Axial spinal implant and method and apparatus for implanting an axial spinal implant within the vertebrae of the spine
a spinal implant and axial technology, applied in the field of spinal implants, can solve the problems of high failure rate of fusion procedure, neurologic deficit in nerve function, and usually extreme pain
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
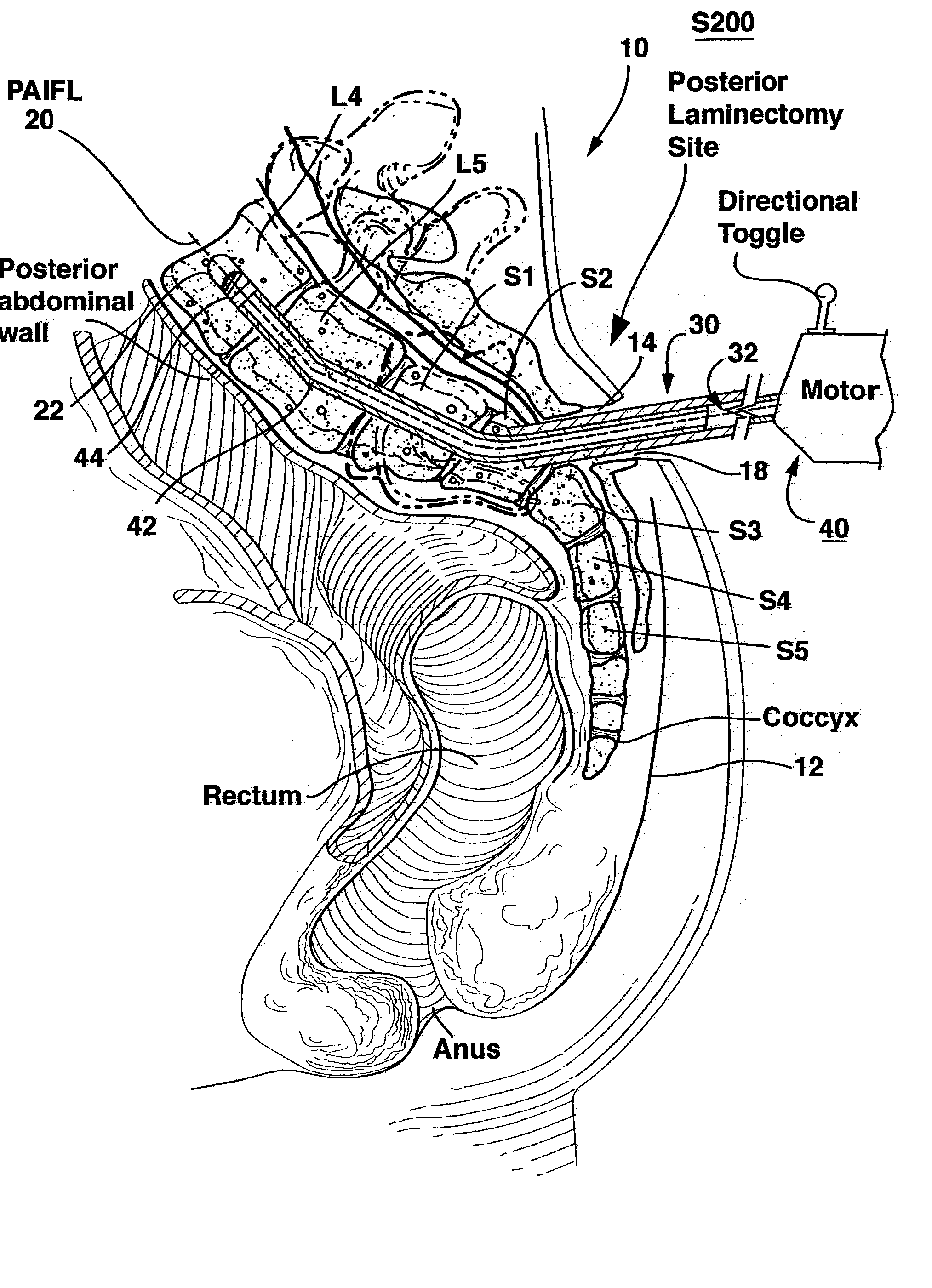
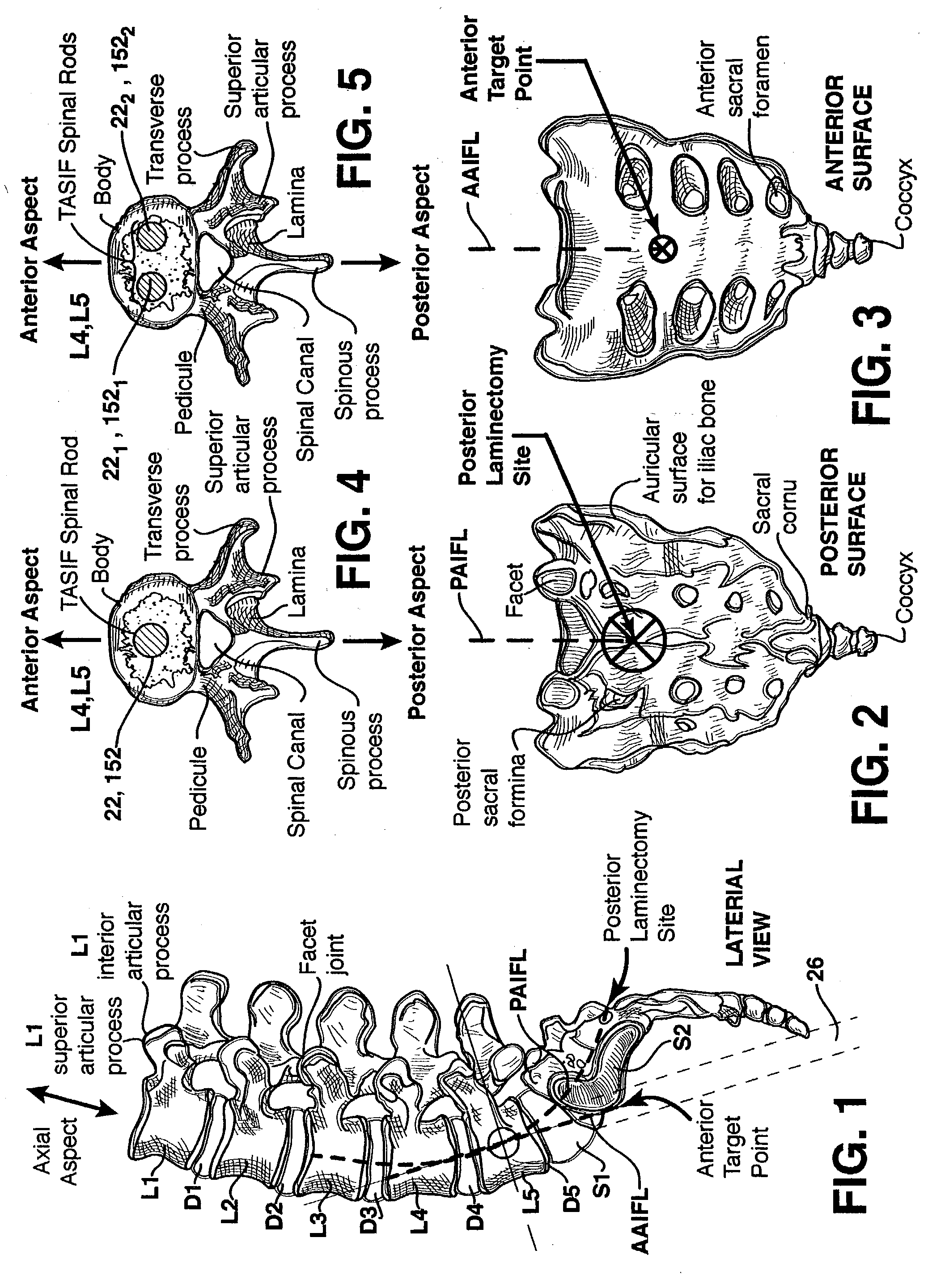
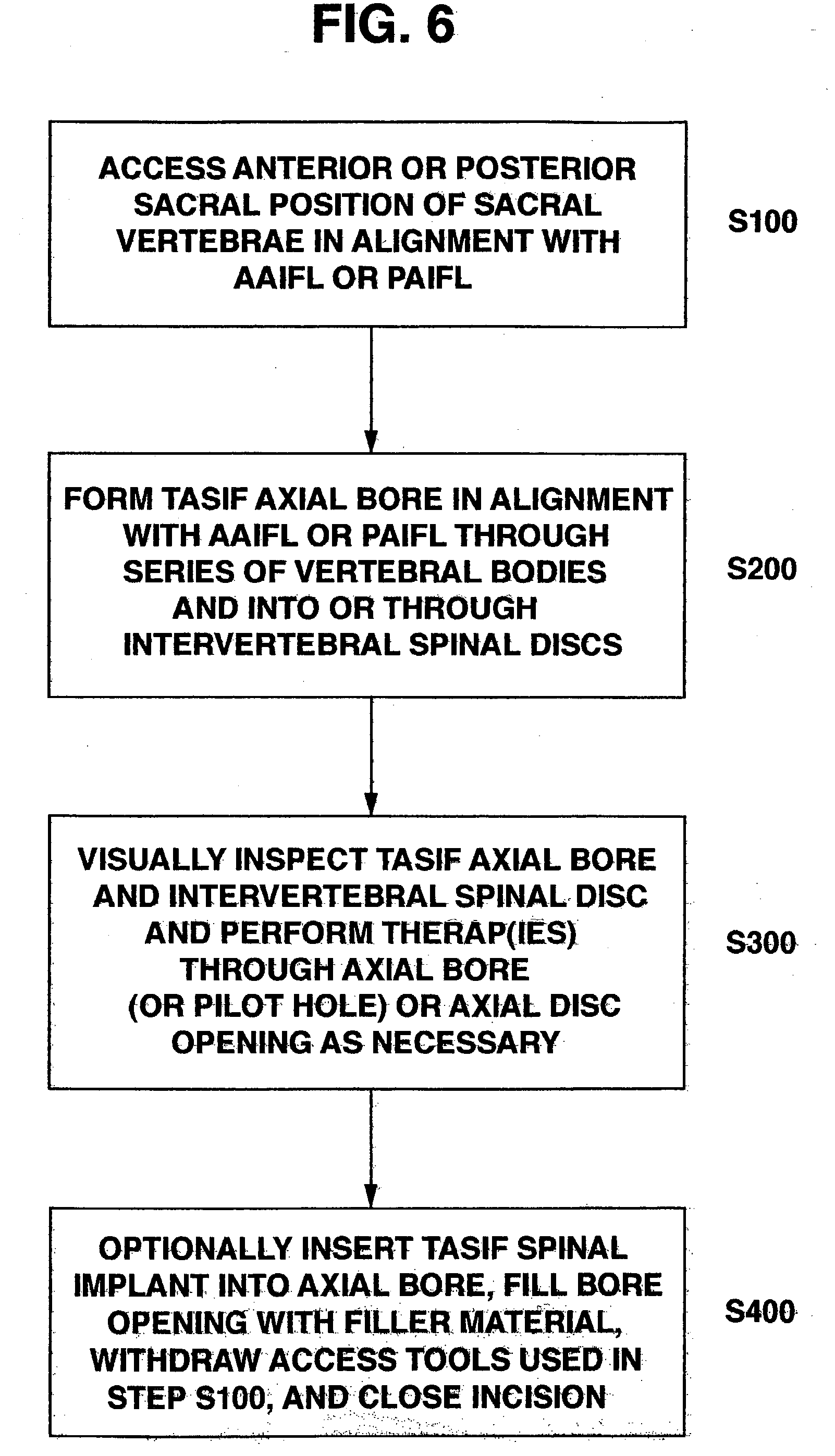
[0059] The methods and surgical instrumentation and spinal implants disclosed in the above-referenced provisional application No. 60 / 182,748 and in co-pending, commonly assigned application Ser. No. 09 / 640,222 filed Aug. 16, 2000, for METHOD AND APPARATUS FOR PROVIDING POSTERIOR OR ANTERIOR TRANS-SACRAL ACCESS TO SPINAL VERTEBRAE can be employed in the practice of the present invention. The '222 application discloses a number of related TASIF methods and surgical tool sets for providing posterior and anterior trans-sacral access to a series of adjacent vertebrae located within a human lumbar and sacral spine having an anterior aspect, a posterior aspect and an axial aspect, the vertebrae separated by intact or damaged spinal discs. Certain of the tools are selectively employed to form a percutaneous (i.e., through the skin) pathway from an anterior or posterior skin incision to a respective anterior or posterior position, e.g., a target point of a sacral surface or the cephalad end ...
PUM
| Property | Measurement | Unit |
|---|---|---|
| Temperature | aaaaa | aaaaa |
| Length | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com