System for management and documentation of health care decisions
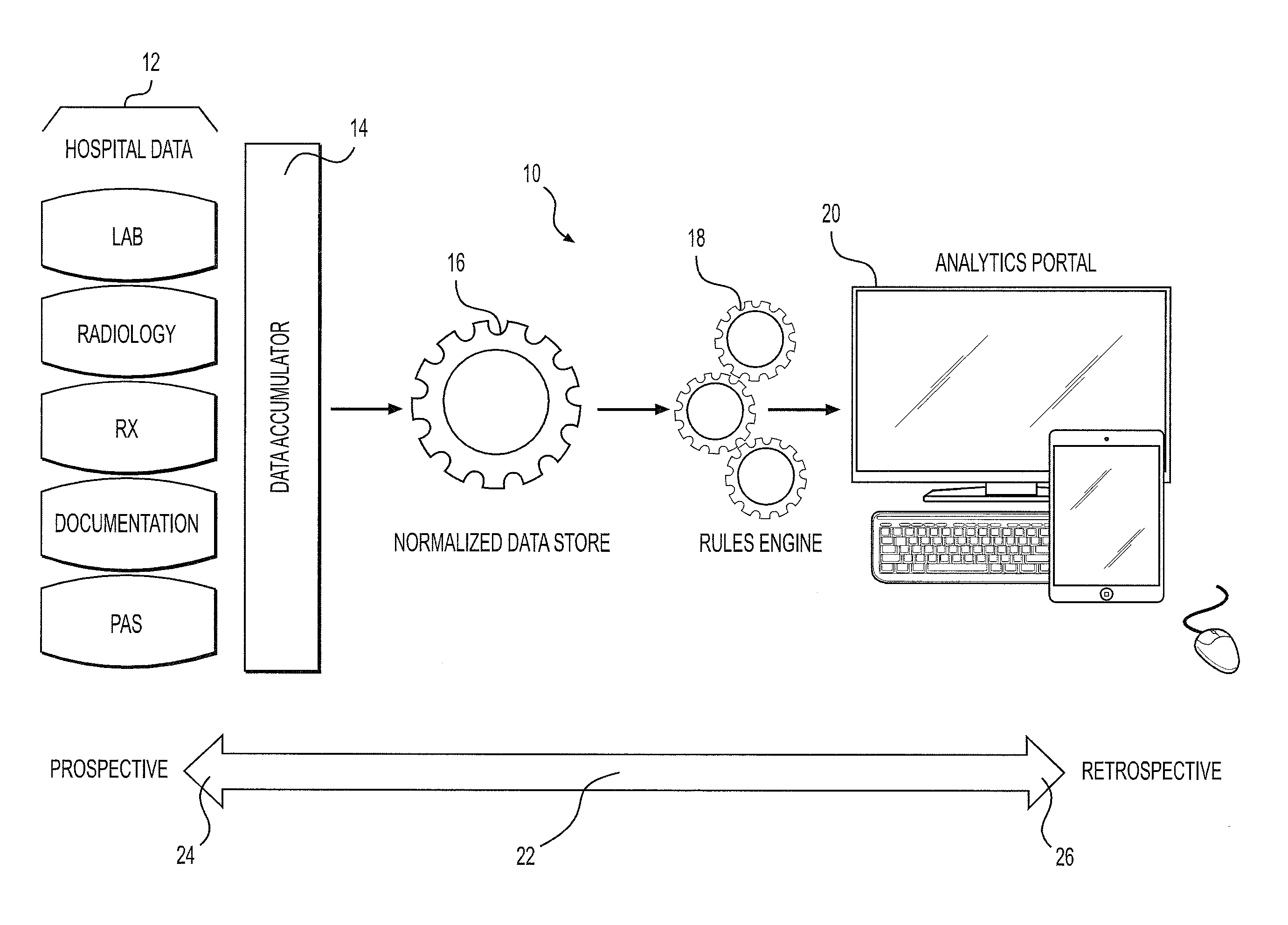
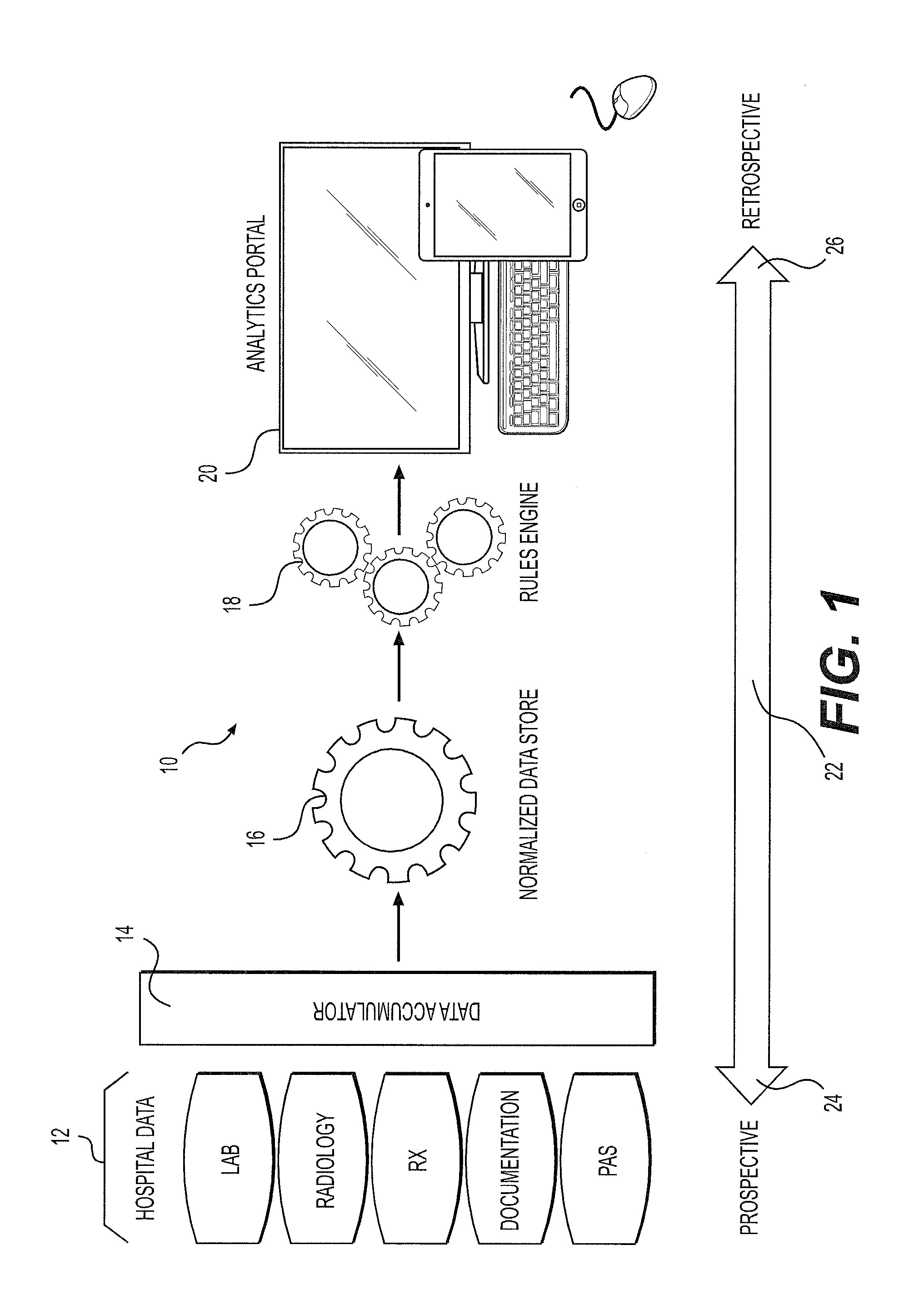
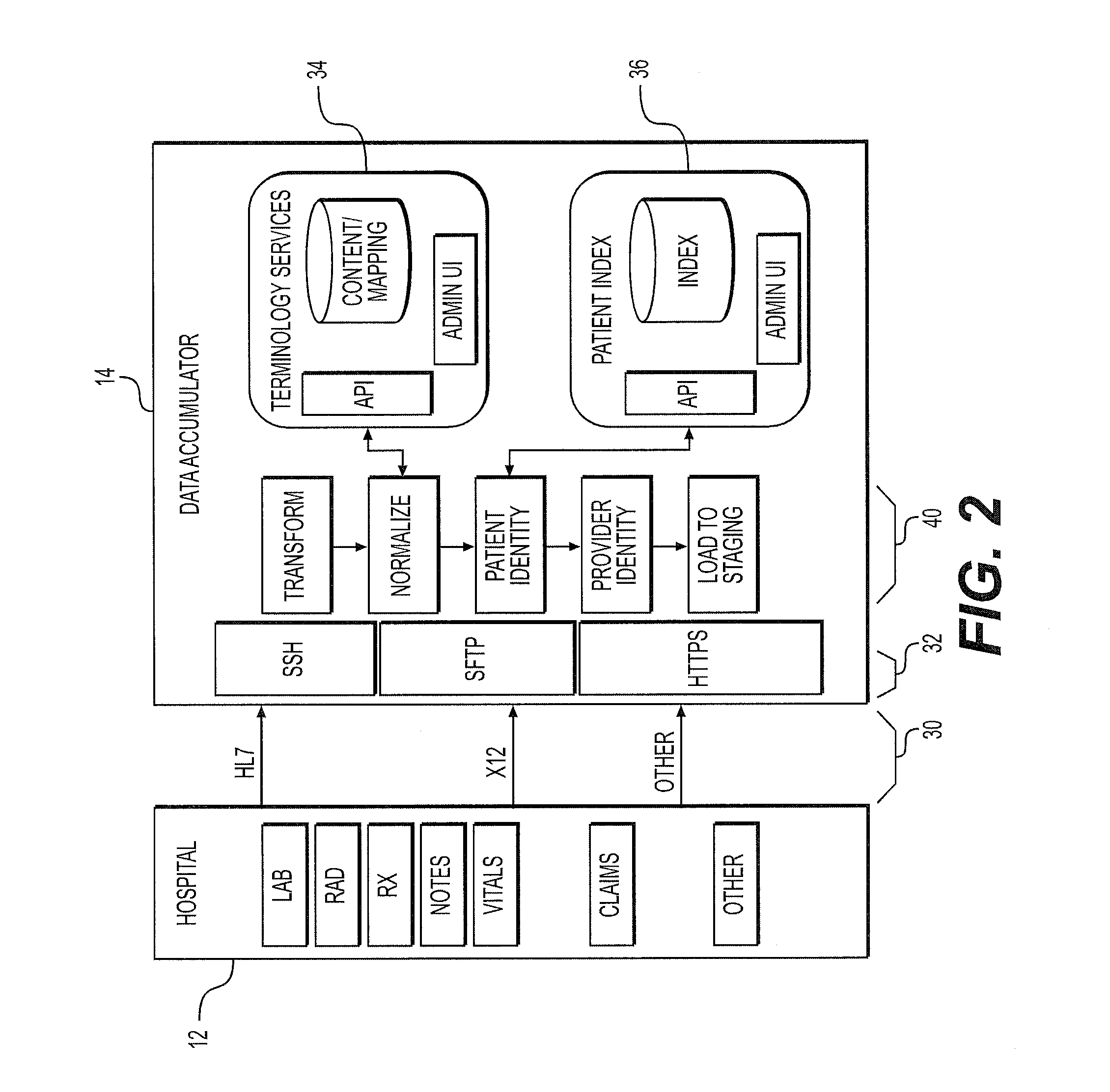
a health care decision and decision-making technology, applied in the field of health care decision-making system, can solve the problems of providers lack the ability to accurately document decisions, and lose billions of dollars annually owing to unreimbursed or under-reimbursed services
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Provider Use, Prospective Application
[0079]Determination of Patient Status
Step 1—Assessment
[0080]Patient presents to the Emergency Room with signs of Pneumonia. Via the tool, the end user reviews the patient dashboard to determine the general health of the patient (wellness score) and that initial labs (i.e. WBC, Troponin, Lactic Acid) and vitals (i.e. Heart Rate, Blood Pressure, Temperature) are within normal ranges (acuity score). For example, if the wellness score presented as Good (green) and the acuity score presented as Low (green), the end user could assume the patient was in relatively good condition.
Step 2—Level of Care Determination
[0081]Next, the end user would use the care level score (CLS) score to guide them in their evaluation of appropriate patient status. For example, if the CLS was less than 70, the end user could rationally place the patient in an appropriate observation status. Conversely, if the CLS measured greater than 70, the end user could assume the patient...
example 2
Provider / Payer, Use Retrospective Application
[0084]Denial Response / Appeal Review
[0085]In today's environment, the review of a denied claim for medical necessity by a provider and the review of the corresponding appeal by a payer is largely a manual process. Key components for both entities in the review process is 1) Severity of Illness (SOI); 2) Intensity of Services (IS) and 3) Does the patient require Hospital Based Care. Currently, the hospital clinician and the payer auditor must review clinical information—likely a printed medical record ranging anywhere from 50 to 500+ pages depending on the complexity of the case to make their determinations. Via the tool, this review process is streamlined as follows:
Step 1—Accessing Scoring Outputs
[0086]Via the tool, the clinician (hospital) and auditor (payer) access the patient dashboard to evaluate the key components listed above (SOI, IO and Hospital Based Care requirements). These components are displayed on the dashboard as wellness,...
example 3
Payer Use, Prospective Application—Authorization for Services
[0089]In today's environment, the process of obtaining and granting authorization for services is largely a manual, paper intensive, iterative and time consuming process. Typically a list of patients requiring authorization is faxed to the payer on a daily basis along with documentation to support the request. Often, there is discrepancy between what services the Provider requests and what the Payer will approve. In these cases, additional documentation is faxed and the case is escalated to the Provider's Attending Physician and the Payer's Utilization Management Physician (peer to peer review). Today, a platform does not exist to minimize the exchange of paper documentation, to manage the communication between the payer and provider and to facilitate decision making based on objective, data driven criteria. The tool provides this platform.
Step 1—Request for Authorization
[0090]Via the too, analytics portal and specifically...
PUM
| Property | Measurement | Unit |
|---|---|---|
| time | aaaaa | aaaaa |
| clinical strength | aaaaa | aaaaa |
| financial strength | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com