Method for stimulating a host immune system by administering an allogeneic cell material
a technology of allogeneic cells and host immune system, applied in the field of allogeneic cell infusion to treat diseases, can solve the problems of major limitation of matched donor requirements, therapy protocols, loss of functioning immune system,
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
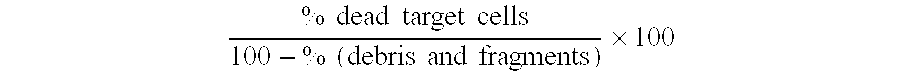
Image
Examples
examples
[0134]The following examples are included for illustrative purposes only and are not intended to limit the scope of the invention.
Methods:
Microsphere Preparation
[0135]The solvent evaporation method was used for preparation of microspheres. Lactel® (Birmingham Polymers, Birmingham, Ala.) 50 / 50 DL-PLG product number 50DG020 with a inherent viscosity of 0.15 to 0.25 dl / g was used as the polymer. The DL-PLG powder was dissolved in 20 ml of methylene chloride to a final 5% DL-PLG w / v ratio. The 5% DL-PLG solution was then added dropwise to 125 ml of 2.4% hydroxypropylmethylcellulose in 0.1M glycine / HCl buffer pH 1.1 under constant stirring at 1000 rpm at room temperature (25±2° C.). Stirring was maintained until complete evaporation of the organic solvent (about 3 hours). Microspheres were collected by centrifugation at 1000 rpm, 5 min at 40 C followed by three cycles of washing with distilled water, filtered and dried overnight. The microsphere sizes ranged from 3.0 to 7.0 um with a CV ...
example # 1
Example #1
Phenotypic Analysis of Allogeneic Cell Product
[0137]A sample of allogeneic cell product was taken on day 1 and day 10 for phenotypic analysis. For cell immunophenotyping, surface labeling was performed by a direct fluorescence technique using monoclonal antibodies (Becton-Dickinson, San Jose, Calif., USA), against human CD4, CD8, CD14, CD19, CD56, CD4 / CD25, CD4 / DR, CD4 / CD45RA, CD4 / CD45RO, CD4 / CD62L, CD4 / CD154 (FasL), CD4 / TRAIL. To detect intracellular cytokines, mononuclear cells were permeabilized with FACS permeabilizing solution (Becton-Dickinson). Flow cytometry analyses were carried out with a FACSort equipment (Becton-Dickinson) using the Cellquest software. The results are reported as the percent of stained cells calculated from 10,000 events for all immunophenotypes.
Results in percentage of total cells (MFIR):DAY 1DAY 10CD492.599.8CD80.80CD144.80CD190.90CD561.70CD4 / CD252.392.9CD4 / DR4.589.7CD4 / CD45RA70.310.9CD4 / CD45RO16.678.1CD4 / CD62Lhi69.40.9CD4 / CD154 (FasL)0.874.3...
example # 2
Example #2
Cytokine Gene Profile of Allogeneic Cell Product
[0139]To determine the cytokine profile of the Allogeneic Cell Product, cytosolic RNA was purified using a RNeasy kit (Qiagen) and reversed transcribed using a Roche First Strand cDNA synthesis kit. Primers and probes were purchased from Applied Biosystems or were designed using Primer Express software. Real-time PCR amplification and product detection was performed according to manufacturer's recommended procedures on an ABI Prism 7700. Gene product is expressed relative to GAPDH expression, which is set at a value of 100,000 on day 1 and day 10.
Day 1Day 10IL-1beta857IL-2418,450IL-420IL-500IL-600IL-101110IL-12p351212IL-12p4000IL-13823IL-15111200IL-18108TNF-alpha2184,880IFN-gamma1894,600TGF-beta00
PUM
| Property | Measurement | Unit |
|---|---|---|
| concentrations | aaaaa | aaaaa |
| concentrations | aaaaa | aaaaa |
| temperature | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com