System and method for magnetic-resonance-guided electrophysiologic and ablation procedures
a magnetic resonance and electrophysiologic technology, applied in the field of electrophysiologic diagnostic and therapeutic procedures, can solve the problems of inability to determine the optimal approach, inability to achieve the optimal approach, so as to improve the safety and accuracy of electrophysiologic procedures, improve the resolution and reliability, and simplify the production of continuous linear lesions
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
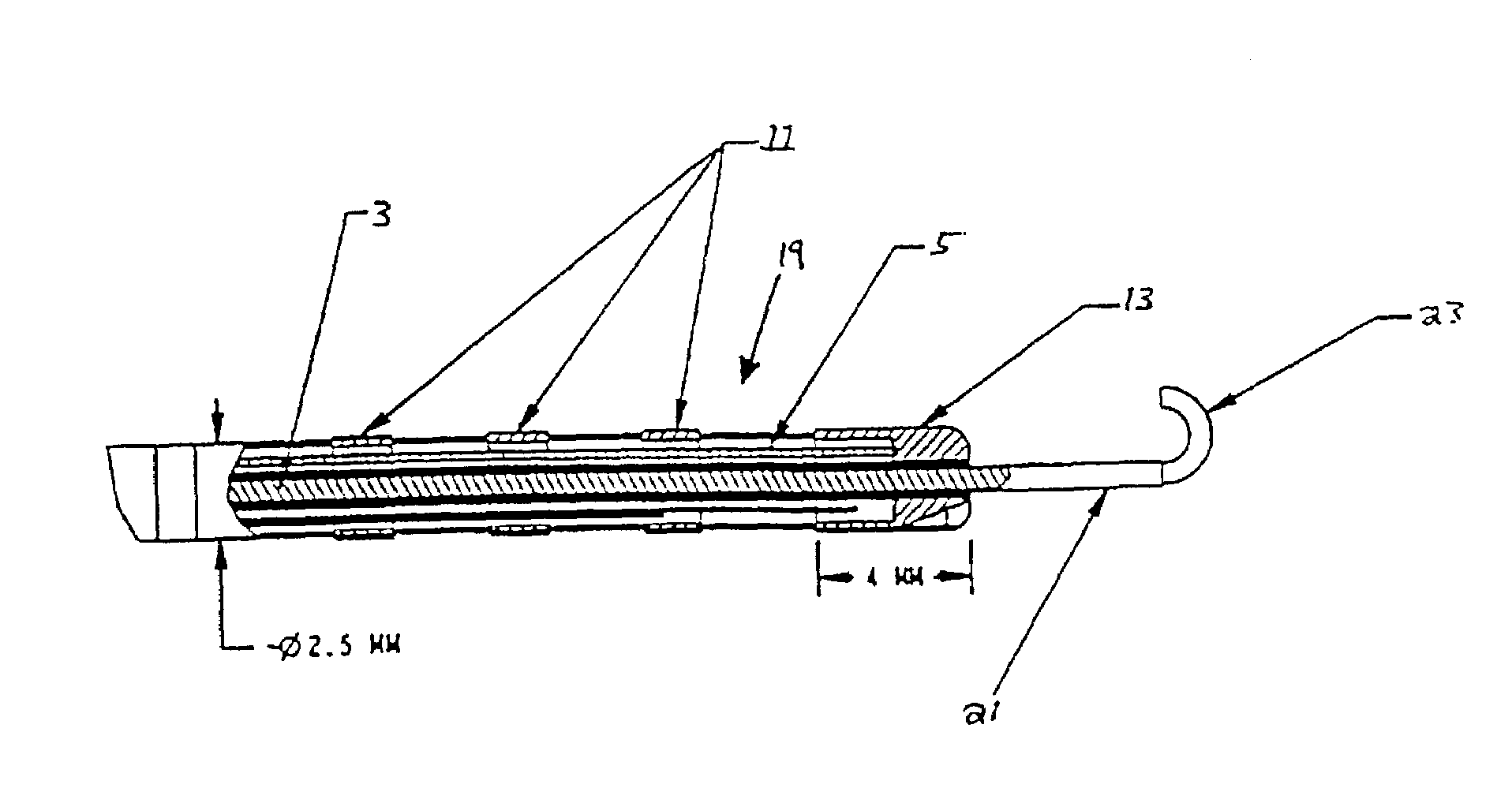
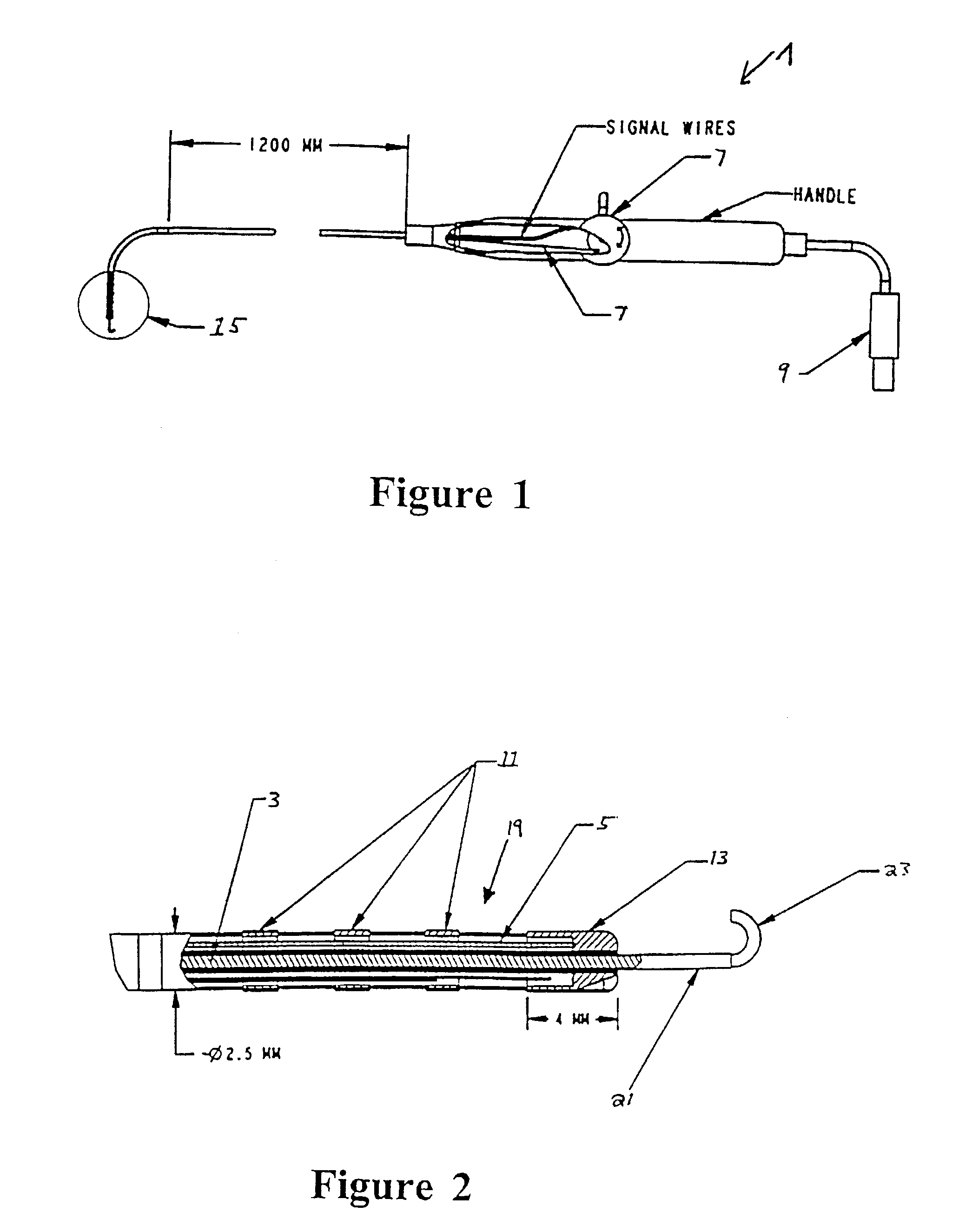
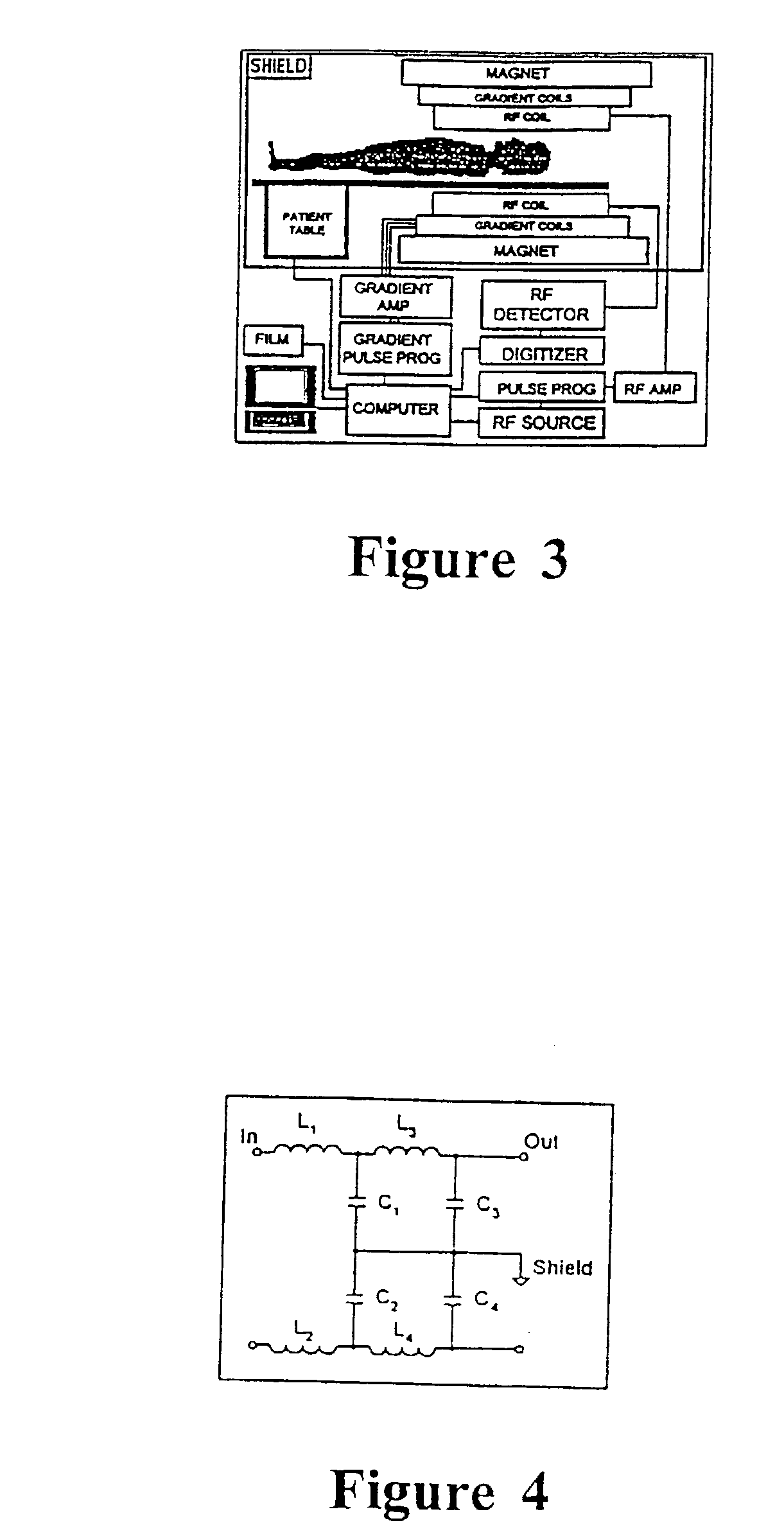
[0033]The invention in its preferred embodiment uses MR imaging to allow catheters to be placed without radiation, and provides very accurate localization of catheter tips in 3-dimensional space. With current MRI scanners, resolution is limited by the distance the RF coil is from the volume of tissue being imaged. RF from any particular imaging volume is picked up by the surface coil. The gradients select a volume inside the body for imaging, but the coil outside the body picks up the signal from the volume. The farther the surface coil is from the imaging volume, the more noise will be present.
[0034]In accordance with a preferred embodiment of the invention, an intracardiac receiving coil / antenna is used so that the receiving coil / antenna is closer to the imaging volume (lesions), thereby reducing noise, increasing signal, and improving resolution where it is needed most.
[0035]In a first embodiment of the invention, MRI is used to facilitate catheter ablation of atrial fibrillation...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com