Biodegradable tissue replacement implant and its use
a tissue replacement and biodegradable technology, applied in the field of cell-based therapies, can solve problems such as serious vision loss
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Materials and Methods
Research and Clinical-Grade iPSC Derivation, Maintenance, and RPE Differentiation
[0231]Reporter iPSC line expressing GFP under the control of TYROSINASE enhancer and constitutive RFP was previously published (Maruotti et al., Proc Natl Acad Sci USA 112, 10950-10955 (2015)) and used to optimize the research-grade differentiation protocol. iPSCs were cultured on MEFs for 4 days before using for differentiation. To make cell aggregates, iPSCs were treated with Collagenase for 20 mins. After collagenase was aspirated, NEIM (DMEM / F12, KOSR, supplemented with N2, B27, LDN-193189 10 uM, SB431452 10 nM, CKI-7 hydrochloride 0.5 uM, and IGF-1 1 ng / ml) was added to the wells (1 ml / well) and cell scarper was used to scrape the colonies. Cell aggregates were grown in 10 cm2 low attachment corning dishes in NEIM medium for 48 hrs. After 48 hours, floating cell aggregates were collected and seeded in MATRIGEL® coated plates in RPEIM (DMEM / F12, KOSR, supplemented with N2, B27, ...
example 2
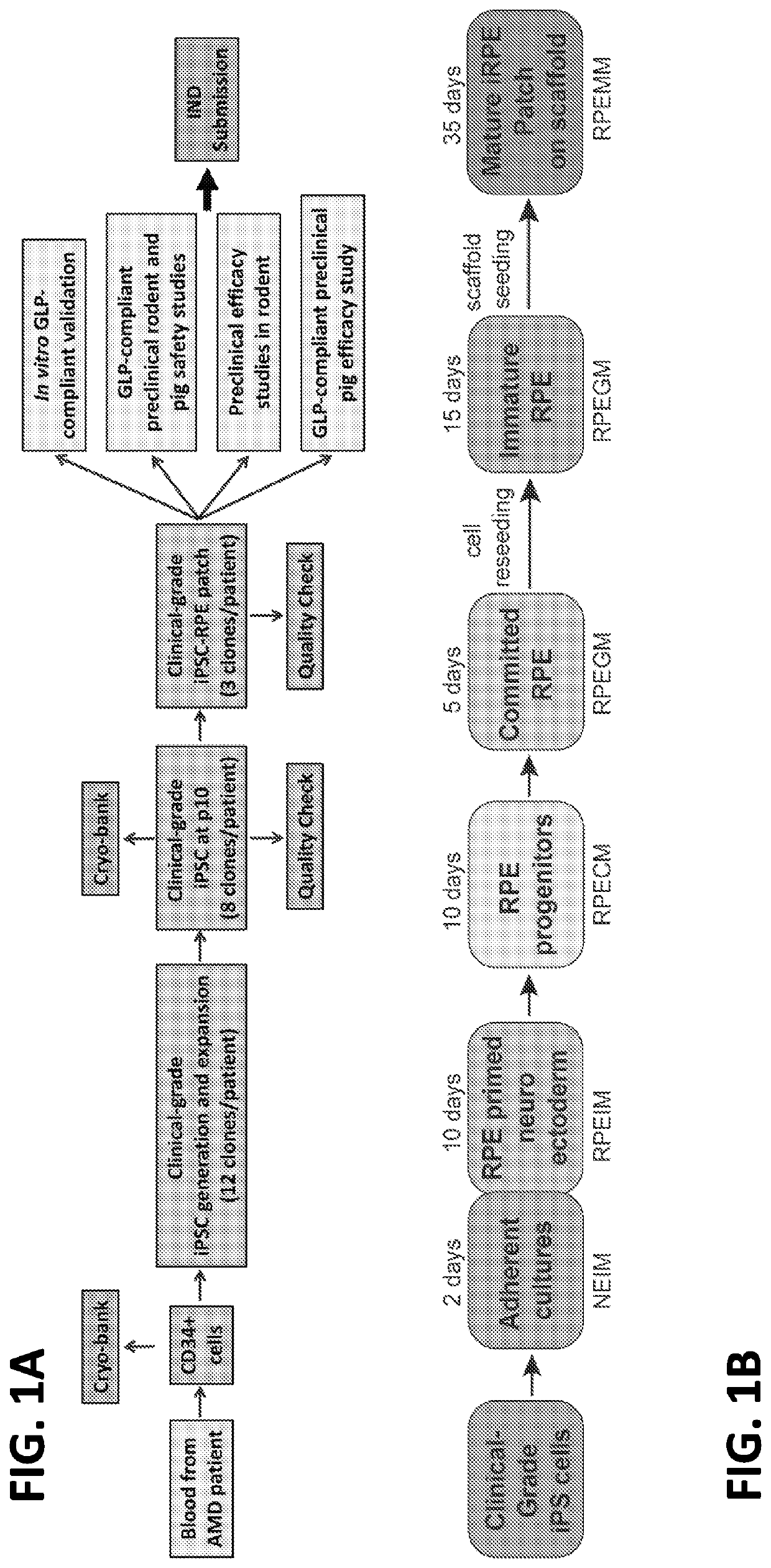
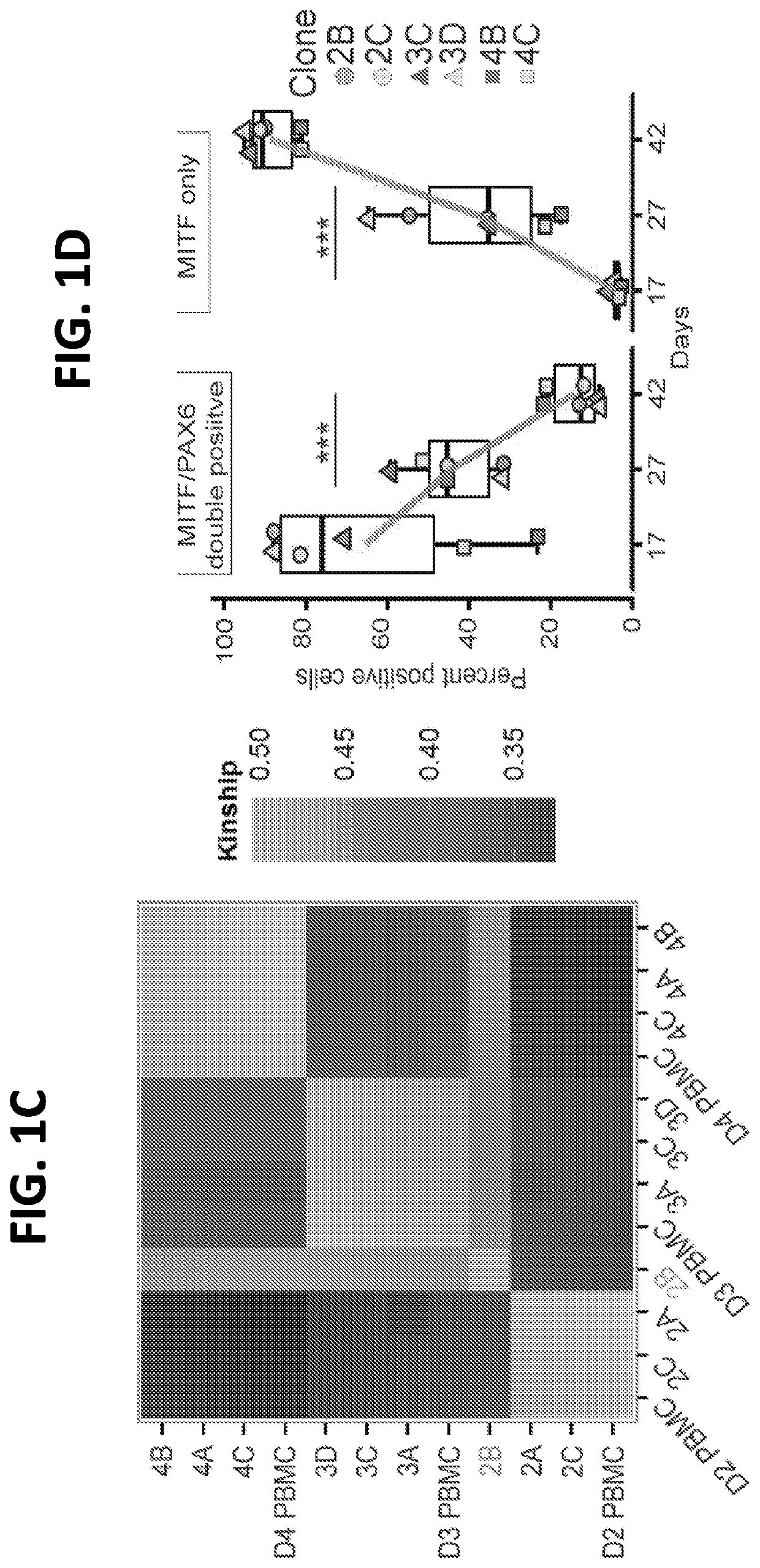
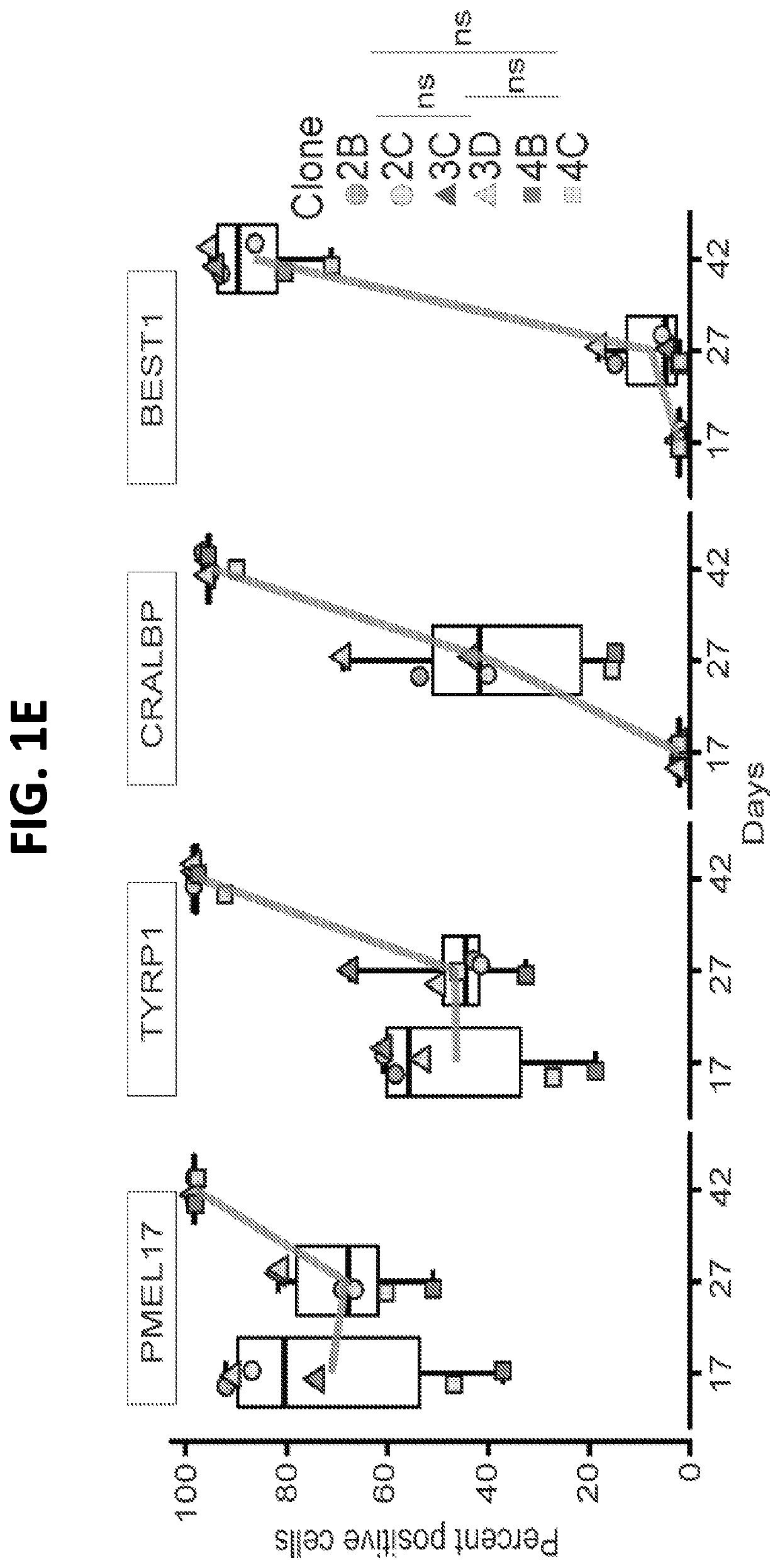
Clinical-Grade Triphasic Protocol Efficiently and Reproducibly Generates AMD-iRPE Cells
[0252]iPSC-derived from AMD-patient skin fibroblasts under clinical-grade conditions attained chromosomal copy number changes, likely during the reprograming process (Mandai et al., N Engl J Med 376, 1038-1046 (2017)). However, skin fibroblasts are not considered an ideal starting source when deriving iPSCs from older patients (Kang et al., Cell Stem Cell 18, 625-636 (2016)). Therefore, a manufacturing workflow was developed for autologous iPSC-derived RPE-patch from patient CD34+ peripheral blood cells. A pipeline for generation, functional validation, and in vivo testing of clinical-grade AMD patient-specific iPSC-RPE patch (FIGS. 1A, B) was developed. Due to the progenitor and proliferative nature, CD34+ cells isolated from patients' peripheral blood could provide a good source for iPSC generation. Multiple iPSC clones were generated from CD34+ cells and skin fibroblasts of three advanced “dry”...
example 3
Biodegradable Scaffold Helps Clinical-Grade AMD-iRPE Cells to Functionally Mature into a Monolayer Tissue
[0256]It was hypothesized that a biodegradable scaffold would provide suitable material for RPE cells to secrete extracellular matrix (ECM) to form a polarized monolayer. As the scaffold degrades, ECM and cells would constitute a native-like RPE tissue that would enhance the possibility of long-term integration of iRPE-patch in patients' eyes. Scaffolds used in the clinical-grade process were manufactured using poly-(lactic-co-glycolic acid) / PLGA (50:50 lactic acid / glycolic acid, IV midpoint 1.0 dl / g), with 350 nm mean fiber diameter previously shown to be optimal for RPE growth (Liu, et al., Biomaterials 35, 2837-2850 (2014); Stanzel et al., Stem Cell Reports 2, 64-77 (2014)). A single layer heat-fused nanofibers scaffold was selected for iRPE-patch manufacturing because of its high Young's Modulus that correlated with the ease of transplantation (FIGS. 2A, 2B). As expected for ...
PUM
| Property | Measurement | Unit |
|---|---|---|
| diameter | aaaaa | aaaaa |
| pore size | aaaaa | aaaaa |
| thickness | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com