Emboli protection devices and related methods of use
a protection device and shield technology, applied in the field of shield devices, can solve the problems of blockages, whether partial or full, that can have serious medical consequences, damage to the heart, and other vessels are also prone to narrowing
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
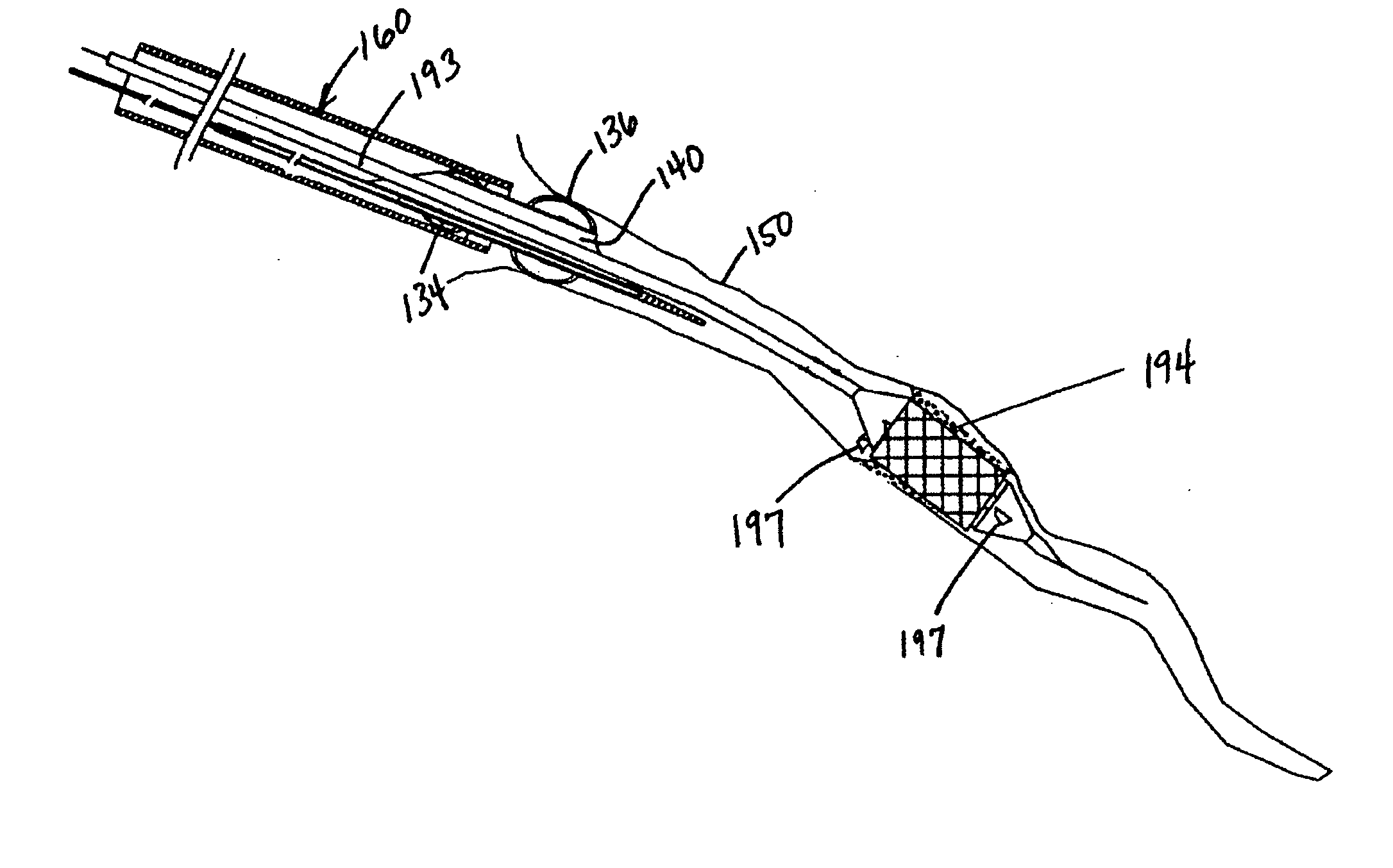
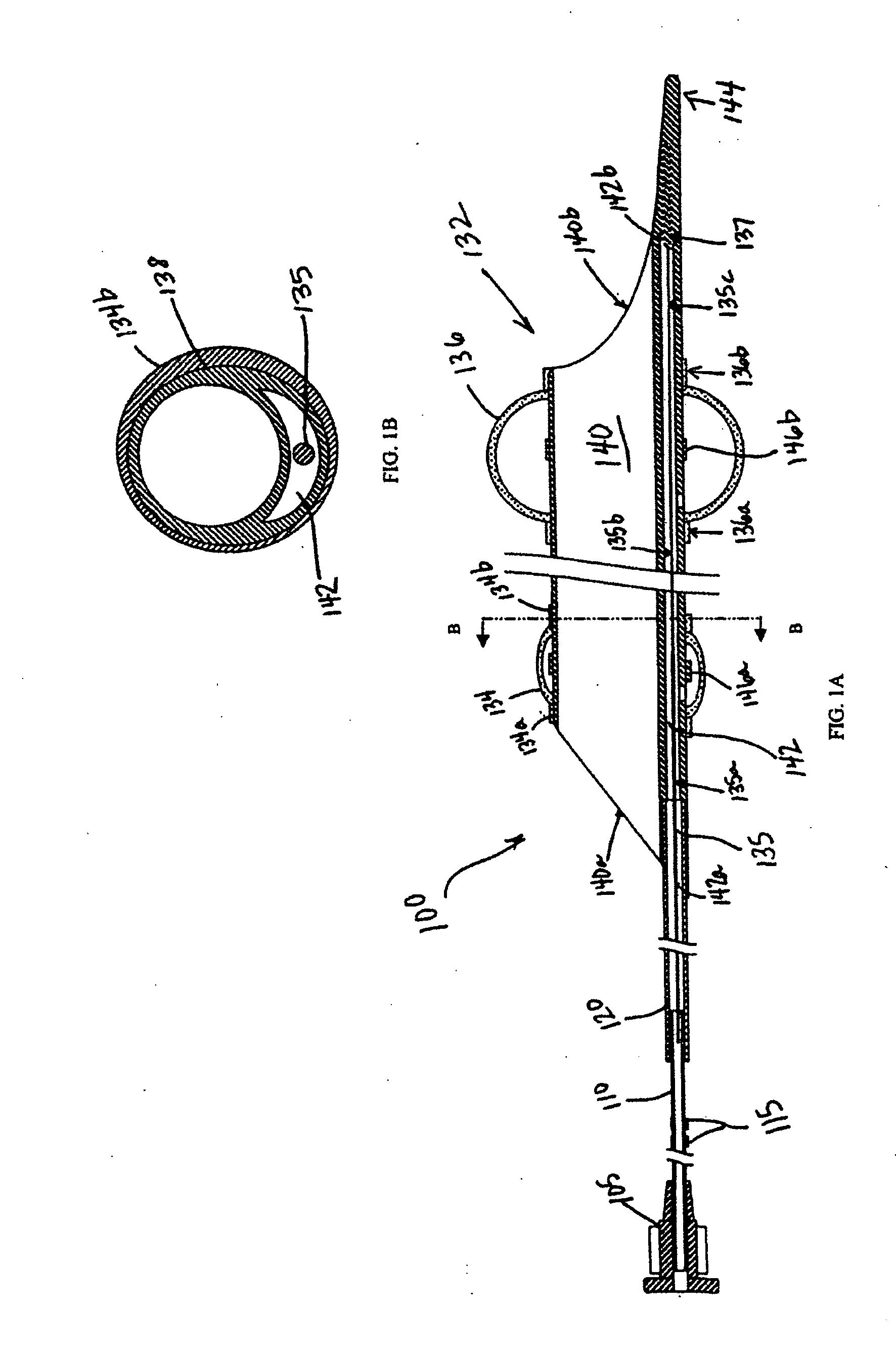
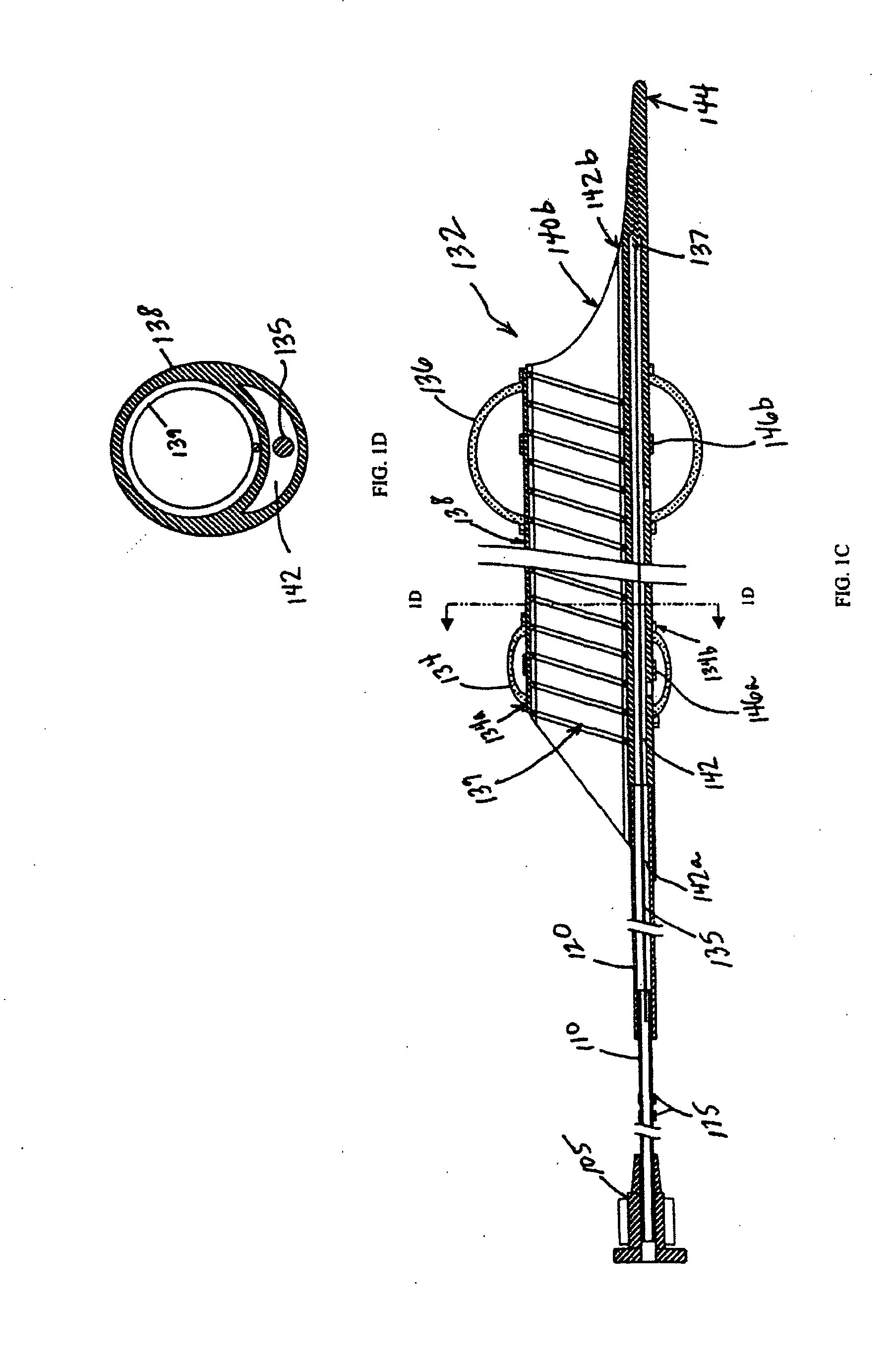
[0100]Reference will now be made in detail to the present embodiments of the invention, examples of which are illustrated in the accompanying drawings. Wherever possible, the same reference numbers will be used throughout the drawings to refer to the same or like parts.
[0101]The present invention provides a system and method for evacuating emboli, particulate matter, and other debris from a blood vessel, and particularly from an occluded blood vessel. As used herein, an “occlusion,”“blockage,” or “stenosis” refers to both complete and partial blockages of the vessels, stenoses, emboli, thrombi, plaque, debris and any other particulate matter which at least partially occludes the lumen of the blood vessel.
[0102]Additionally, as used herein, “proximal” refers to the portion of the apparatus closest to the end which remains outside the patient's body, and “distal” refers to the portion closest to the end inserted into the patient's body.
[0103]This method and apparatus are particularly ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com