Intravascular blood filters and methods of use
a technology of blood filter and filter plate, which is applied in the field of intravascular blood filter, can solve the problems of tissue ischemia (lack of oxygen and nutrients), morbidity and mortality, stroke, and even death, and achieve the effect of avoiding or minimizing thromboembolic disorders and increasing the level of particulate protection
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
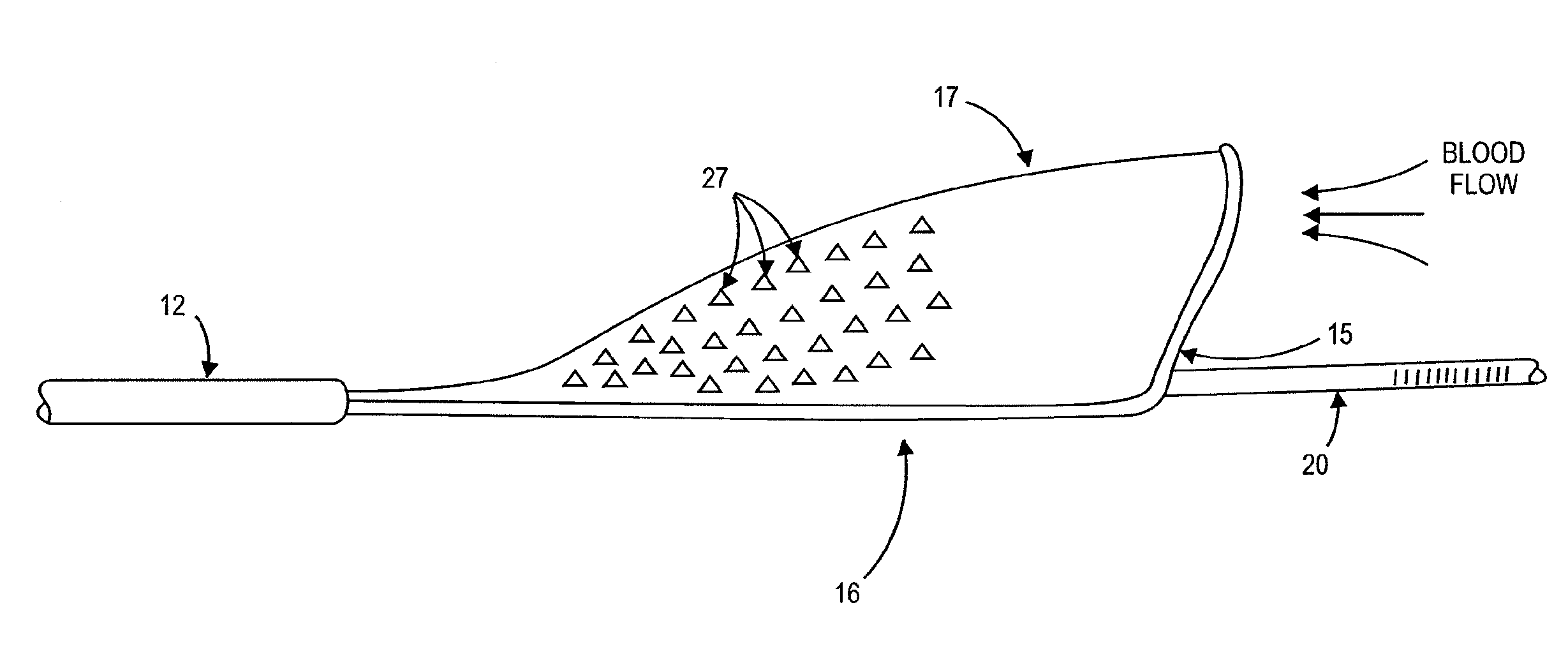
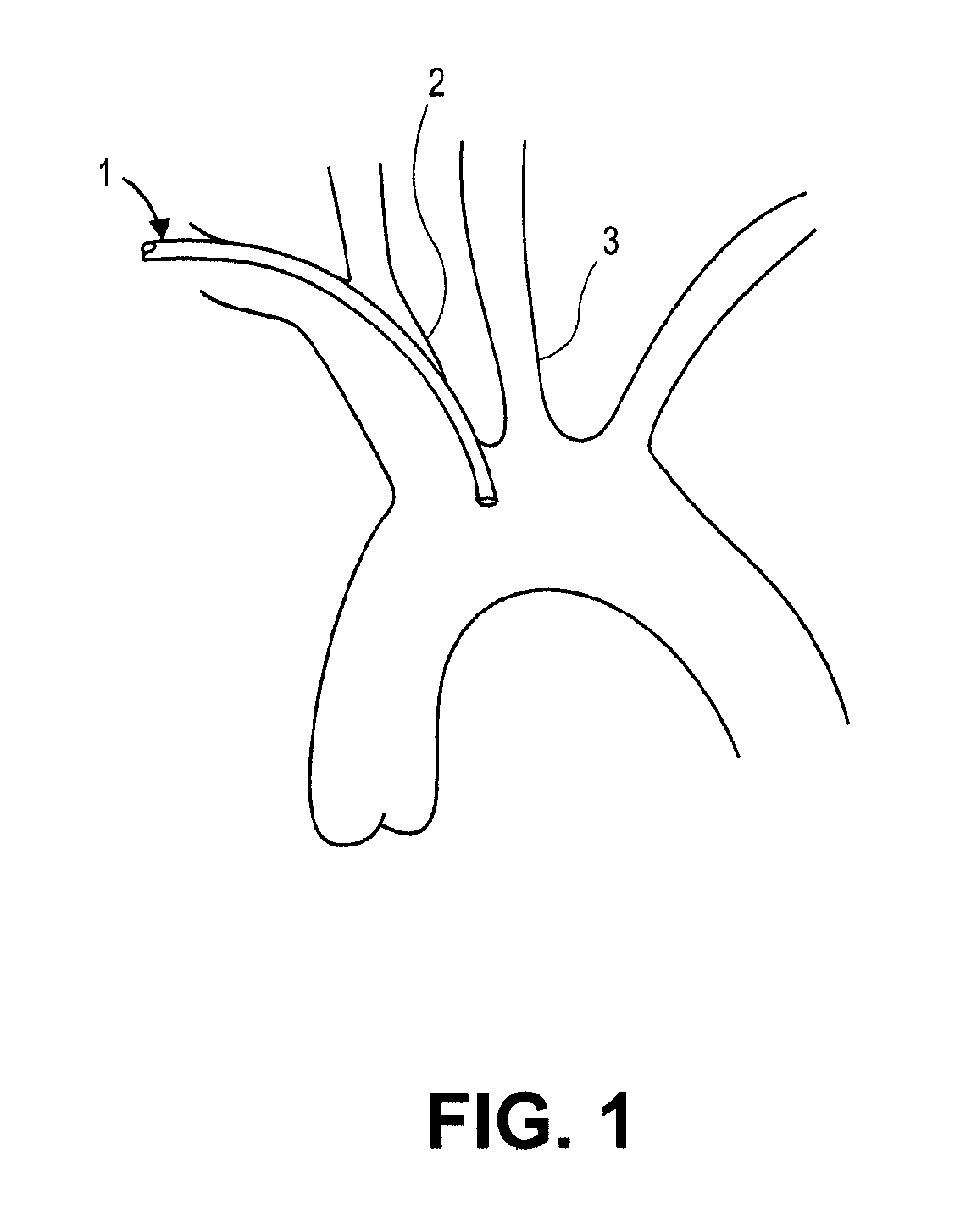
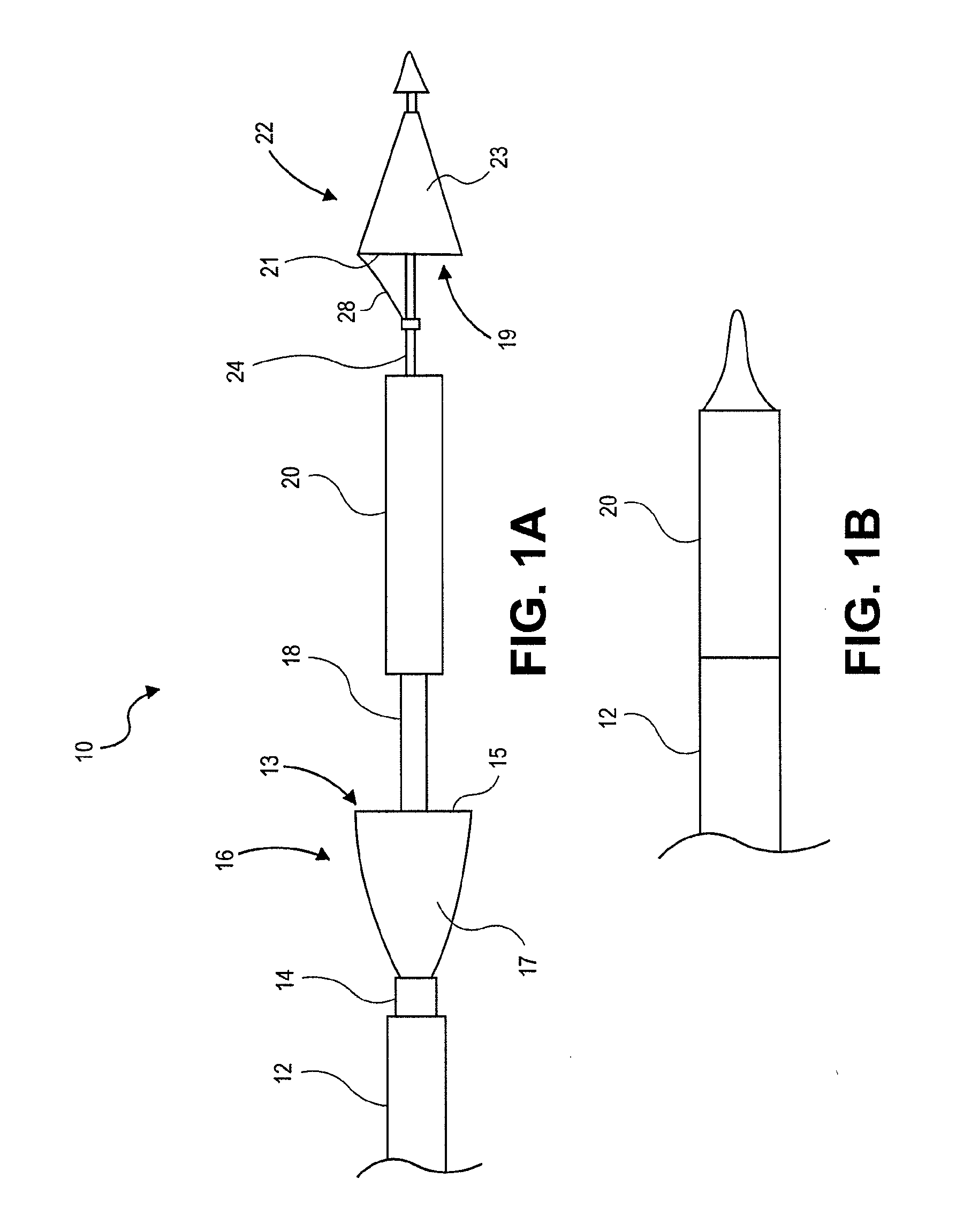
[0052]The disclosure relates generally to intravascular blood filters used to capture foreign particles. In some embodiments the blood filter is a dual-filter system to trap foreign bodies to prevent them from traveling into the subject's right and left common carotid arteries. The filter systems described herein can, however, be used to trap particles in other blood vessels within a subject, and they can also be used outside of the vasculature. The systems described herein are generally adapted to be delivered percutaneously to a target location within a subject, but they can be delivered in any suitable way, and need not be limited to minimally-invasive procedures.
[0053]In one application, the filter systems described herein are used to protect the cerebral vasculature against embolisms and other foreign bodies entering the bloodstream during a cardiac valve replacement or repair procedure. To protect both the right common carotid artery and the left common carotid artery during s...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com