Simulation model for evaluating tumor ablation range through ultrasonic mono-modal image fusion
An image fusion, single modality technology, applied in the medical field
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
[0125] Embodiment 1 Preparation of Nano Lipid Microbubble Ultrasonic Contrast Agent
[0126] 1. Dissolve the phospholipid components dipalmitoyl phosphatidylcholine, distearoylphosphatidylethanolamine and dipalmitoylphosphatidic acid in chloroform. The mass-number ratio of dipalmitoylphosphatidylcholine, distearoylphosphatidylethanolamine and dipalmitoylphosphatidic acid is 18:1:3.5.
[0127] 2. Add double distilled water containing 10% glycerol (v / v) and 2mg / mL Pluronic F68 after the chloroform volatilizes naturally to form a phospholipid film, and hydrate at 37°C for 1 hour. Acoustic vibration was performed at the liquid-liquid junction for 5 minutes, and octafluoropropane gas was introduced at the same time.
[0128] 3. Centrifuge the microbubble solution at 50×g for 5 minutes, absorb the milky white liquid in the lower layer and transfer it to a tube, centrifuge at 805×g for 30 minutes, discard the lower layer liquid, and resuspend it with PBS to obtain nano-lipid microbu...
Embodiment 2
[0130] Example 2 Preparation of phantom model before ablation
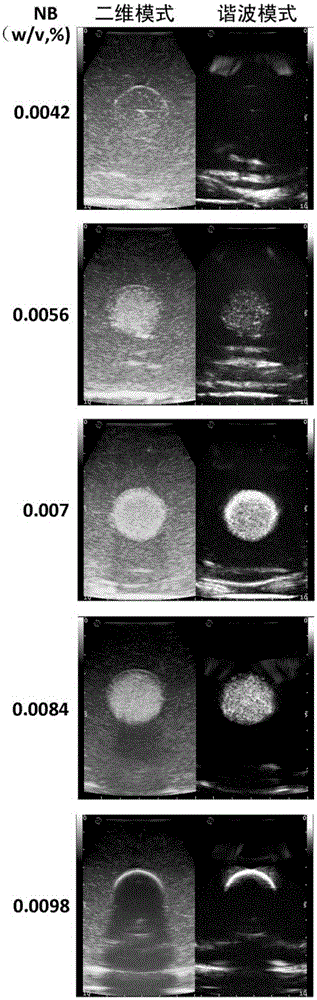
[0131] Weigh 20 g of carrageenan and 1 g of gastric window acoustic contrast agent in a beaker with an electronic balance, and add 1000 mL of double distilled water at 60°C. Place the beaker in a constant temperature water bath at 60°C and stir with a glass rod until the solute is completely dissolved to form normal tissue matrigel. Take 38 mL of Matrigel in a small beaker, add 2 mL of milk to form tumor gel Matrigel, then add nano-lipid microbubble ultrasound contrast agent, stir evenly to form tumor gel. In this example, tumor gel models with nanoscale lipid microbubble ultrasound contrast agent concentrations (calculated by phospholipid mass) of 0.0042%, 0.0056%, 0.007%, 0.0084% and 0.0098% (w / v) were prepared respectively. After placing the tumor glue in a sphere mold with a diameter of 3 cm, place it in ice water and cool it for 5 minutes, and take it out to obtain the tumor glue model.
[0132] The tumor g...
Embodiment 3
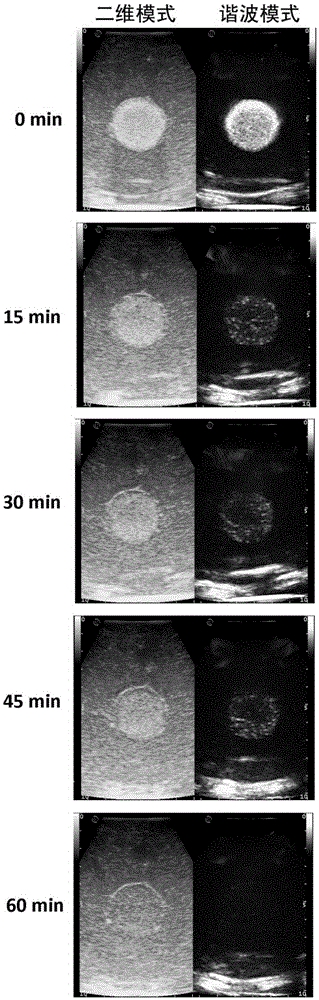
[0133] Example 3 Detection of Ultrasonic Imaging Effects of the Phantom Model Before Ablation
[0134] The phantom phantoms with different concentrations of nanoscale contrast agents were examined with contrast-enhanced ultrasound. In this embodiment, Esaote MyLabtwice model clinical ultrasonic diagnostic instrument and linear array probe are used to detect the phantom, the imaging frequency band is 3-11 MHz, the focal point is placed in the middle of the tumor, and the gain is 0.5. For harmonic contrast ultrasound imaging mode, use a mechanical index of 0.03 and a gain of 0.38. 10 min after the phantom model was taken out of the refrigerator was defined as 0 min, and two-dimensional ultrasound and harmonic contrast ultrasound imaging were performed on the phantom model at different time points.
[0135] The result is as figure 2 As shown, at the time point of 0 min, phantom models prepared with different concentrations of nano-scale contrast agents showed different imaging...
PUM
| Property | Measurement | Unit |
|---|---|---|
| Particle size | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com