Methods for forming regional tissue adherent barriers and drug delivery systems
a tissue adherent barrier and tissue technology, applied in the direction of drugs, synthetic polymeric active ingredients, prosthesis, etc., can solve the problems of reducing the effect of skill, reducing the risk of adhesion formation, and reducing the effect of adhesion formation
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
[0133] A macromer is synthesized as described in U.S. Pat. No. 5,410,016 to Hubbell et al. The macromer may be an acrylated copolymer of poly(ethylene glycol) (M.W. 20,000) and dl-lactide (3-5 equivalents). The material is dissolved in water to form a solution that is 5% w / w, and the solution is divided into two parts. To part A is added enough hydrogen peroxide to give a 150 ppm concentration of H2O2. To part B is added enough of a ferrous gluconate salt to achieve a concentration of 3000 ppm. It may be verified that on mixing approximately equal parts of these two solutions, a flexible hydrogel is formed within 10 seconds of pouring into a mold, in the absence of activation by any external energy source.
example 2
[0134] To assess the efficacy of the regional adhesion barrier of Example 1, the following experiment may be conducted. Twelve Sprague Dawley male rats having an average weight of 250 g are divided into two groups of 6 for treatment and control, respectively. The abdomen is shaved and prepared with a betadine solution. A midline incision is made under anesthesia. The cecum is located and 4 to 5 scrapes made on a region about 2×1 cm on one side of the cecum, using a 4×4 in gauze pad to produce serosal injury and punctuate bleeding. Other abdominal organs also may be allowed to desiccate for 10 minutes during this period. The abdominal incisions in these animals are closed using a continuous 4-0 silk suture for the musculoperitoneal layer and 7.5 mm stainless steel staples for the cutaneous layer. A topical antibiotic then is applied at the incision site.
[0135] The first group consists of 6 animals serving as controls without treatment, to confirm the validity of the model. The secon...
PUM
| Property | Measurement | Unit |
|---|---|---|
| tensile strength | aaaaa | aaaaa |
| molecular weight | aaaaa | aaaaa |
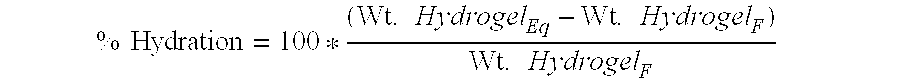
| equilibrium water content | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com