Handheld physiological sensor
a physiological sensor and hand-held technology, applied in the field of sensors, can solve the problems of nullifying the value of such measurements, affecting treatment, and measurement errors, and achieve the effects of reducing costs, facilitating consistent, daily measurements, and being convenient to us
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
1. Product Overview
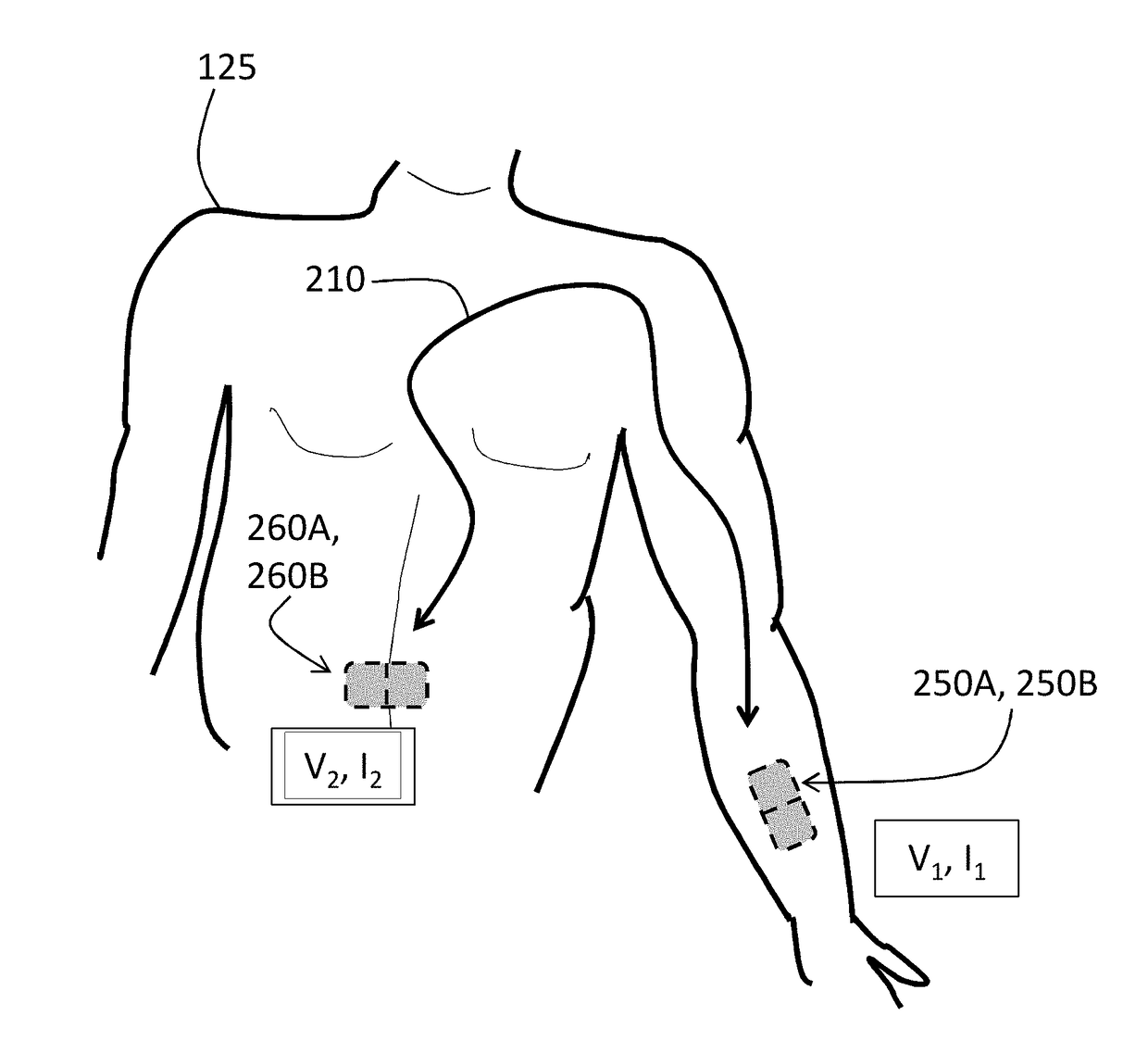
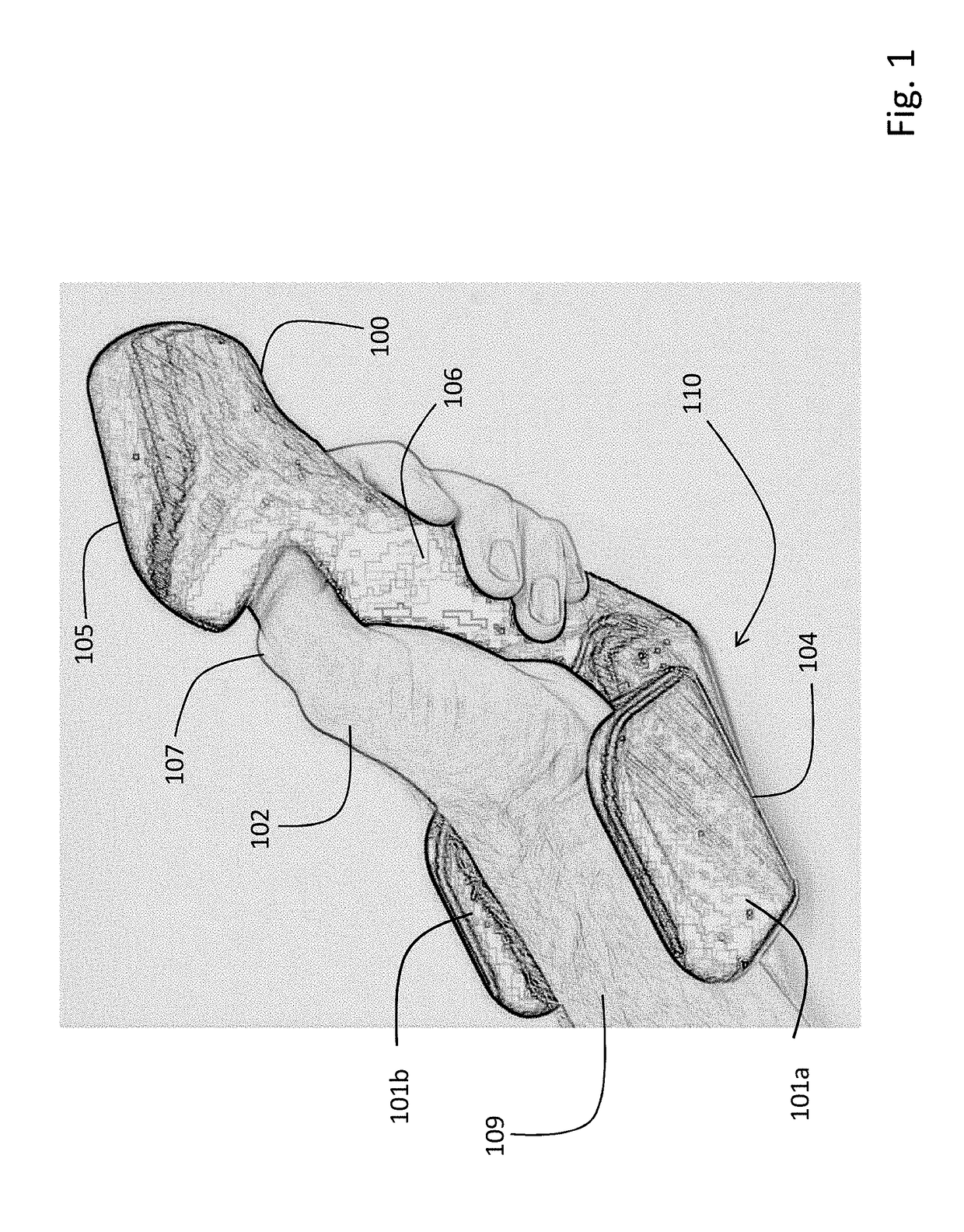
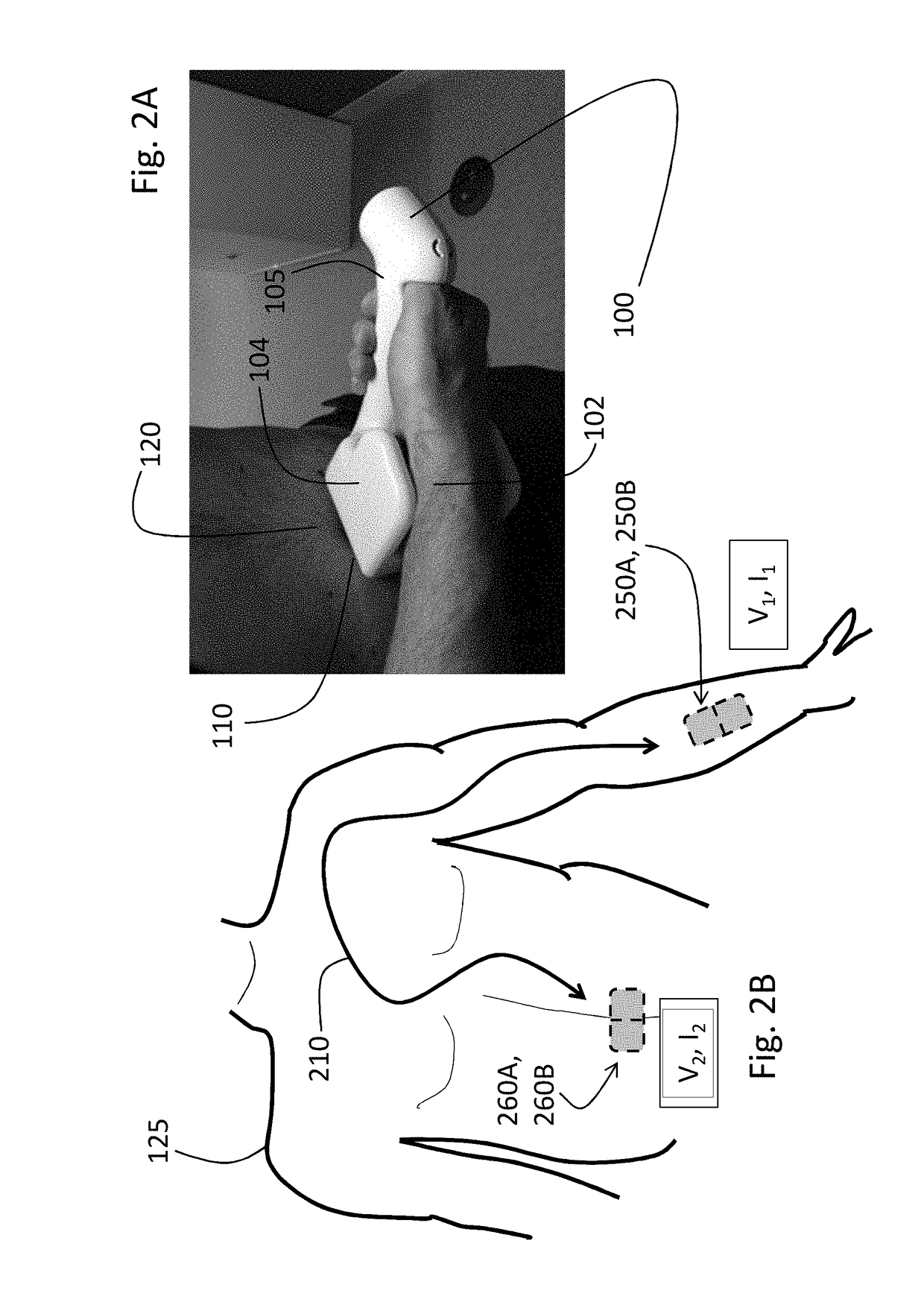
[0059]A handheld device according to the invention integrates measurement of all vital signs and some hemodynamic parameters from the human body into a single, easy-to-use device. More specifically, the device measures the following waveforms: 1) ECG; 2) pressure; 3) PPG; and 4) TBI. Digital electronics in the device process these waveforms to calculate the following numerical information: 1) SYS, DIA, and MAP; 2) SpO2; 3) HR and HRV; 4) RR; 5) TEMP; 6) SV; 7) CO; and 8) FLUIDS. It uses permanent, reusable components (e.g. electrodes), and transmits numerical and waveform information through a patient's mobile device to a web-based system.
[0060]The handheld device supplants more complex prior systems that include, e.g., multiple devices to measure vital signs and hemodynamic parameters. For example, such prior systems may include a separate blood pressure cuff, pulse oximeter, Holter monitor or patch-based system, and spirometer to measure vital signs. Determining...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com