Fracture fixation systems
a fixation system and fracture technology, applied in the field of orthopaedic implants, can solve the problems that the bones of the patient may also degrade over time to harmless resorbable, and achieve the effects of facilitating orthopedic surgery, rapid restoration, and promoting normal healing
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
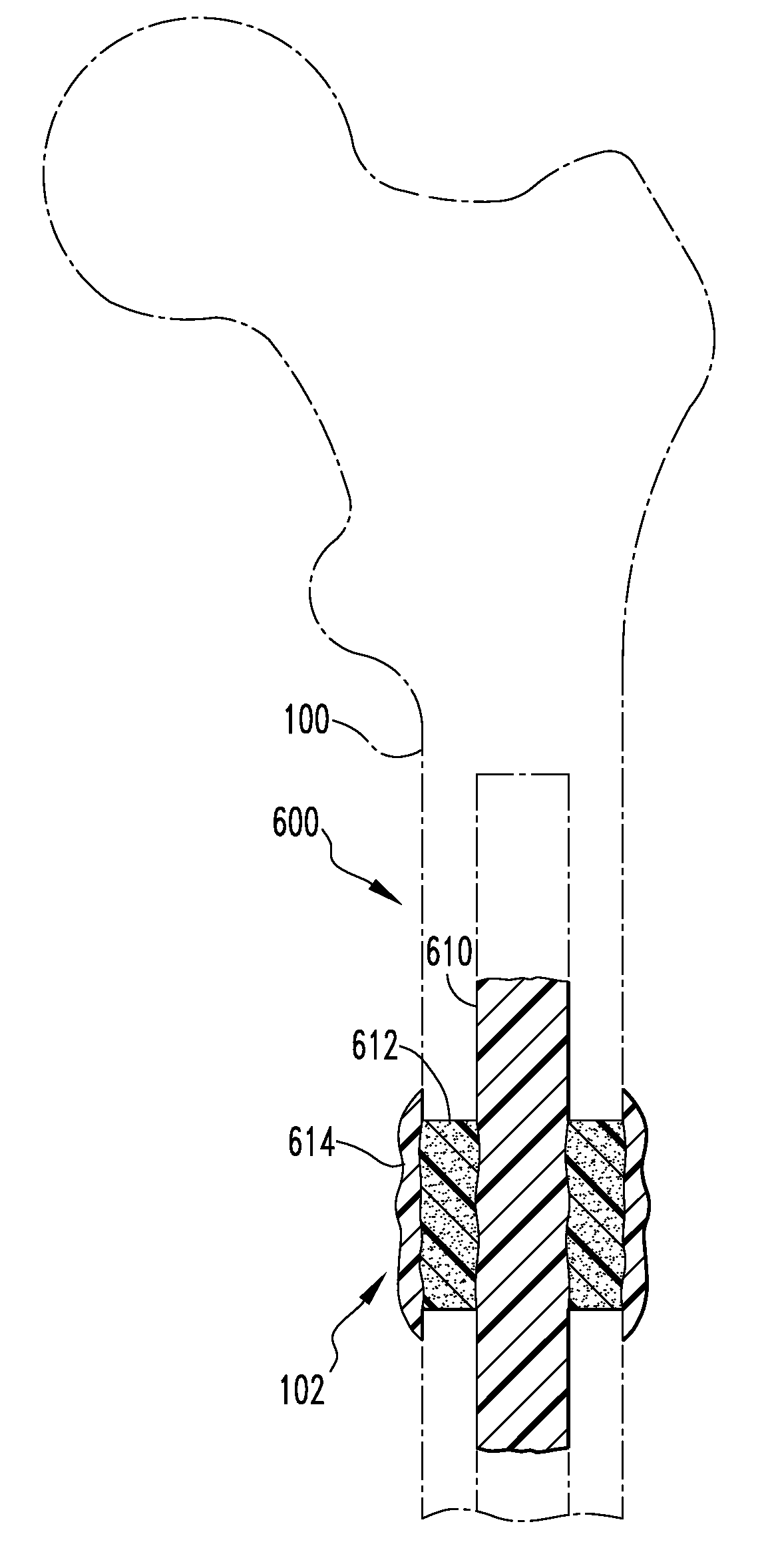
[0133]The disclosed systems and methods are also advantageously used in treatment of bone fractures associated with disease, pathological conditions or injury.
[0134]Treatment of Bone Fractures
[0135]Healing of bone fractures generally occurs, at least to some degree, naturally in humans or animals as a result of formation of new bone tissue in a fractured bone. New bone formation, which is sometimes termed “ossification” or bone “in-growth,” naturally occurs due to the activity of bone cells, such as osteoblasts and osteoclasts and eventually results in closing of a fracture site with newly formed tissue. In order for the bone tissue to grow such that a fractured bone heals into its pre-fracture form and restores its function, the bone pieces or fragments have to be located in their appropriate natural physical position and orientation, a process referred to as “reduction.” Further, the bone fragments must be maintained in said position and orientation for the duration of the healing...
PUM
| Property | Measurement | Unit |
|---|---|---|
| length | aaaaa | aaaaa |
| mean diameters | aaaaa | aaaaa |
| mean particle size | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com