Method for preparing tumor cell vaccine based on non-thermal plasma
A low-temperature plasma and tumor cell vaccine technology, applied in the field of plasma tumor cell vaccine preparation
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
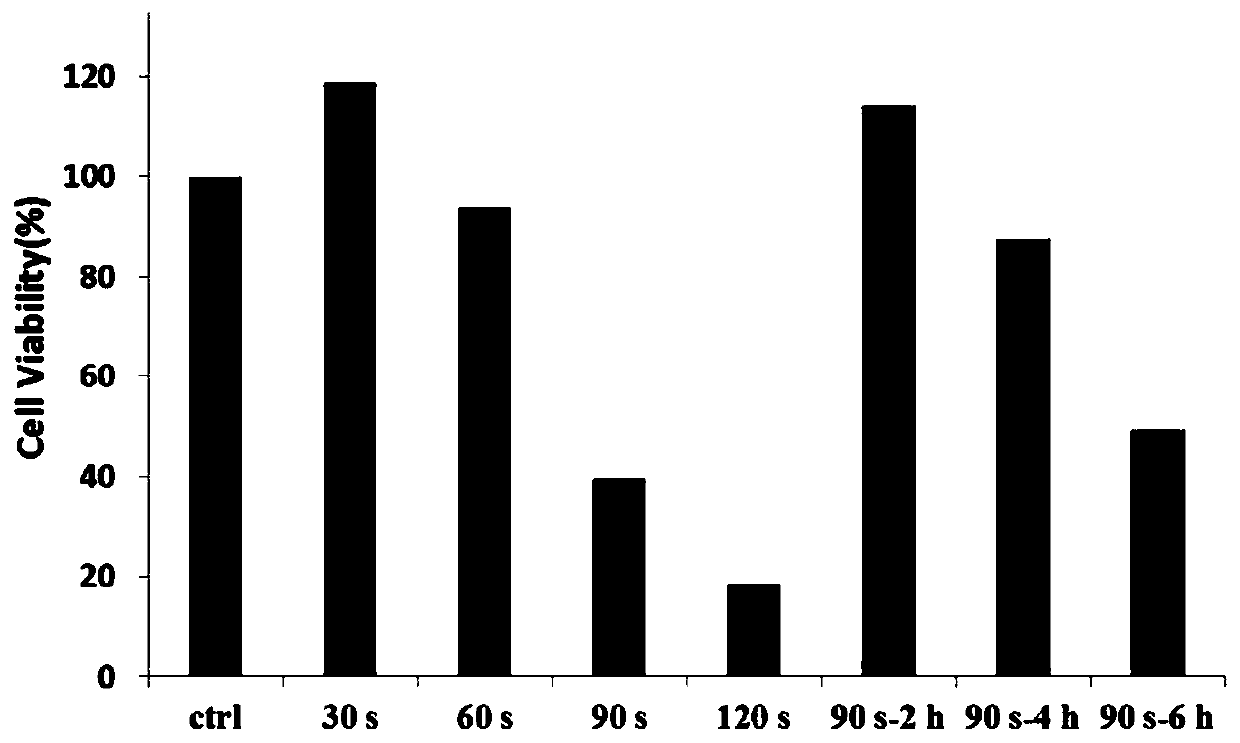
[0027] Example 1 Cell Counting Kit-8 (CCK-8 kit) detects the killing effect of low temperature plasma on cancer cells
[0028] The dielectric barrier discharge low-temperature plasma device is adopted, and the device mainly includes two parts: a high-voltage power supply and a plasma reaction chamber. Wherein, the plasma reaction chamber is composed of 4 pairs of electrodes, and helium is selected as the working gas in all the embodiments of the present application.
[0029] The mouse melanoma cell B16-F10-OVA was used as the test object (purchased from the Cell Bank of the Type Culture Collection Committee of the Chinese Academy of Sciences). %CO 2 Under certain conditions, culture in DMEM high-glucose medium containing 10% fetal bovine serum and 1% penicillin-streptomycin, and subculture when the cell fusion degree reaches 80%-90%.
[0030] Take the cells growing in the logarithmic phase, wash with preheated PBS, add 1.0 mL of trypsin, centrifuge at 2000 rpm for 5 minutes,...
Embodiment 2
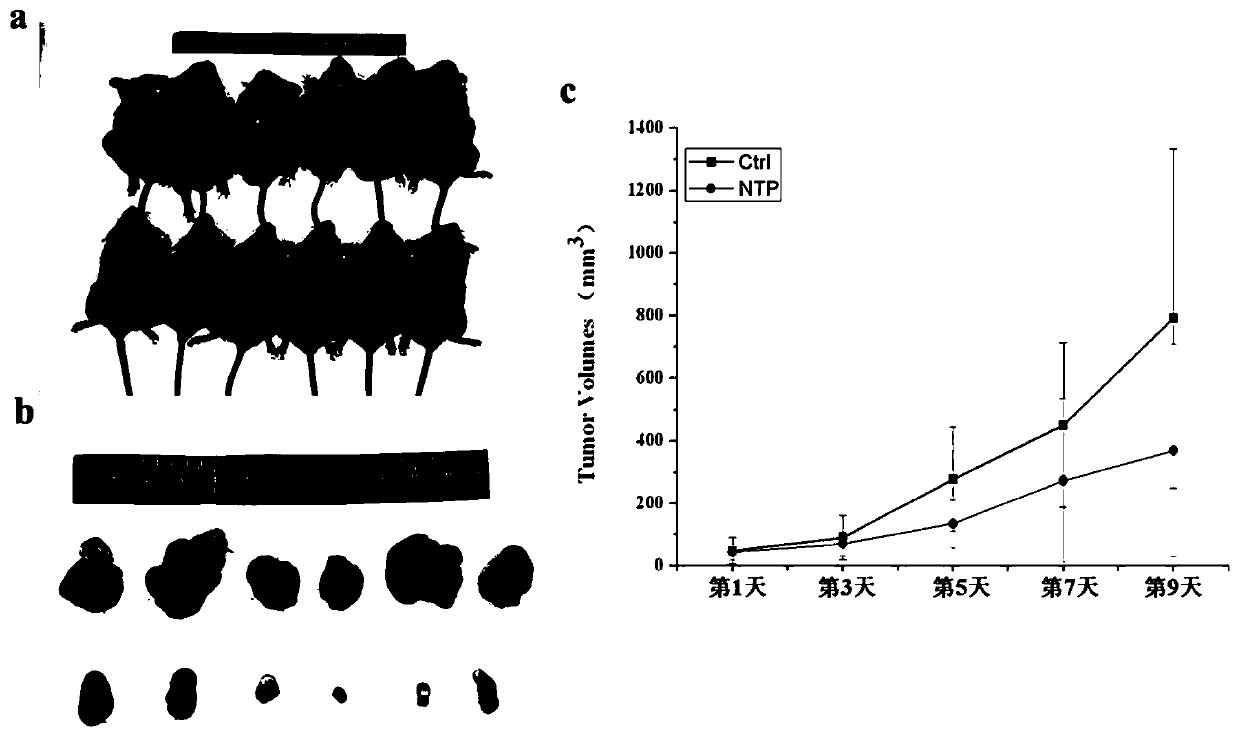
[0033] Example 2 In vivo experiments verify the effectiveness of tumor cell vaccines
[0034] The low-temperature plasma device, experimental materials and low-temperature plasma treatment method are the same as those in Example 1. After low-temperature plasma treatment for 120 seconds, the mouse melanoma cell B16-F10-OVA was cultured for 12 hours, trypsinized, centrifuged at 2000 rpm for 5 minutes, and the cells were collected. Wash the cells with pre-cooled PBS, resuspend and count, and adjust the concentration to 10 7 cells per milliliter. Take 20 C57BL / 6 mice aged 6-8 weeks, and divide them into 2 groups, 10 mice in each group, which are the control group and the experimental group, respectively. On the first day, the mice in the control group were injected intraperitoneally with PBS group (100ul), and the mice in the experimental group were injected intraperitoneally with low-temperature plasma inactivated tumor cells (100ul, about 1-3×10 6 cell). On the third day, th...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com