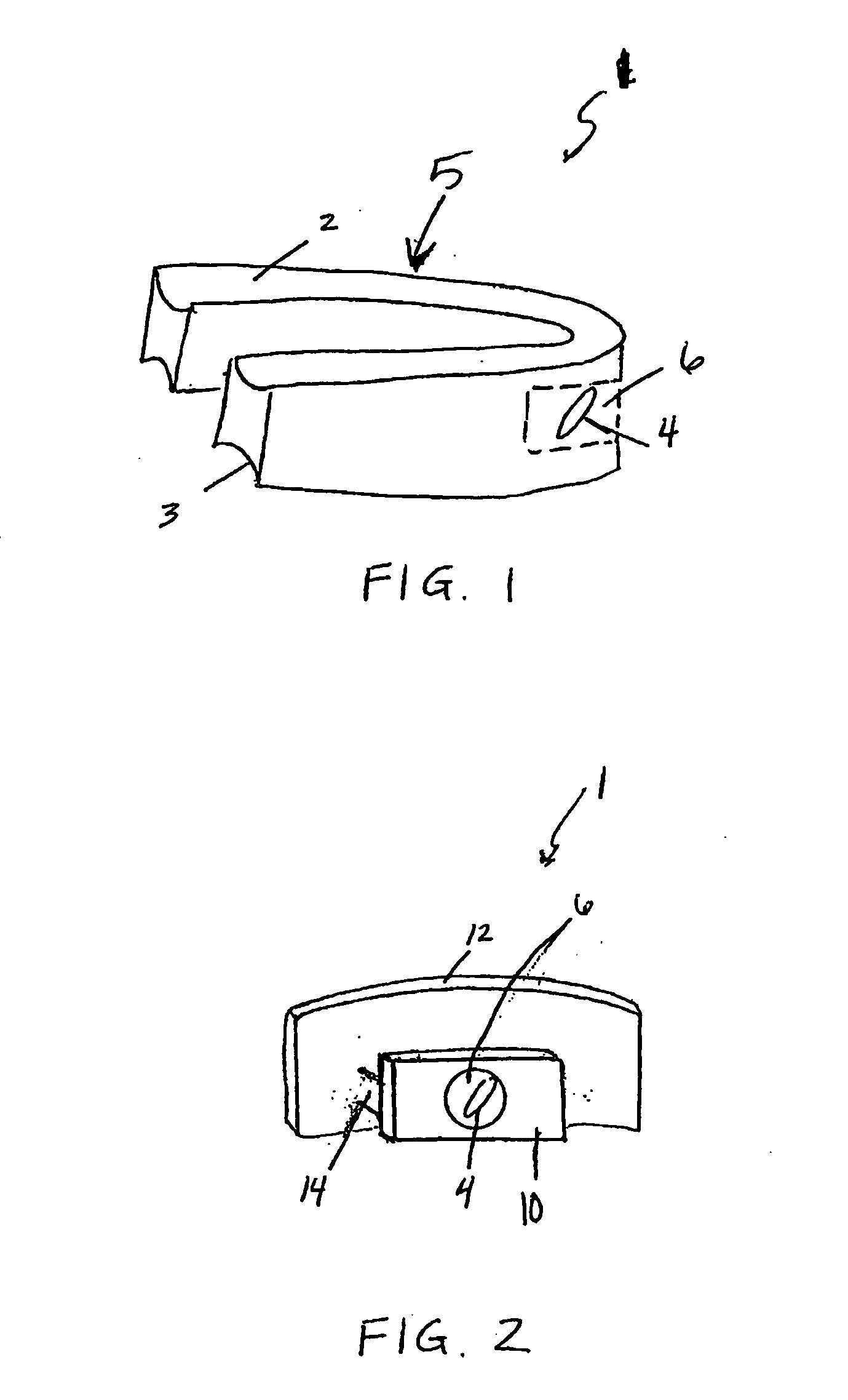
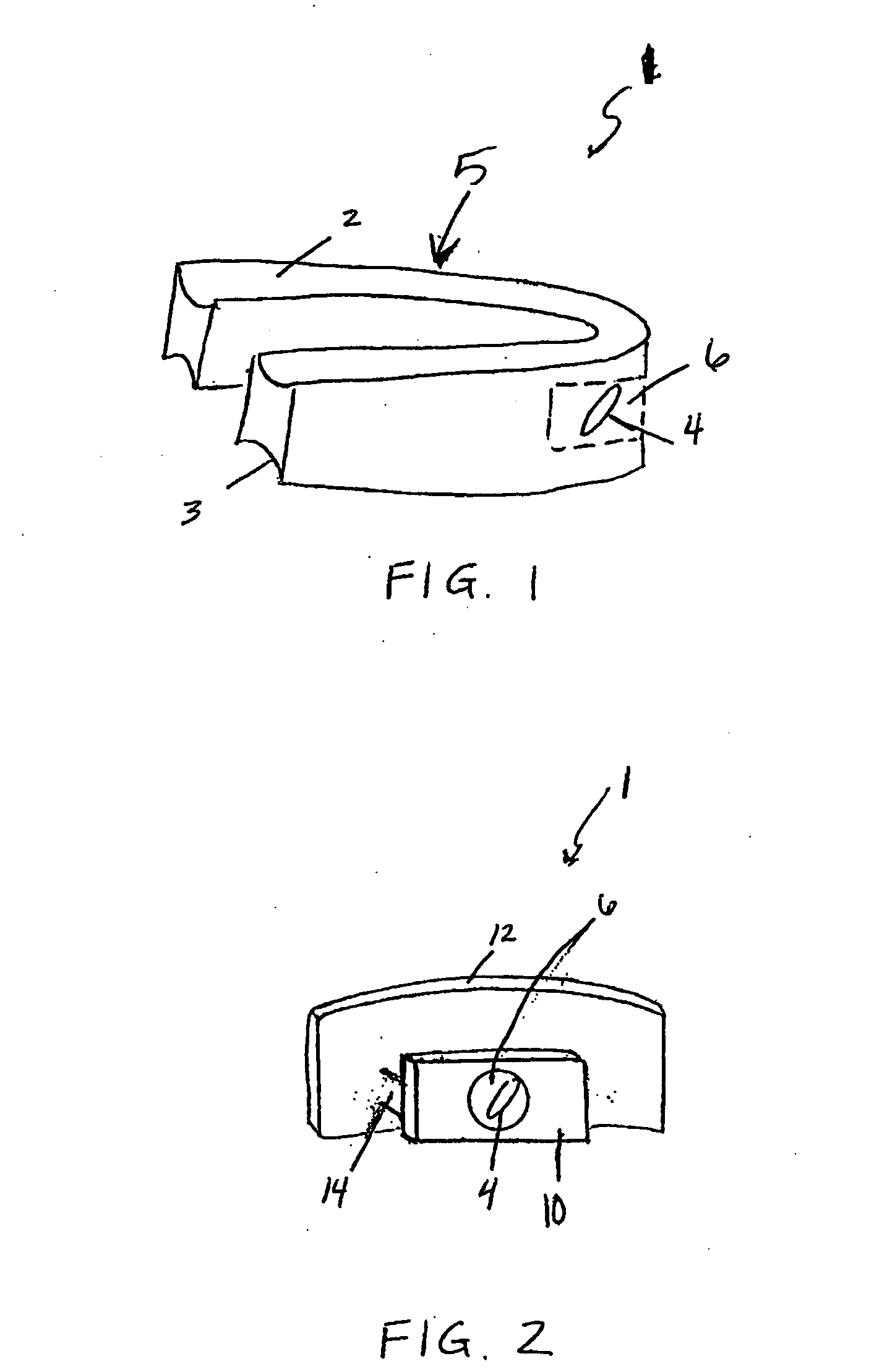
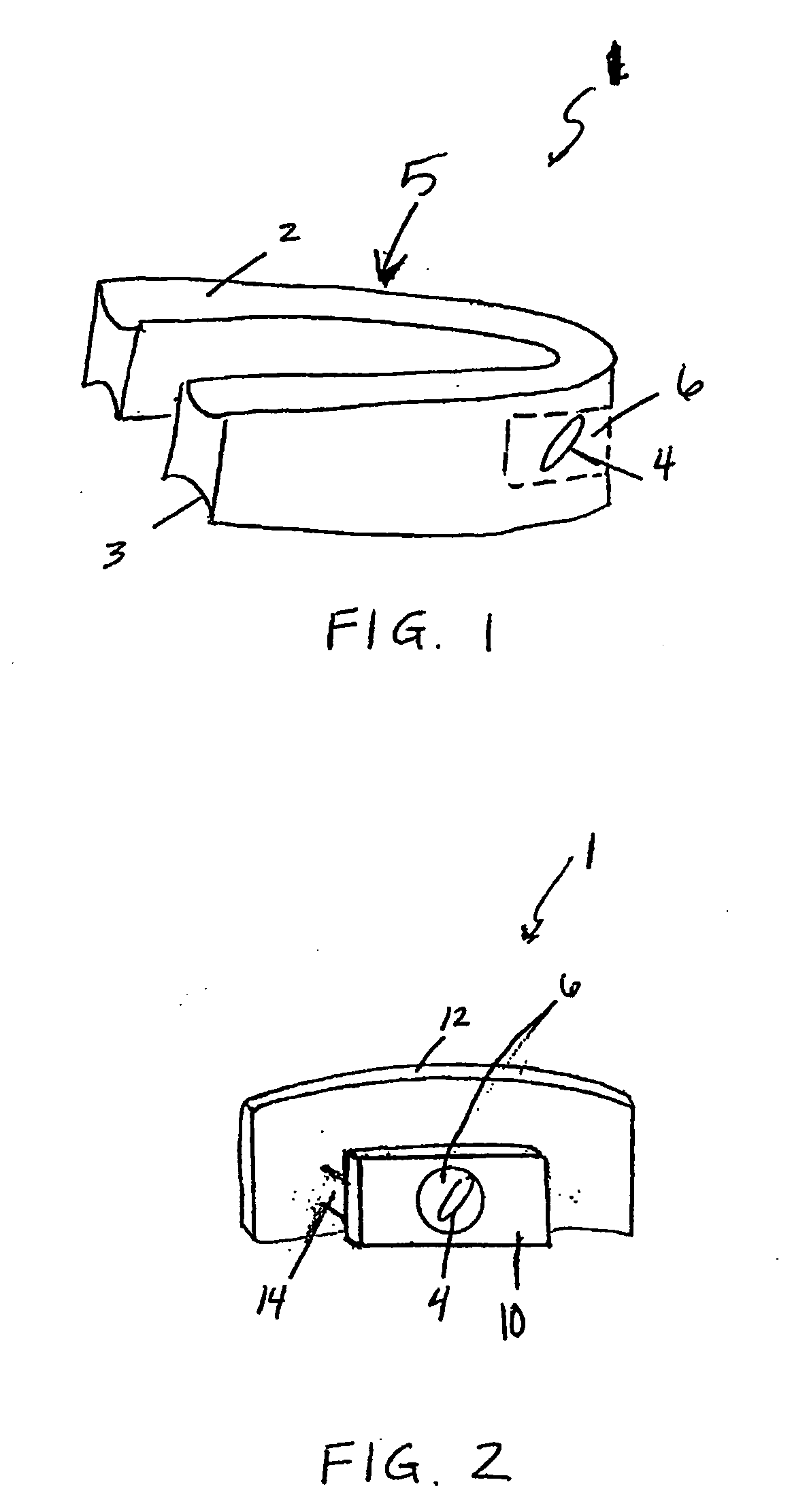
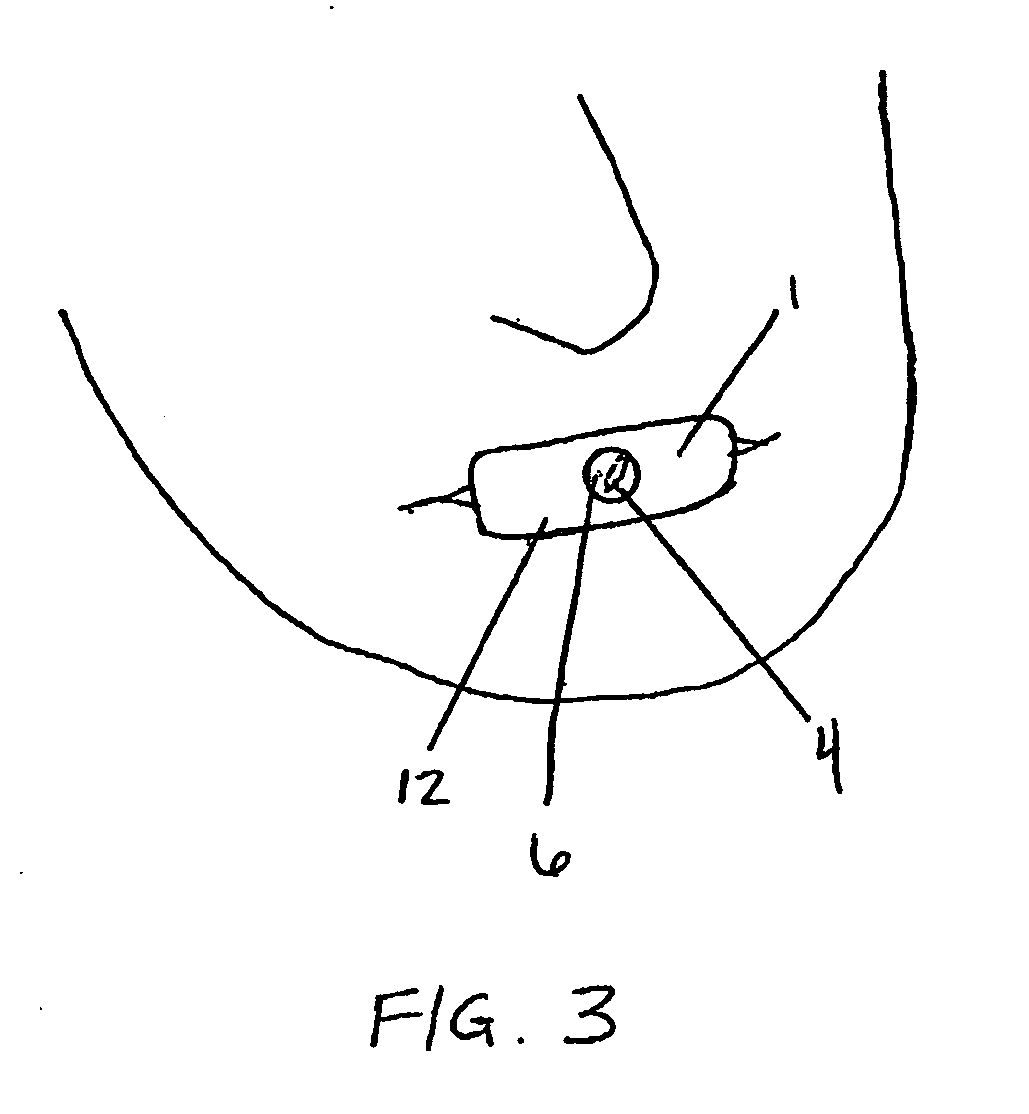
Respiratory devices
InactiveUS20060144398A1Avoid inhalationAvoid expirationOperating means/releasing devices for valvesBreathing filtersNostrilMedical disorder
Described here are devices for altering the flow of air in a respiratory cavity such as the mouth and nostrils of the nose. These methods and devices may be useful for affecting a physiologic benefit in patients suffering from a variety of medical diseases, particularly those that may benefit from “pursed-lip” breathing and non-invasive ventilation, such as COPD, heart failure, sleep apnea, and other medical disorders. The devices are typically removable devices that may be placed over or in a respiratory cavity to increase resistance to airflow within the respiratory cavity. Resistance to expiration may be selectively increased relative to inspiration. Removable oral and removable nasal devices are described. Oral and nasal devices that filter inhaled airflow of debris and allergens are also provided. A nasal device that increases patency of the nares is also provided.
Owner:THERAVENT
Methods of treating respiratory disorders
InactiveUS20060150978A1Improve the immunityChange trafficBreathing filtersRespiratory masksMedical disorderNostril
Owner:THERAVENT
Nasal respiratory devices
InactiveUS20060150979A1Improve the immunityChange trafficBreathing filtersRespiratory masksMedical disorderNostril
Described here are methods, devices, and kits for altering the flow of air in a respiratory cavity such as the nostrils of the nose. These methods and devices may be useful for affecting a physiologic benefit in patients suffering from a variety of medical diseases, particularly those that may benefit from “pursed-lip” breathing and non-invasive ventilation, such as COPD, heart failure, sleep apnea, and other medical disorders. The devices are typically removable devices that may be placed over or in a respiratory cavity to increase resistance to airflow within the respiratory cavity. Resistance to expiration may be selectively increased relative to inspiration. Removable nasal devices are described.
Owner:THERAVENT
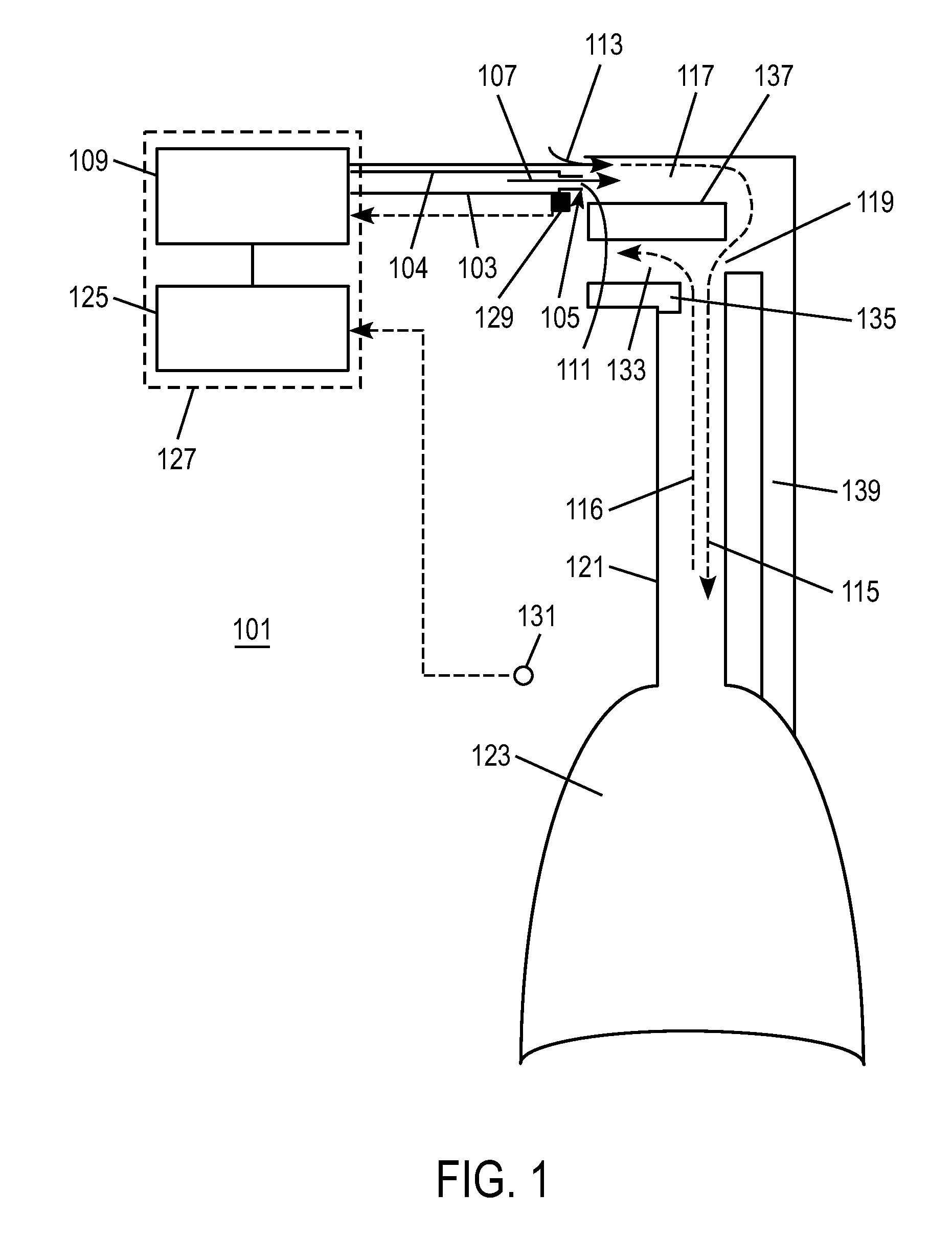
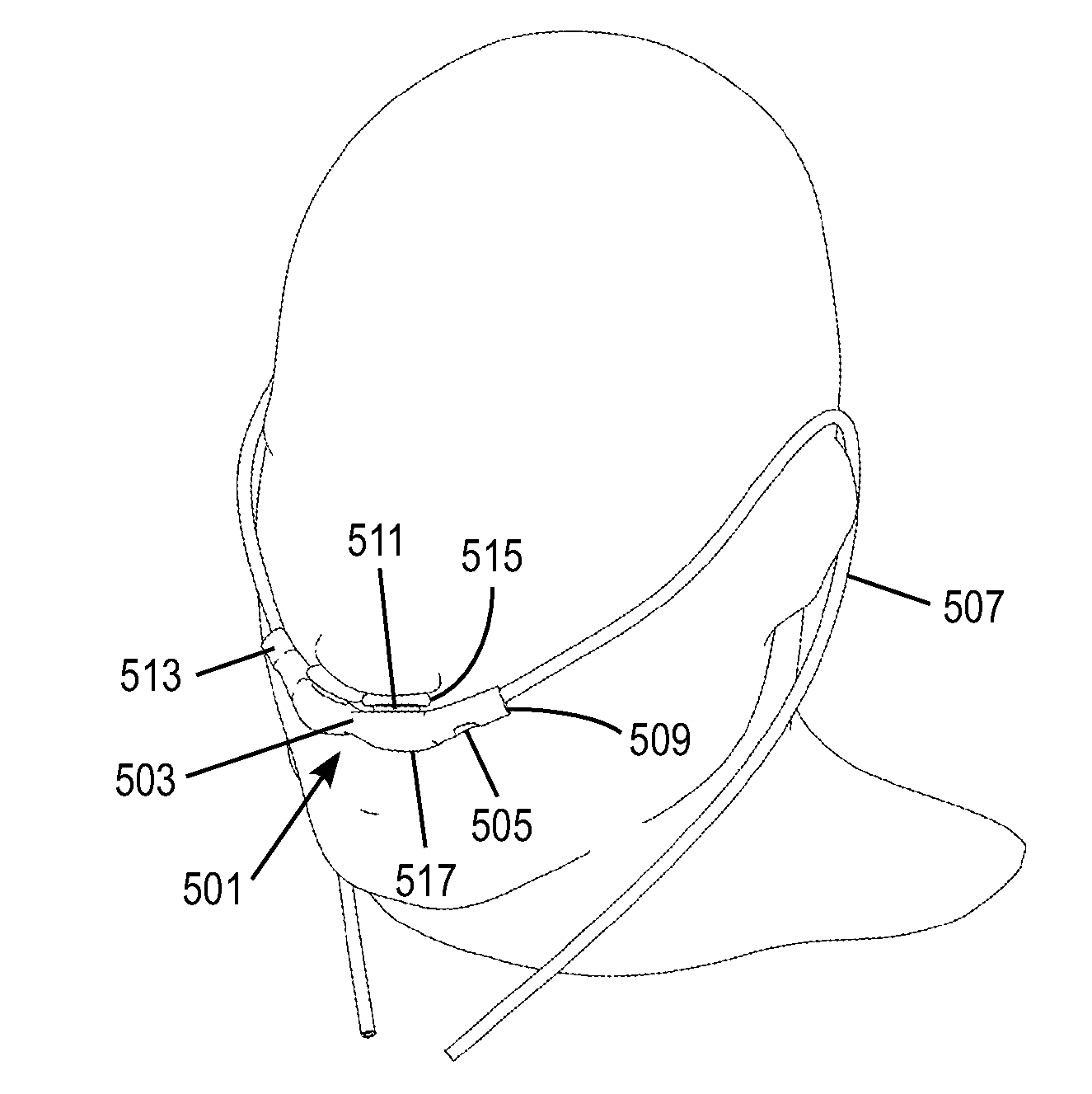
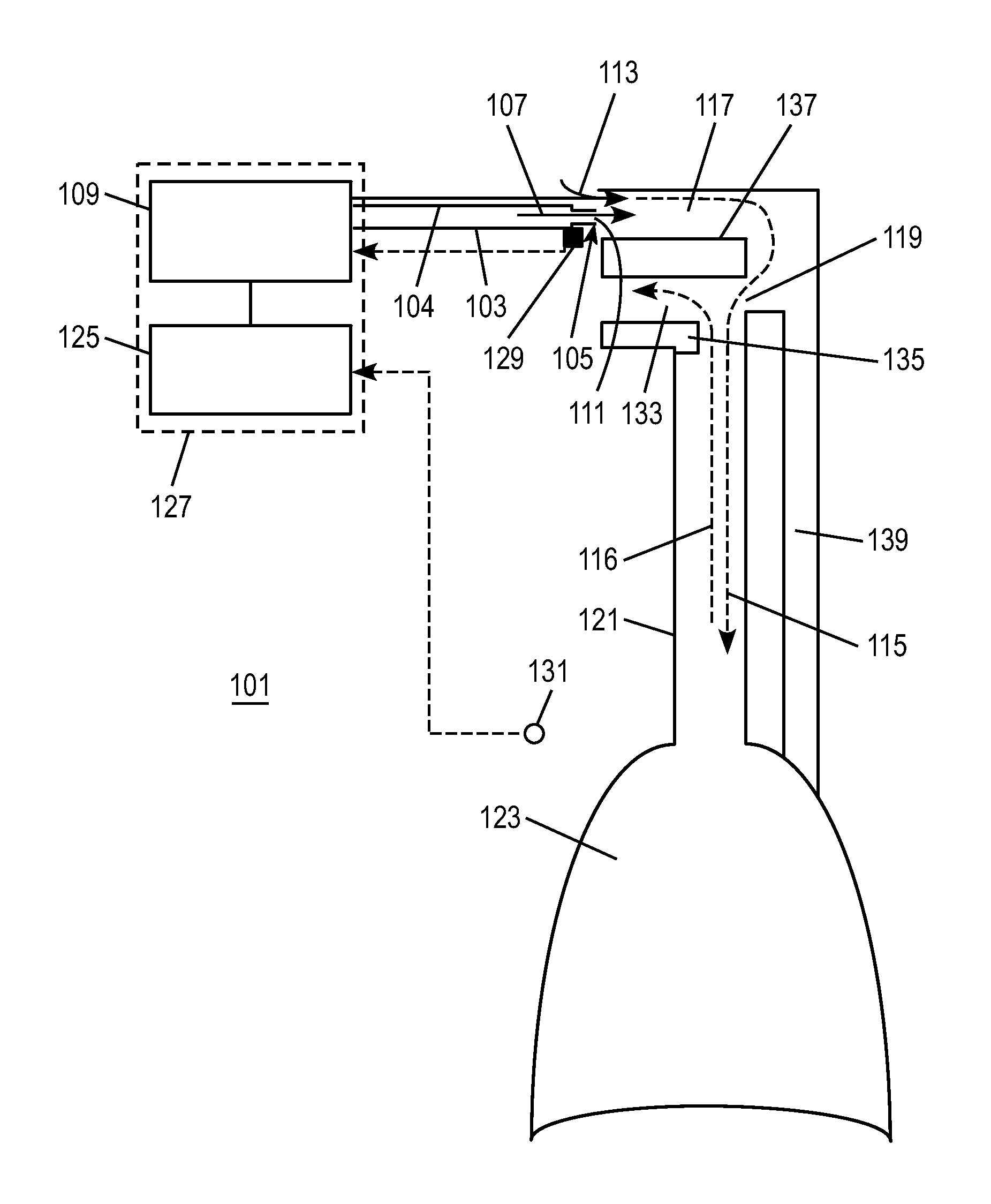
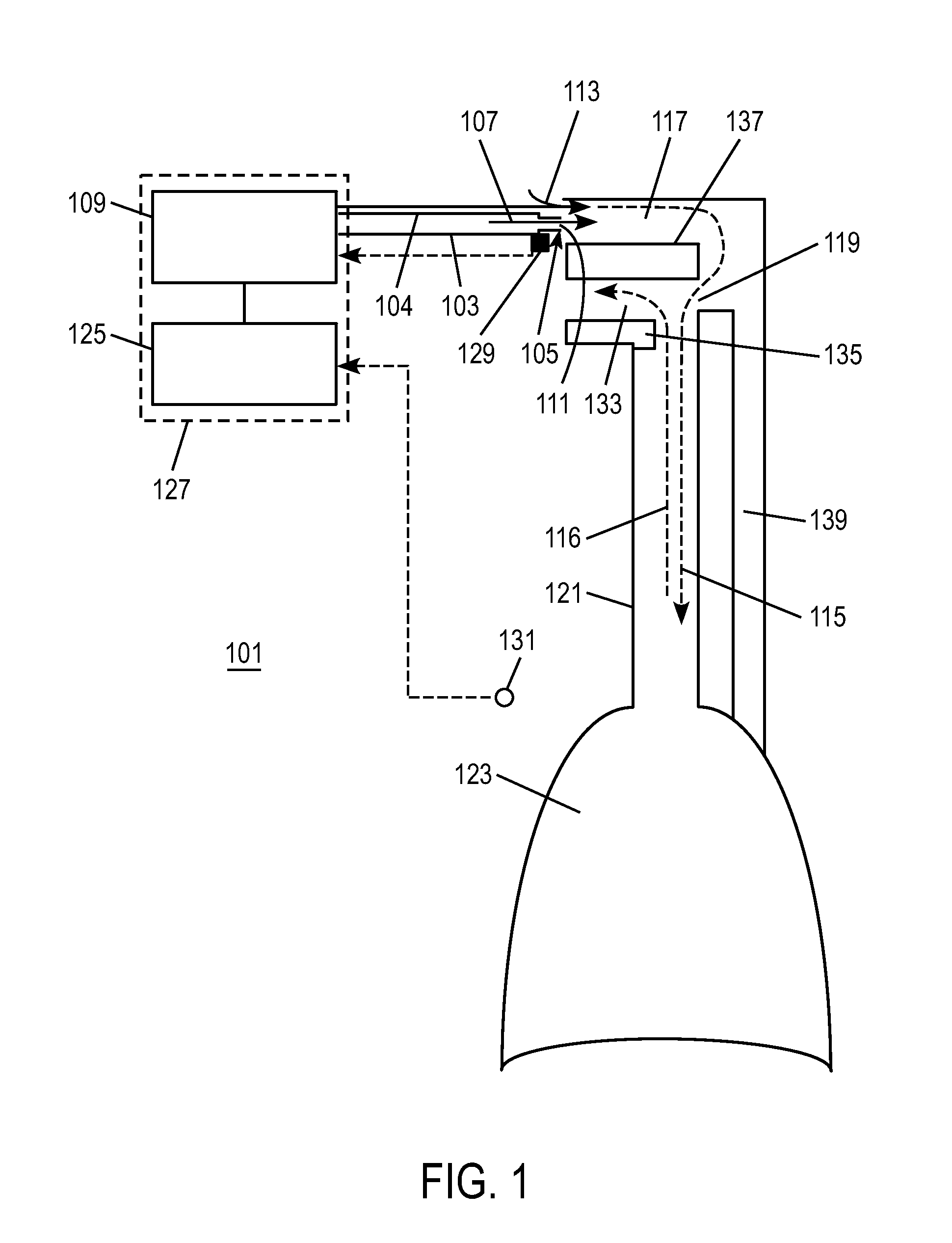
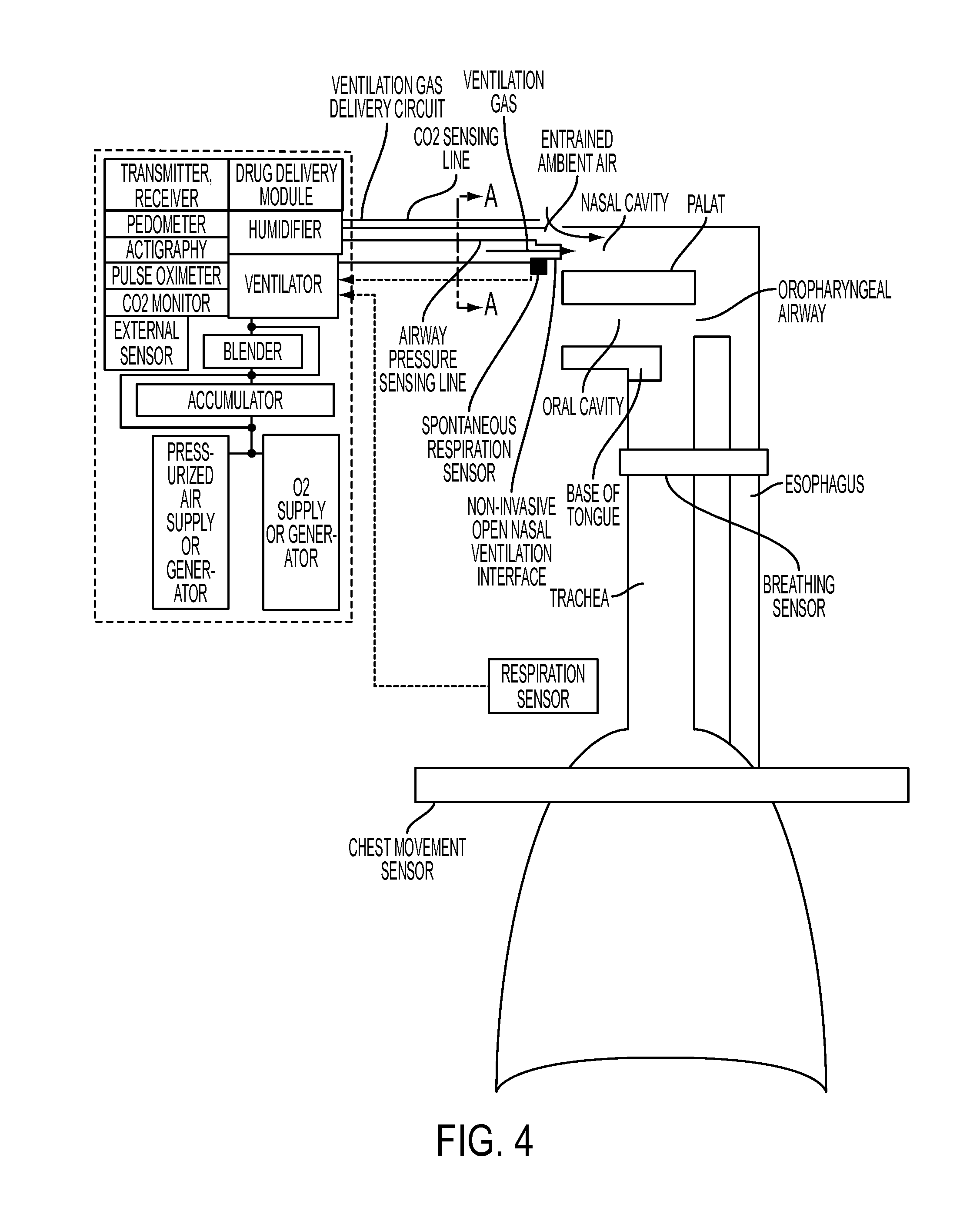
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
ActiveUS20110214676A1Avoid airway obstructionRespiratorsMedical devicesGas delivery sourceAirway pressures
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with a free space nozzle feature
A system for supplying ventilatory support may include a nasal interface configured to communicate with a patient's nose while allowing the patient to breathe ambient air directly without flowing through the nasal interface. A nozzle may be associated with the nasal interface at a distance from a nose. The nozzle may be connectable to the gas delivery circuit and the gas delivery source. The nozzle may be capable of delivering gas into the nasal passage by creating negative pressure area near the nozzle and a positive pressure area near the entrance to the nose. A combination of gas from the gas delivery source and air entrained from the gas exiting the nozzle may provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
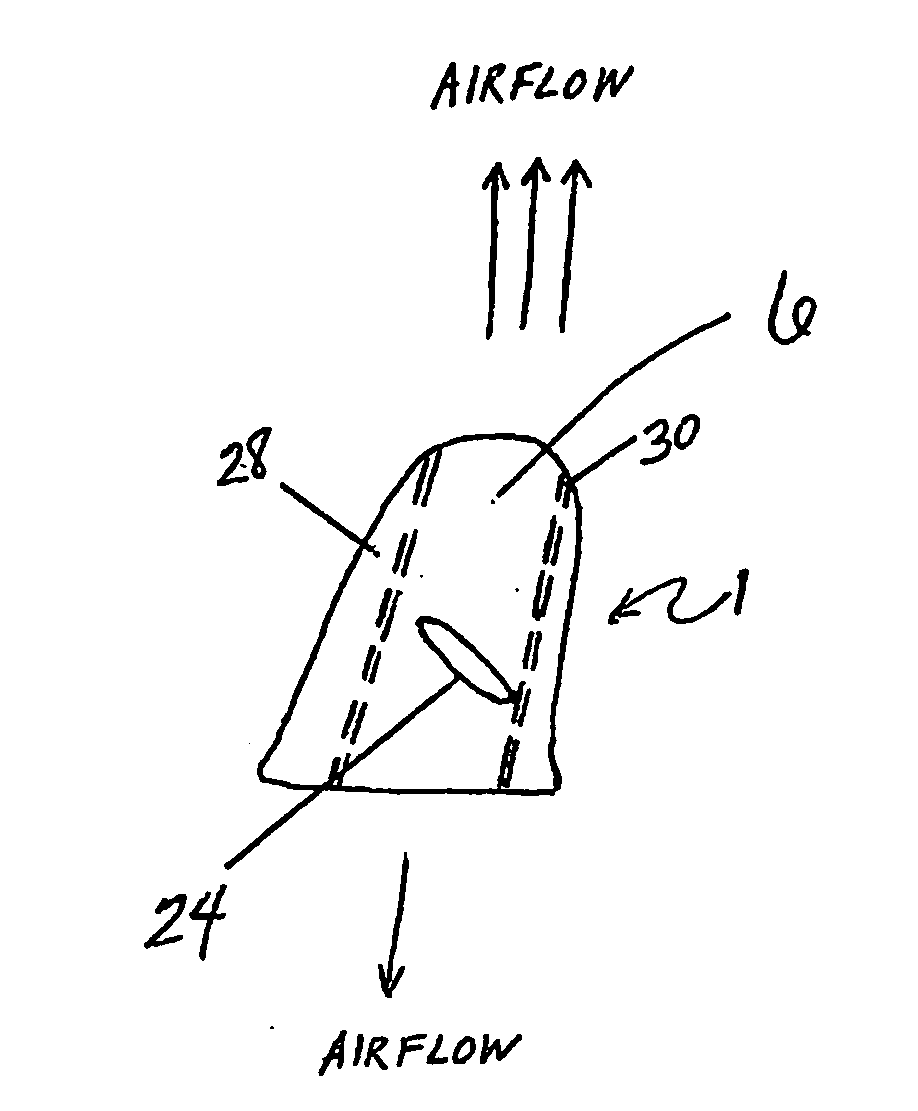
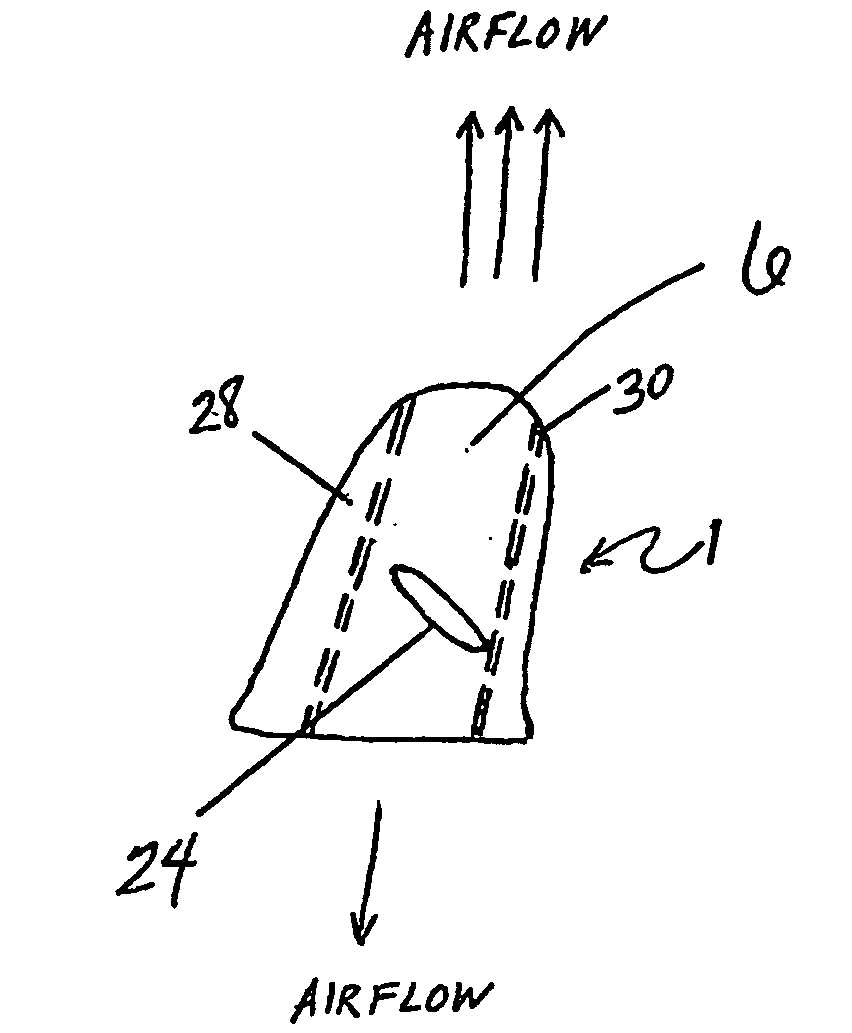
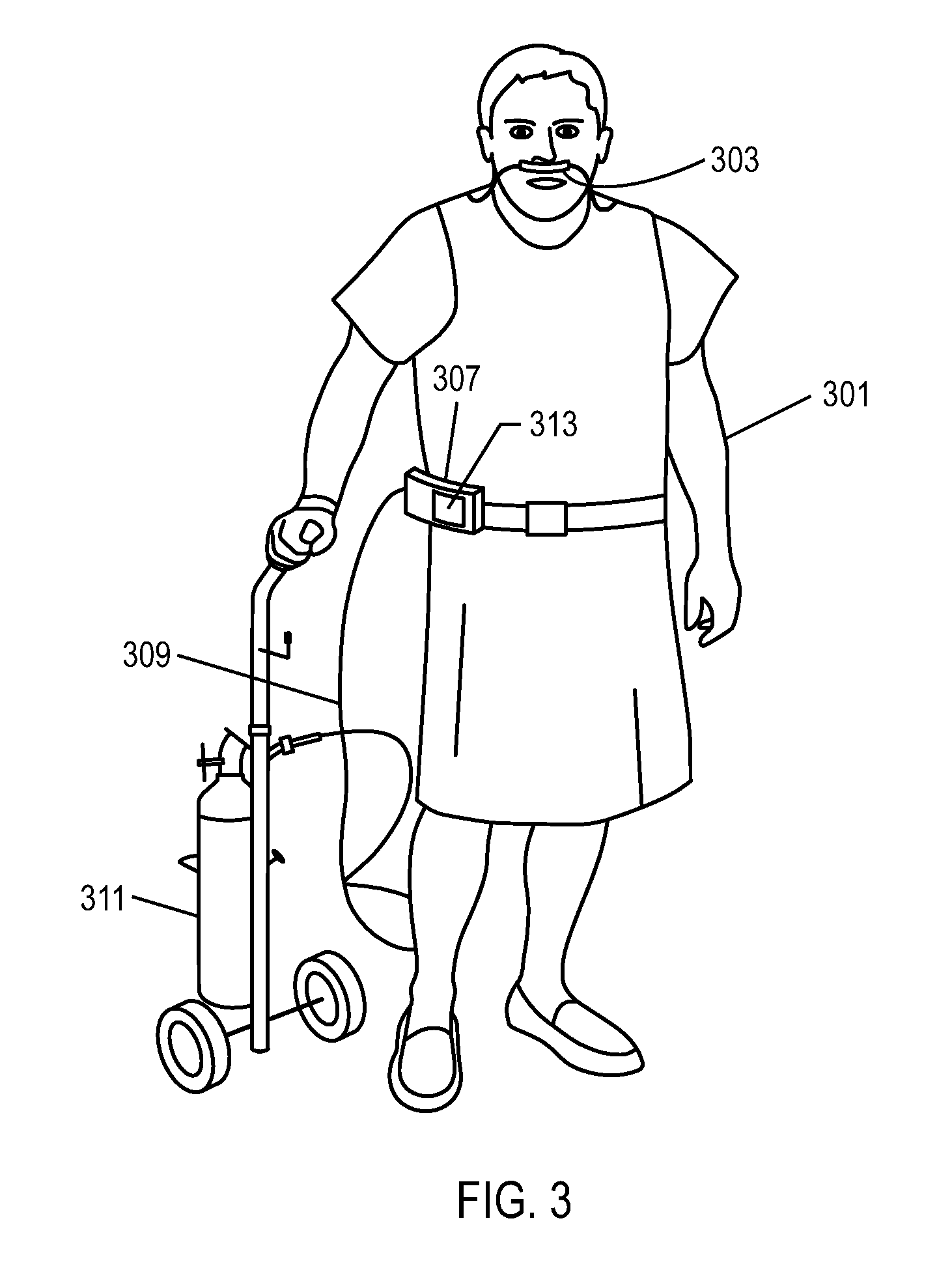
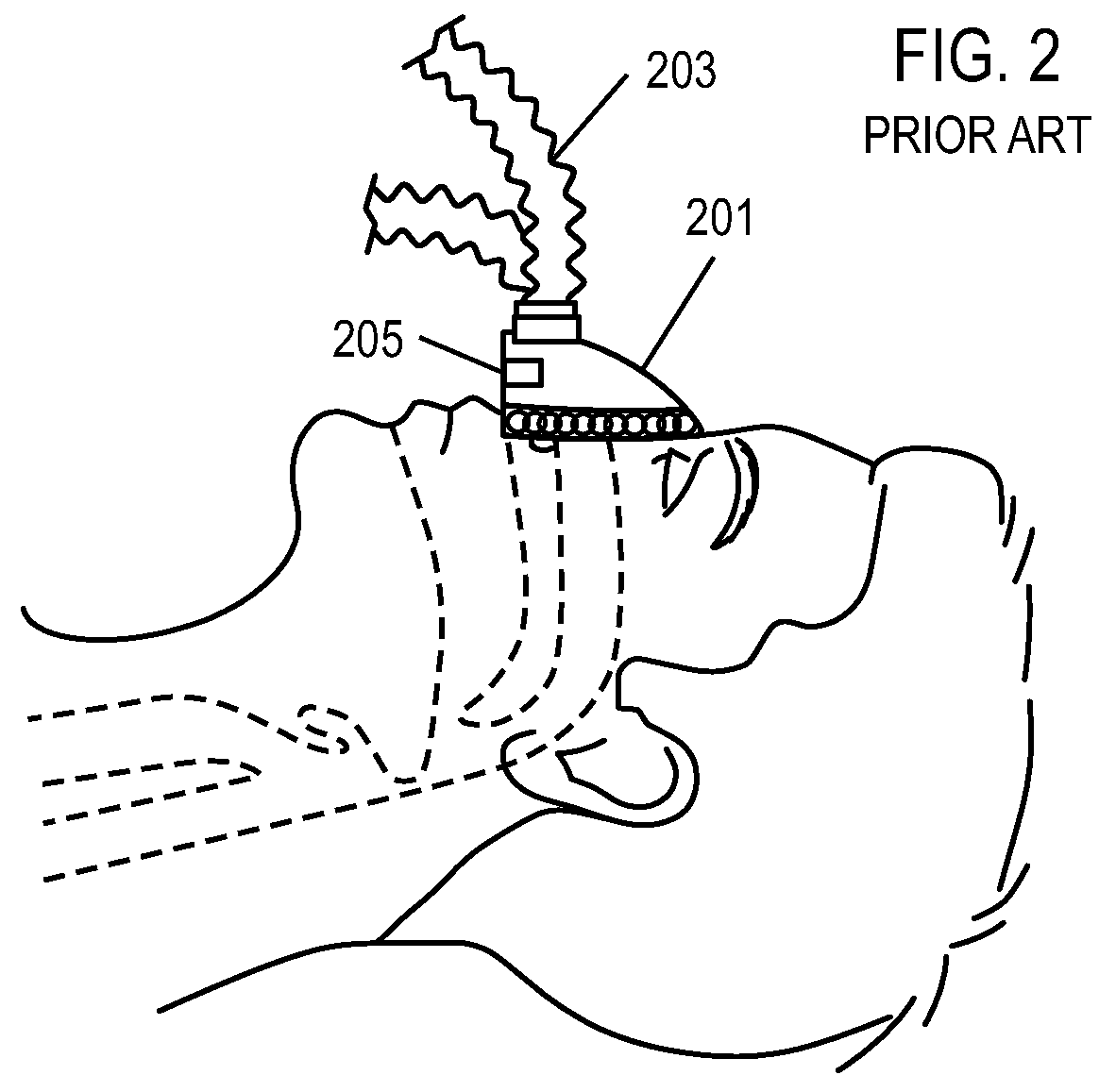
Methods, systems and devices for non-invasive open ventilation with gas delivery nozzles within an outer tube
ActiveUS20100252040A1Work lessIncrease pressureRespiratorsOperating means/releasing devices for valvesThroatEngineering
A non-invasive ventilation system may include at least one outer tube with a proximal lateral end of the outer tube adapted to extend to a side of a nose. The at least one outer tube may also include a throat section. At least one coupler may be located at a distal section of the outer tube for impinging at least one nostril and positioning the at least one outer tube relative to the at least one nostril. At least one jet nozzle may be positioned within the outer tube at the proximal lateral end and in fluid communication with a pressurized gas supply. At least one opening in the distal section may be adapted to be in fluid communication with the nostril. At least one aperture in the at least one outer tube may be in fluid communication with ambient air. The at least one aperture may be in proximity to the at least one jet nozzle.
Owner:BREATHE TECHNOLOGIES INC
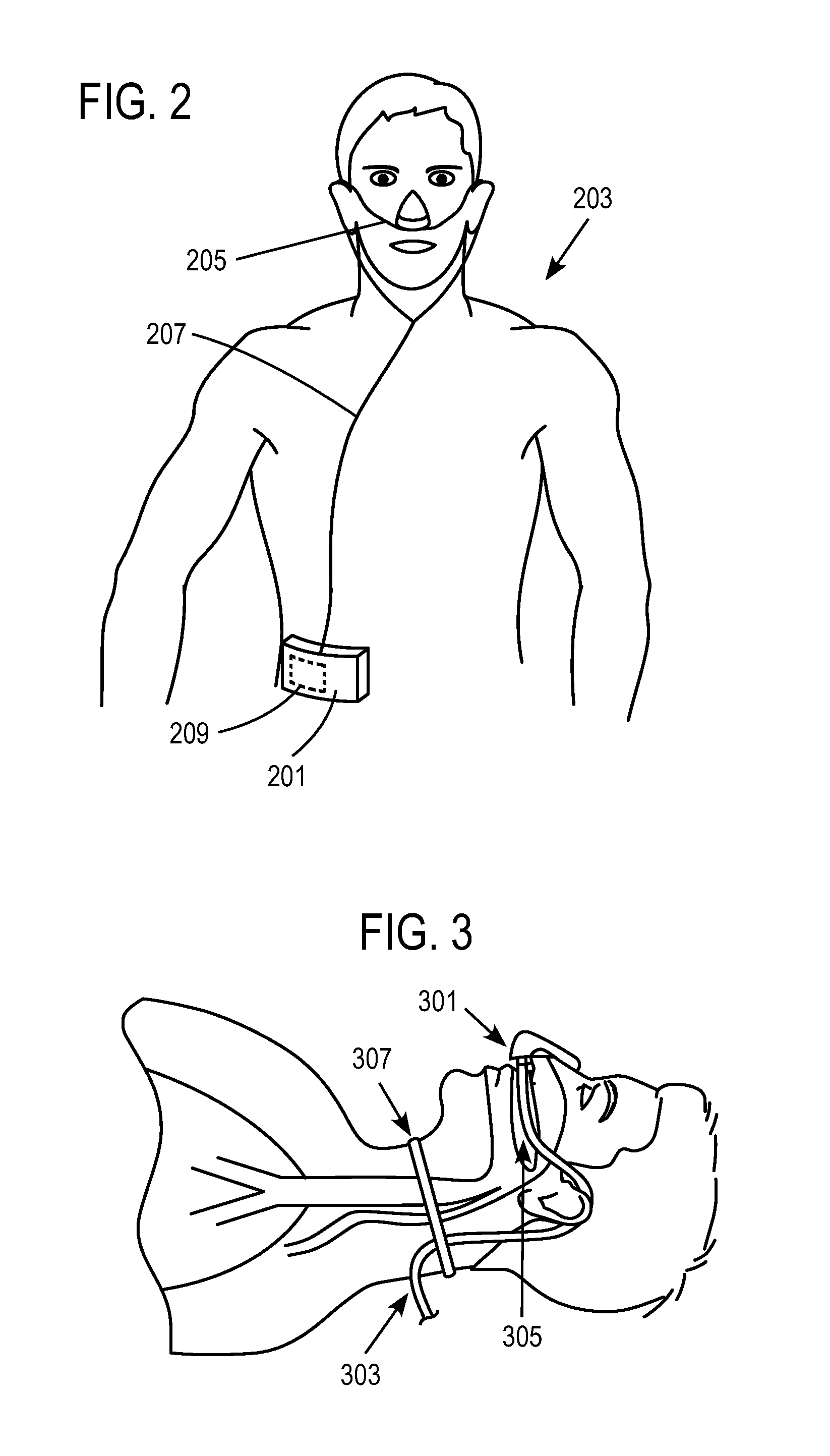
Methods, systems and devices for non-invasive open ventilation with gas delivery nozzles in free space
ActiveUS20100252039A1Work lessIncrease airway pressureRespiratorsOperating means/releasing devices for valvesNoseLung volumes
A non-invasive ventilation system may include an interface. The interface may include at least one gas delivery jet nozzle adapted to be positioned in free space and aligned to directly deliver ventilation gas into an entrance of a nose. The at least one gas delivery jet nozzle may be connected to a pressurized gas supply. The ventilation gas may entrain ambient air to elevate lung pressure, elevate lung volume, decrease the work of breathing or increase airway pressure, and wherein the ventilation gas is delivered in synchrony with phases of breathing. A support for the at least one gas delivery jet nozzle may be provided. A breath sensor may be in close proximity to the entrance of the nose. A patient may spontaneous breathe ambient air through the nose without being impeded by the interface.
Owner:BREATHE TECHNOLOGIES INC
Positive airway pressure therapy mask humidification systems and methods
InactiveUS20120097156A1Additional potential benefitReduce condensationBreathing masksRespiratory masksPositive airway pressureBi-level positive airway pressure therapy
The present inventions provide positive airway pressure therapy apparatus to humidify the pressurized air delivered to a user during various positive airway pressure therapies and corresponding methods. The positive airway pressure therapy apparatus may be configured to administer one or more positive airway pressure therapies, including: continuous positive airway pressure therapy (CPAP), bi-level positive airway pressure therapy (BPAP), auto positive airway pressure therapy (autoPAP), proportional positive airway pressure therapy (PPAP), and / or other positive airway pressure therapies.
Owner:SOMNETICS INT INC
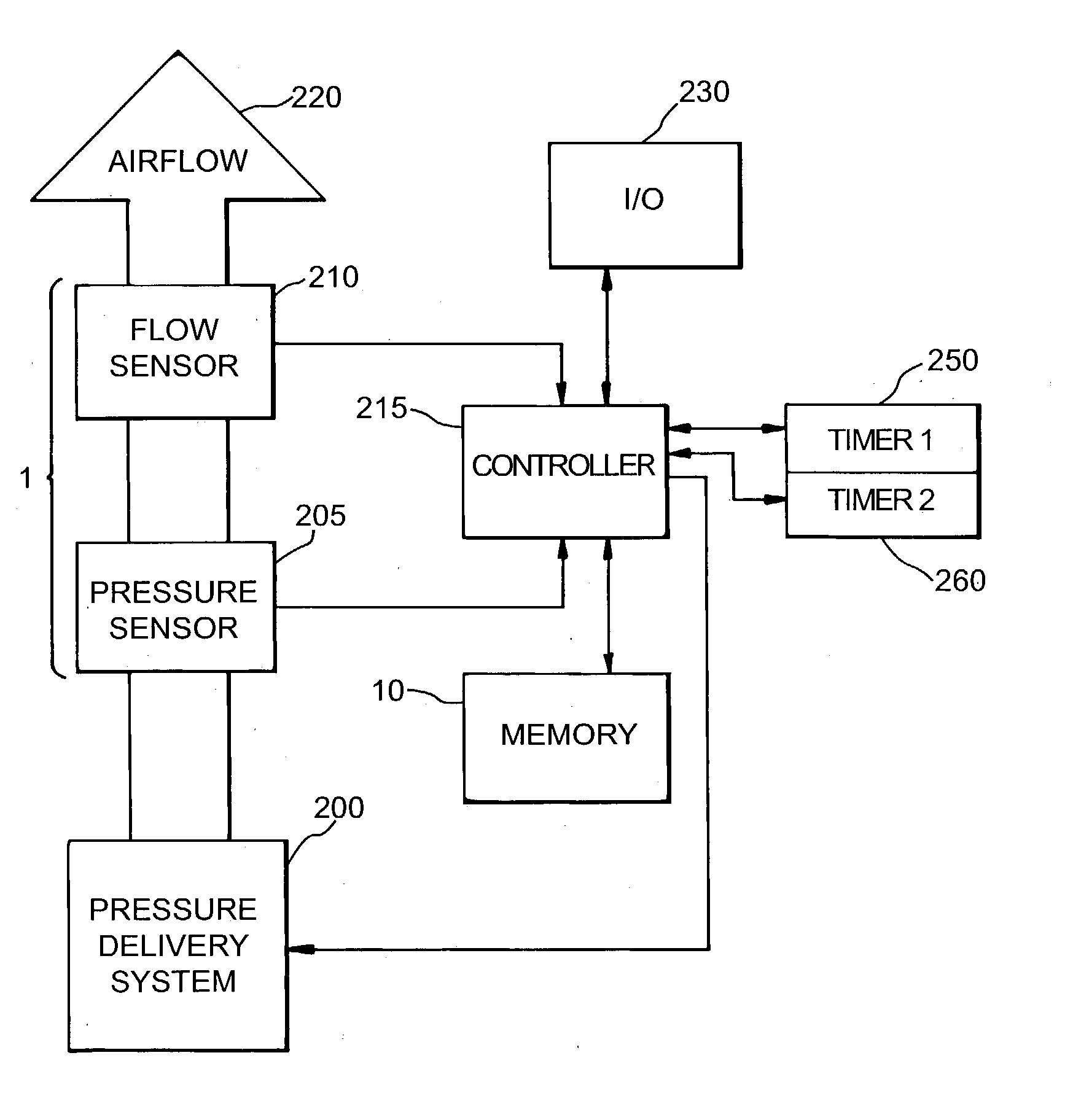
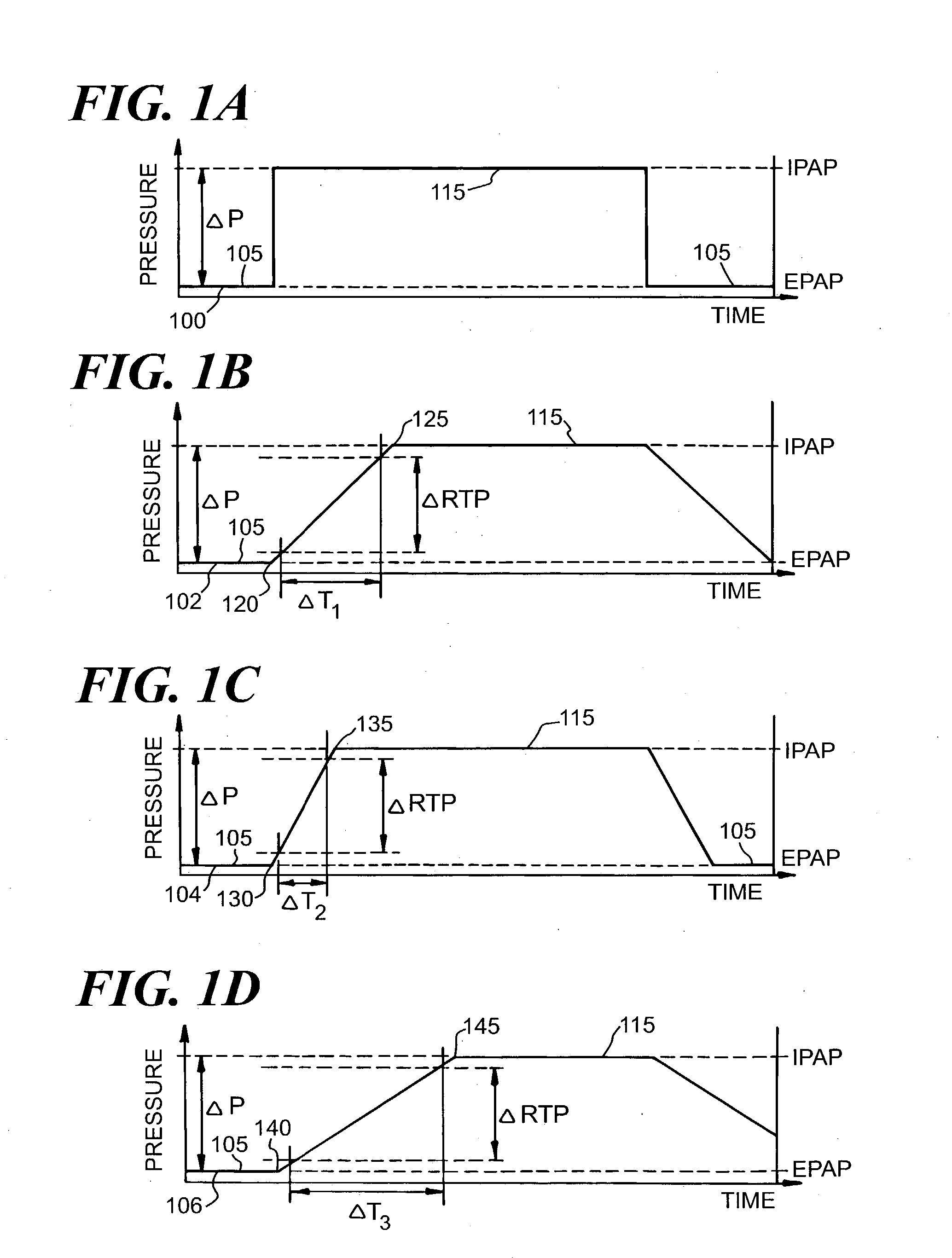
Automatic slope adjustment for bi-levelpressure support system
InactiveUS20030127097A1Operating means/releasing devices for valvesRespiratory masksSupporting systemPositive pressure
An apparatus and method for a bi-level positive airway pressure support in which the rise time from the expiratory positive airway pressure to the inspiratory positive airway pressure is automatically controlled by the pressure support system. The pressure support system includes a sensor, a control system, and a pressure generating system. The sensor monitors the patient's respiration to detect respiratory events, such as an apnea, hyponea or other disturbance, and the control system responds to the sensor information to adjust the rise time from the expiratory positive airway pressure to the inspiratory positive airway pressure gas pressure to maximize patient comfort and pressure support treatment effectiveness.
Owner:RIC INVESTMENTS LLC
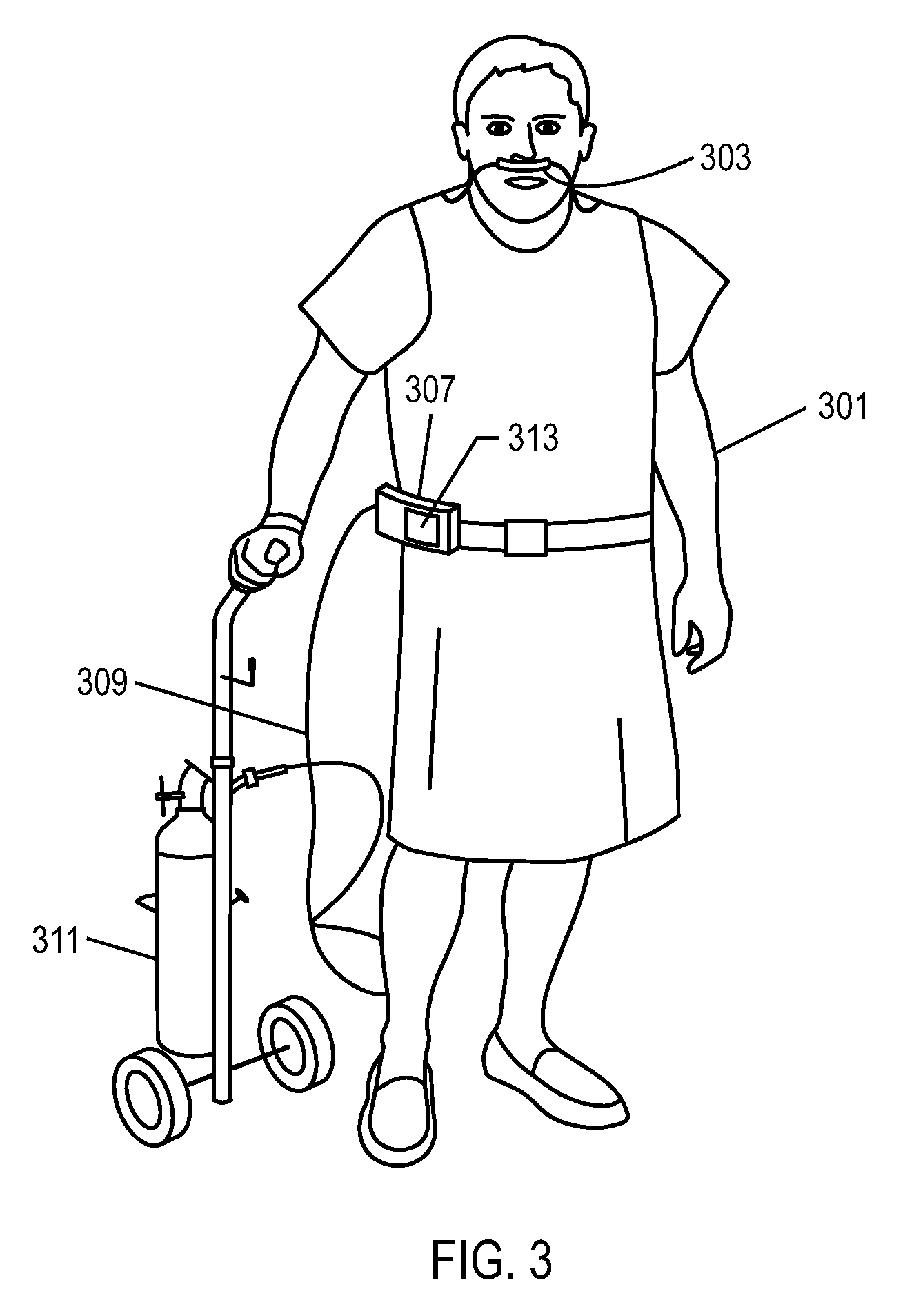
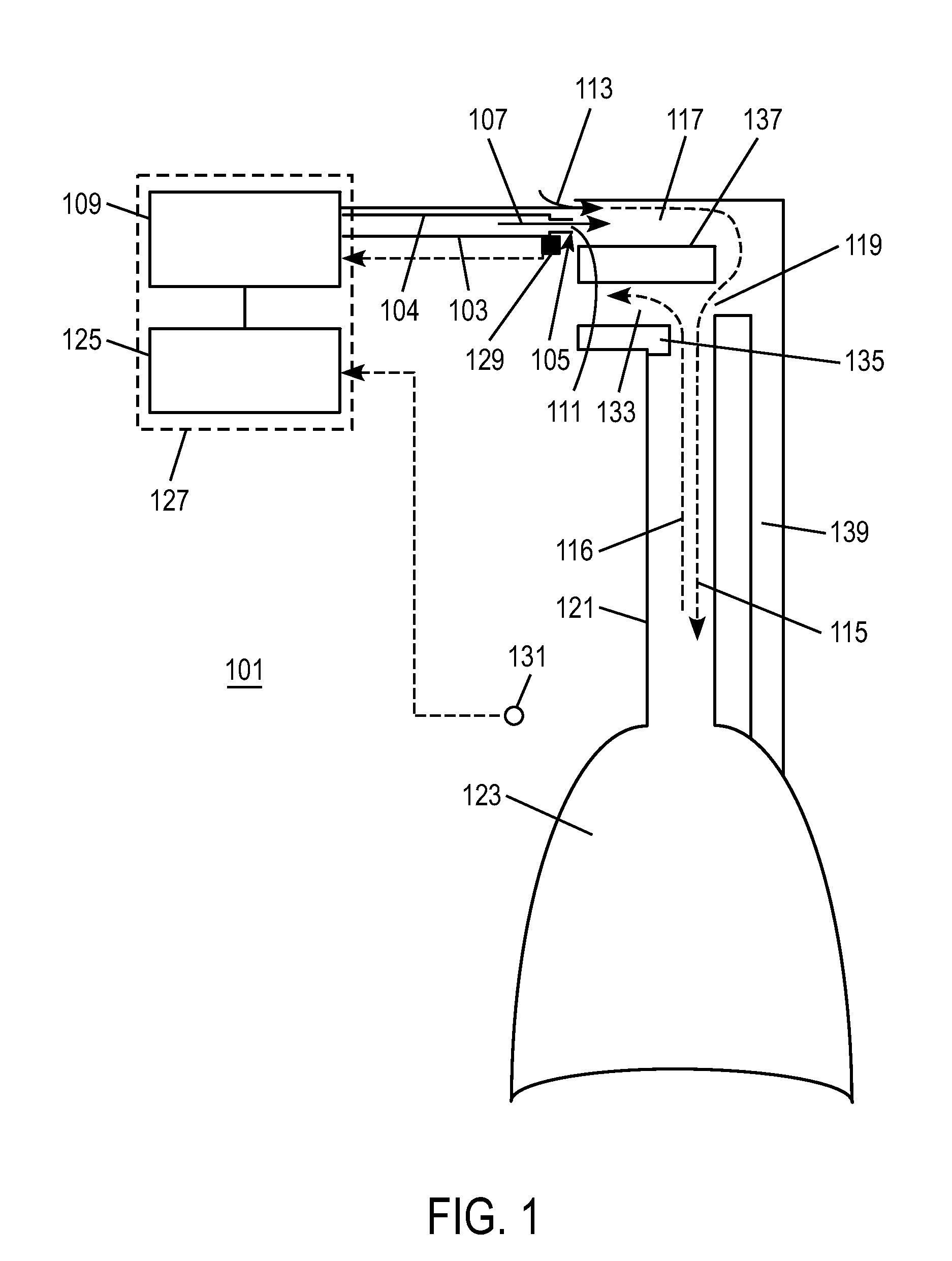
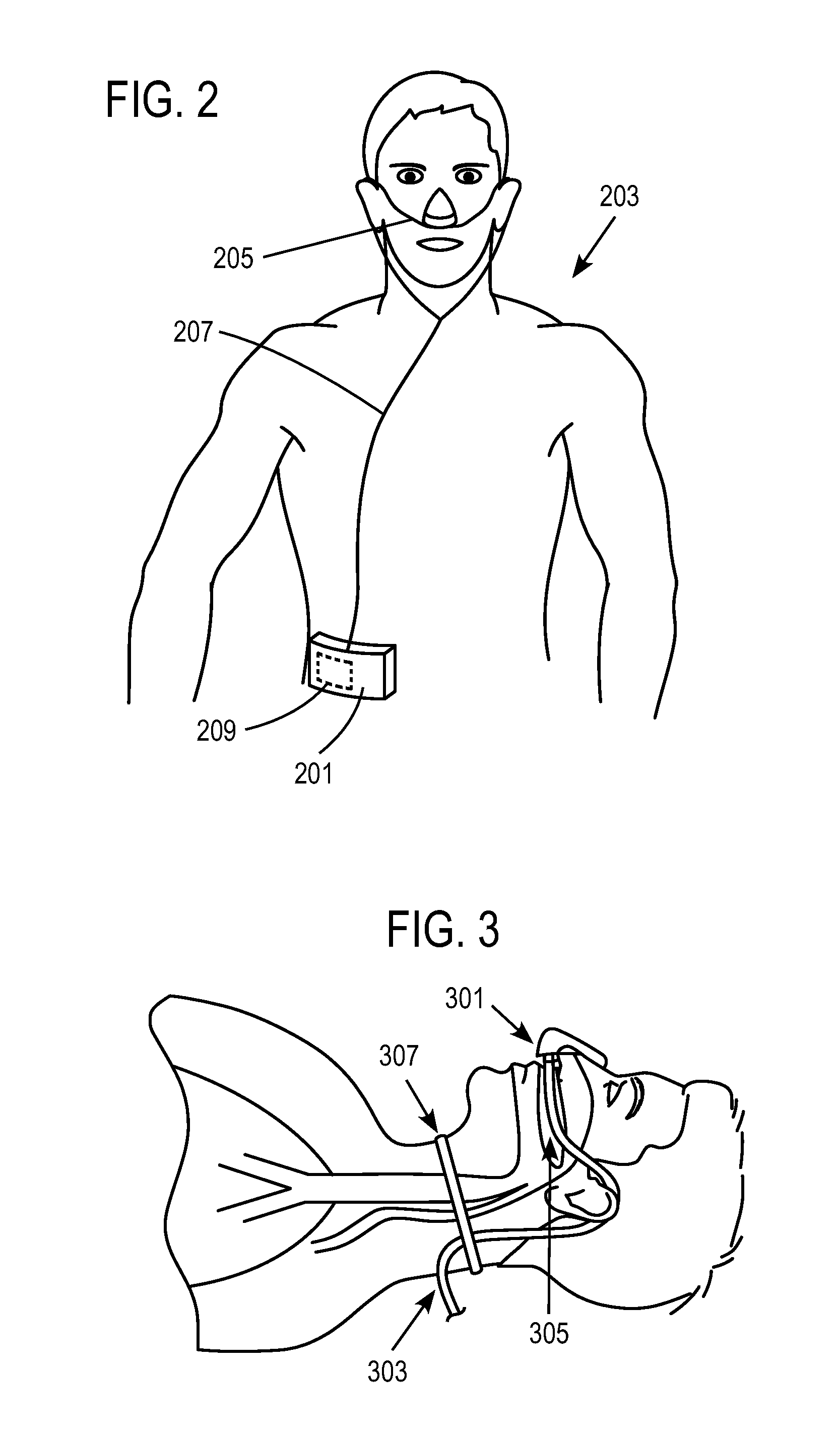
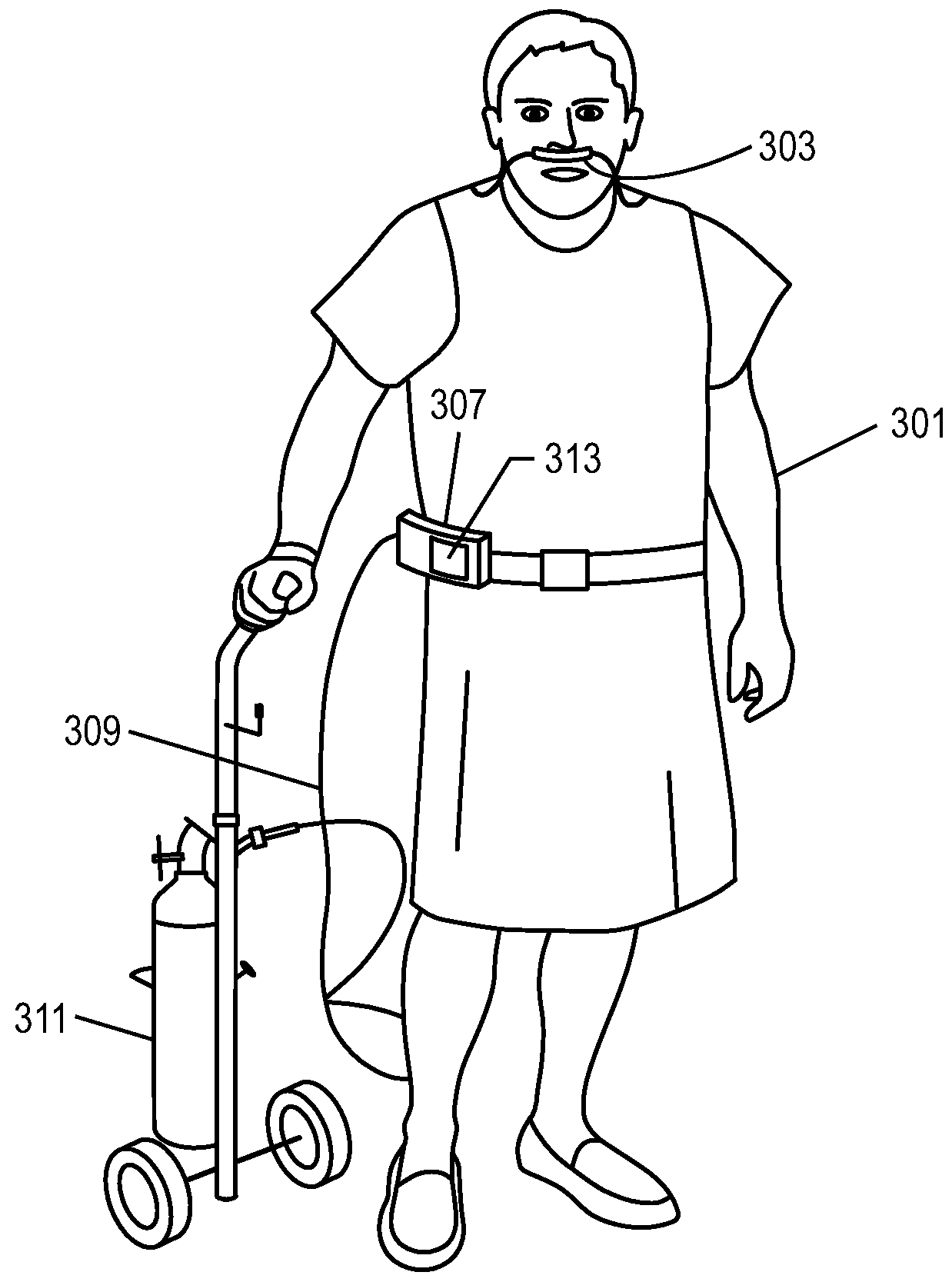
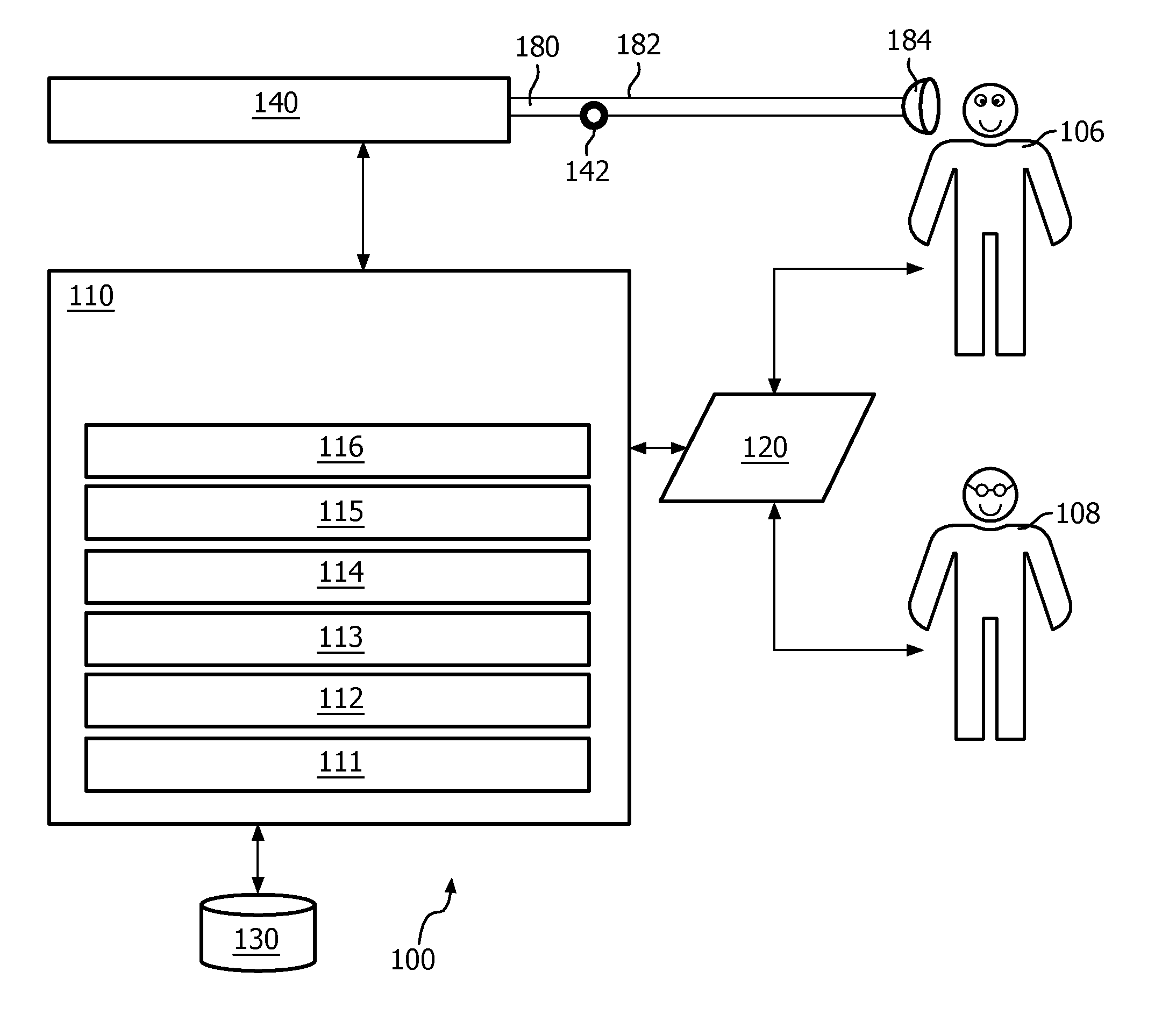
Devices and methods for non-invasive ventilation therapy
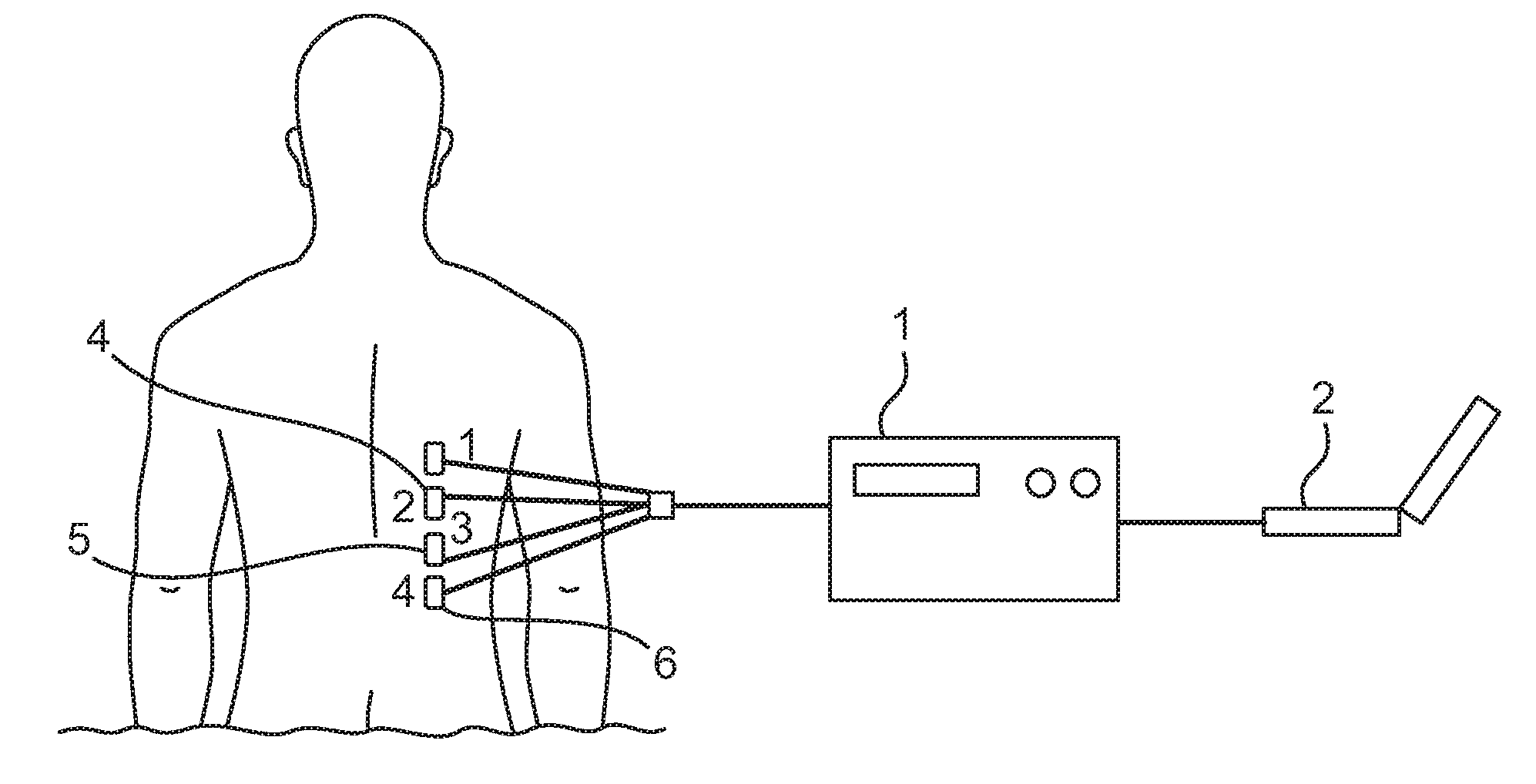
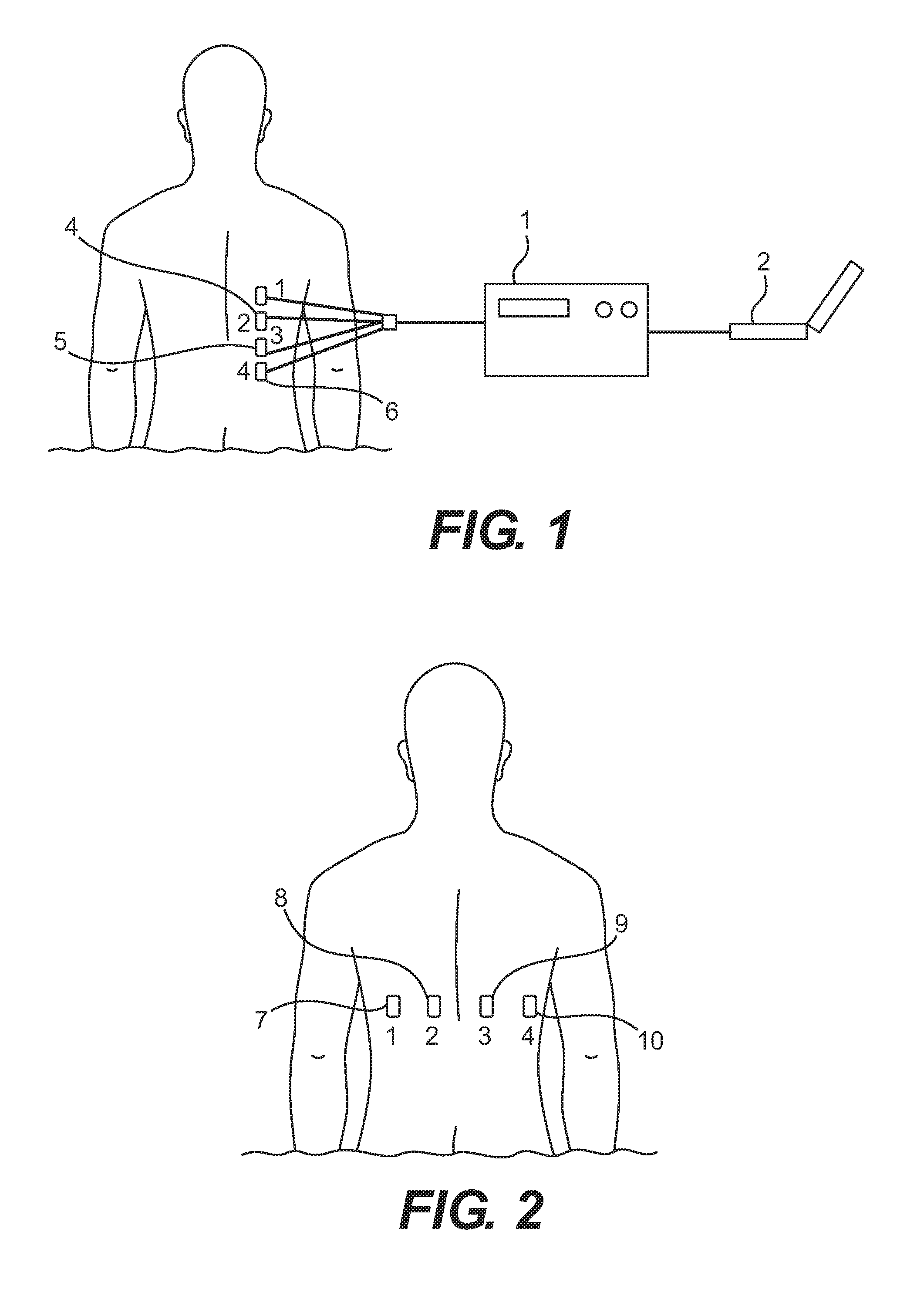
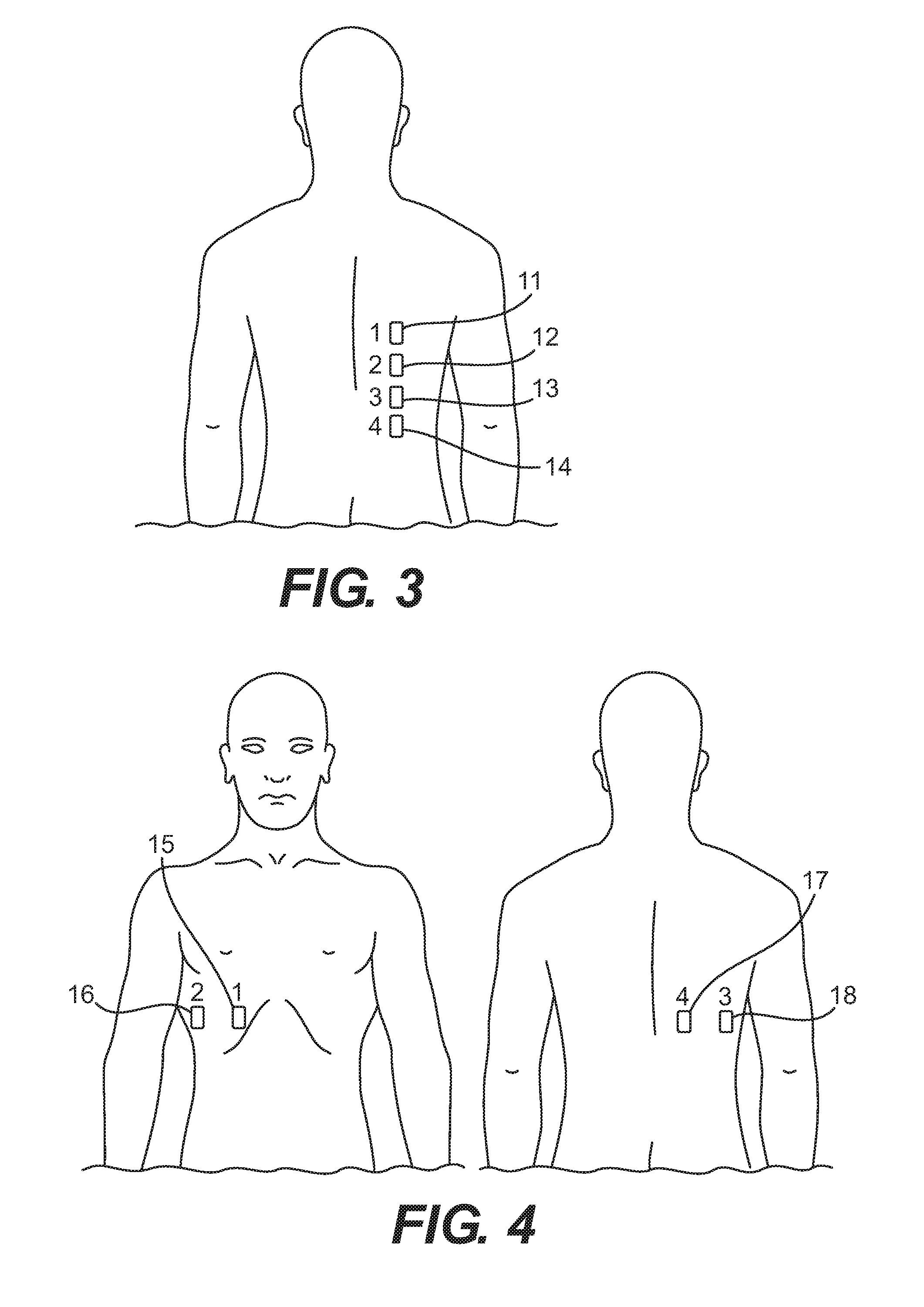
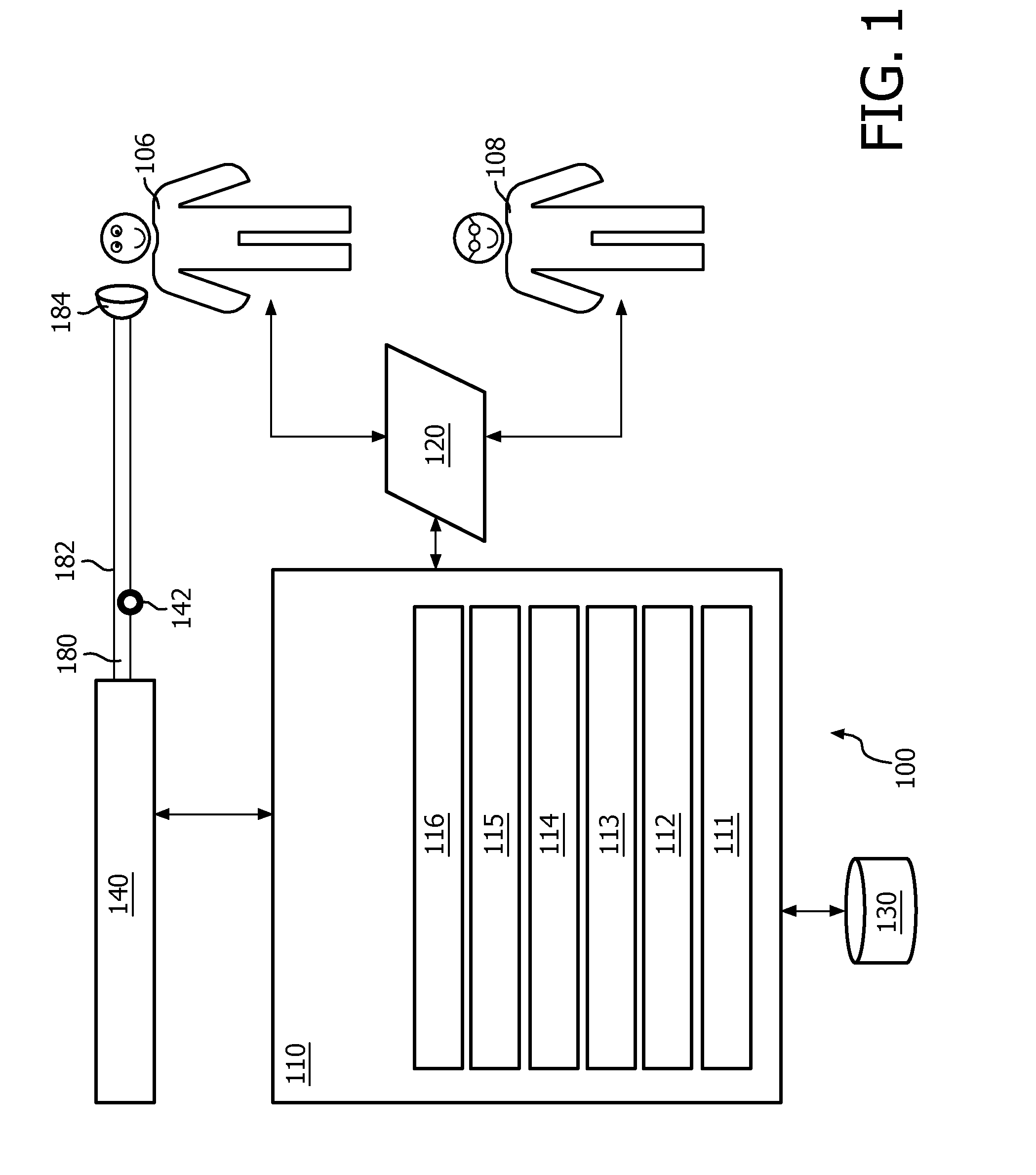
PendingUS20160367186A1Physical therapies and activitiesMechanical/radiation/invasive therapiesTreatment levelNon invasive
Non-invasive ventilation therapy systems and methods are disclosed. The system comprises a ventilation device, a computing device coupled to the ventilation device, and a plurality of sensors for acquiring a physiological bioelectrical impedance signal from a patient, wherein the sensors are functionally connected to the computing device. The computing device receives the physiological bioelectrical impedance signal from the sensors, analyzes the physiological bioelectrical impedance signal, and, based on the analyzed physiological bioelectrical impedance signal, transmits a signal to the ventilation device to adjust therapy levels.
Owner:RESPIRATORY MOTION
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with an entrainment port and/or pressure feature
Systems and methods may include a gas source, a gas delivery circuit, and a nasal interface allowing breathing ambient air through the nasal interface. A gas flow path through the nasal interface may have a distal gas flow path opening. A nozzle may be associated with a proximal end of the nasal interface a distance from the distal end gas flow path opening. At least a portion of an entrainment port may be between the nozzle and the distal end gas flow opening. The nozzle may deliver gas into the nasal interface to create a negative pressure area in the gas flow path at the entrainment port. The nasal interface and the nozzle may create a positive pressure area between the entrainment port and the distal end gas flow path opening. Gas from the gas delivery source and air entrained through the entrainment port may increase airway pressure or lung pressure or provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
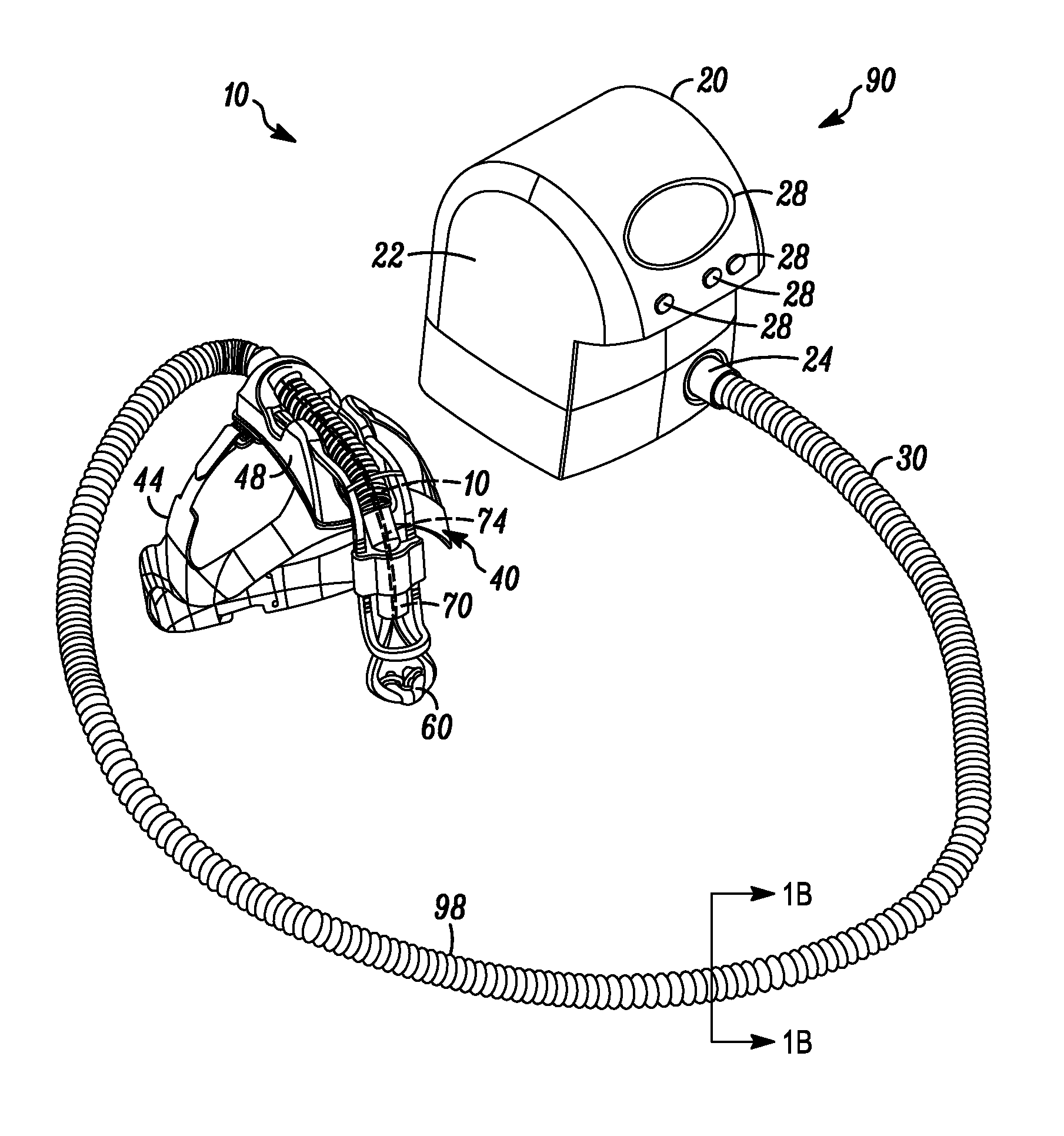
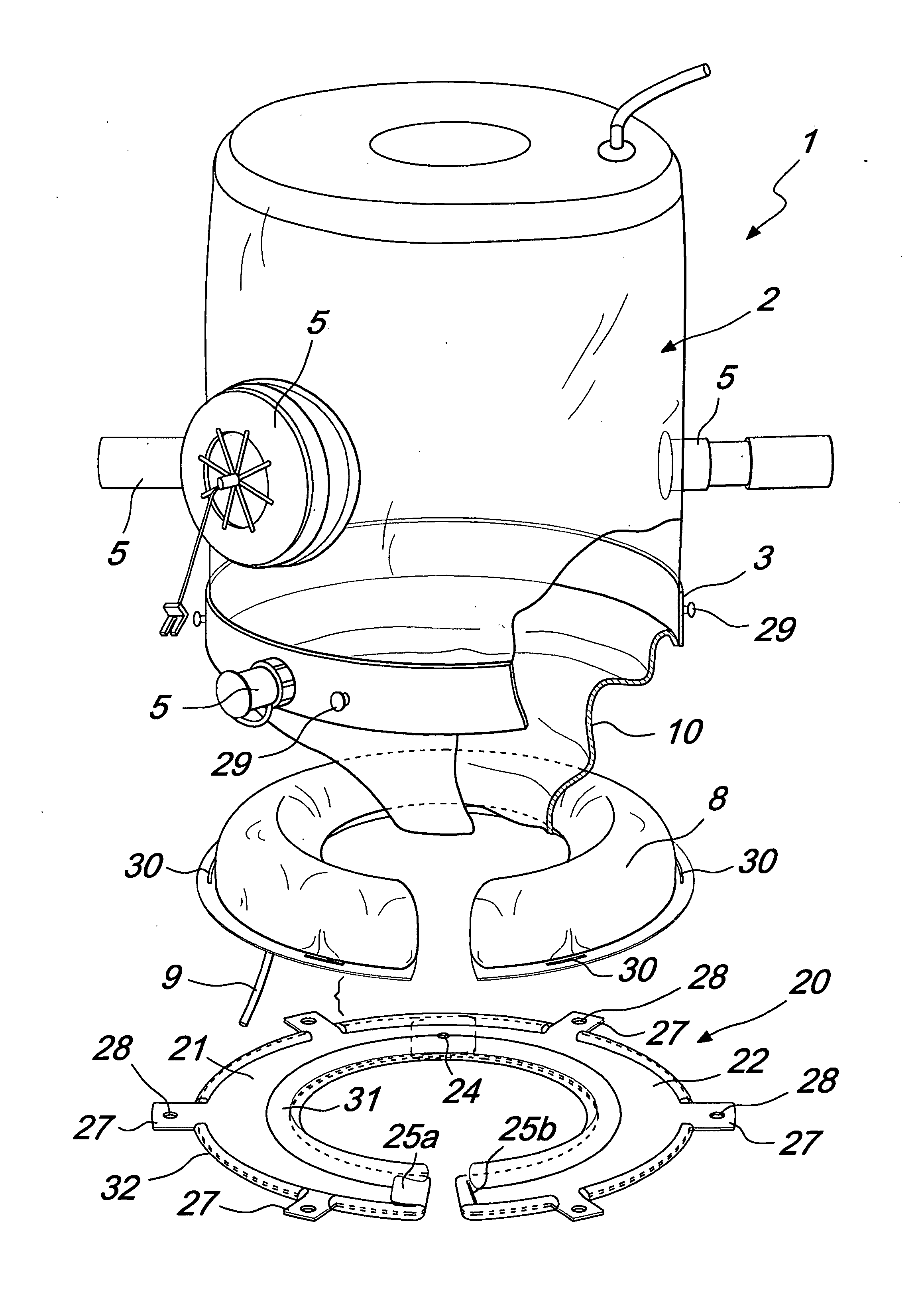
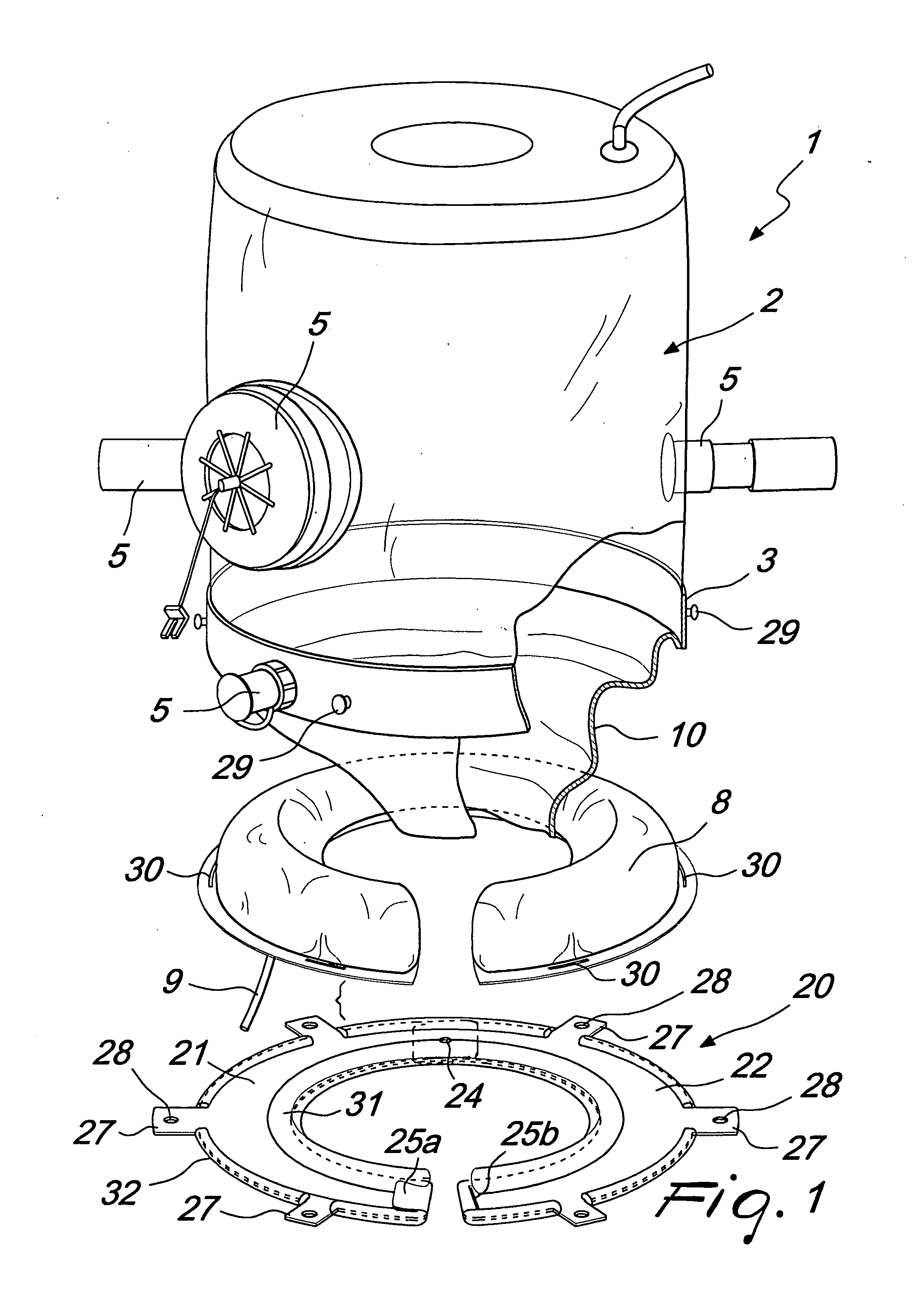
Hood for non-invasive ventilation of patients
InactiveUS20110226240A1Reduce the impactReduce exerciseChemical protectionHeat protectionNon-invasive ventilationEngineering
A hood for non-invasive ventilation of patients, comprising a containment body provided with at least one optically transparent portion and with a collar that can be mated hermetically to the neck of the patient whose head is accommodated within the containment body, the hood further comprising an annular body, on which a cushion is heat-sealed or fixed and which can be associated around the neck and can be fixed to the containment body, the annular body fixed to the containment body is substantially rigid and is adapted to act as an abutment element, together with the cushion, for the collar.
Owner:INTERSURGICAL SPA
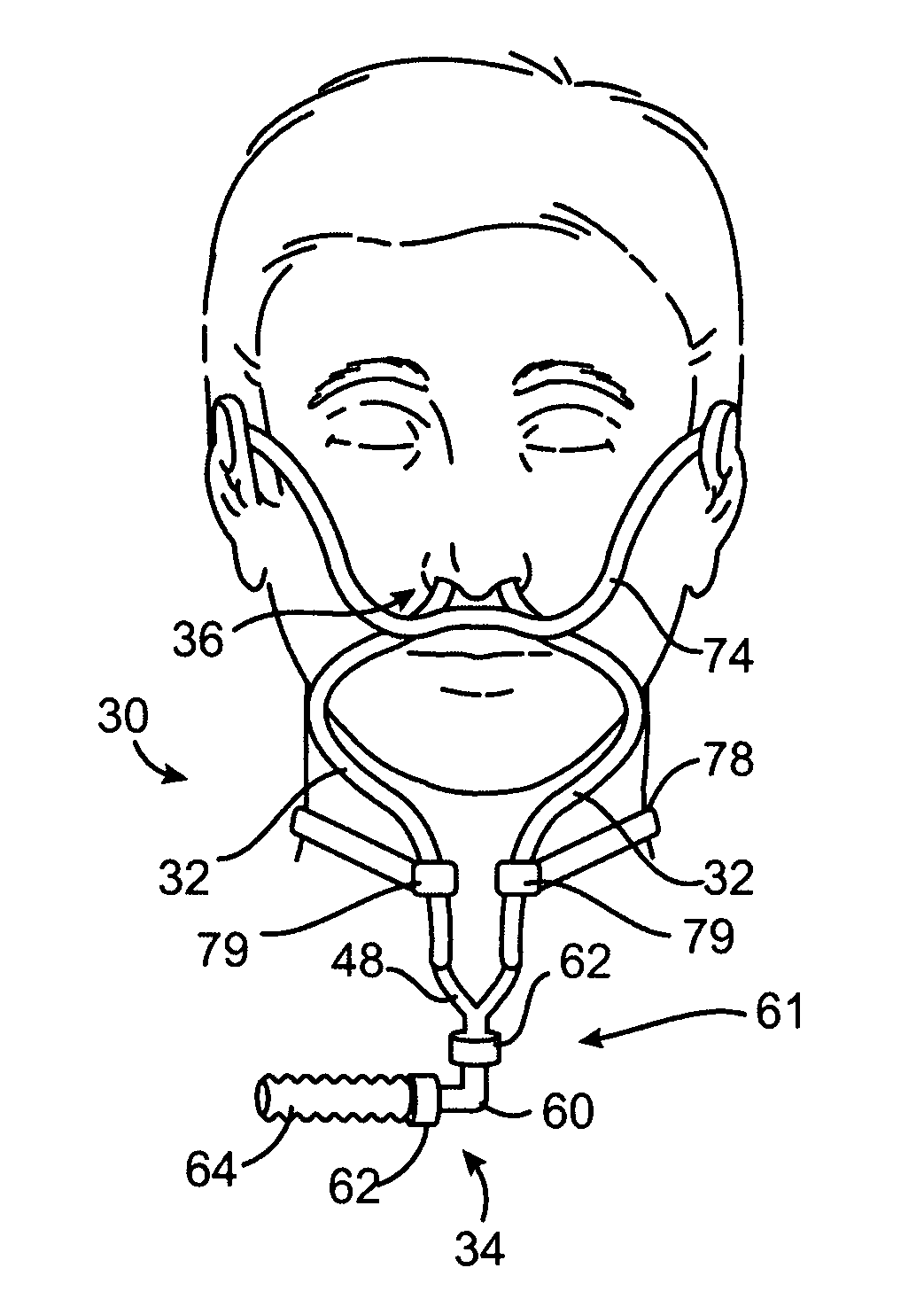
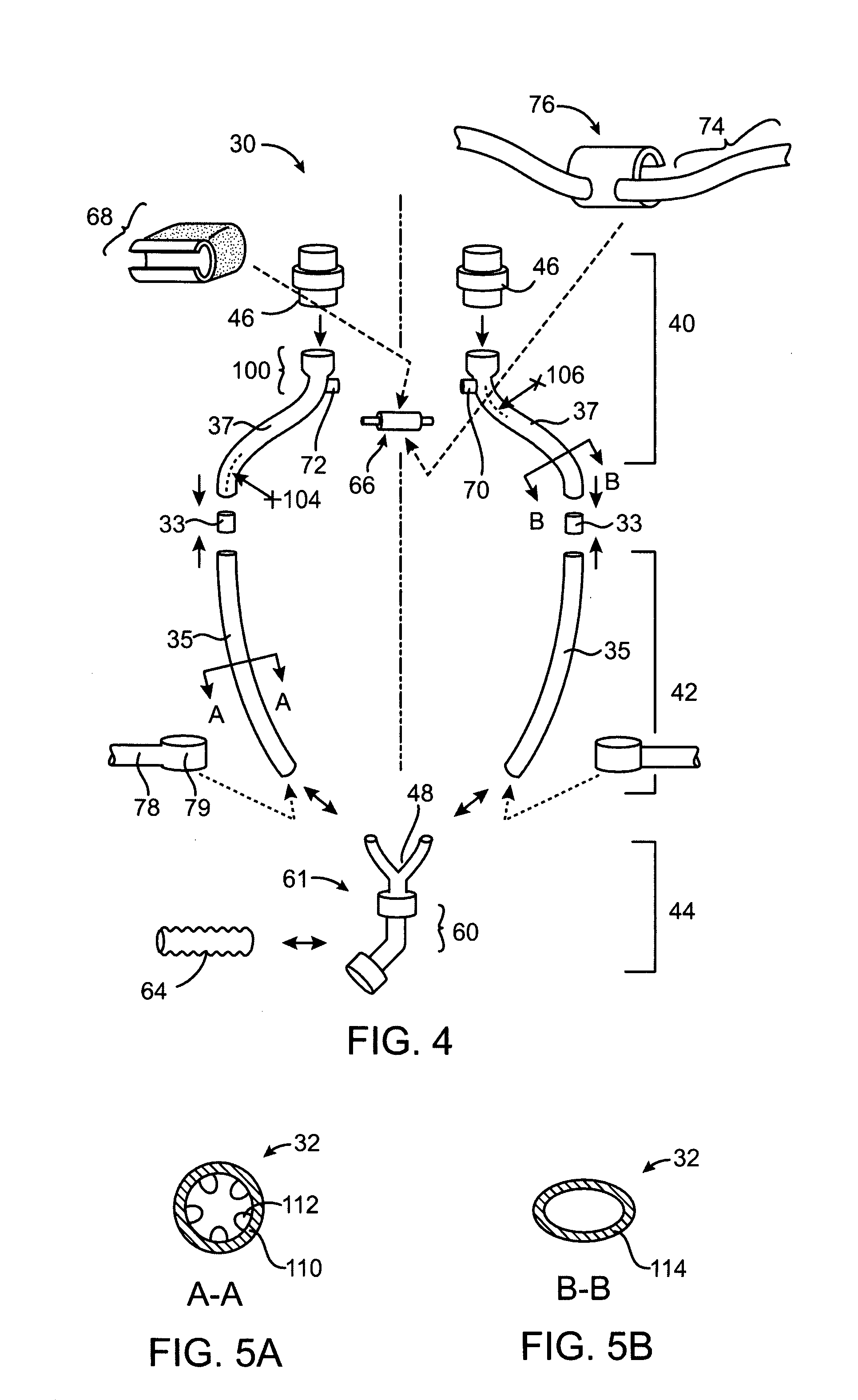
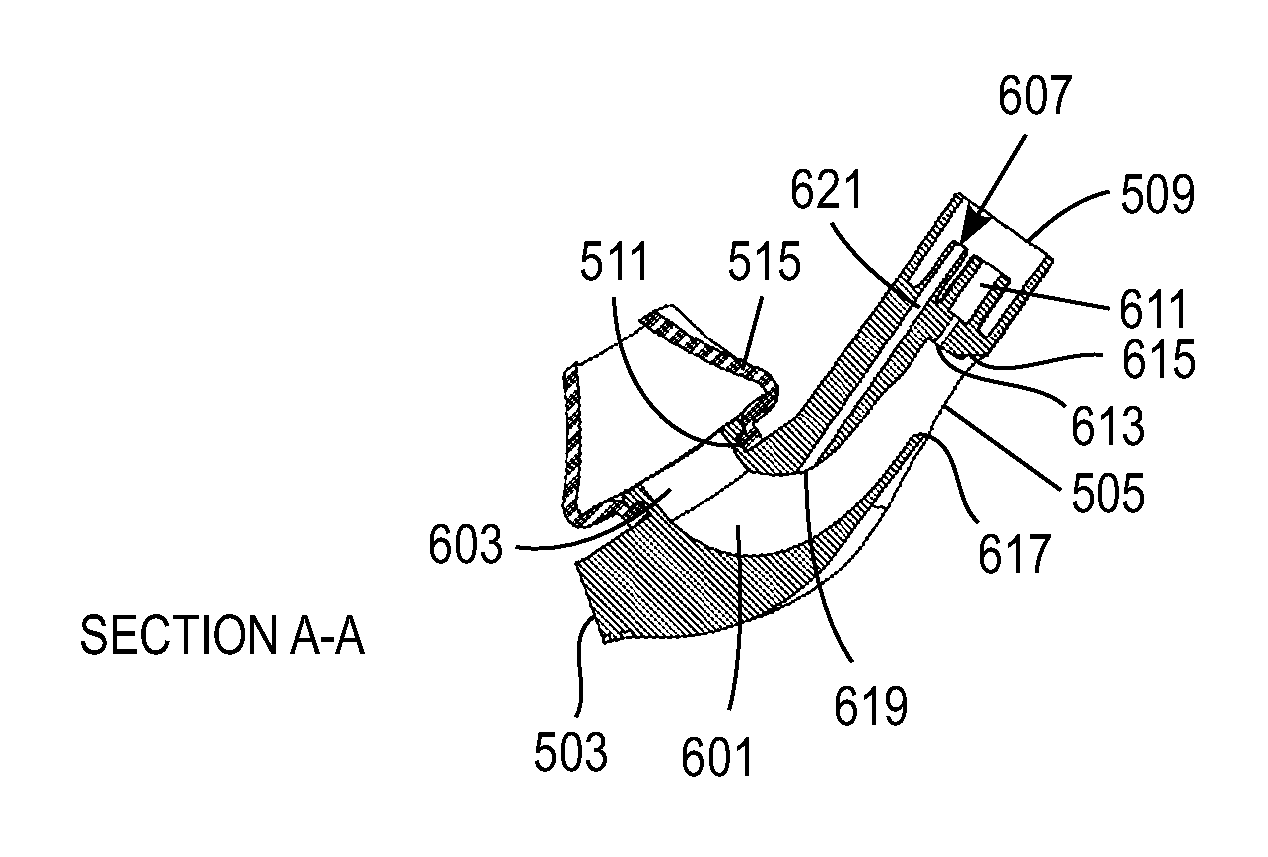
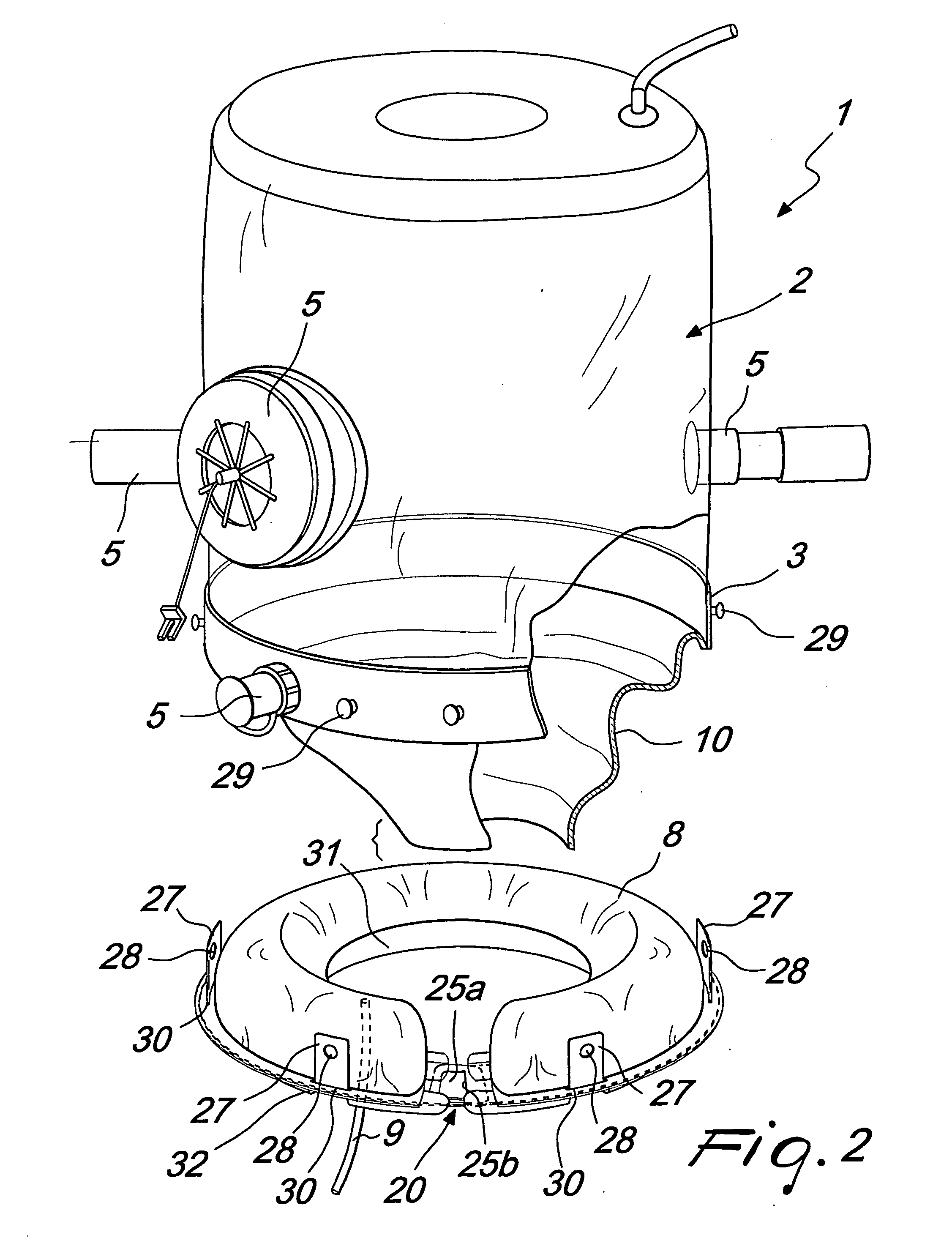
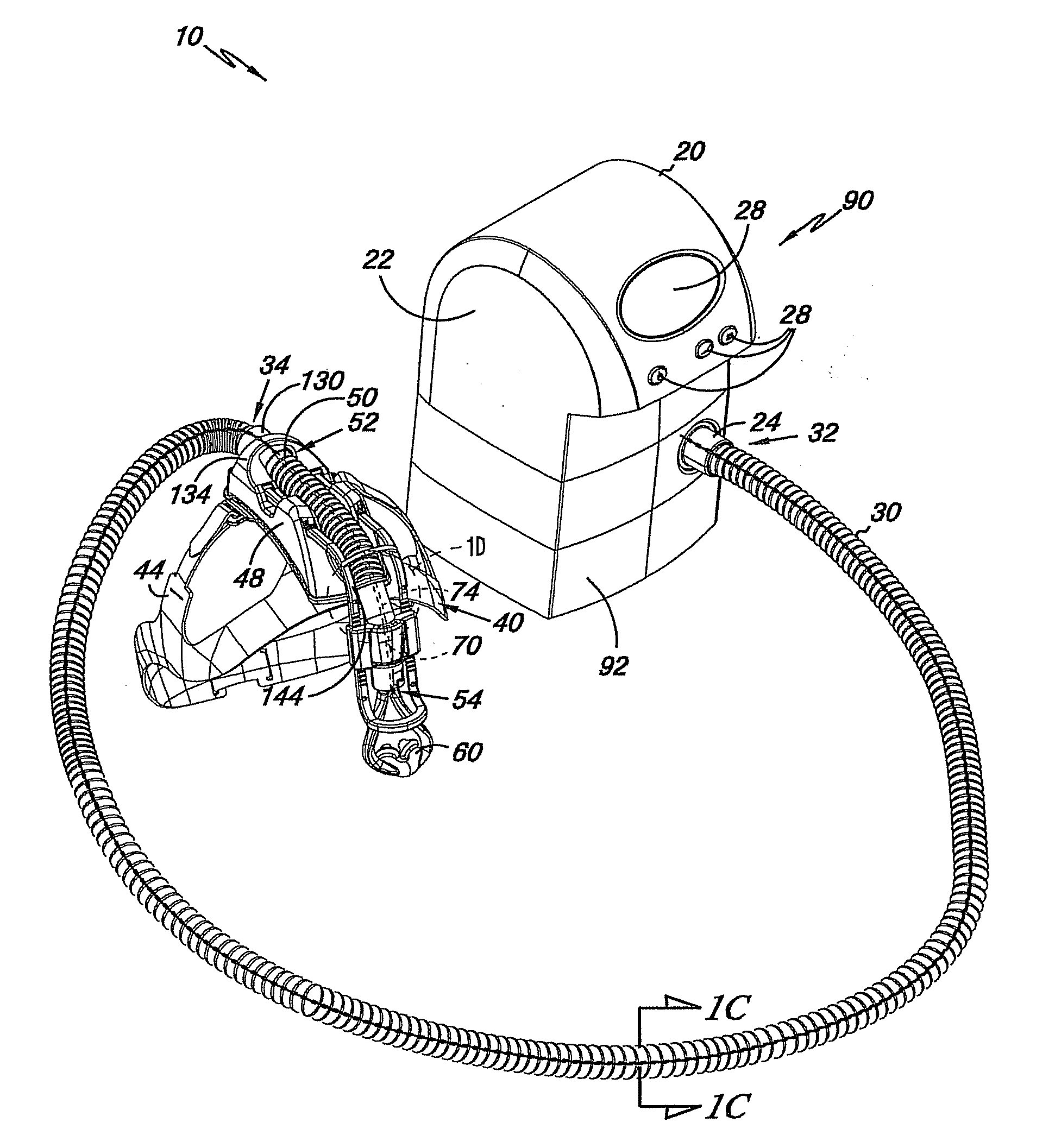
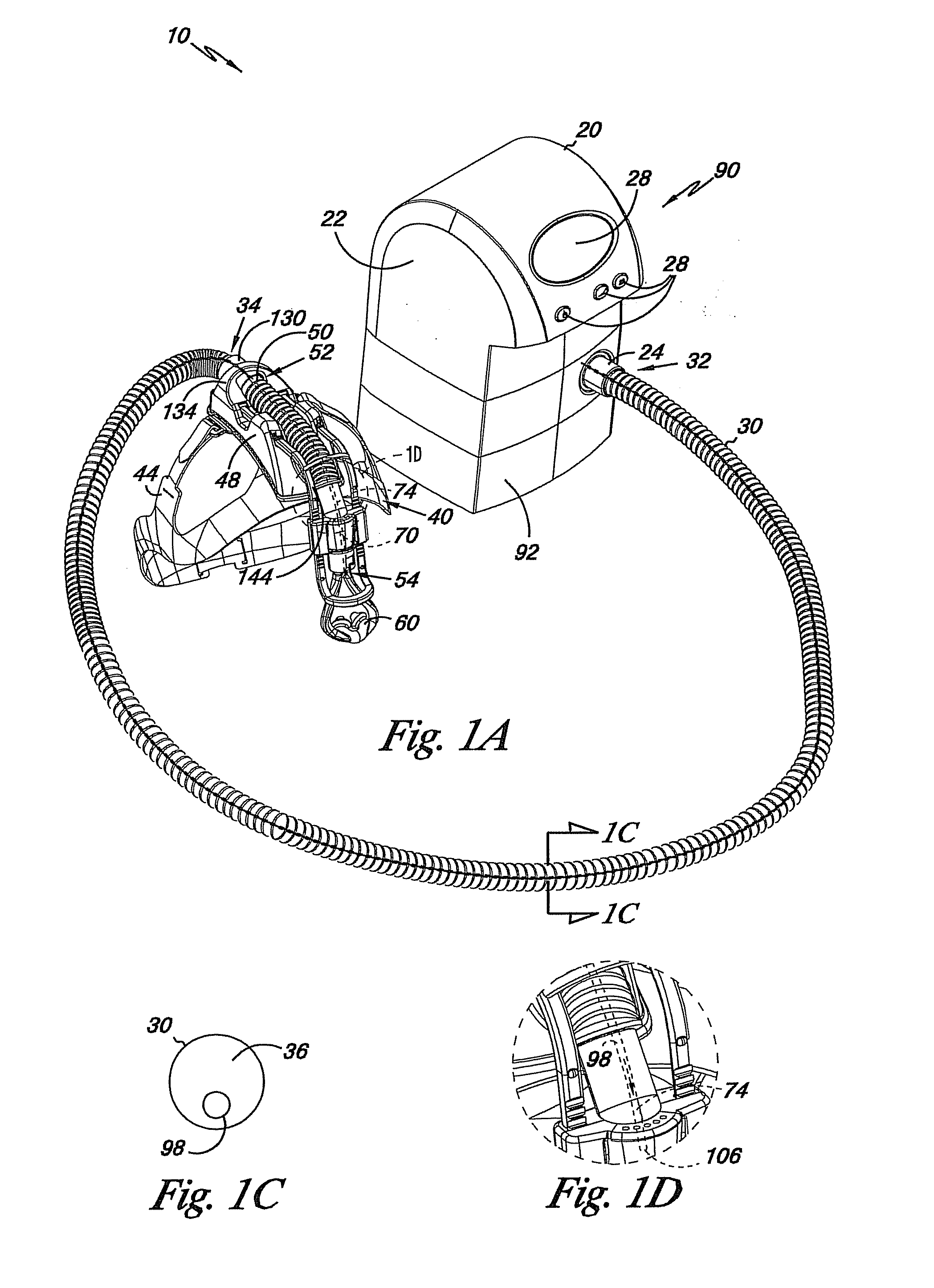
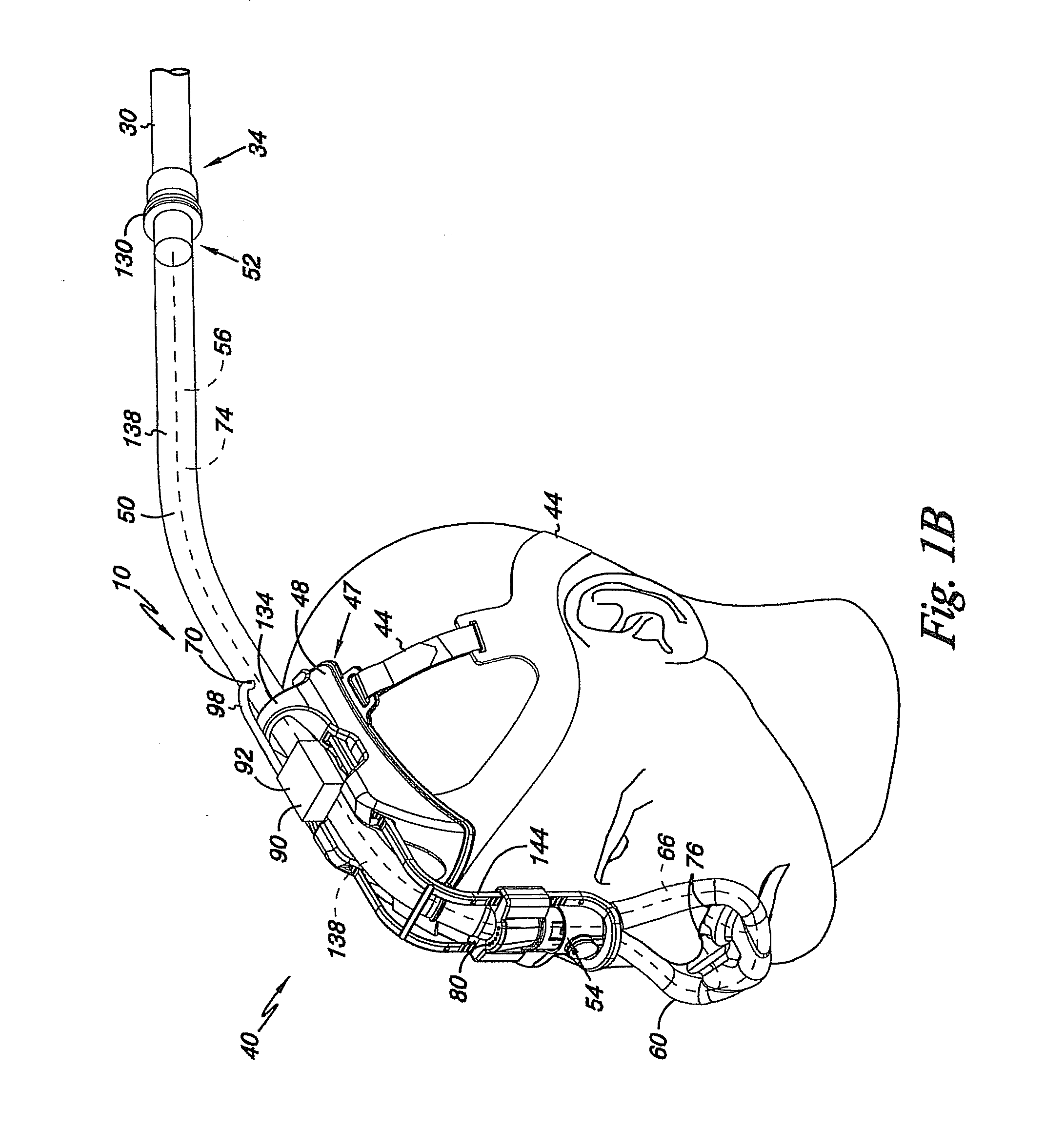
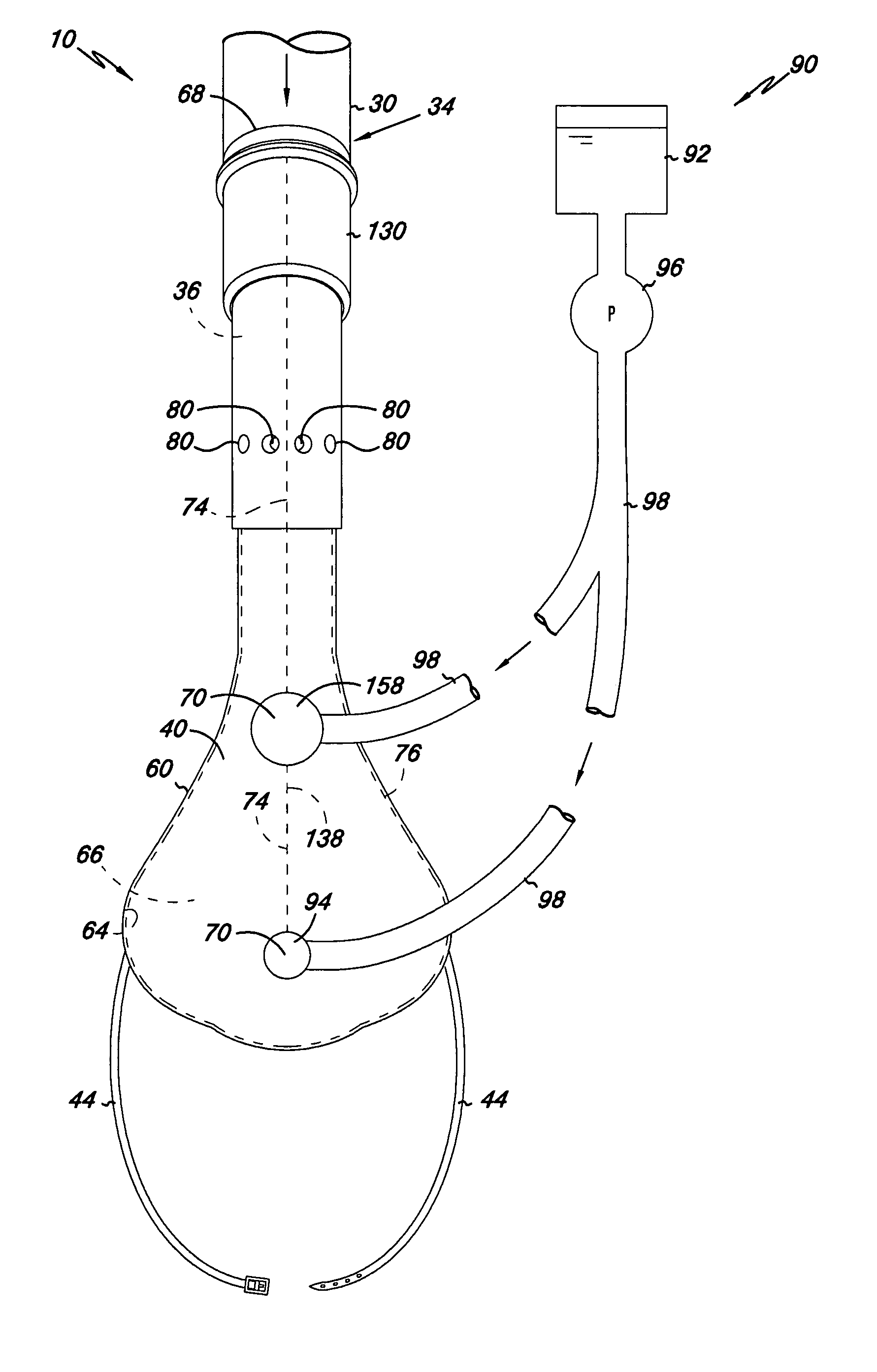
Methods, systems and devices for ventilation using a nasal ventilation mask with a manifold and internal compliant tube and nasal sealing cushion assembly
Embodiments of the present invention may provide ventilation to a patient's lung or airway using a nasal ventilation mask, as part of either a non-invasive ventilation system (NIV) or a non-invasive open-airway ventilation system (NIOV). A ventilation mask may include a rigid or semi-rigid manifold housing. A compliant tube may be located within the manifold housing for forming a main gas pathway through the manifold housing. One or more nasal connectors may be fluidly coupled to the main gas pathway in the compliant tube. A system for sensing airflow through a patient's nose may include a sensing port with a distal opening that opens to a main gas pathway. A protrusion on at least one side of the distal opening may protrude into the main gas pathway.
Owner:BREATHE TECHNOLOGIES INC
Adjustable positive airway pressure or ventilation system
ActiveUS20160015921A1Improve comfortReduce hardnessRespiratory masksBreathing masksPositive airway pressurePositive pressure
The present disclosure relates to a comfortable and adjustable nasal pillow configured to be part of a nasal pillow system that is part of a mask system used with a ventilation or PAP device. The nasal pillows are configured to have multiple degrees of freedom of rotation.
Owner:HUMAN DESIGN MEDICAL
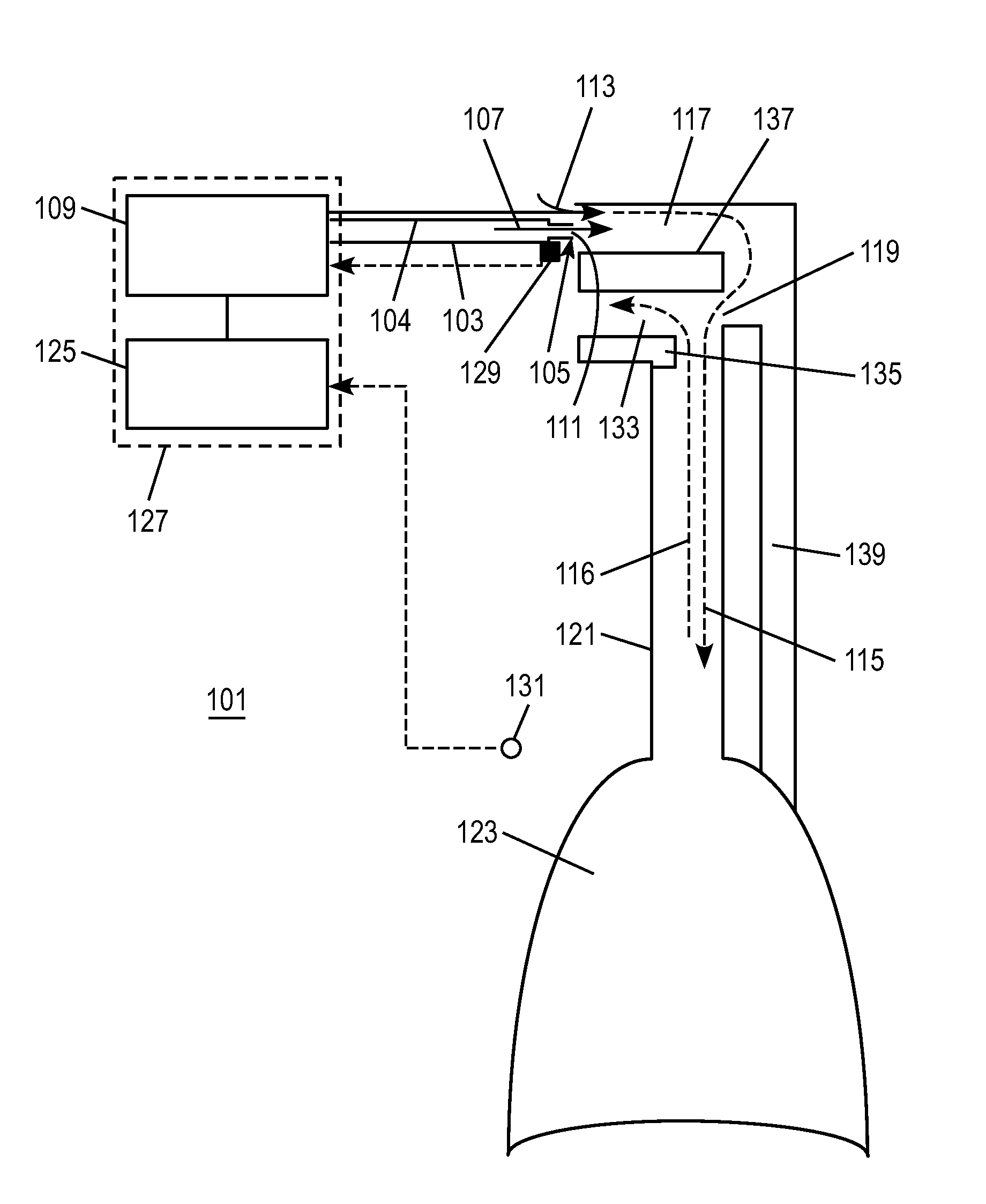
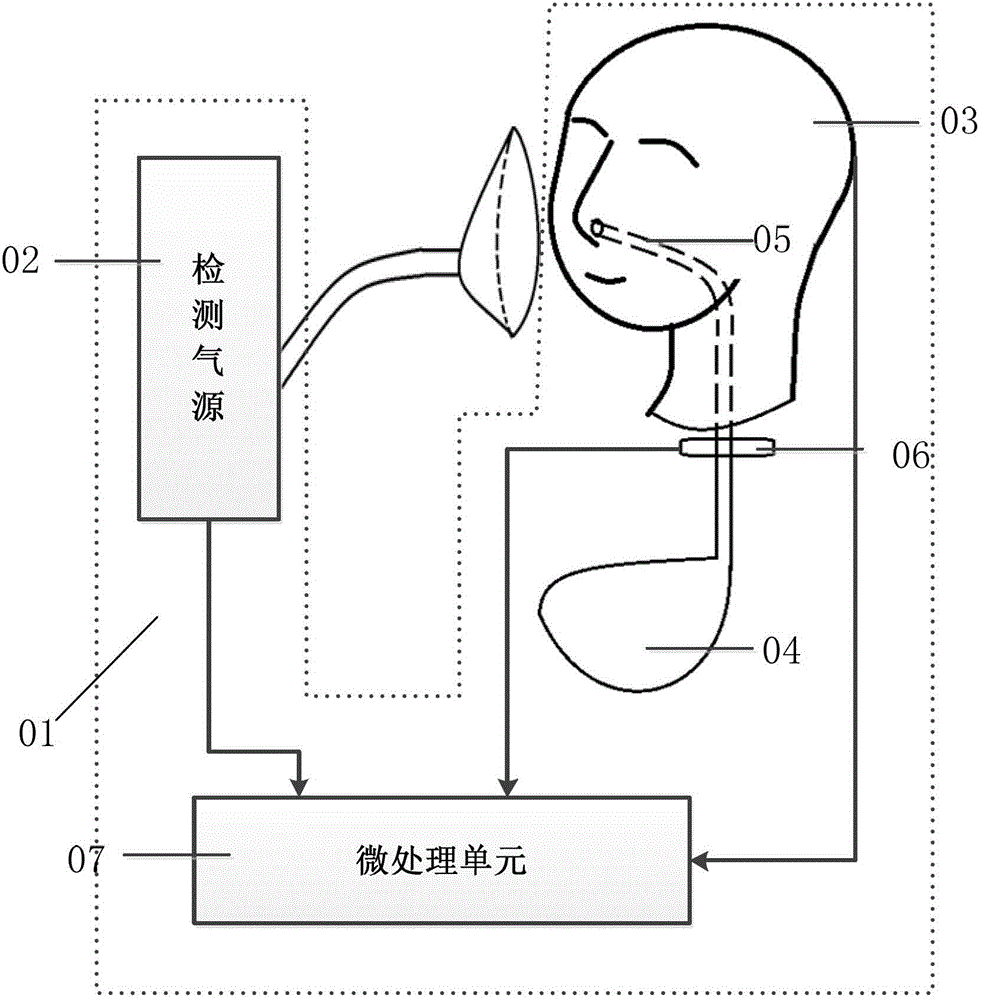
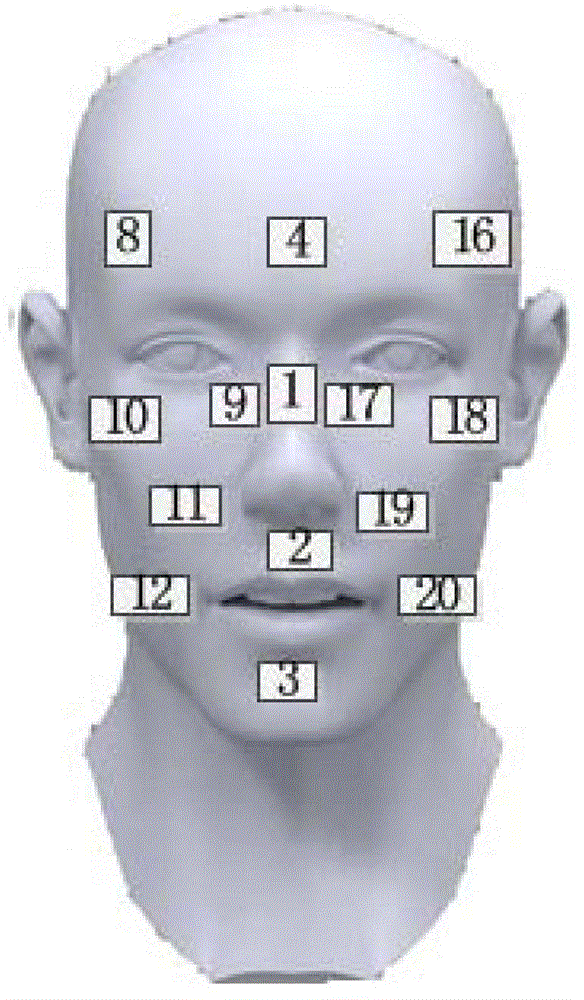
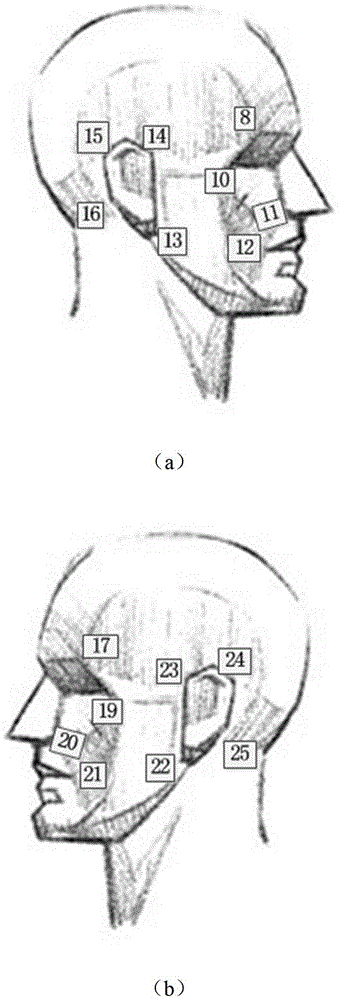
Detection system for noninvasive ventilation interface
InactiveCN102944371AMeasurement of fluid loss/gain rateEducational modelsSurface stressNoninvasive ventilation
The invention belongs to a detection system (01) for a noninvasive ventilation interface and particularly relates to a detection system for evaluating the air leakage and the comfortableness of interfaces such as a nasal mask, a mouth-nose mask and a full-face mask (08) for noninvasive ventilation by combining three-dimensional structure characteristics of human heads. The detection system comprises a detection air source (02), a human head three-dimensional model (03), a simulation trachea (05), a lung model (04) and a micro processing unit (07), wherein the detection air source (02) can be used for generating a designated ventilation waveform; the human head three-dimensional model (03) can be used for detecting the surface stress; the simulation trachea (05) and the lung model (04) are connected with the human head three-dimensional model and allow sensors (06) to be placed; and the micro processing unit (07) can be used for evaluating the air leakage and the comfortableness of the head and the face. The air leakage is detected by comparing the preset ventilation waveform of the air source with the actually-detected waveform of the trachea model, and the stresses of the mask worn at different positions of the head are measured by a plurality of pressure sensors arranged on the head model and are compared with a human tolerance threshold, and thus the comfortableness of the mask is judged.
Owner:BEIHANG UNIV
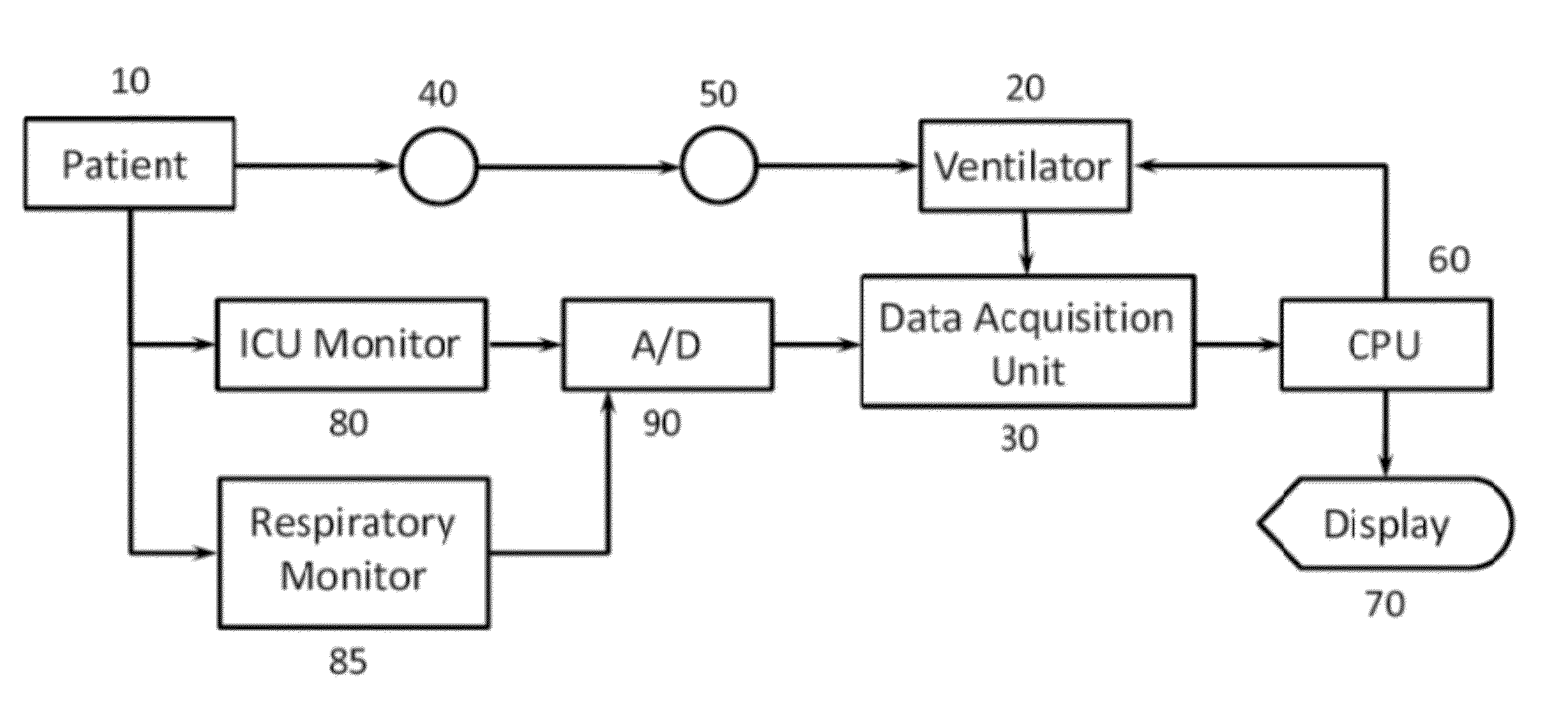
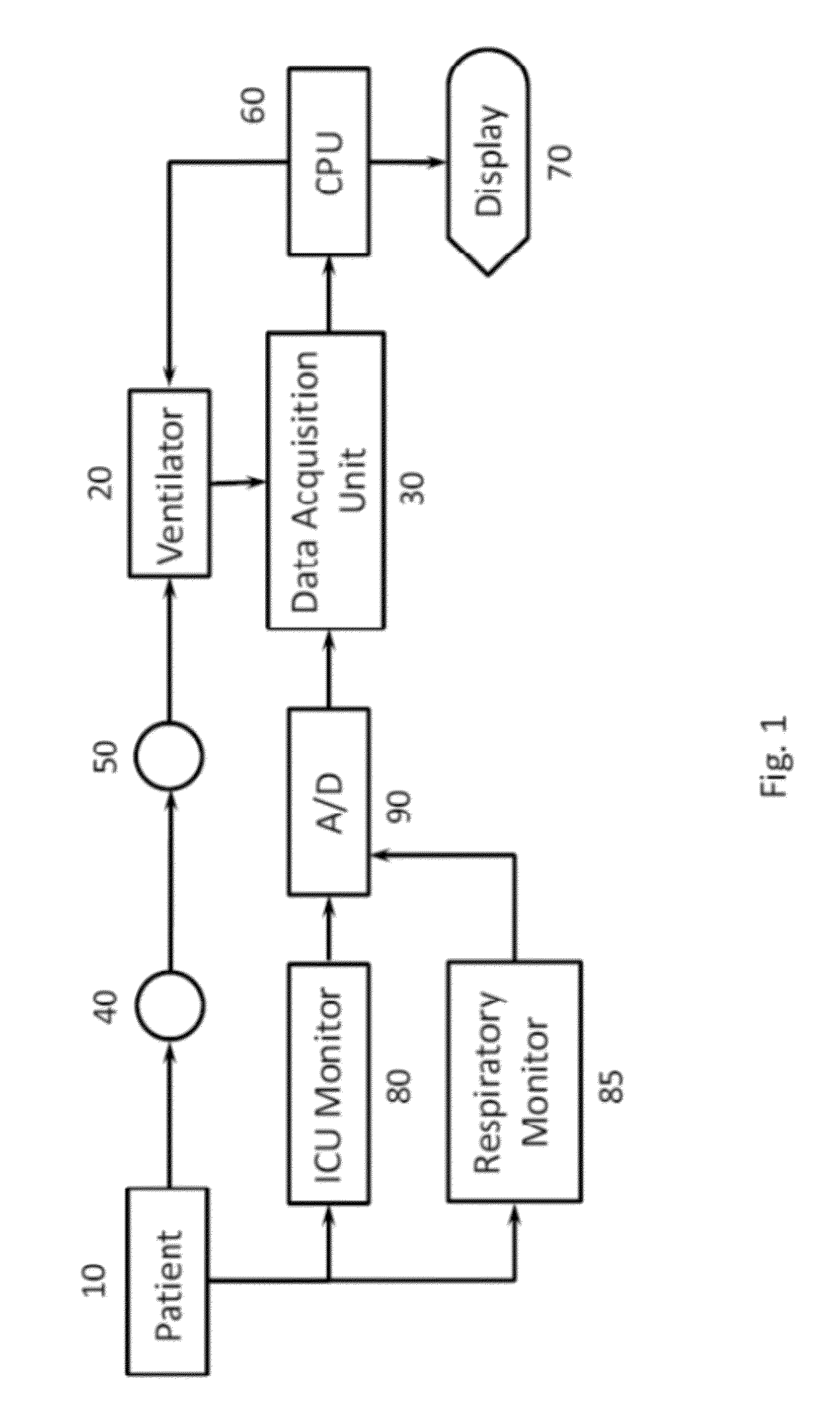
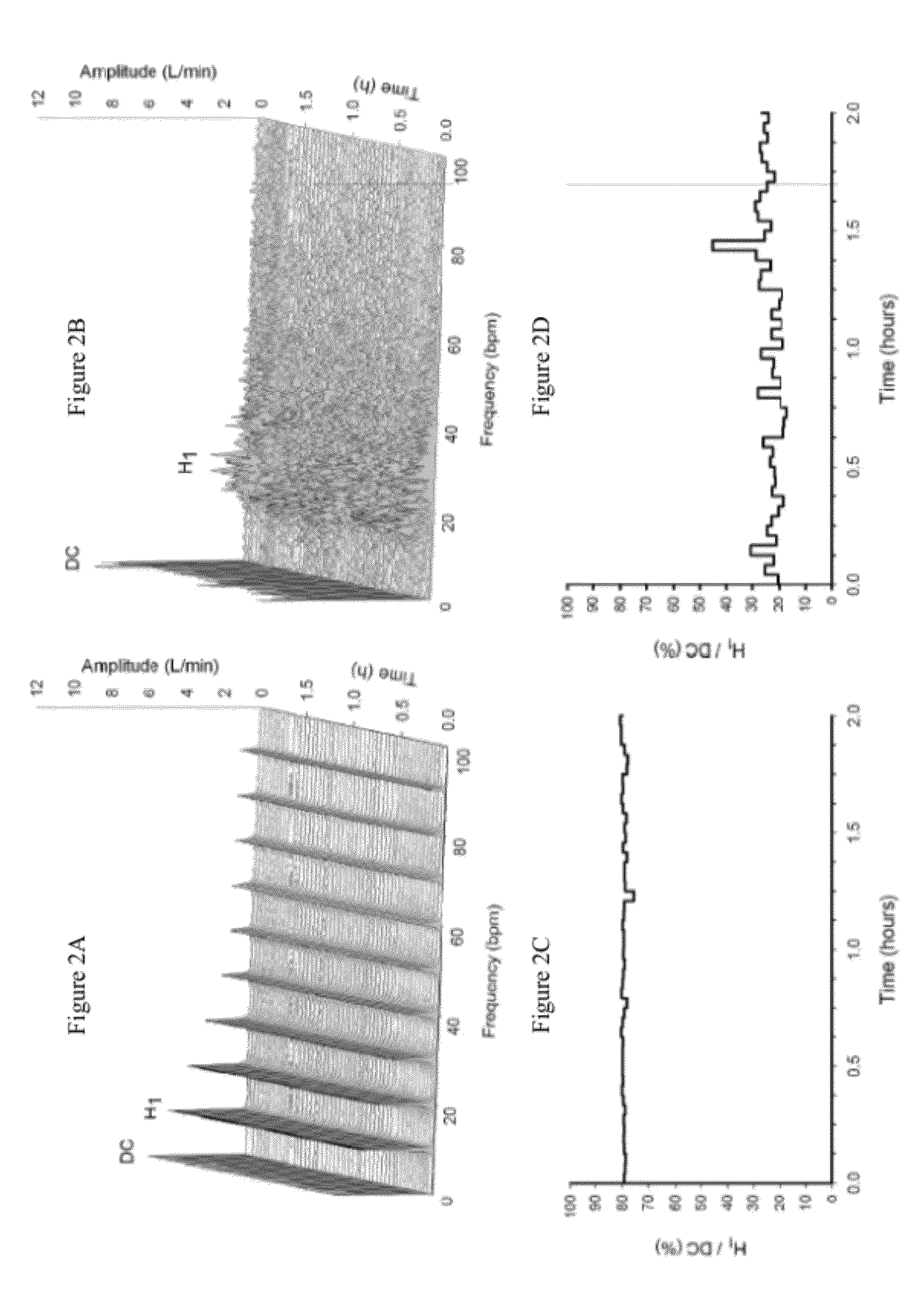
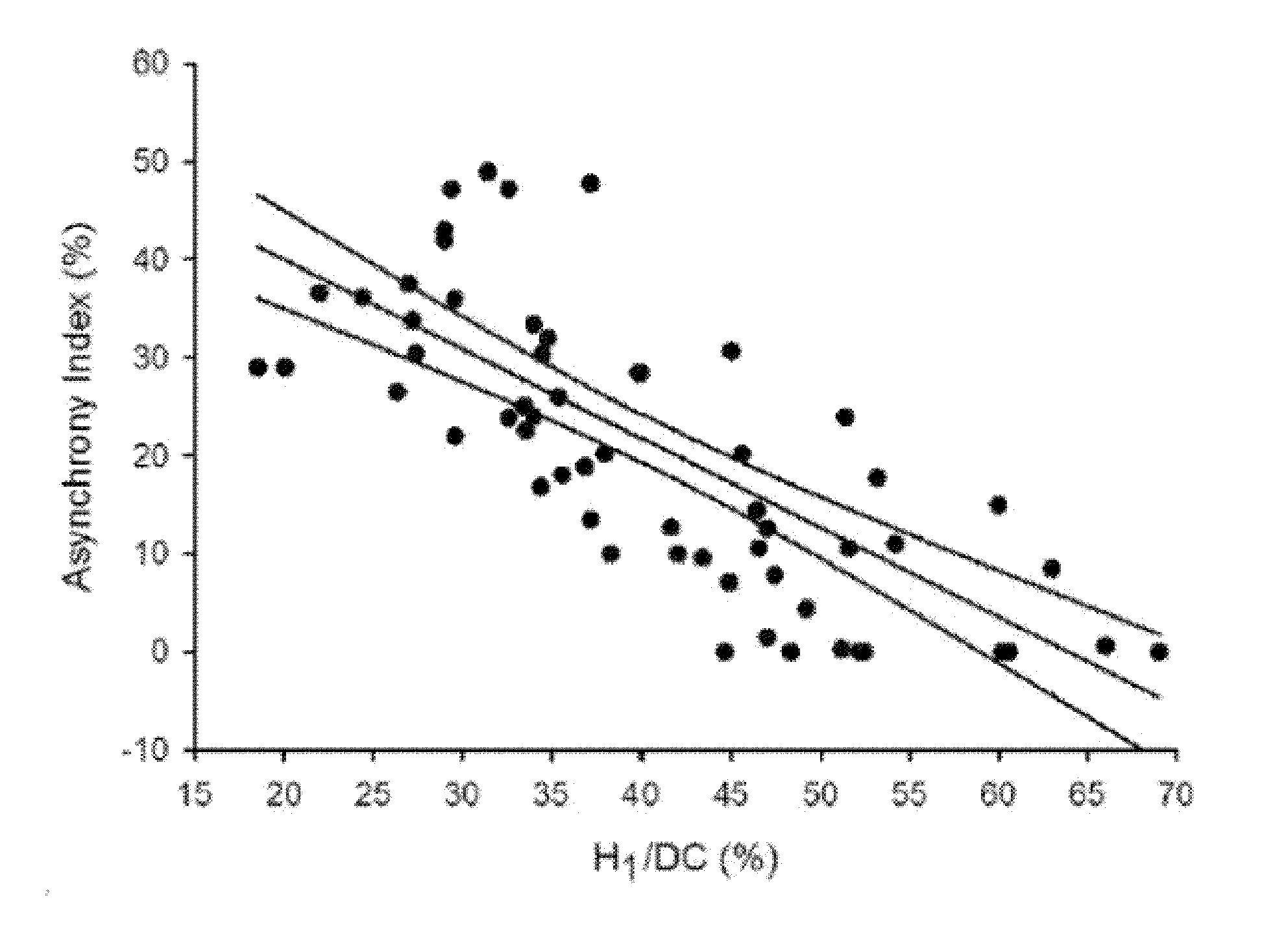
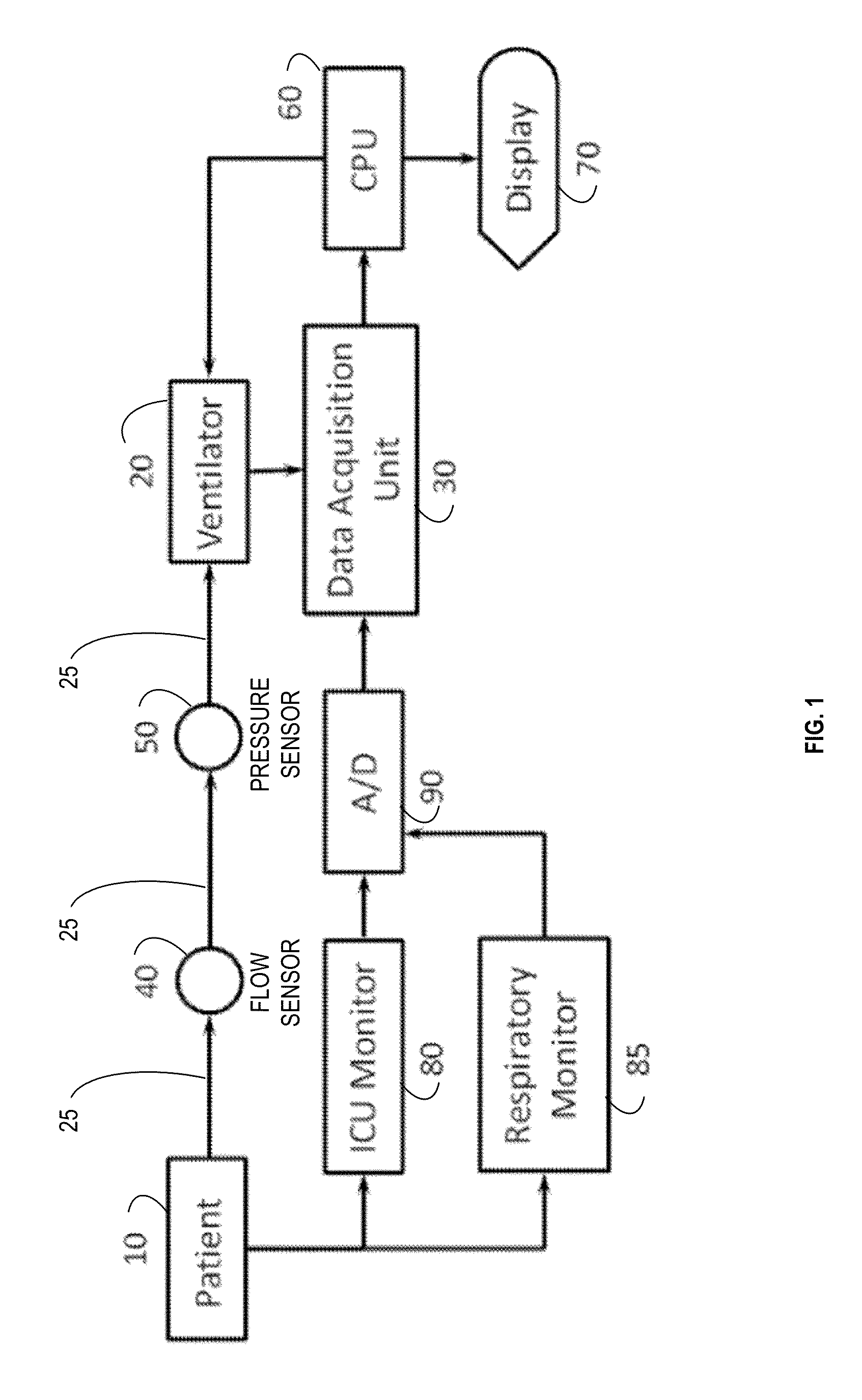
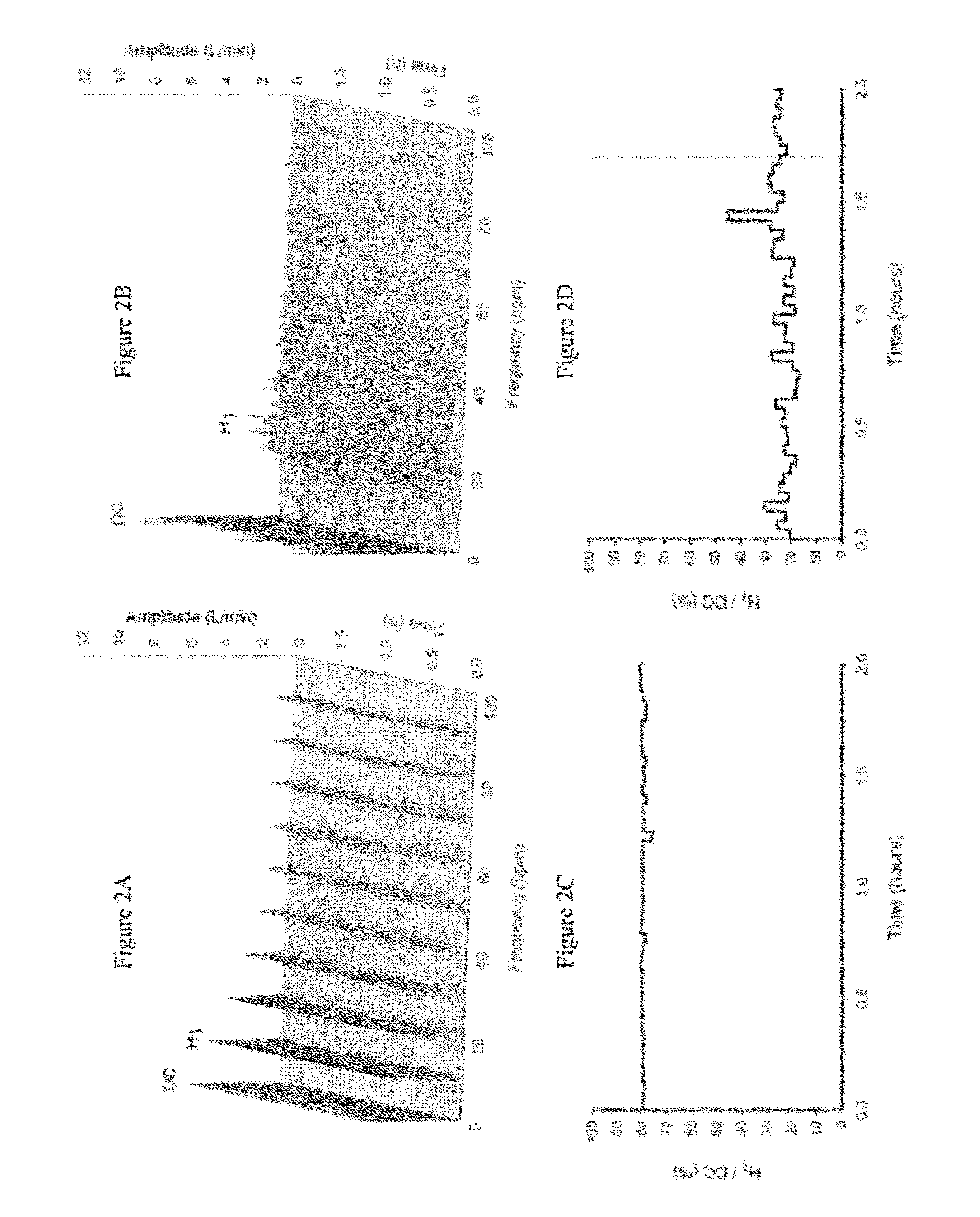
Method and system to detect respiratory asynchrony
ActiveUS20120073574A1RespiratorsOperating means/releasing devices for valvesFrequency spectrumMonitoring system
Owner:RESPIVAR LLC
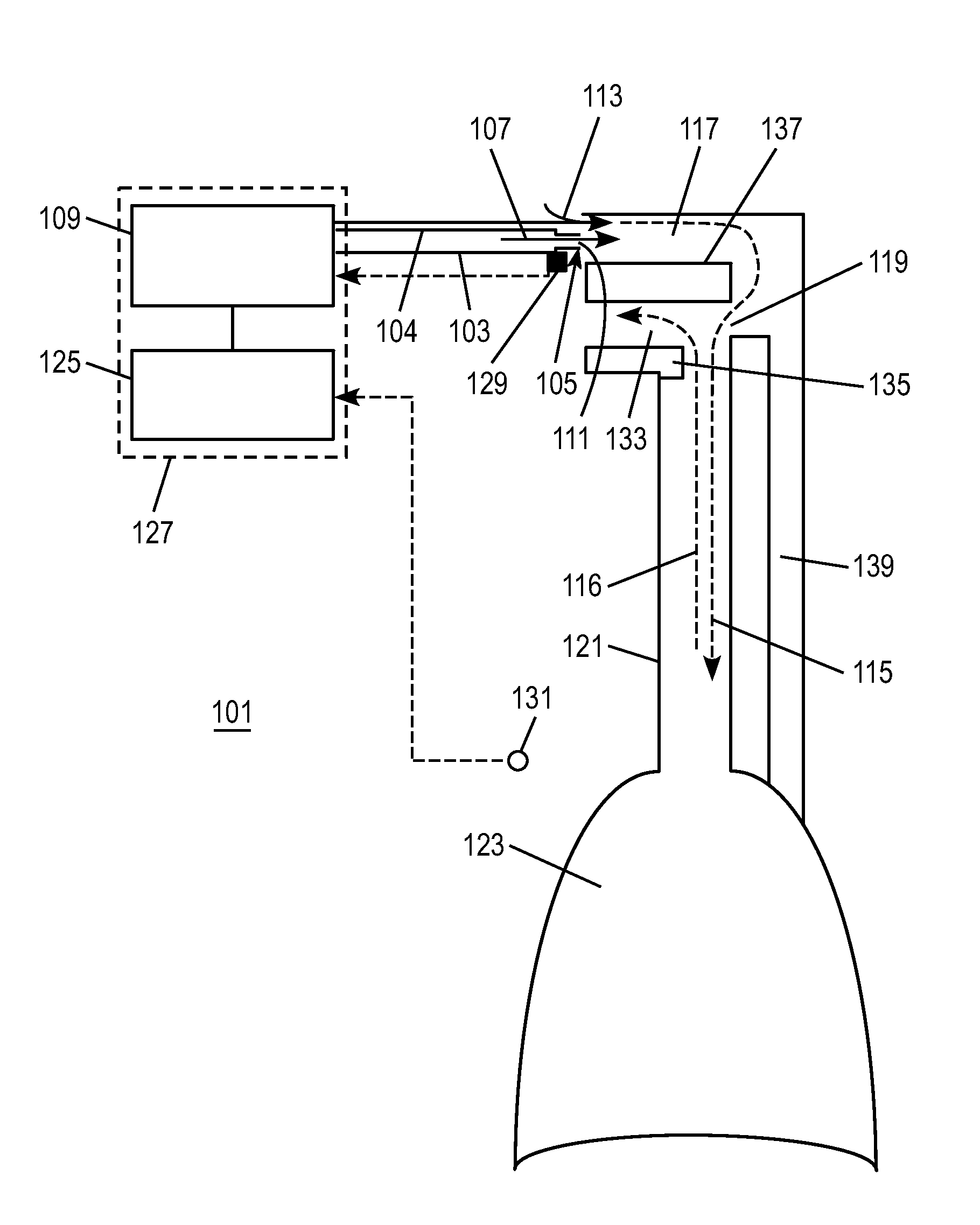
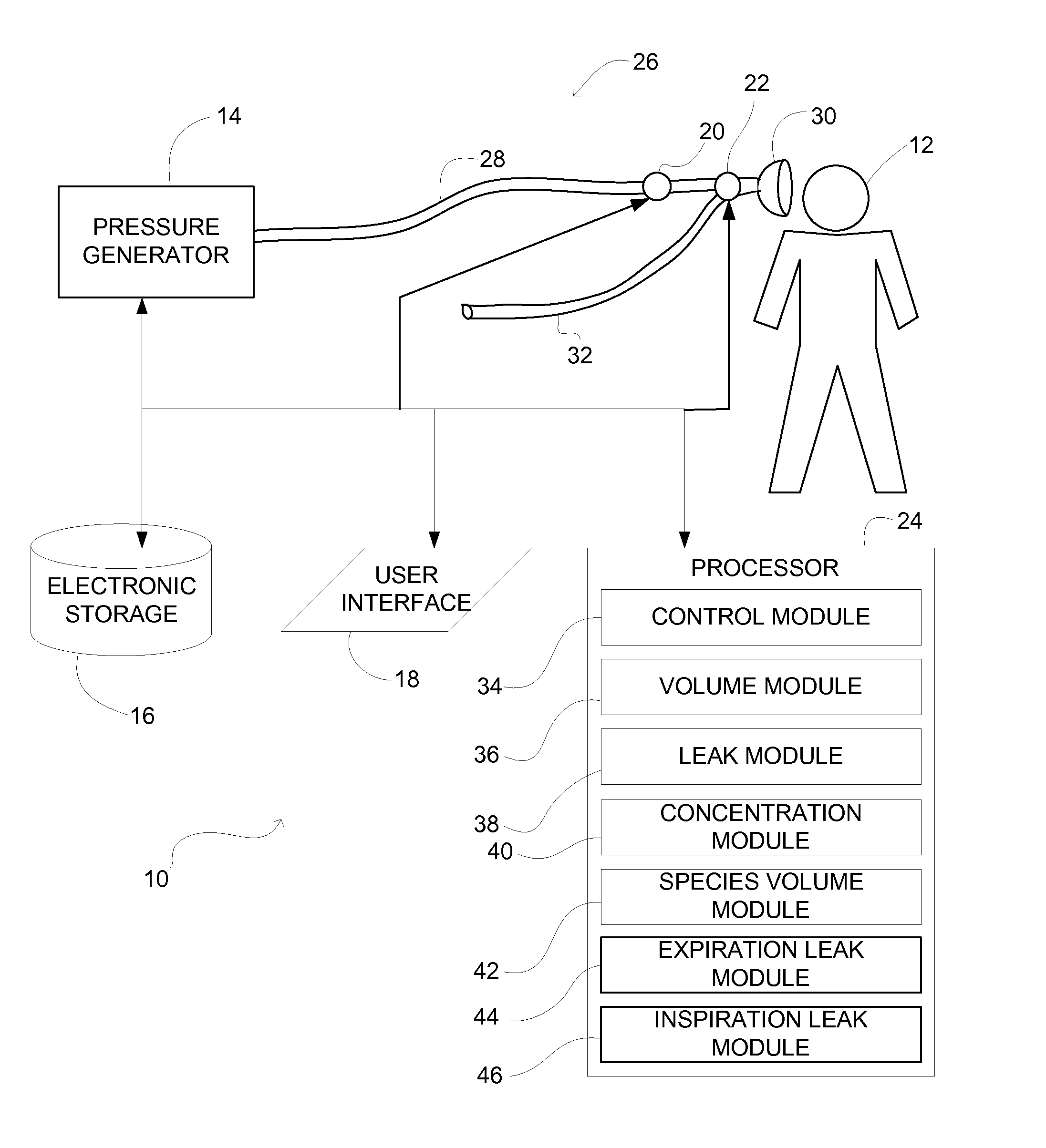
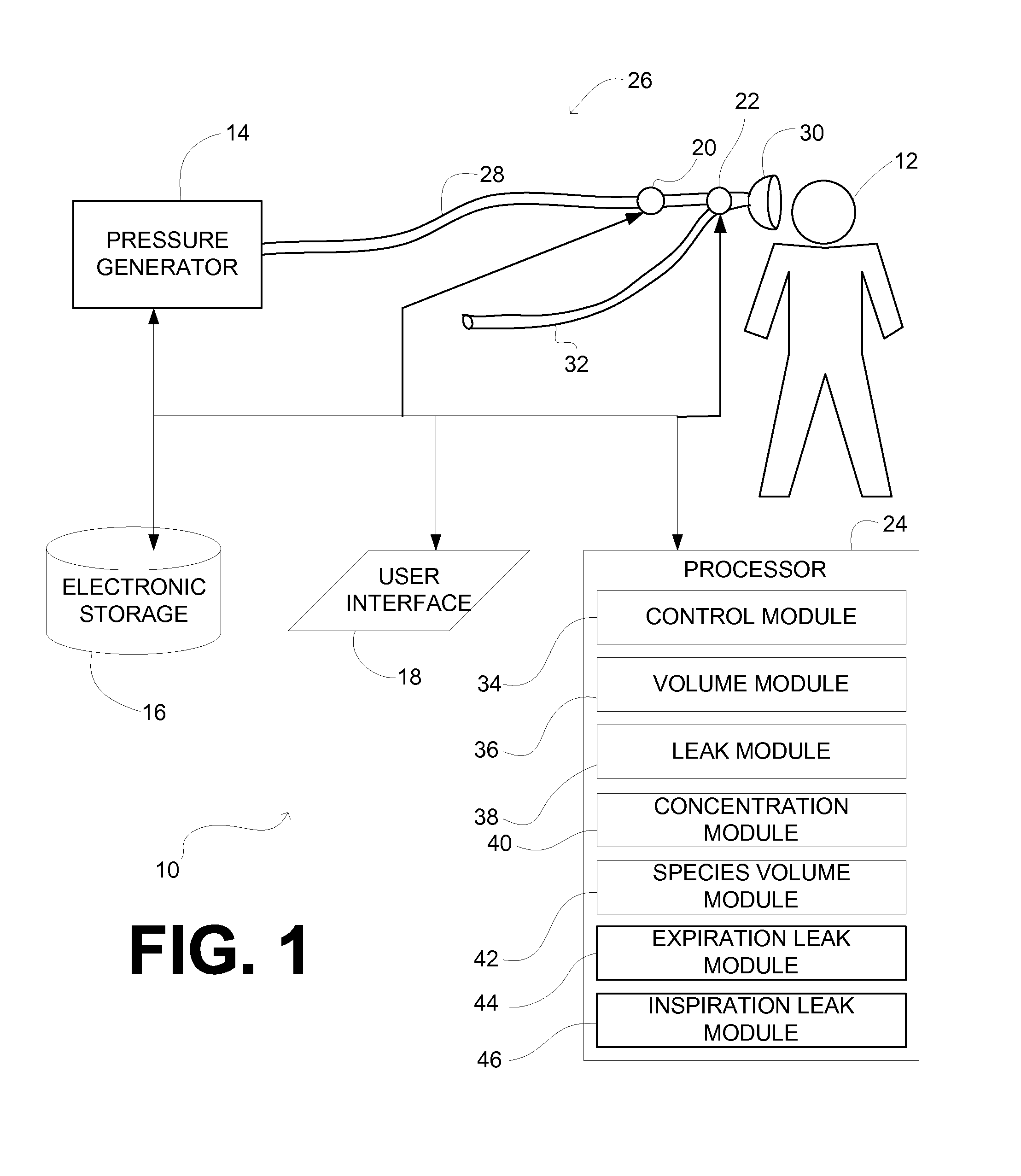
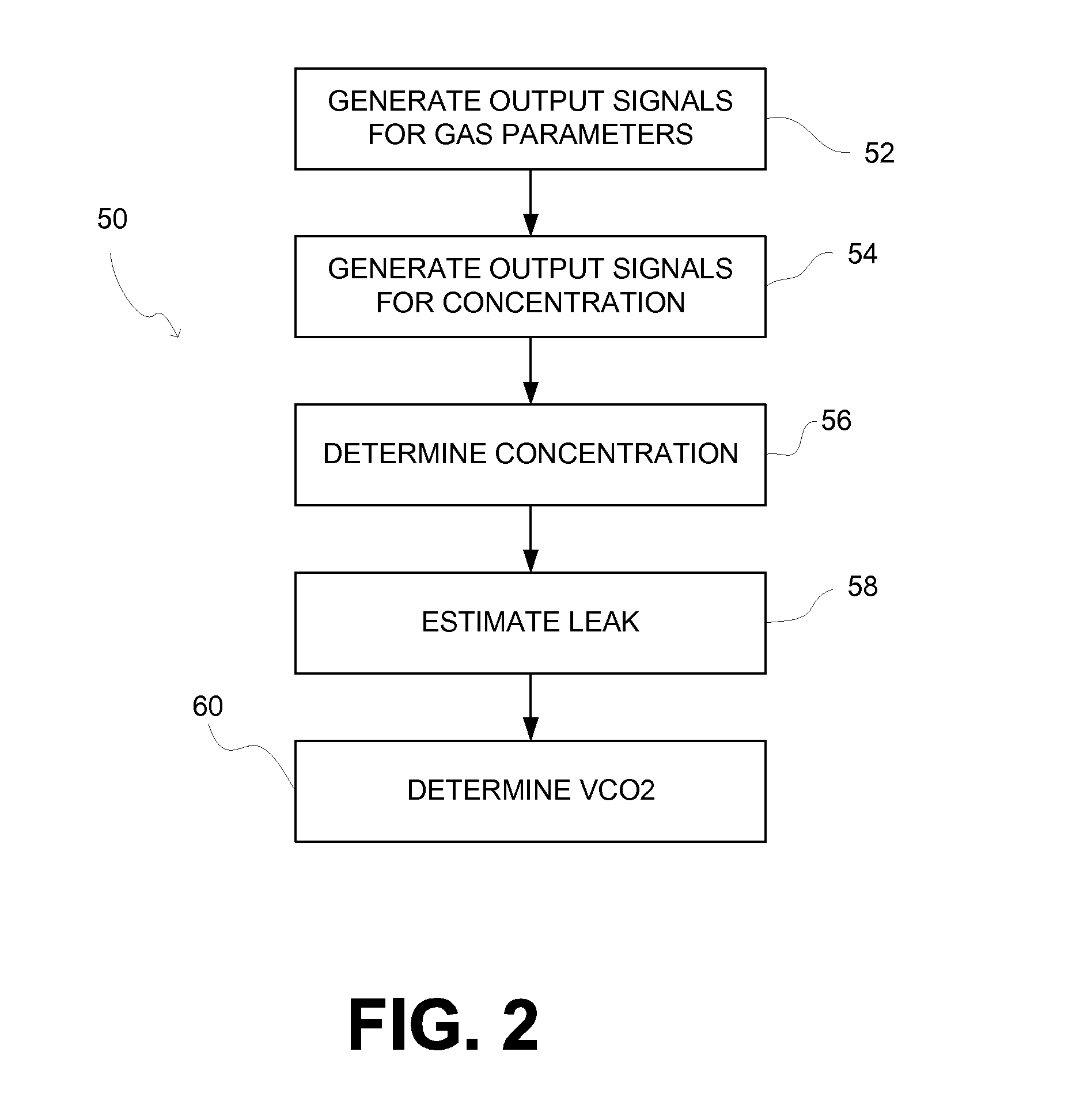
System and method for determining carbon dioxide excreted during non-invasive ventilation
A system is configured to perform capnometry / capnography, and / or other compositional analysis on a non-invasively ventilated subject. As such, the system determines amounts of a molecular species of gas (e.g., carbon dioxide, oxygen, etc.) excreted by the subject on a per-breath basis. Determinations of amounts of the molecular species of gas excreted are adjusted to reflect amounts of the molecular species of gas leaked from the non-invasive interface used to communicate with the airway of the subject.
Owner:KONINKLIJKE PHILIPS ELECTRONICS NV
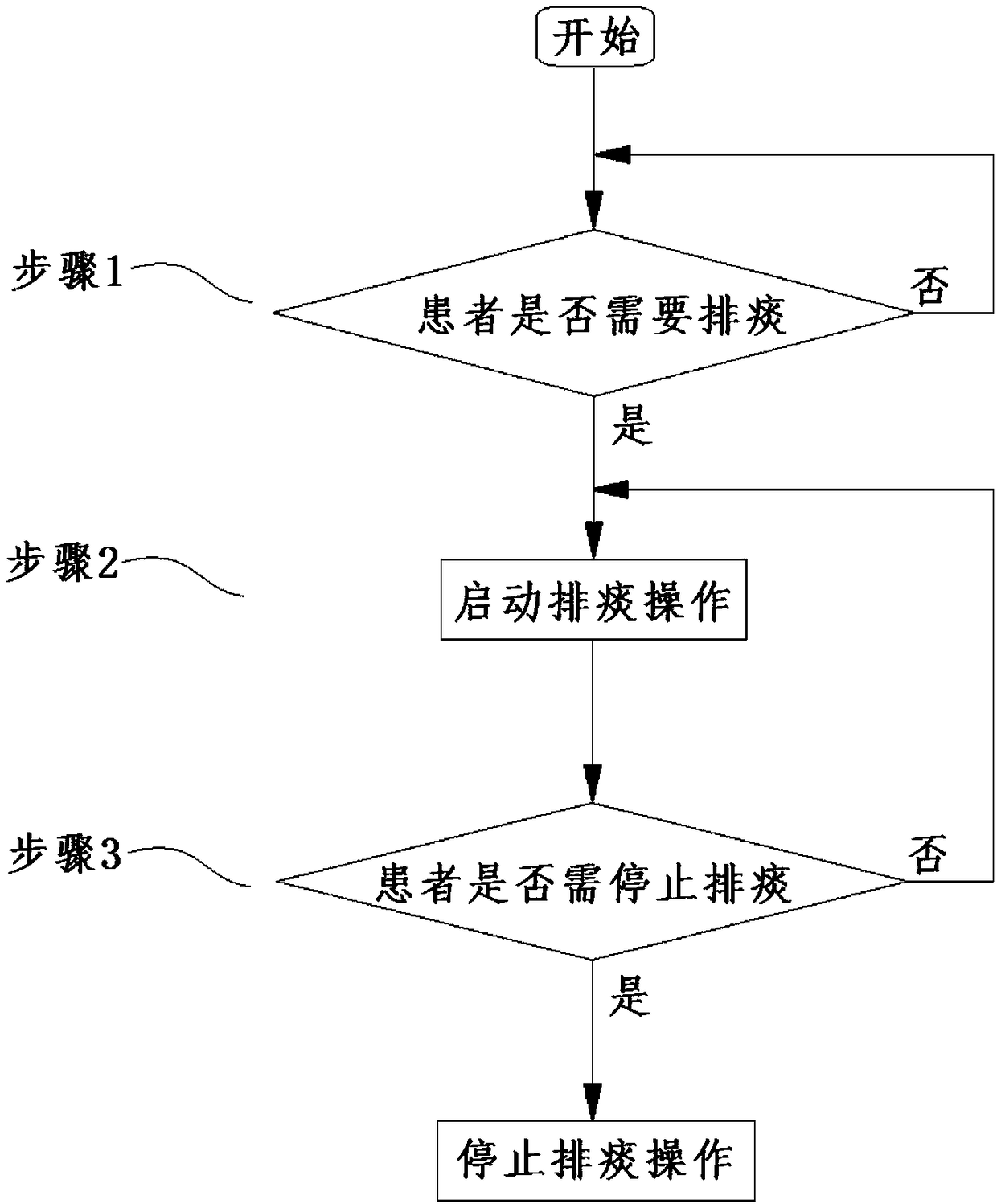
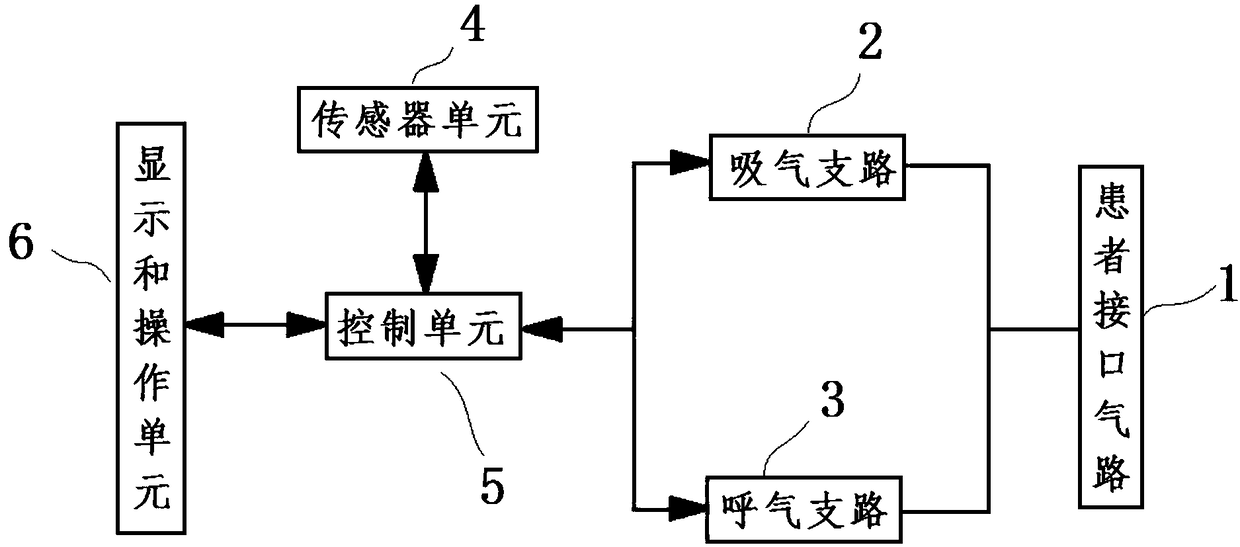
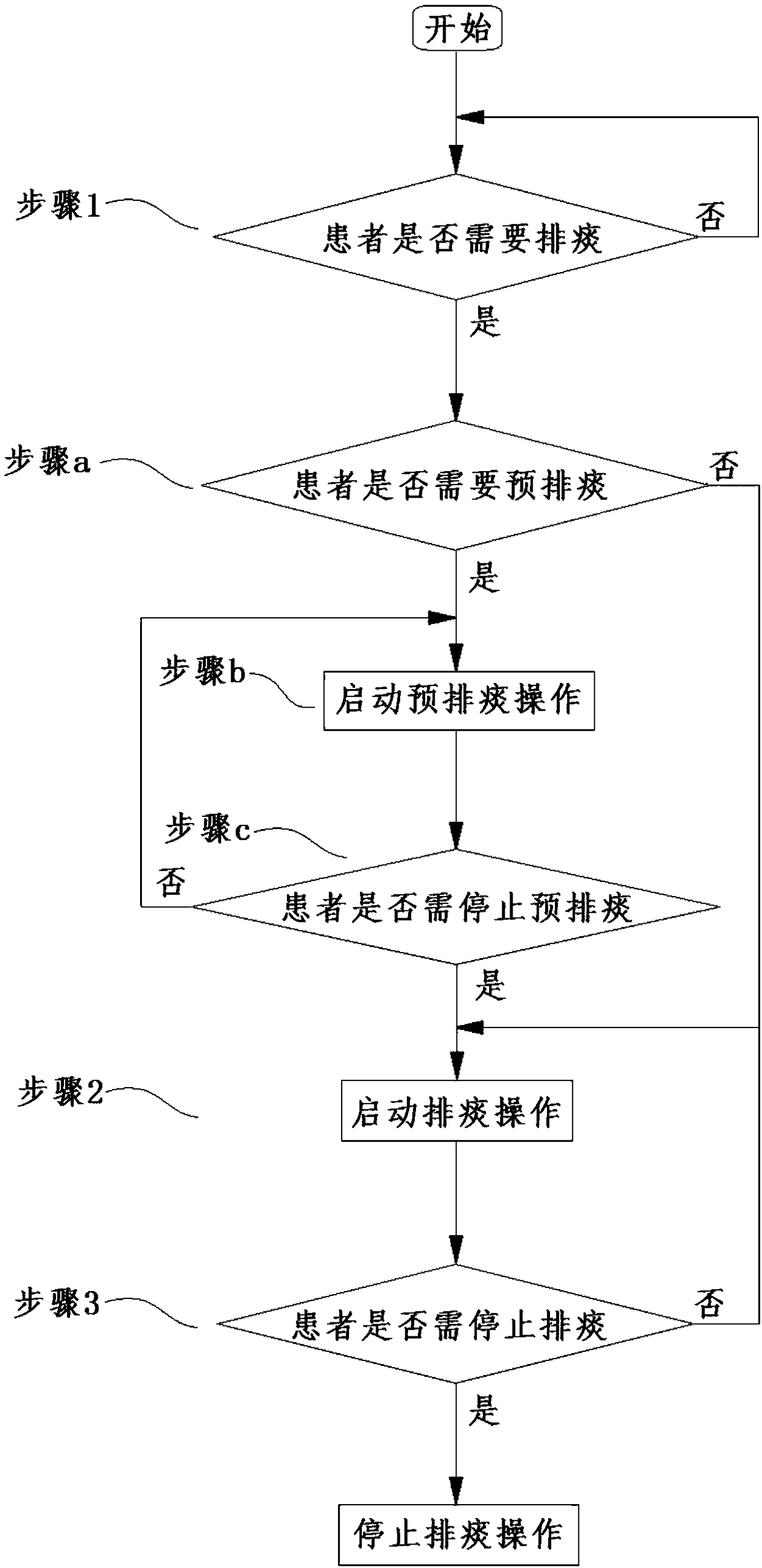
Auxiliary sputum excretion method for non-invasive ventilator and non-invasive ventilator
ActiveCN108543182AReduce in quantityIncrease success rateRespiratorsMechanical/radiation/invasive therapiesPatient needEmergency medicine
The invention relates to the technical field of medical treatment, in particular to an auxiliary sputum excretion method for a non-invasive ventilator and the non-invasive ventilator, and solves the technical problem how to help non-invasive ventilation patients excrete sputum. According to the auxiliary sputum excretion method for the non-invasive ventilator, during the normal mechanical ventilation for the patients by the non-invasive ventilator, after it is determined the patient needs sputum excretion, the sputum excretion operation is started in each respiratory cycle of the patient, andthe sputum excretion operation is not stopped until it is determined that the patient needs to stop sputum excretion. The non-invasive ventilator comprises inspiration and expiration branches, positive and negative pressure air sources, a sensor unit and a control unit, the sensor unit monitors physiological data used for determining whether or not the patient needs sputum excretion and needs to stop sputum excretion, the control unit analyzes the physiological data monitored by the sensor unit to determine whether or not the patient needs sputum excretion and needs to stop sputum excretion, after it is determined that the patient needs sputum excretion, the positive and negative pressure air sources are controlled to perform the sputum excretion operation, and the sputum excretion operation is not stopped until it is determined that the patient needs to stop sputum excretion.
Owner:YAGUO
Apparatus and methods for providing humidity in respiratory therapy
ActiveUS20120080032A1RespiratorsBreathing filtersBi-level positive airway pressure therapyPositive airway pressure
The present inventions provide respiratory therapy apparatus that introduce water into the pressurized air delivered to a user during various positive airway pressure therapies and corresponding methods. The respiratory therapy apparatus may be configured to administer one or more positive airway pressure therapies, including: continuous positive airway pressure therapy (CPAP), bi-level positive airway pressure therapy (BPAP), auto positive airway pressure therapy (autoPAP), proportional positive airway pressure therapy (PPAP), and / or other positive airway pressure therapies. The respiratory therapy apparatus may include a user interface that defines an interface passage to communicate pressurized air to the user for inhalation and a humidifier that introduces water into the pressurized air generally at the interface passage. Methods according to the present inventions may include introducing water into the interface passage at one or more humidifier ports disposed about the interface passage.
Owner:SOMNETICS INT INC
Apparatus and methods for providing humidity in respiratory therapy
ActiveUS8074645B2RespiratorsLighting and heating apparatusBi-level positive airway pressure therapyPositive airway pressure
The present inventions provide respiratory therapy apparatus that introduce water into the pressurized air delivered to a user during various positive airway pressure therapies and corresponding methods. The respiratory therapy apparatus may be configured to administer one or more positive airway pressure therapies, including: continuous positive airway pressure therapy (CPAP), bi-level positive airway pressure therapy (BPAP), auto positive airway pressure therapy (autoPAP), proportional positive airway pressure therapy (PPAP), and / or other positive airway pressure therapies. The respiratory therapy apparatus may include a user interface that defines an interface passage to communicate pressurized air to the user for inhalation and a humidifier that introduces water into the pressurized air generally at the interface passage. Methods according to the present inventions may include introducing water into the interface passage at one or more humidifier ports disposed about the interface passage.
Owner:SOMNETICS INT INC
Method and system to detect respiratory asynchrony
Owner:RESPIVAR LLC
Apparatus and method for adaptive ramped control of positive airway pressure (PAP)
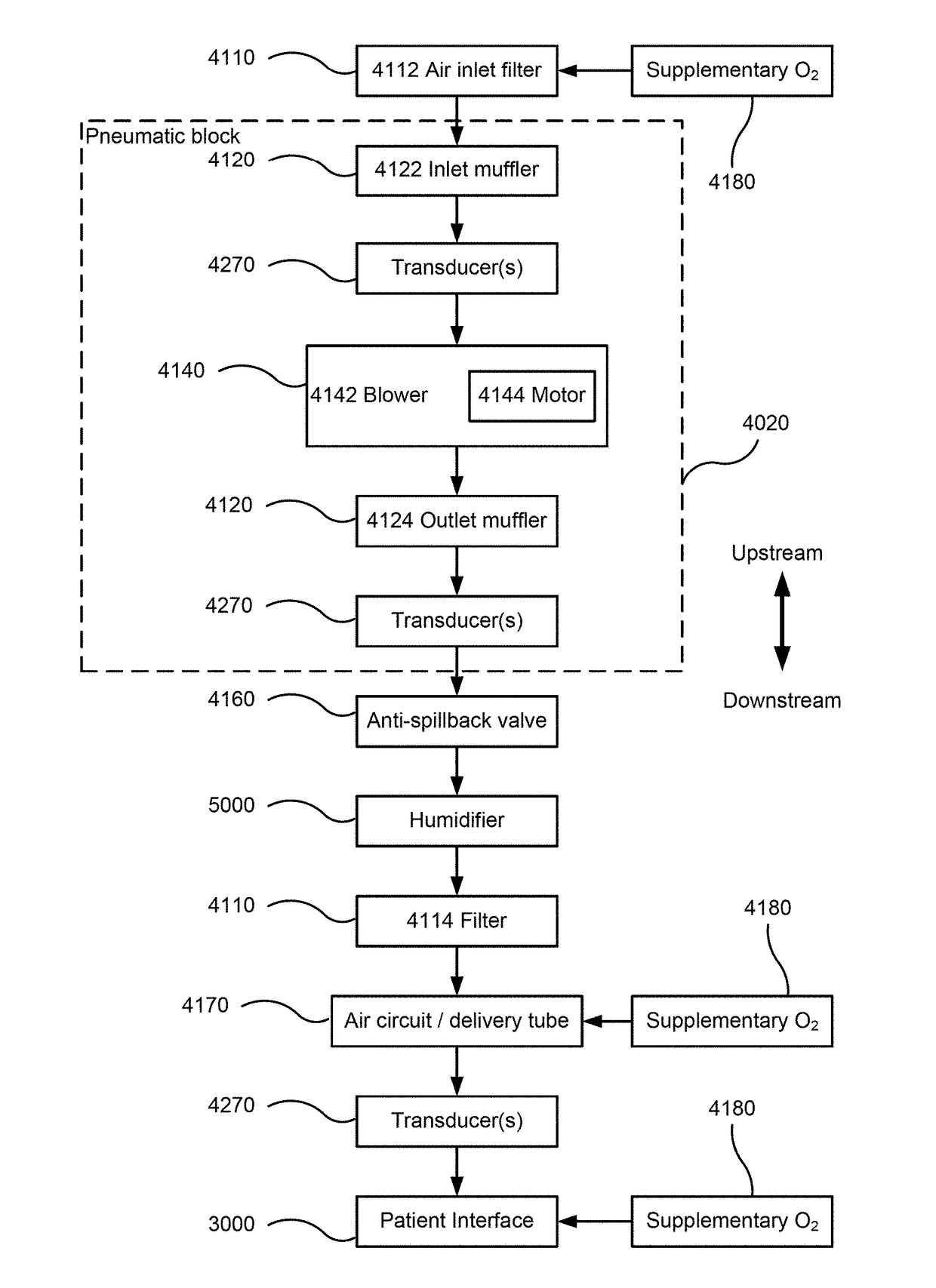
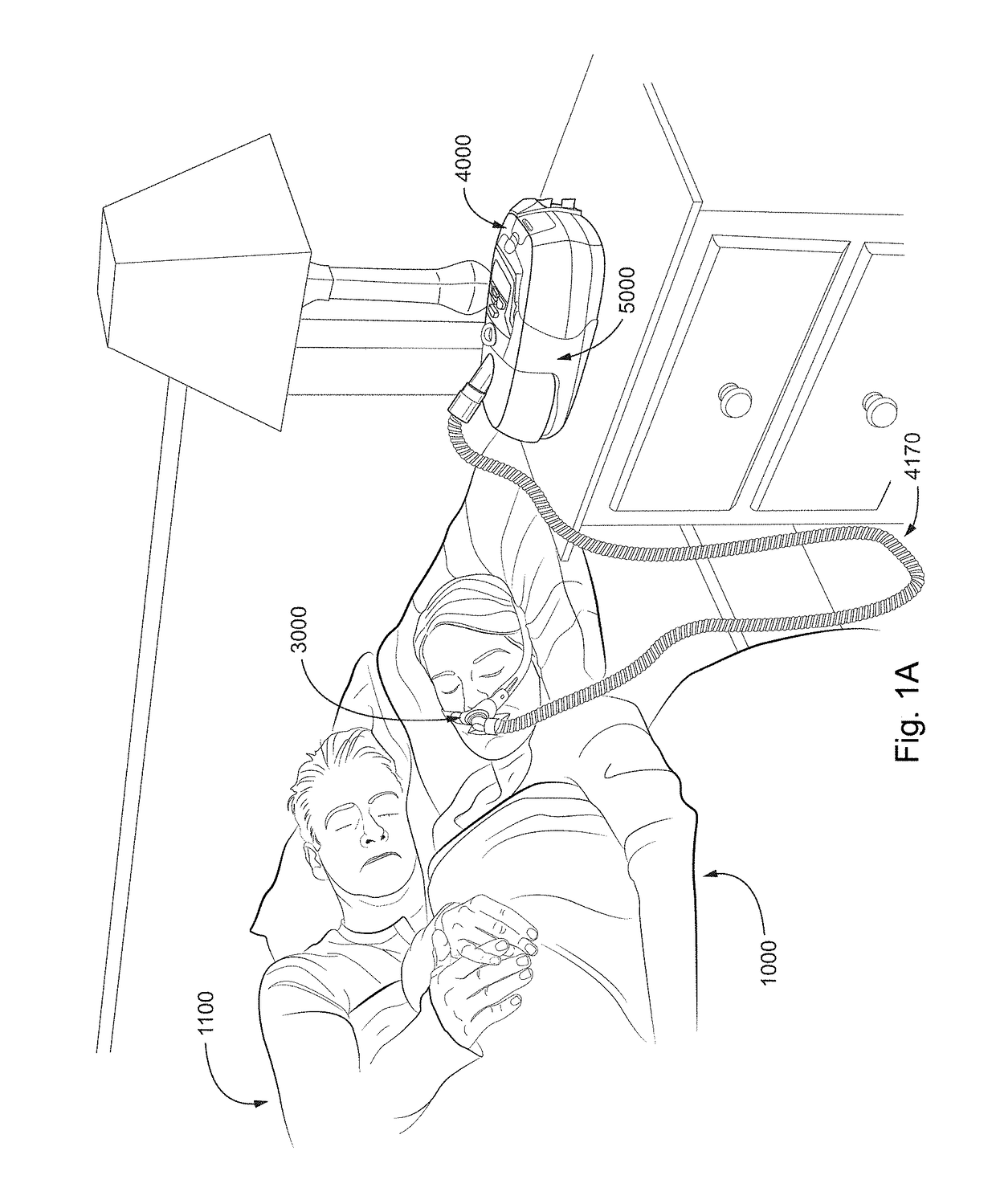
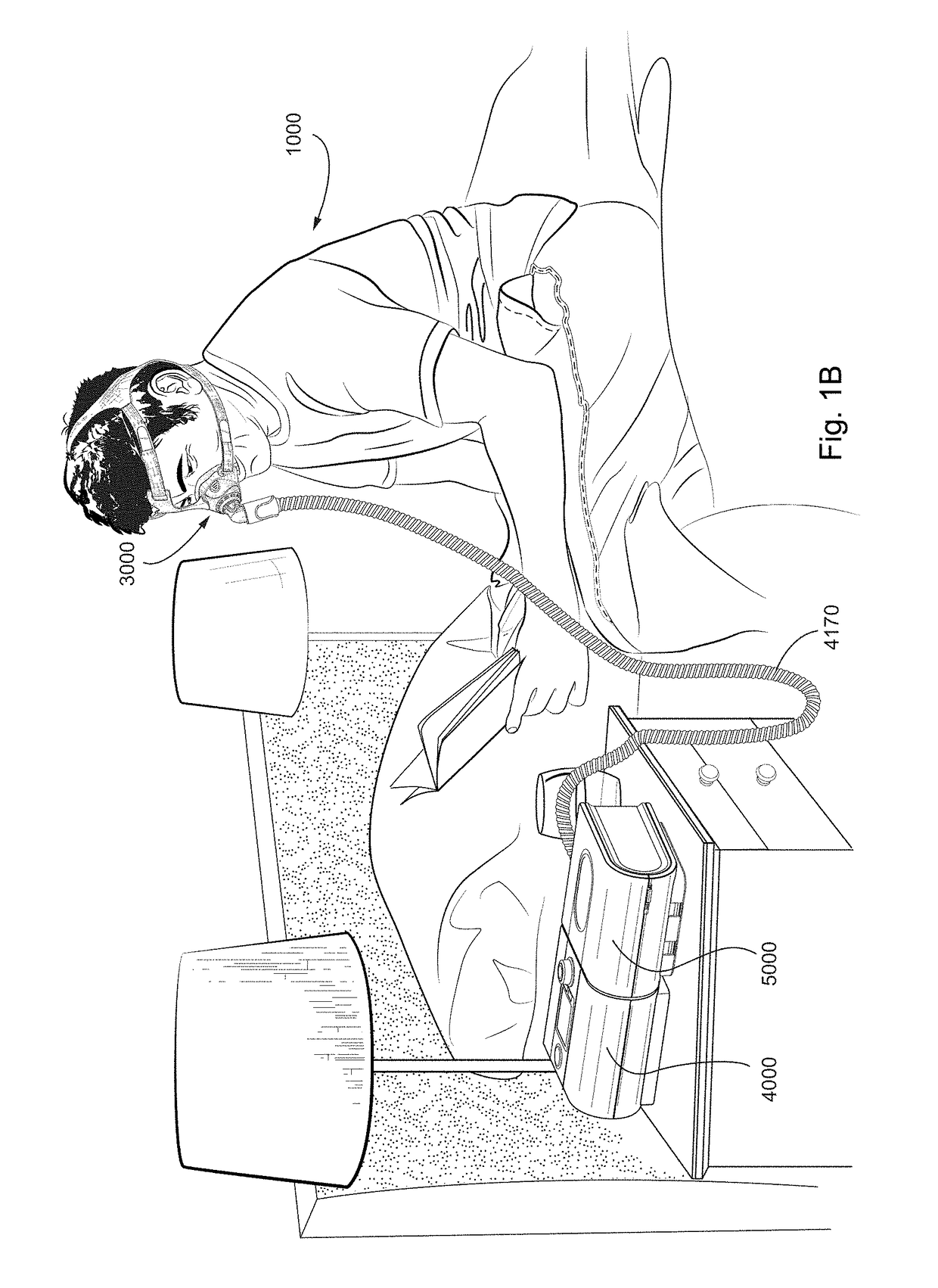
ActiveUS20180071471A1Improve comfortIncrease costRespiratorsMedical devicesSleep disordered breathingSleep disorder breathing
Methods and / or apparatus automate setting of a pressure ramp to permit pressure to gradually arrive at a treatment pressure such as in the initial or pre-sleep stages of use of a respiratory therapy pressure device for treatment of a respiratory disorder during sleep (e.g., sleep disordered breathing). In an example, apparatus for treating a respiratory disorder may include a breathable gas pressure generating device. The apparatus may include a controller, including a processor(s). The controller may be configured to collect historic sleep onset parameter(s) concerning timing of a patient falling asleep. The apparatus may determine, based on the historic sleep onset parameter(s), a pre-sleep limit. The apparatus may determine a pre-sleep profile of pressure versus time having a duration spanning the pre-sleep limit and having a plurality of ramping sub-therapeutic pressures. The apparatus may control, upon initiation of treatment, setting of the pressure generating device according to the pre-sleep profile.
Owner:RESMED LTD
Methods, systems and devices for non-invasive ventilation including a non-sealing ventilation interface with a free space nozzle feature
A system for supplying ventilatory support may include a nasal interface configured to communicate with a patient's nose while allowing the patient to breathe ambient air directly without flowing through the nasal interface. A nozzle may be associated with the nasal interface at a distance from a nose. The nozzle may be connectable to the gas delivery circuit and the gas delivery source. The nozzle may be capable of delivering gas into the nasal passage by creating negative pressure area near the nozzle and a positive pressure area near the entrance to the nose. A combination of gas from the gas delivery source and air entrained from the gas exiting the nozzle may provide ventilatory support.
Owner:BREATHE TECHNOLOGIES INC
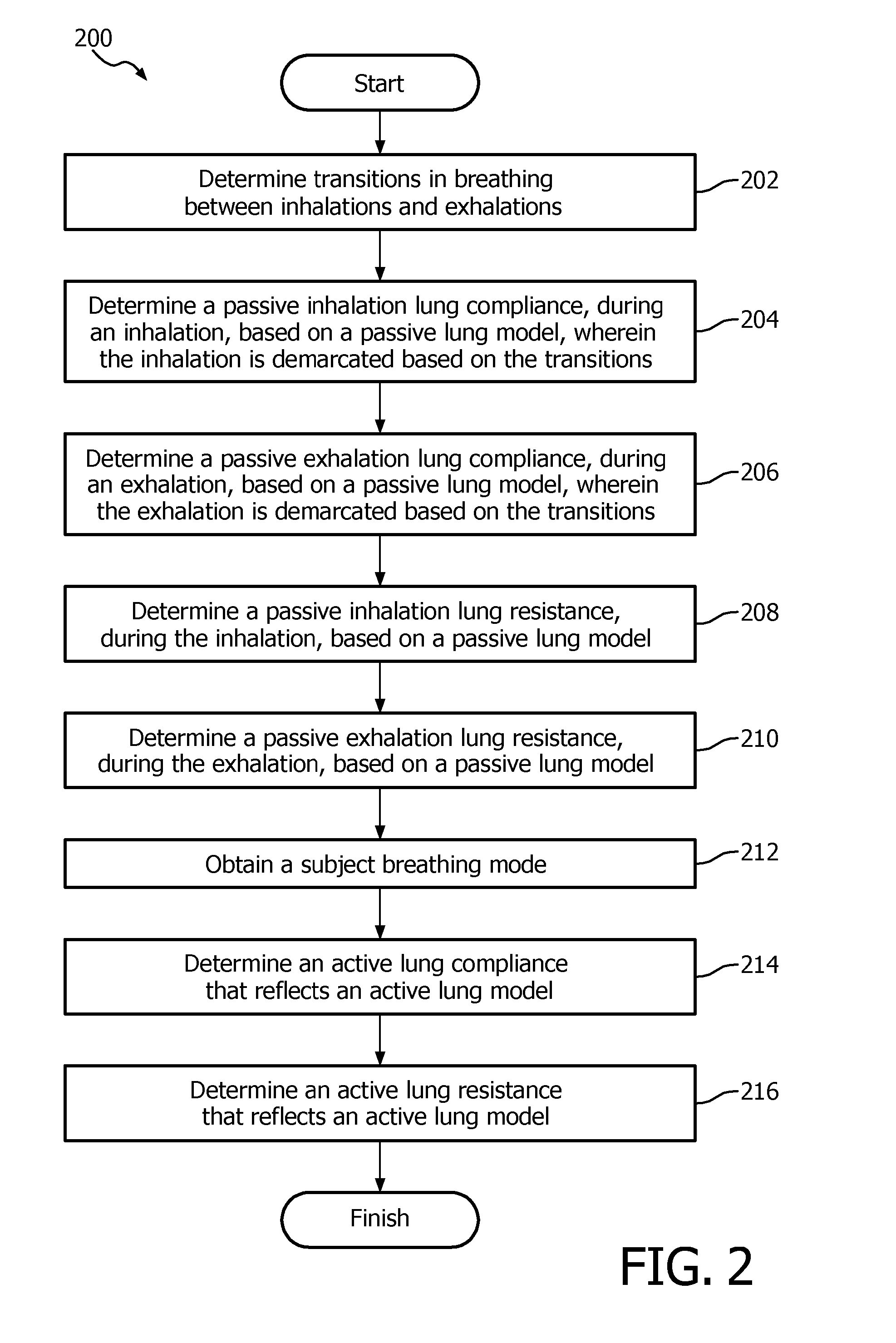
Non-invasive ventilation measurement
Determining the lung compliance and lung resistance of a subject undergoing respiratory therapy using non-invasive ventilation requires taking the presence of leaks into account. In particular, variable and unintentional leaks at or near a subject interface appliance may be dynamically determined based on an average resistance of the leak orifice of the subject.
Owner:KONINKLIJKE PHILIPS ELECTRONICS NV
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com