Registration of ultrasound to fluoroscopy for real time optimization of radiation implant procedures
a radiation implant and fluoroscopy technology, applied in the field of ultrasound and carm fluoroscopy imagery registration, can solve the problems of not being able to meet the most likely conditions of c-arms, few attempts to relate fluoroscopic images to soft tissue anatomy with little success, and not being able to achieve quantitative intra-operative analysis, etc., to achieve the effect of improving the localization of radiation doses, improving visualization and control, and avoiding the use of c-arms
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
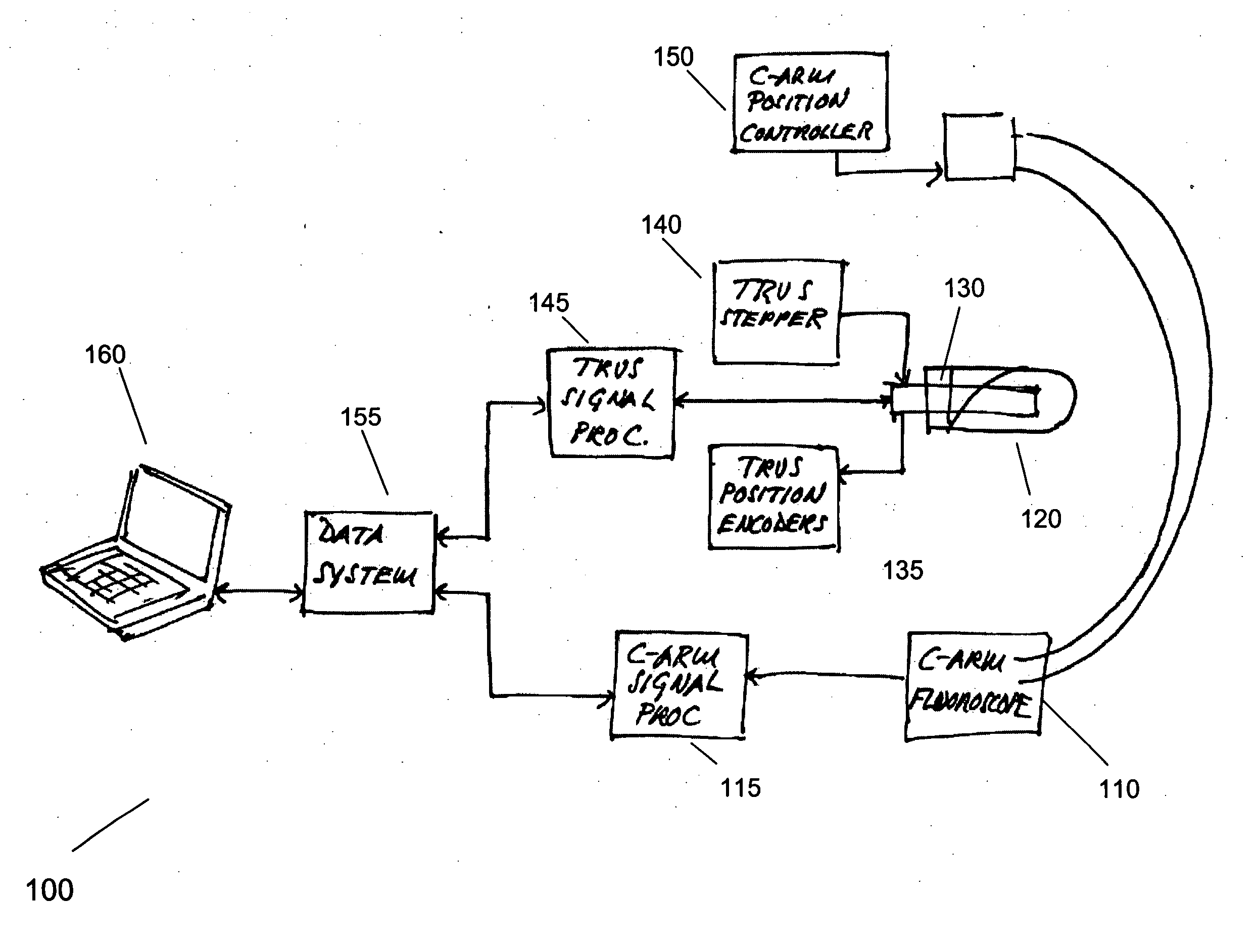
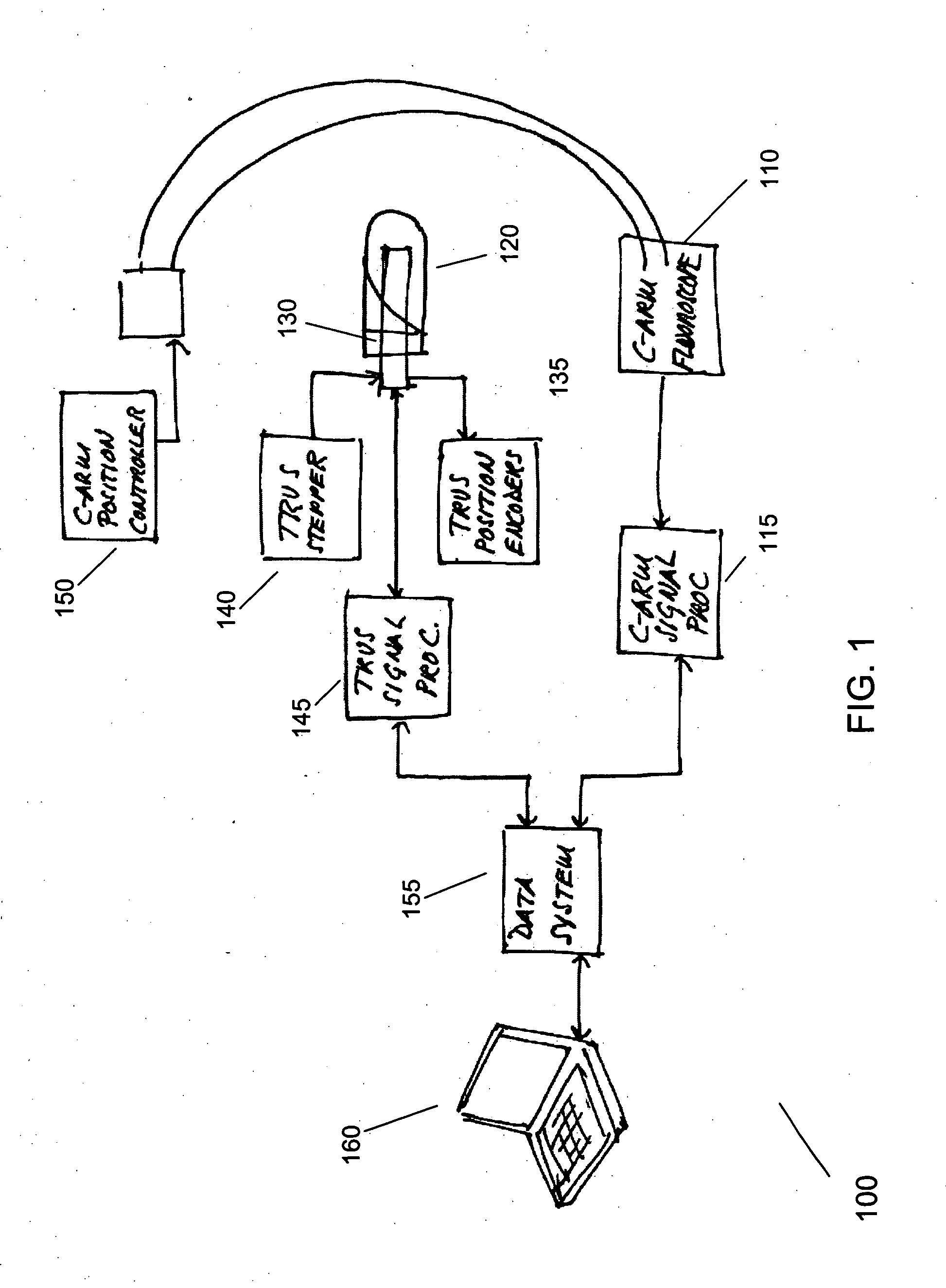
[0030]FIG. 1 shows an exemplary system 100 for registering ultrasound and C-arm fluoroscopy according to the present invention. The system 100 generally comprises commercially available TRUS and C-arm fluoroscopy hardware. The system 100 includes a C-arm fluoroscope 110; related C-arm fluoroscope signal processing hardware and software 115; a C-arm position controller 150; a transrectal sheath 120; a TRUS probe 130; a TRUS stepper; a TRUS probe position encoder 135; TRUS signal processing hardware and software 145; a data system software 155; and a computer 160, which stores and executes the data system software 155. The computer 160 may comprise multiple computers, including remote databases and embedded processors. It will be apparent to one skilled in the art that the data system software 155, and the computer 160, may be provided in many different configurations.
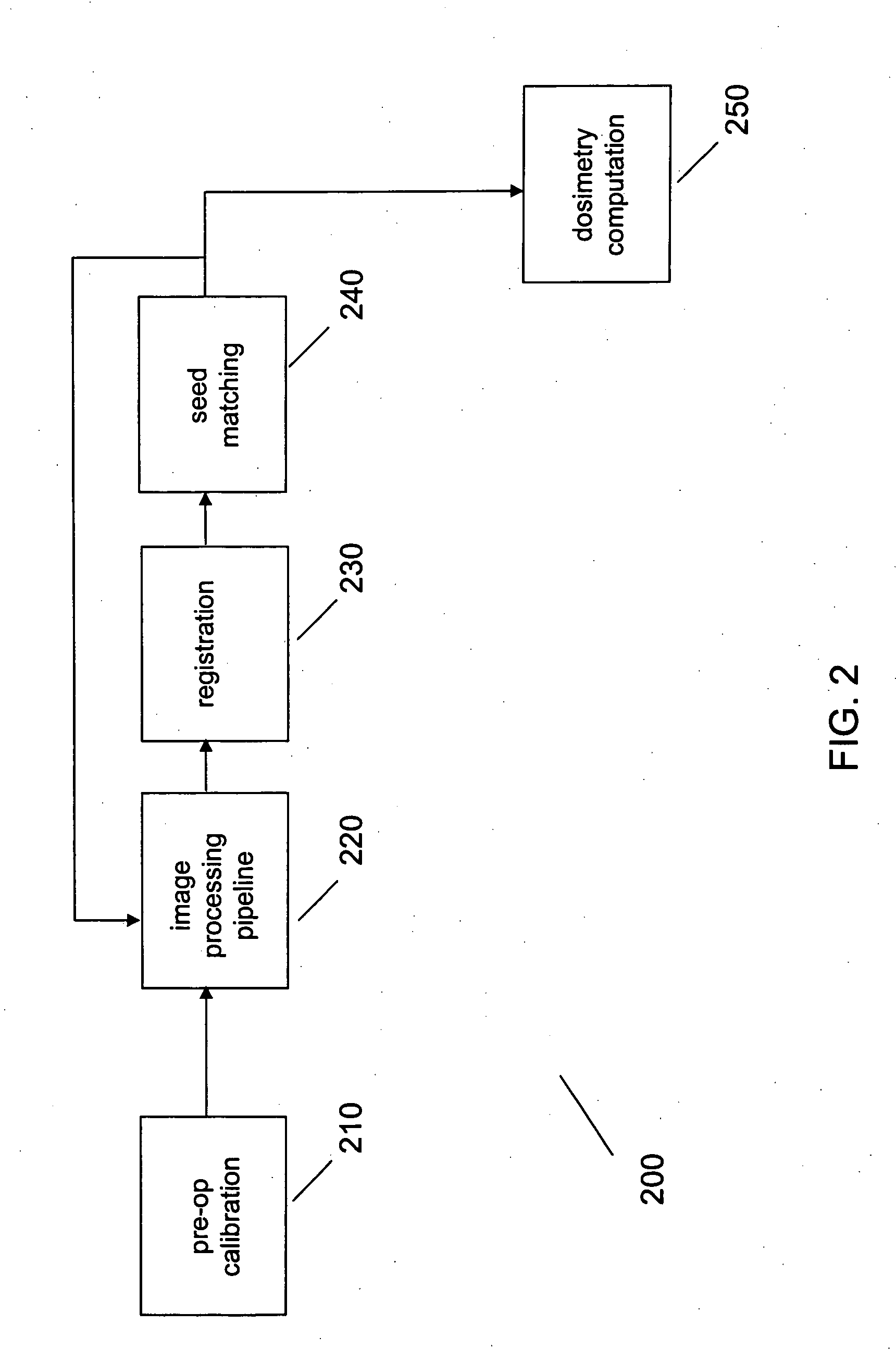
[0031]FIG. 2 shows an exemplary process 200 for registering ultrasound and C-arm fluoroscopy according to the present...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com