Personalized cancer vaccines and adoptive immune cell therapies
A cancer vaccine and cancer cell technology, applied in biochemical equipment and methods, cancer antigen components, medical raw materials derived from mammals, etc.
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
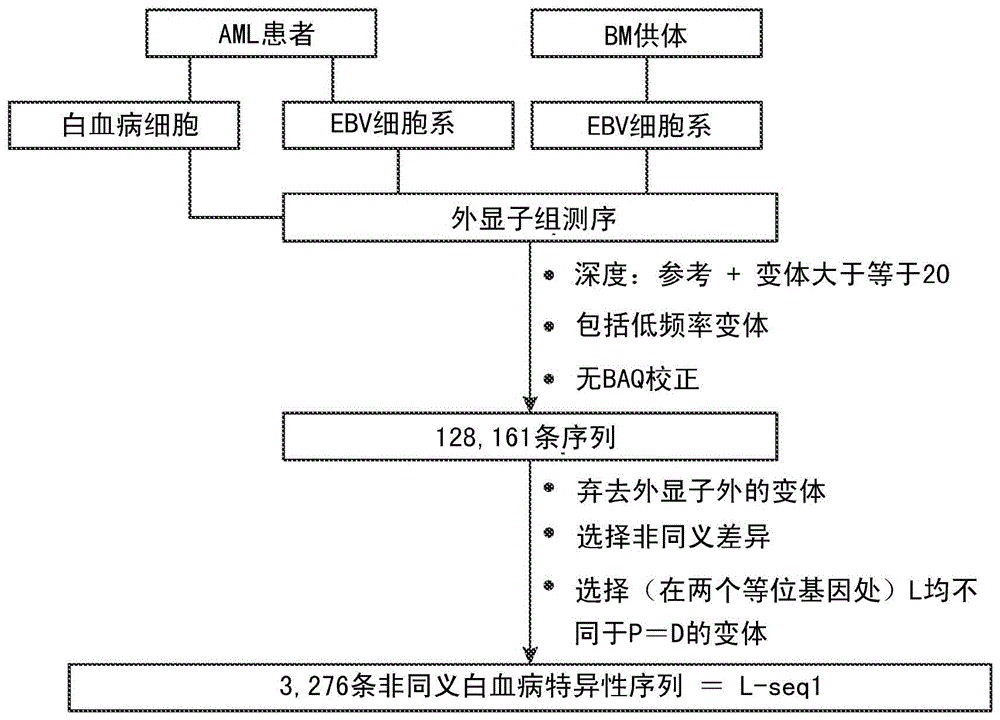
[0103] Example 1: Identification of cancer mutations from exome and transcriptome libraries using NGS
[0104] Figure 1a–c shows a schematic for identifying mutations in cancer cells that can be targeted for immune recognition. Leukemic cells (L) and Epstein-Barr virus transformed B cells (patient EBV cell line) (P) were obtained from patient #1 prior to hematopoietic stem cell transplantation (HSCT). Leukemic cells were isolated from blood (22, 27) and EBV cells were prepared using previously published methods (see, eg, Caputo JL et al., J. Tissue Culture Methods 13:39-44, 1991). EBV cell lines were similarly produced from bone marrow donors (D). Freeze cells in liquid nitrogen.
[0105] DNA exome preparation using NGS methods from Patient #1 Leukemia Cells, Patient #1 EBV Cell Line, and Donor EBV Cell Line under contract with Expression Analysis, Inc., Durham, NC library. RNA transcriptome libraries were prepared by Expression Analysis Inc. using patient leukemia cells...
Embodiment 2
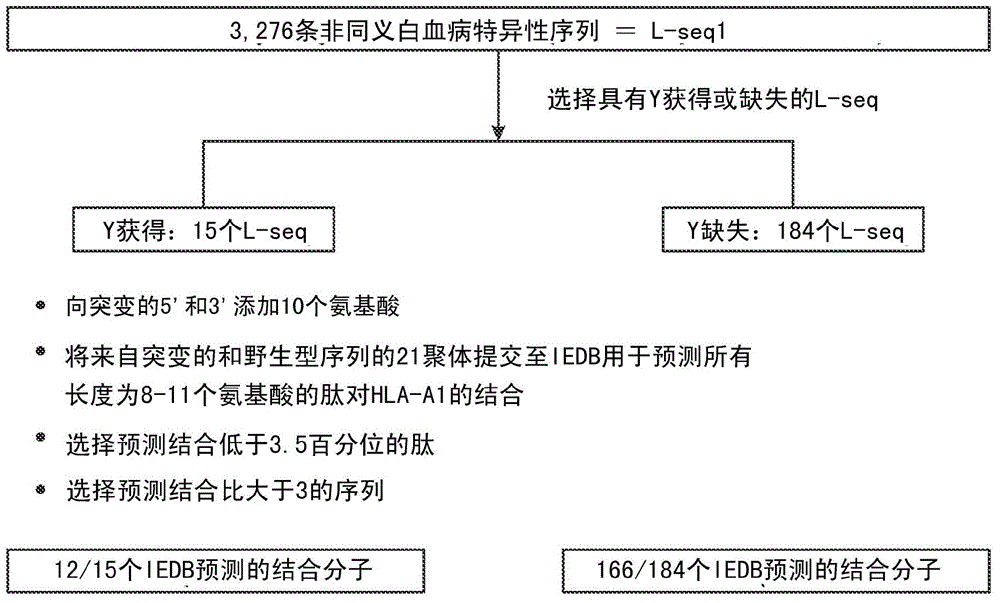
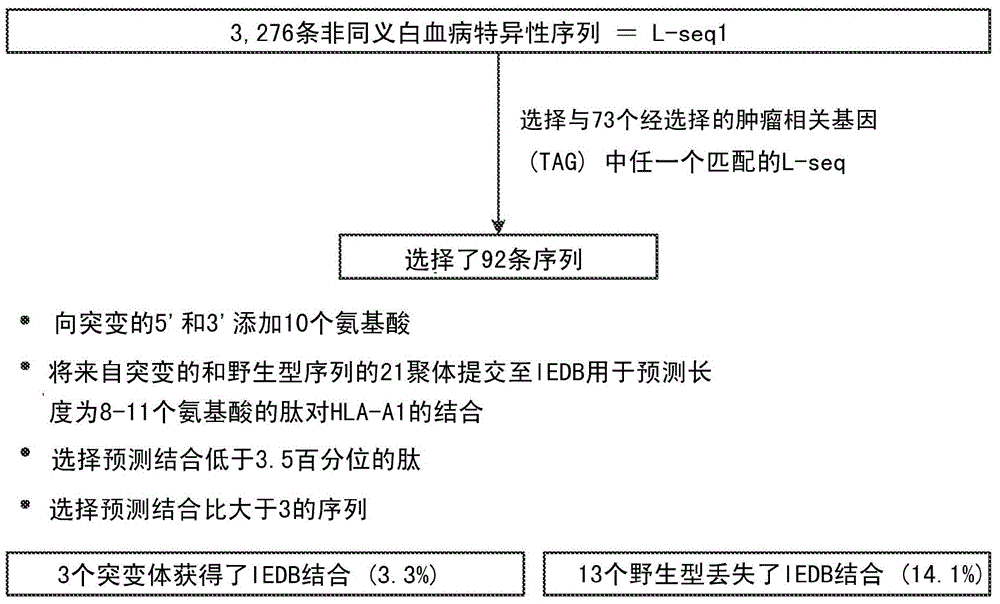
[0118] Example 2: Selection of cancer-specific mutations with potential HLA-binding motifs
[0119] Further selections were performed on the mutation sets from L-seq1 and Lseq2 to identify smaller subgroups with the potential to bind cancer patient HLA antigens. To this end, each L-seq was assessed for mutations involving tyrosine gains or losses. For L-seq1, there were 15 sequences with tyrosine gains and 184 sequences with tyrosine deletions (Fig. 1b). Of the 127 sequences in L-seq2 from cancer cell expressed genes, there were 5 sequences with tyrosine gains and 10 sequences with tyrosine deletions (Fig. 2b).
[0120] Peptide sequences containing mutant sequences involving tyrosines (gains and deletions) and corresponding wild-type peptides (by in silico) were transcribed into 21-mer peptides containing 10 on both sides of the tyrosine-involving sites amino acid. This 21-mer peptide was then assessed to have an 8-11 amino acid epitope shown to bind HLA-A1 under the IEDB...
Embodiment 3
[0126] Example 3 : Identification of Cancer Mutations – Patient #2
[0127] A modified schematic for identifying mutations in cancer cells that can be used as targets for immune recognition was used for samples obtained from patient #2 and is shown in Figure 8a. Leukemic cells (L) and Epstein-Barr virus-transformed B cells (patient PHA cell line) (P) were obtained from patients before hematopoietic stem cell transplantation (HSCT). Leukemic cells were isolated from blood (22, 27) and EBV cells were prepared using previously published methods (see, eg, Caputo JL et al., J. Tissue Culture Methods 13:39-44, 1991). EBV cell lines were similarly generated from bone marrow donors (D). Freeze cells in liquid nitrogen.
[0128] DNA exome libraries were prepared using NGS methods from patient leukemia cells, patient EBV cell lines, and donor EBV cell lines under contract with Expression Analysis, Inc., Durham, NC. RNA transcriptome libraries were prepared by Expression Analysis In...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com