Patents
Literature
413 results about "Cardiac output" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
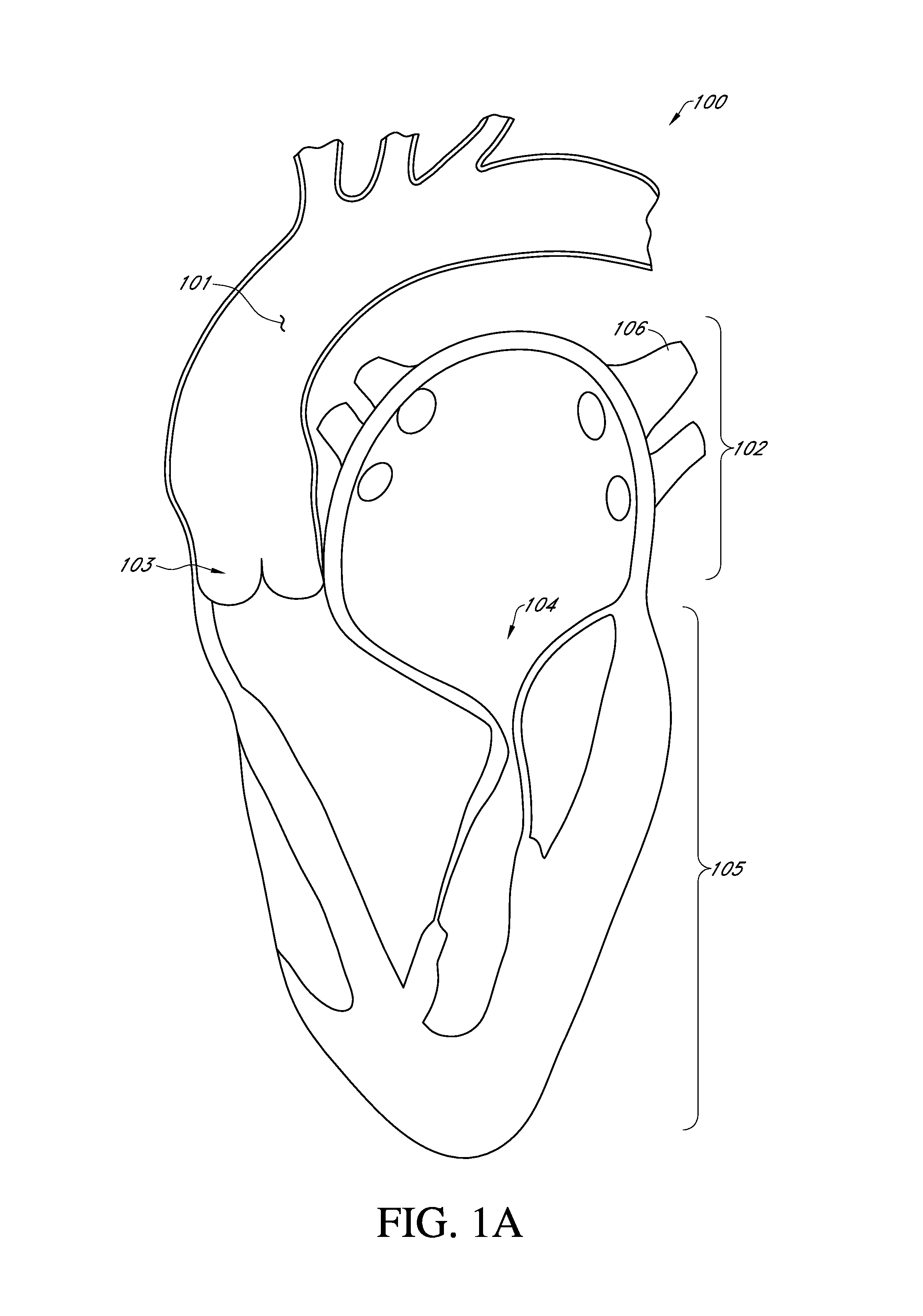
Cardiac output, also denoted by the symbols Q, or Qc, is a term used in cardiac physiology that describes the volume of blood being pumped by the heart, in particular by the left or right ventricle, per unit time. Cardiac output is the product of the heart rate (HR), or the number of heart beats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the ventricle per beat; thus, CO = HR × SV.
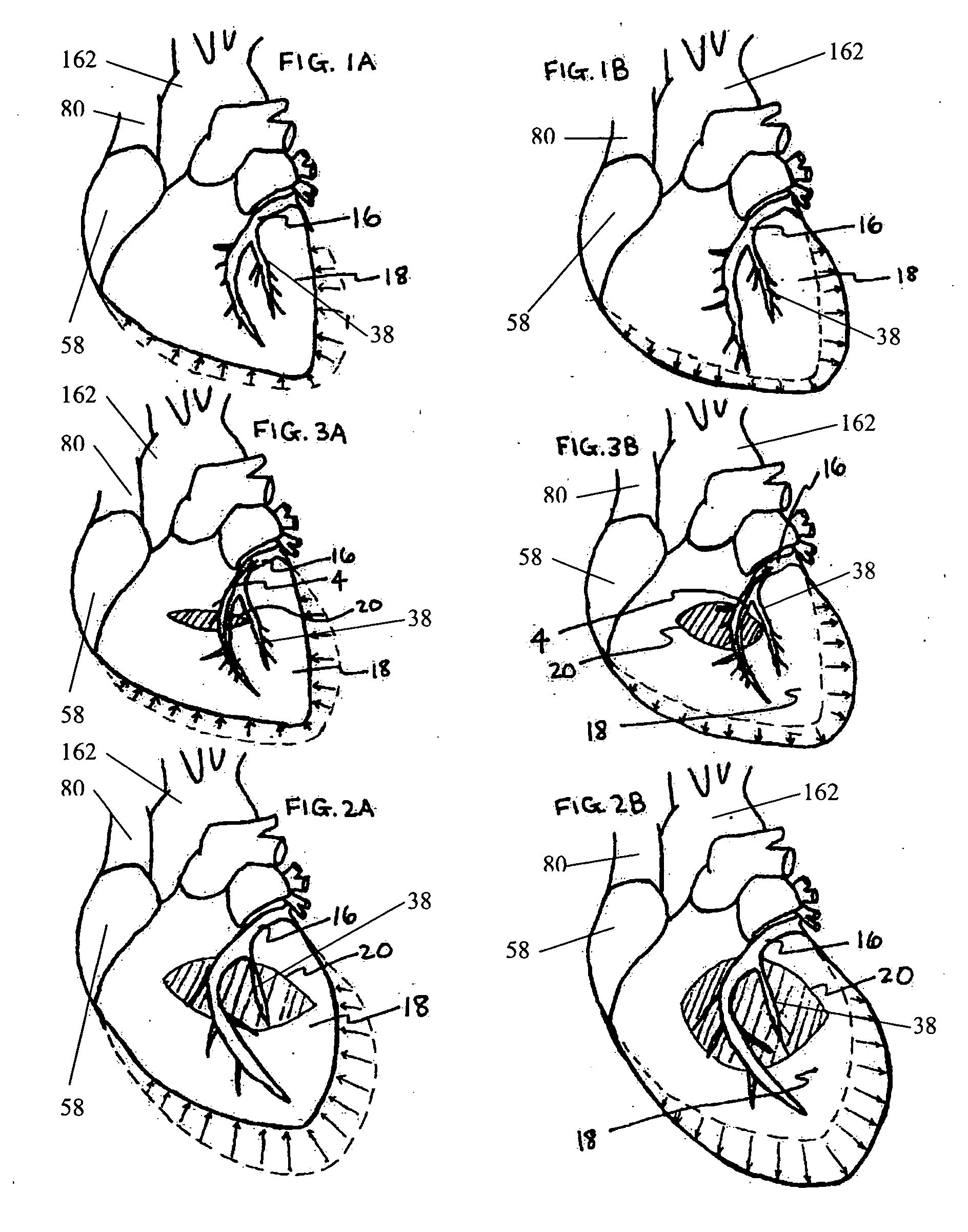
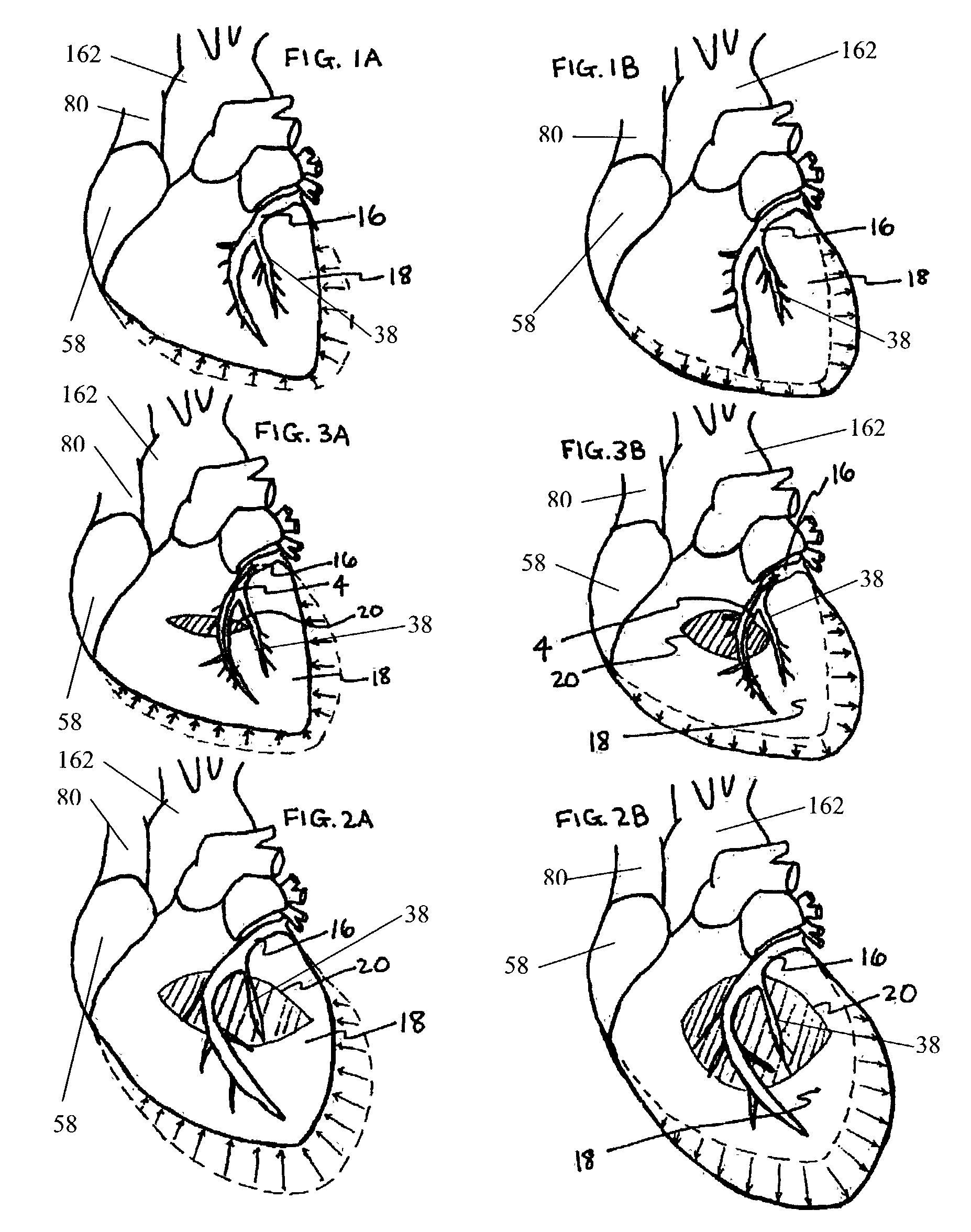
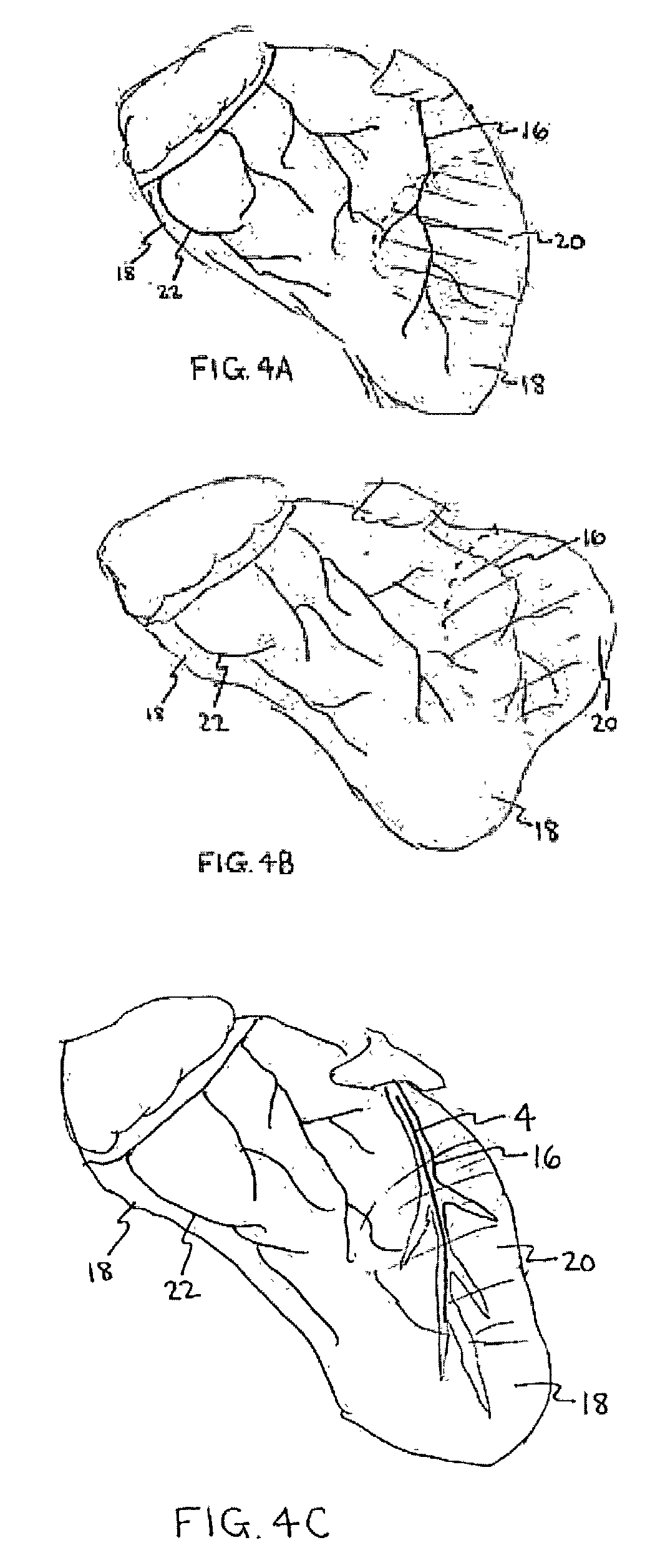
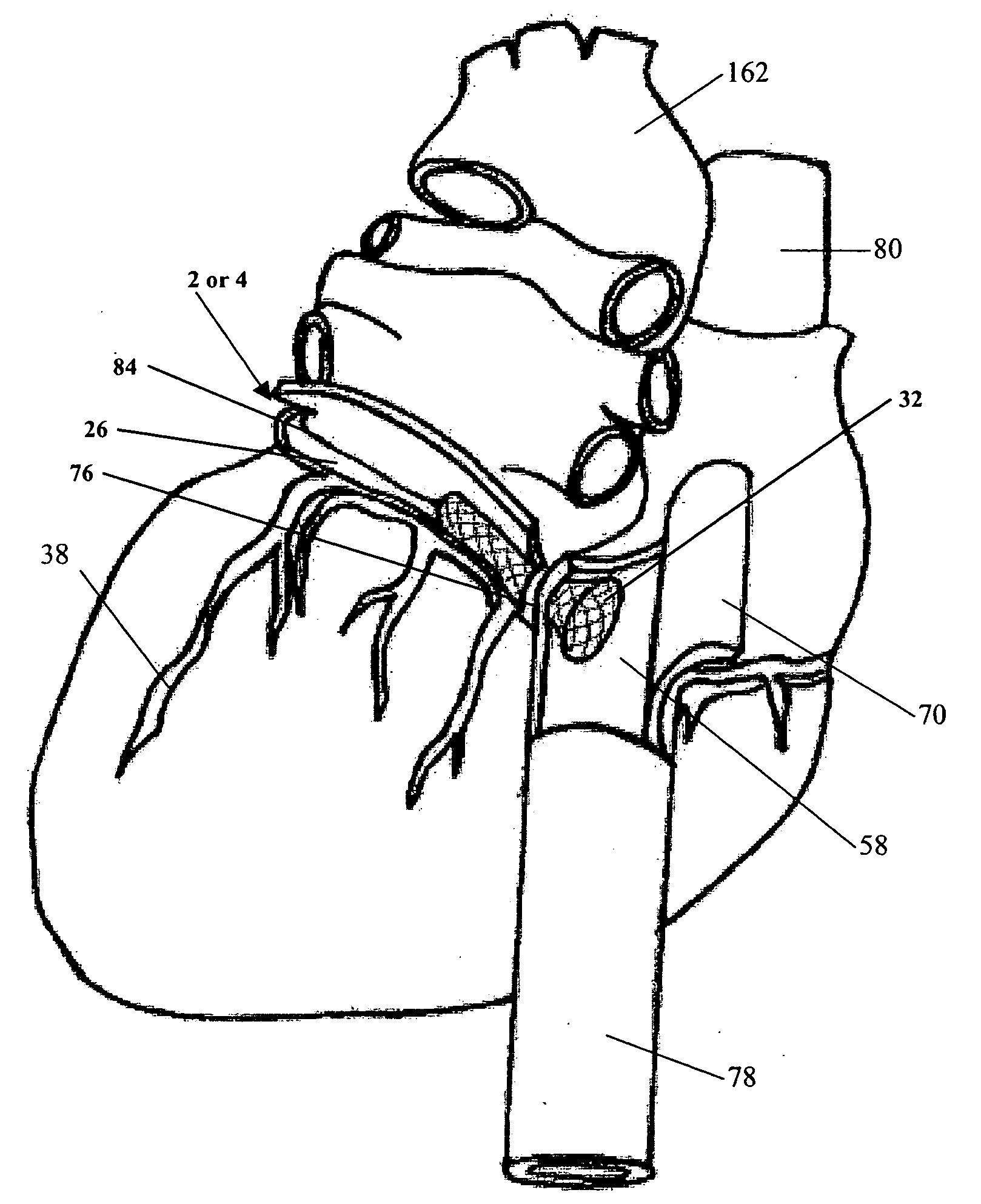
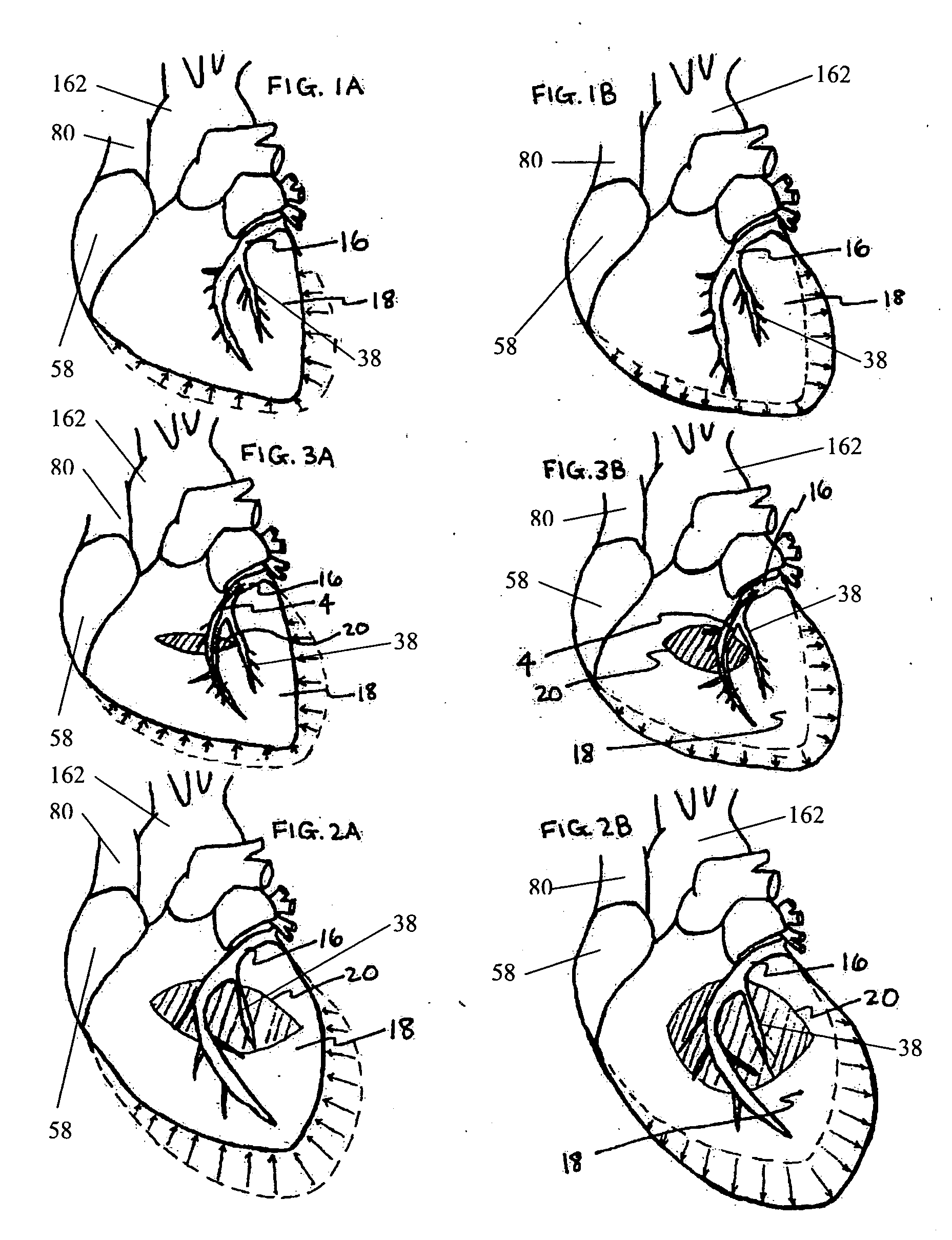
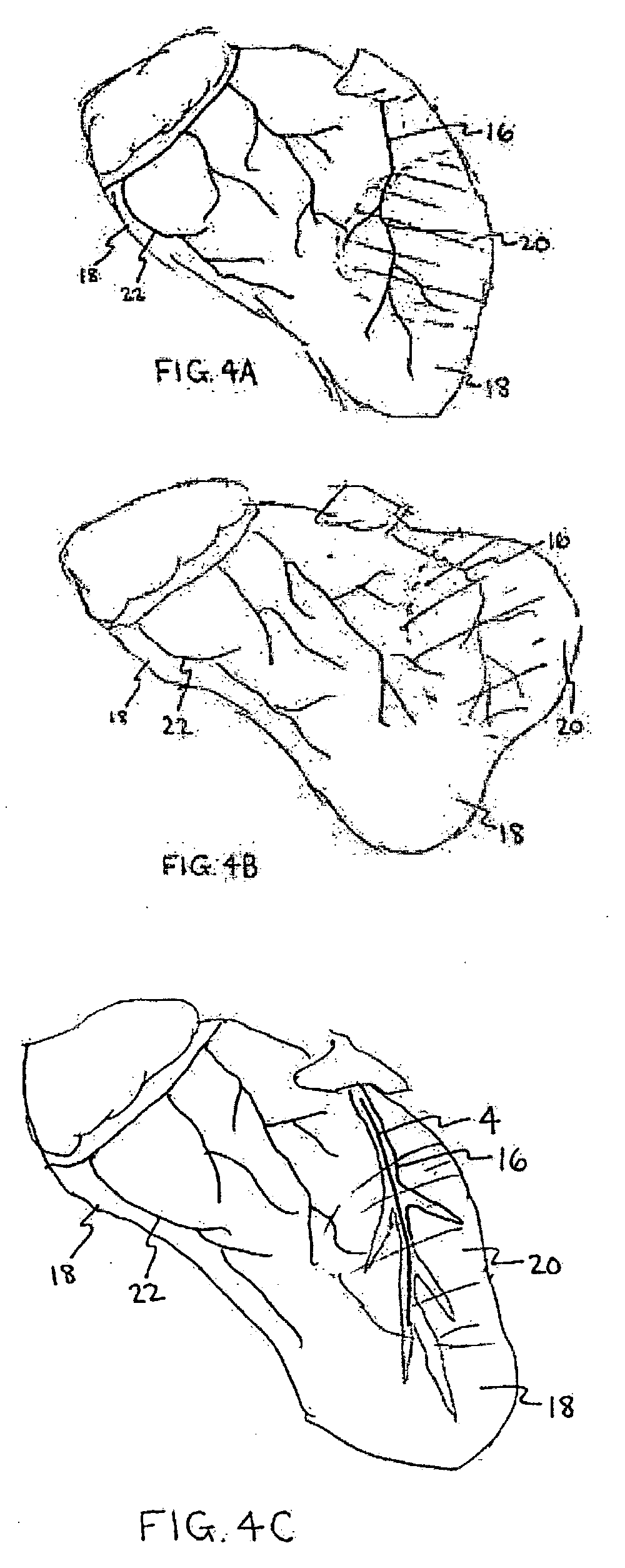
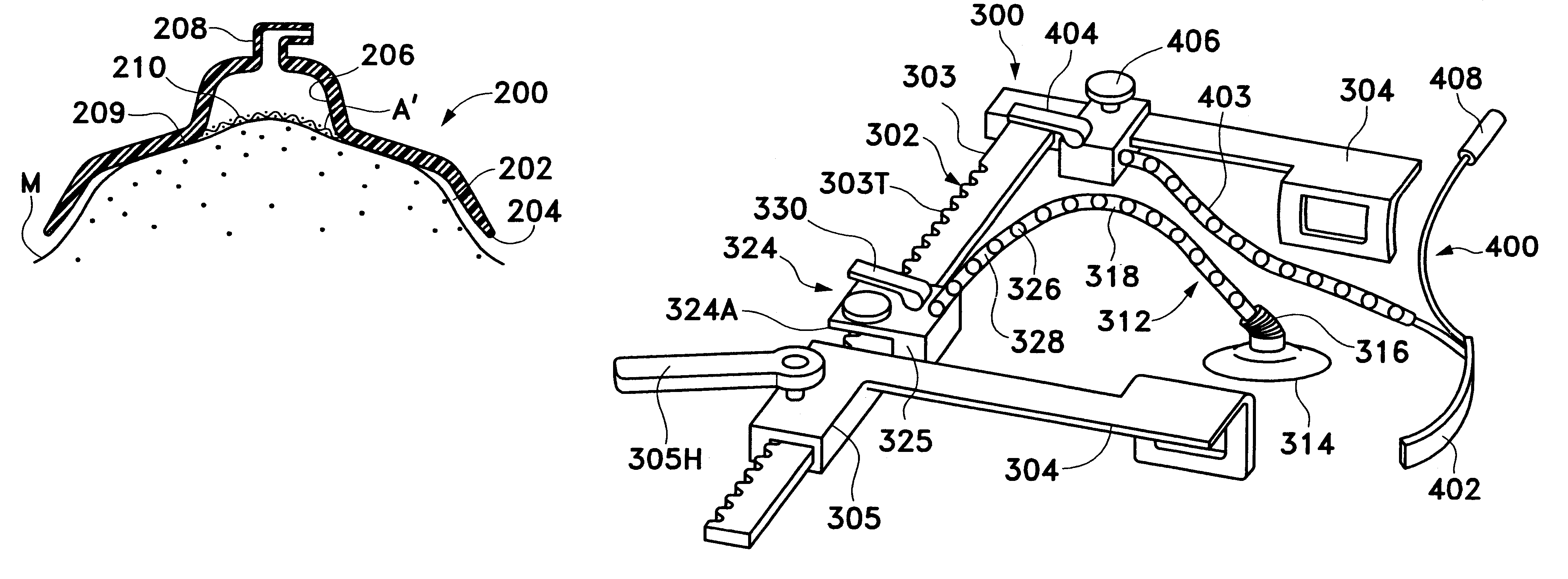
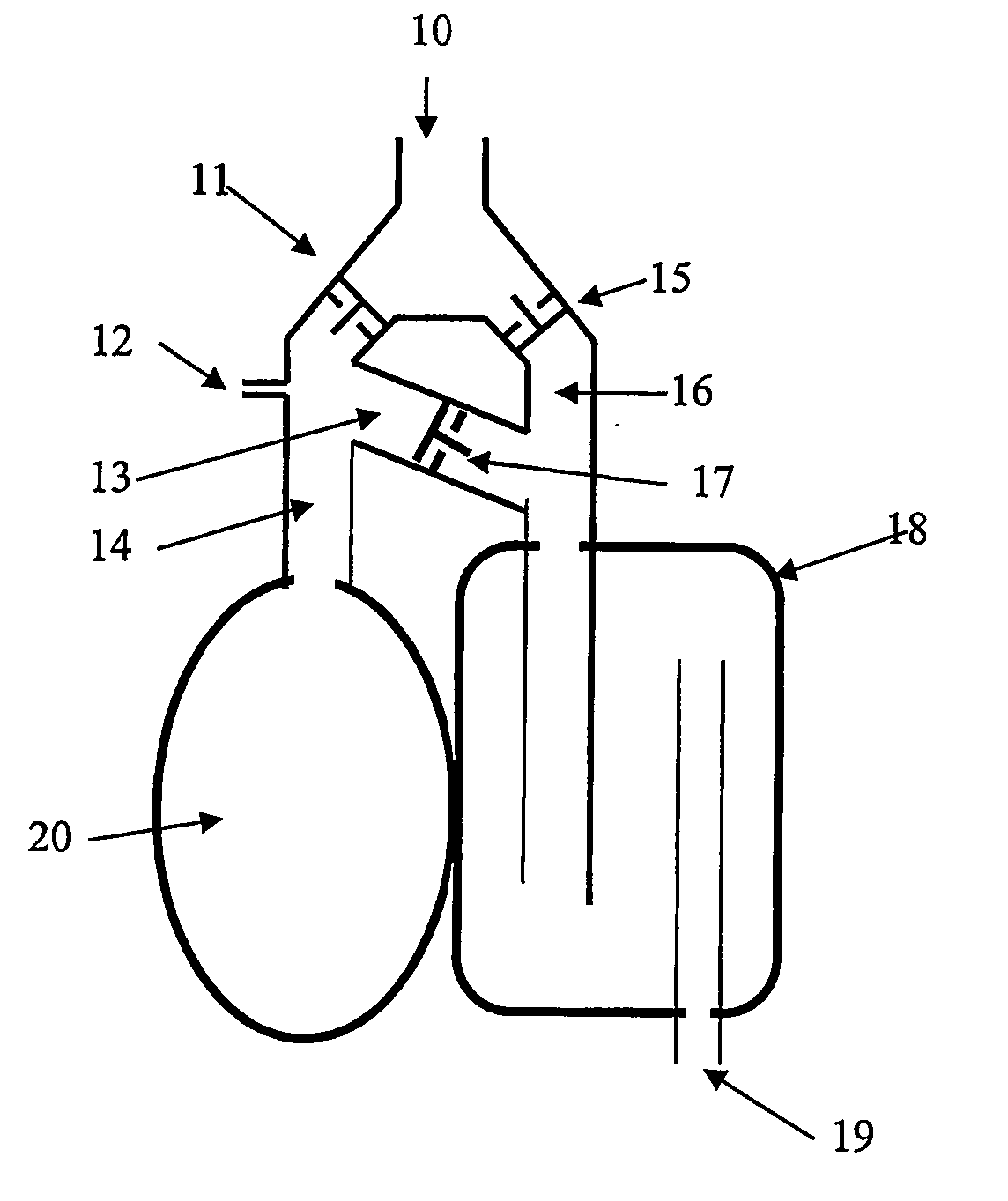
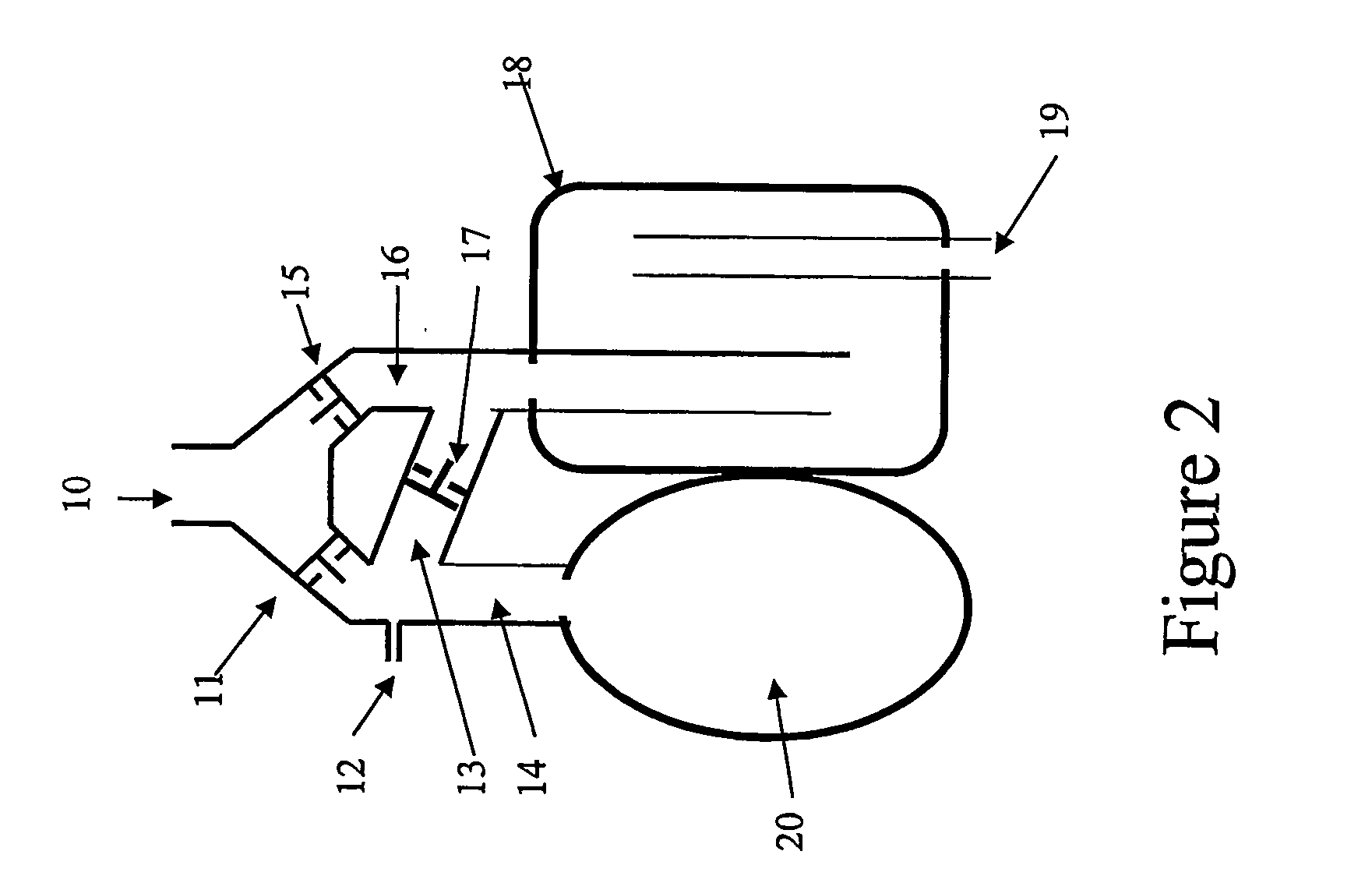
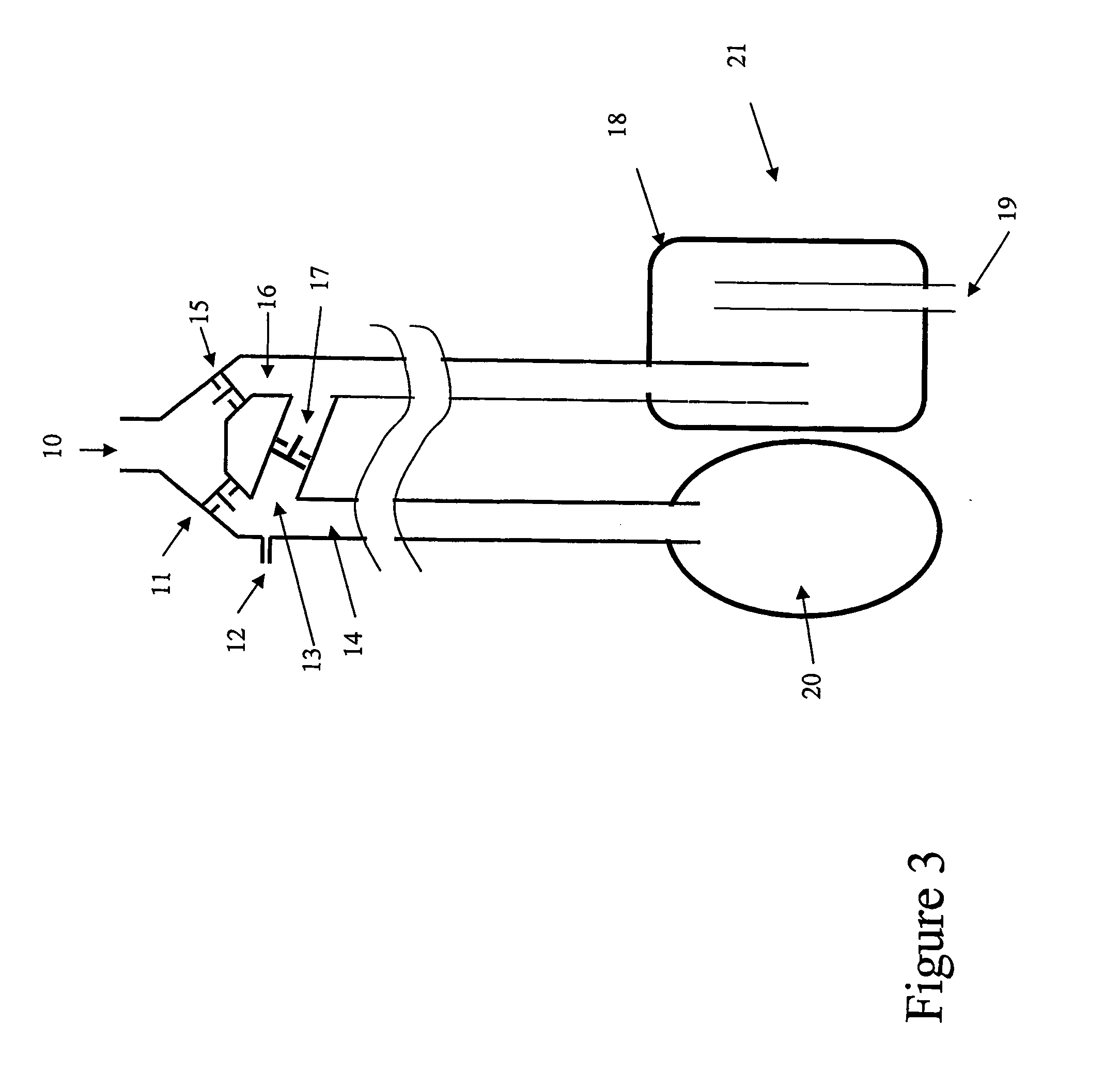
Device to permit offpump beating heart coronary bypass surgery
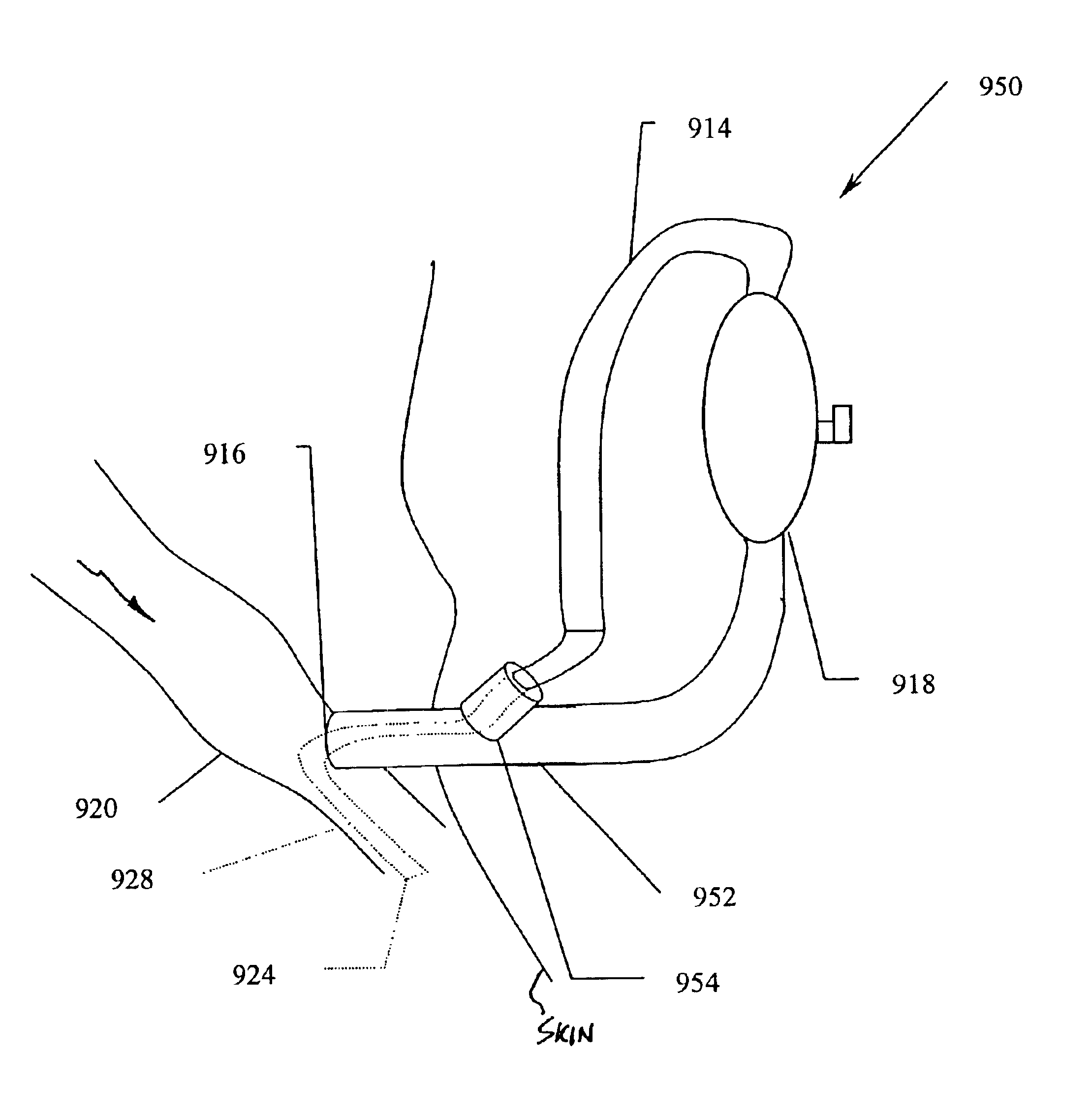
InactiveUS6019722ALess effectEliminate needSurgical pincettesProsthesisLess invasive surgeryCardiac retractor
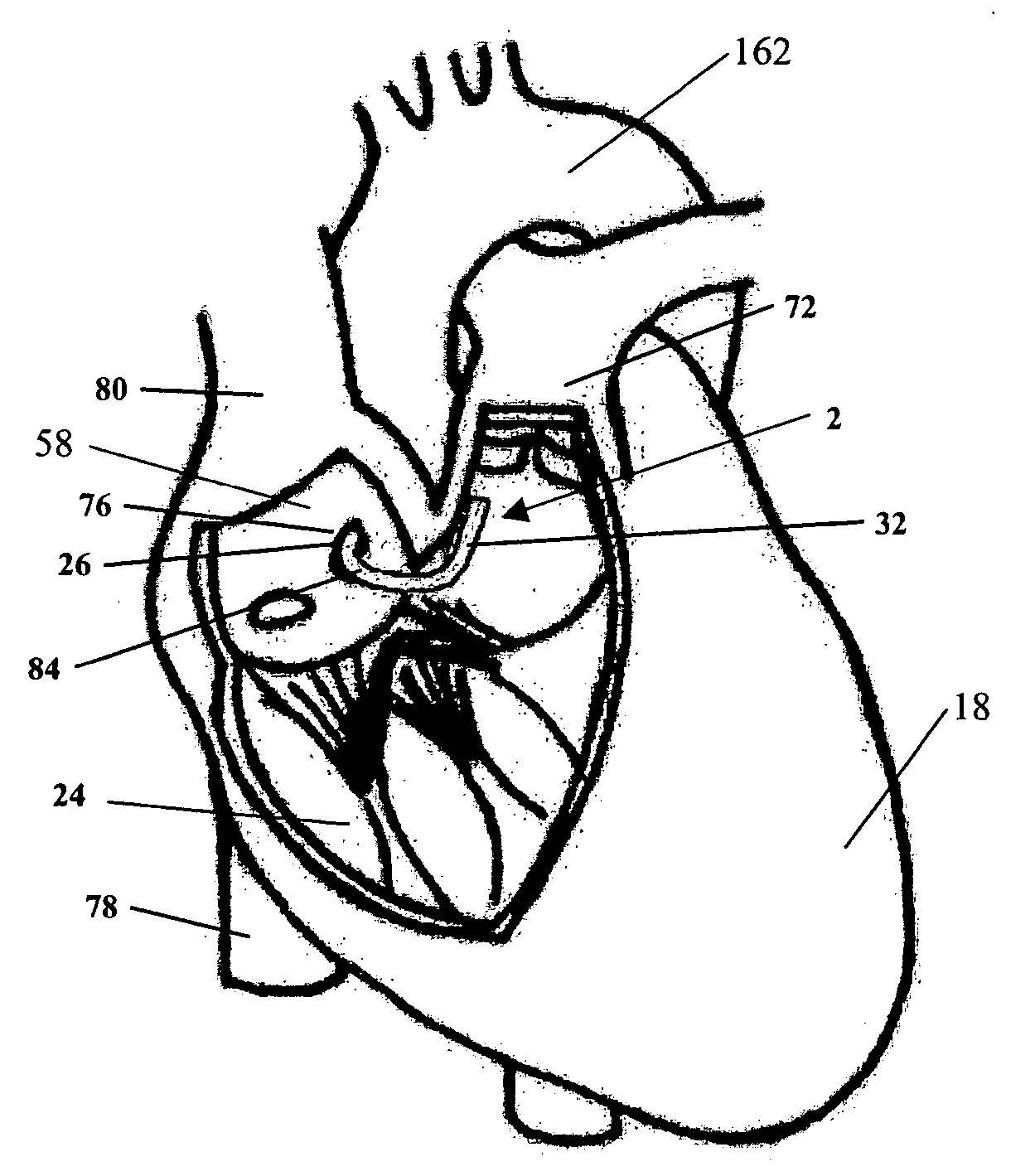
A heart retractor links lifting of the heart and regional immobilization which stops one part of the heart from moving to allow expeditious suturing while permitting other parts of the heart to continue to function whereby coronary surgery can be performed on a beating heart while maintaining cardiac output unabated and uninterrupted. Circumflex coronary artery surgery can be performed using the heart retractor of the present invention. The retractor includes a plurality of flexible arms and a plurality of rigid arms as well as a surgery target immobilizing element. One form of the retractor can be used in minimally invasive surgery, while other forms of the retractor can accommodate variations in heart size and paracardial spacing.
Owner:MAQUET CARDIOVASCULAR LLC
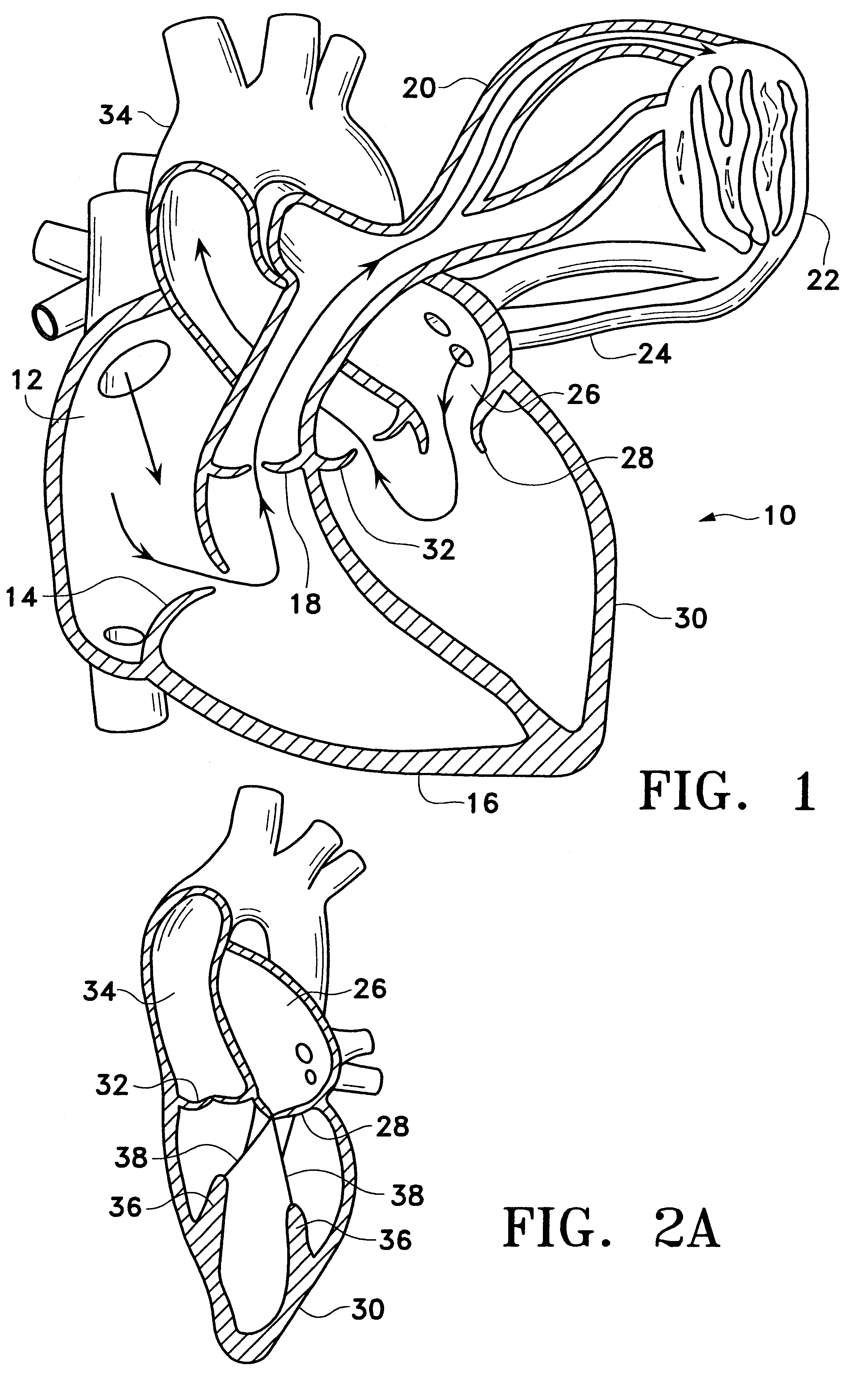
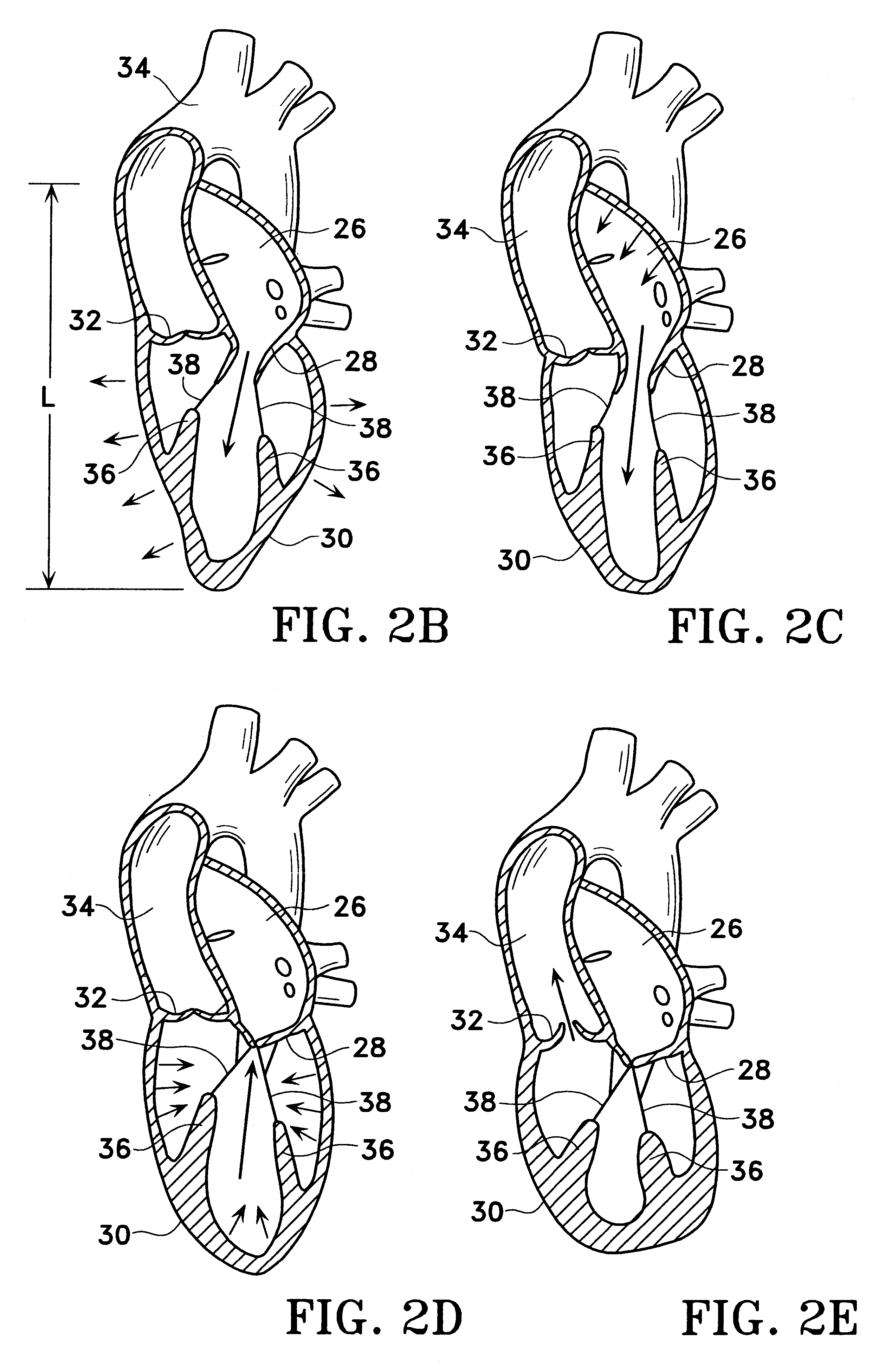
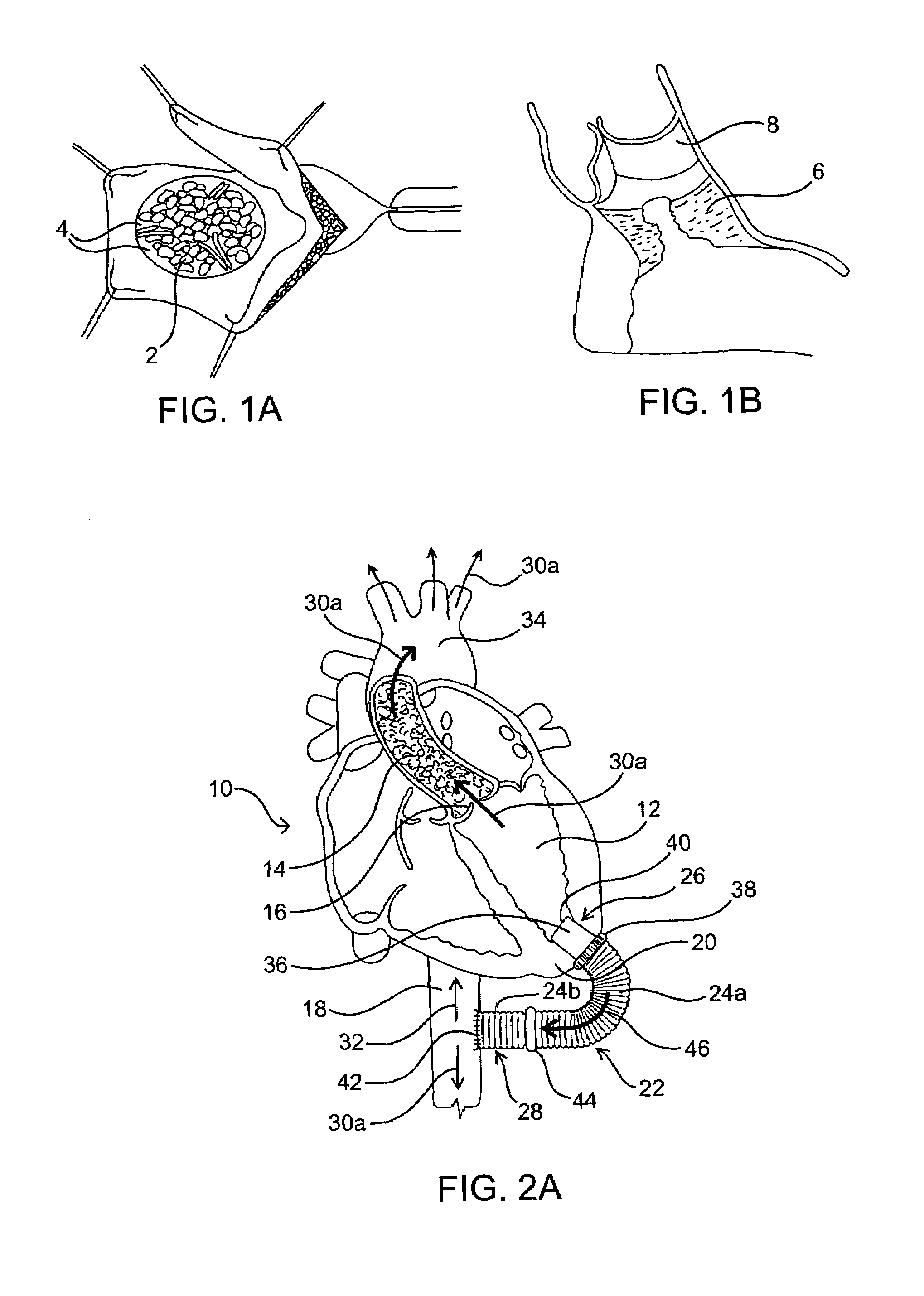
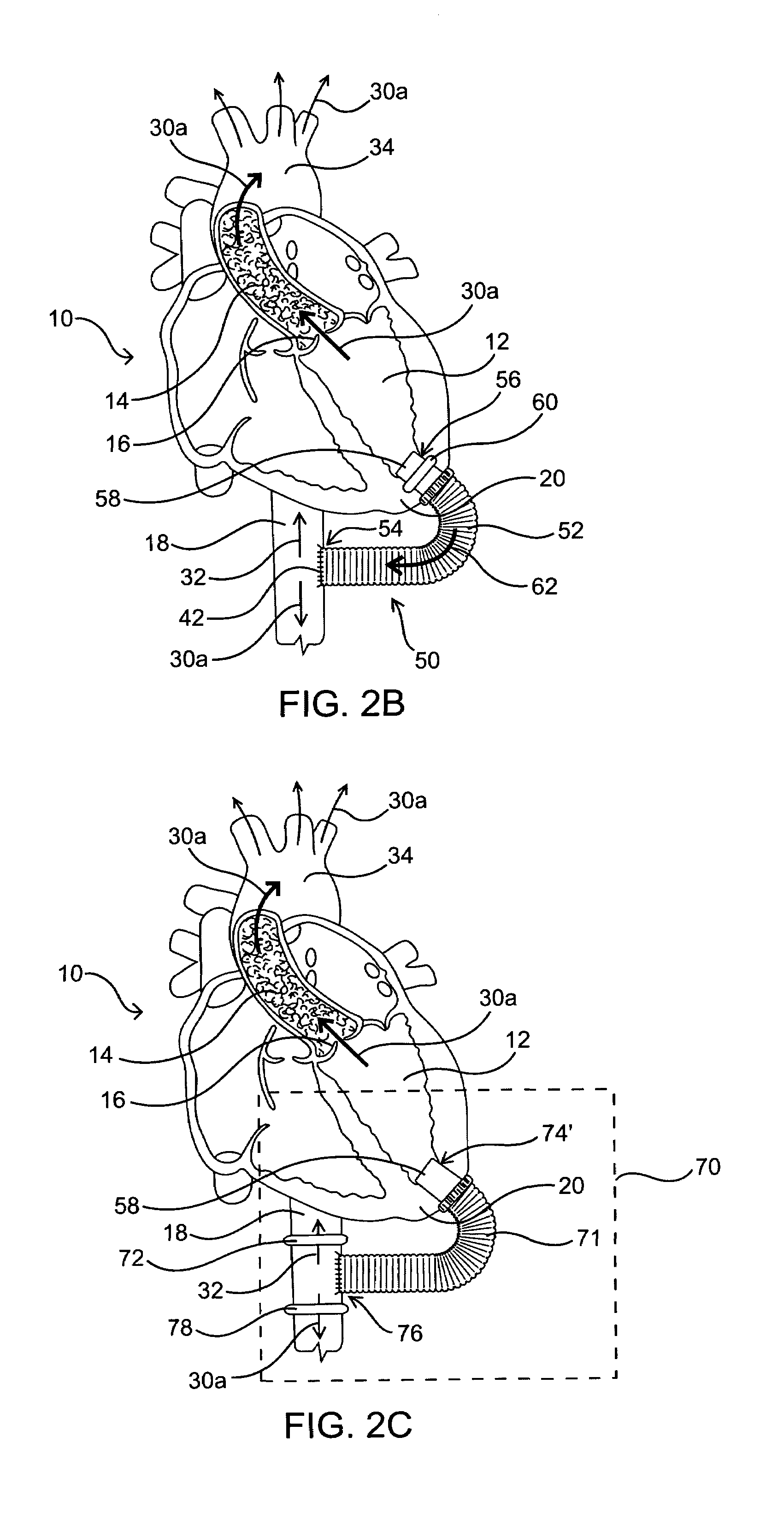
Systems for heart treatment
InactiveUS20050197694A1Reduce stressReduce/limit volumeSuture equipmentsElectrotherapyLeft ventricular sizeTherapeutic treatment
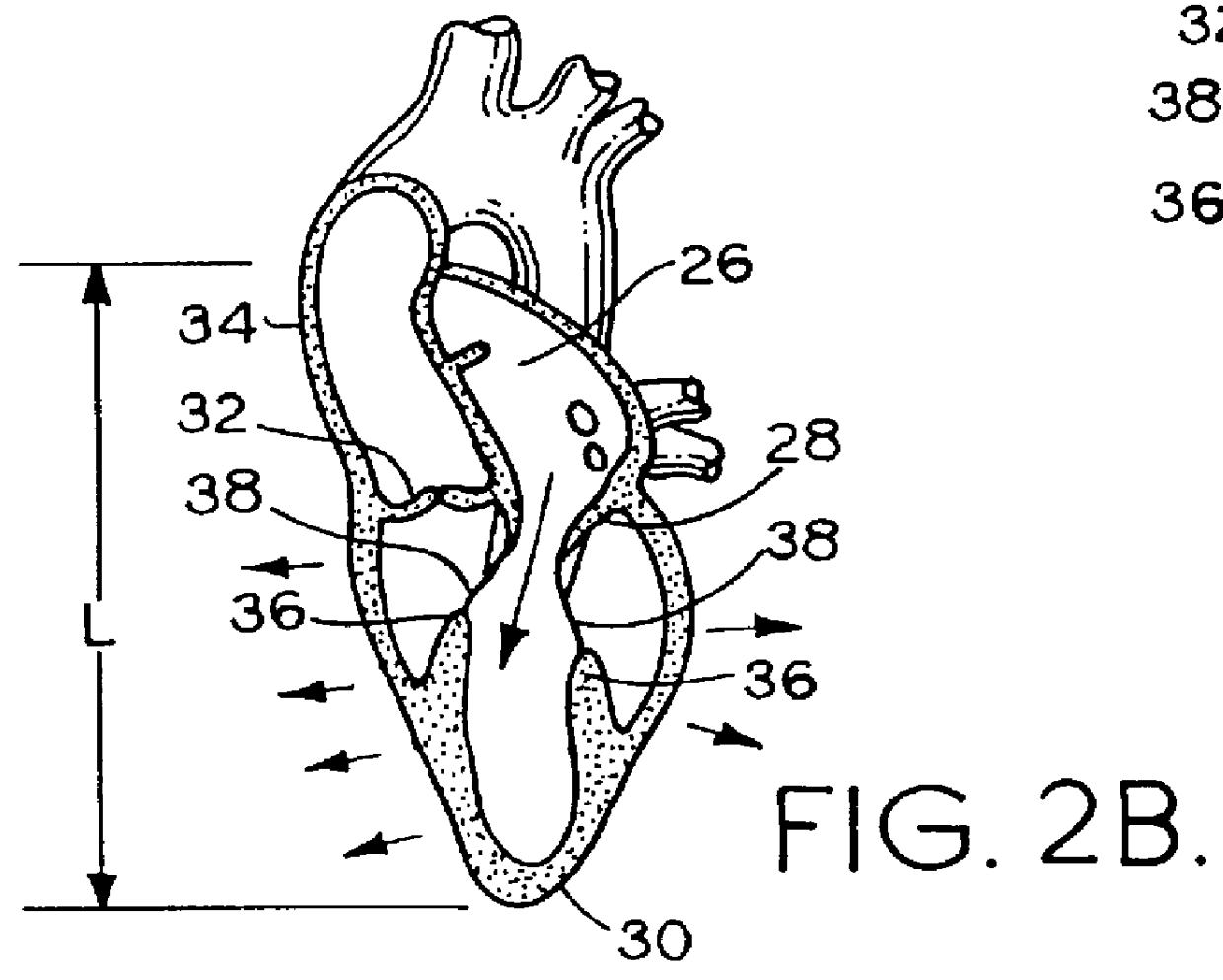
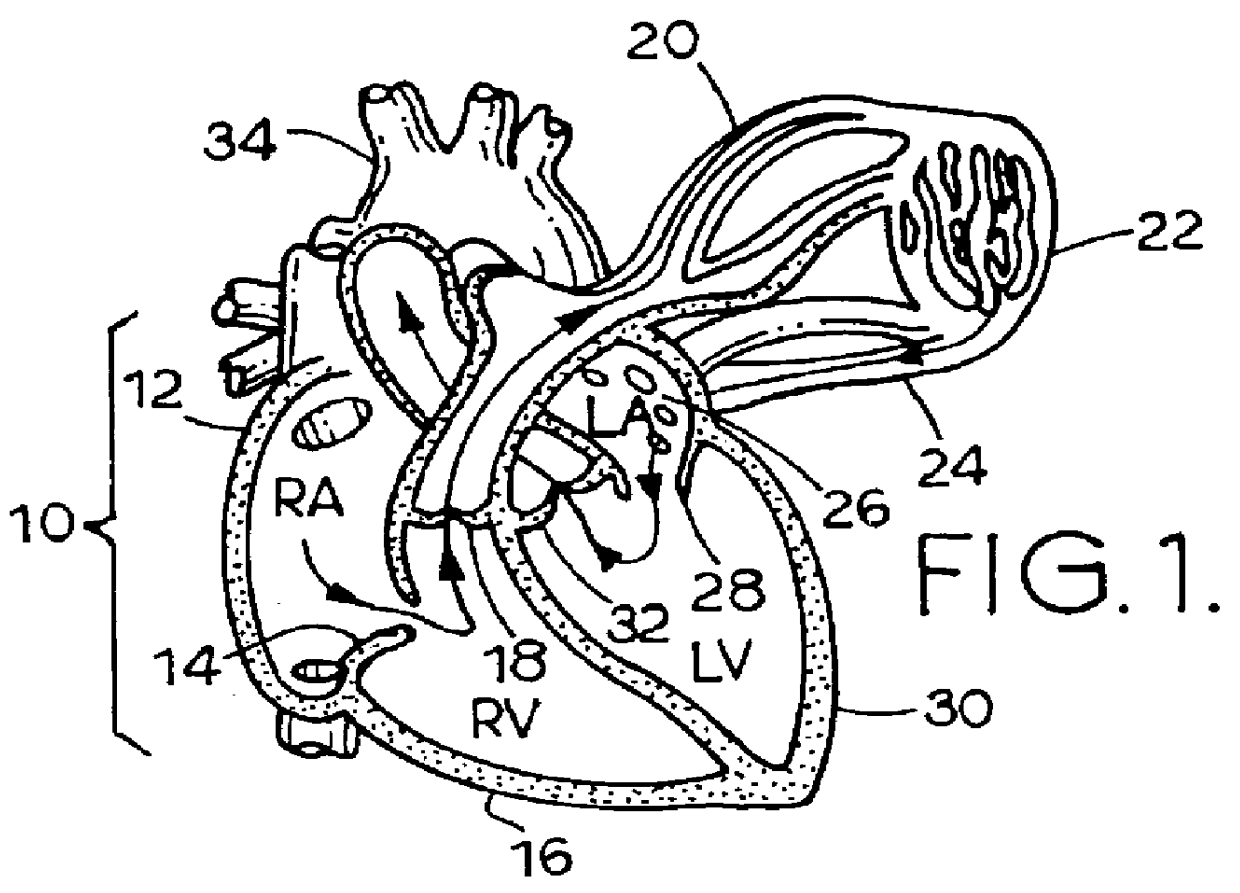
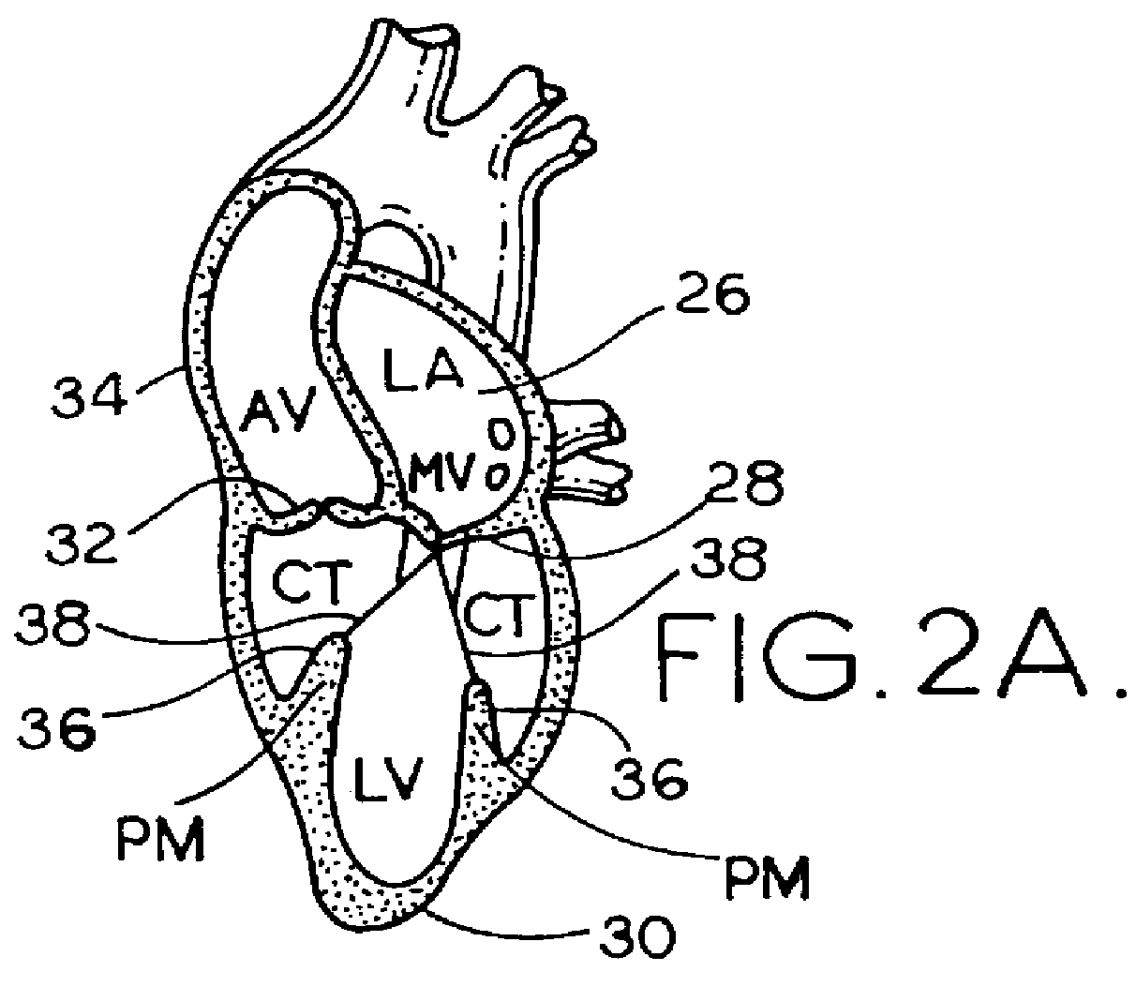
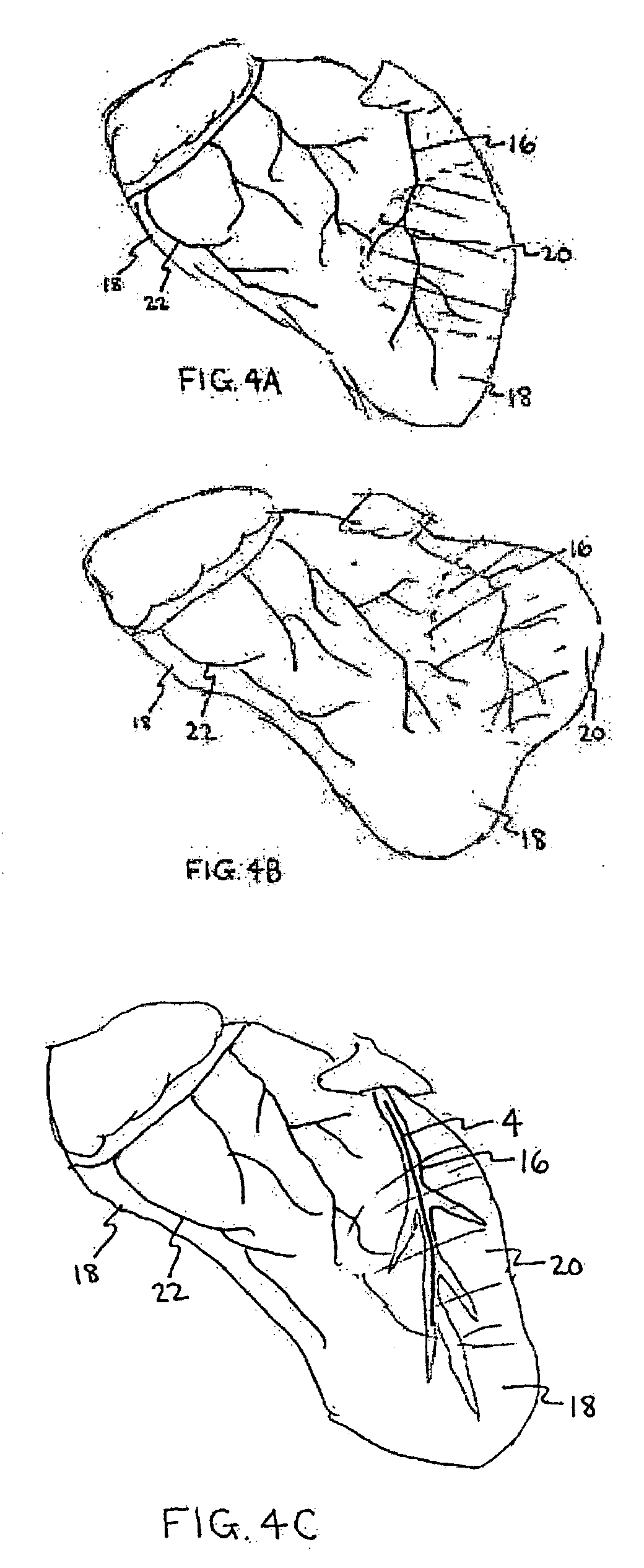
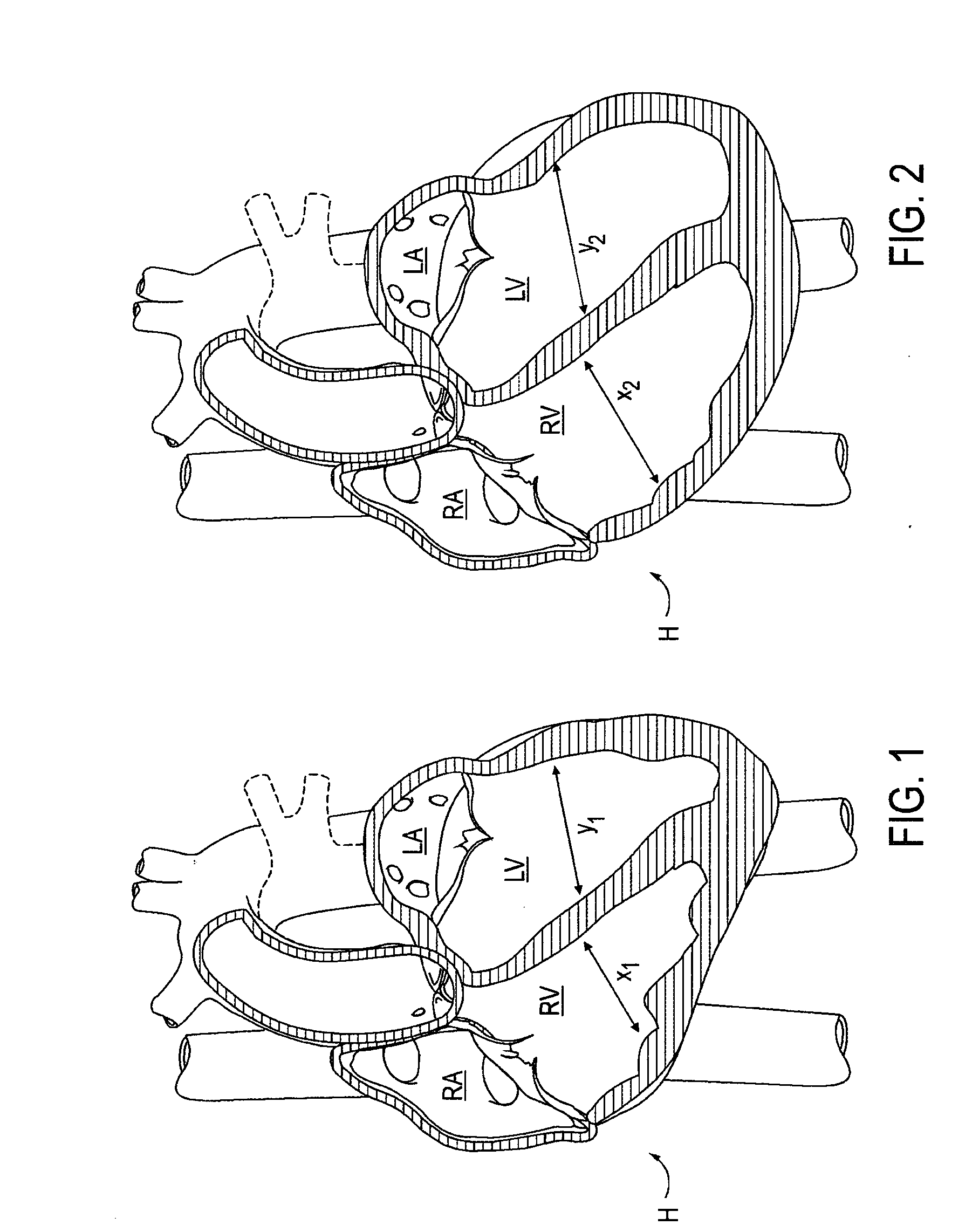
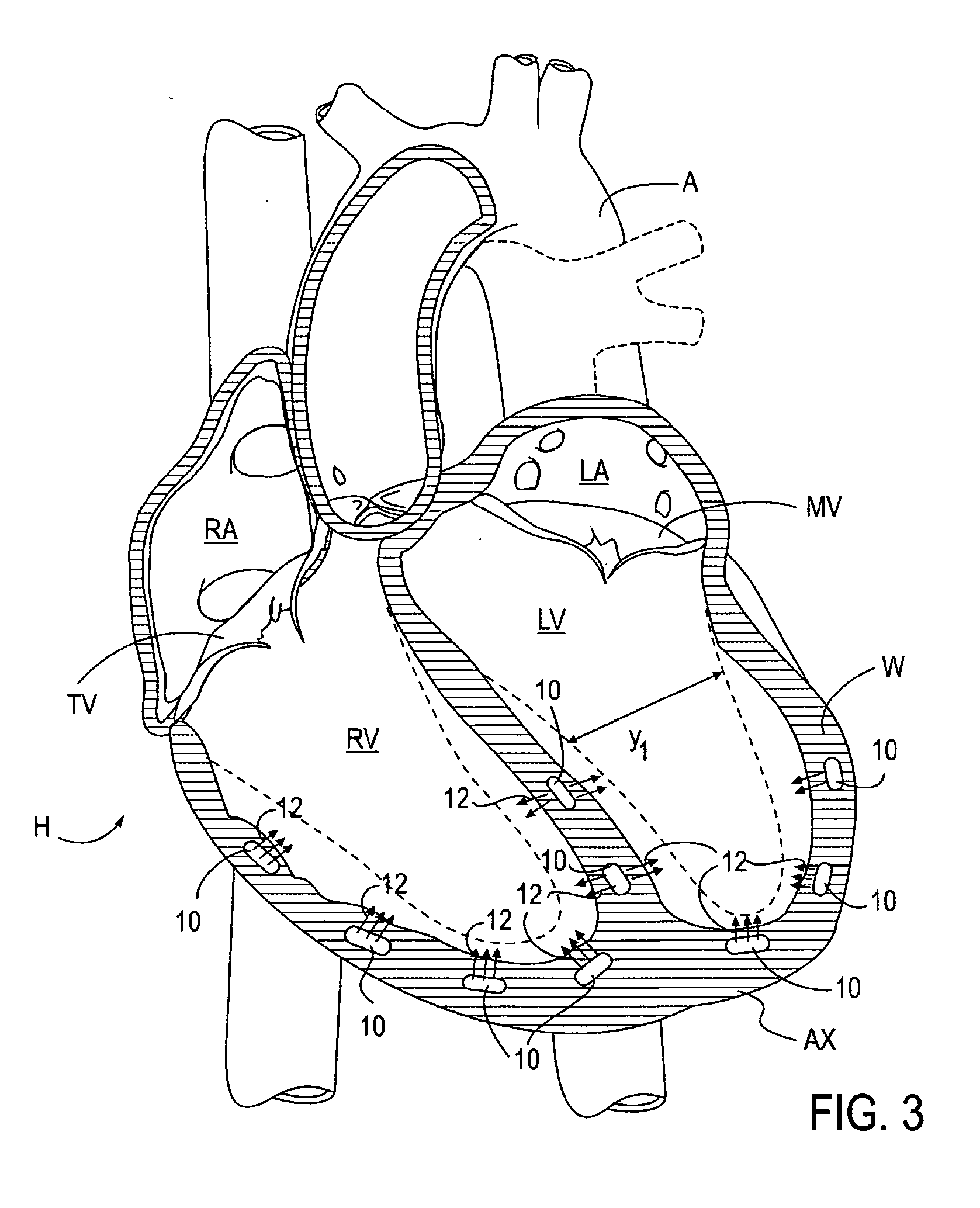
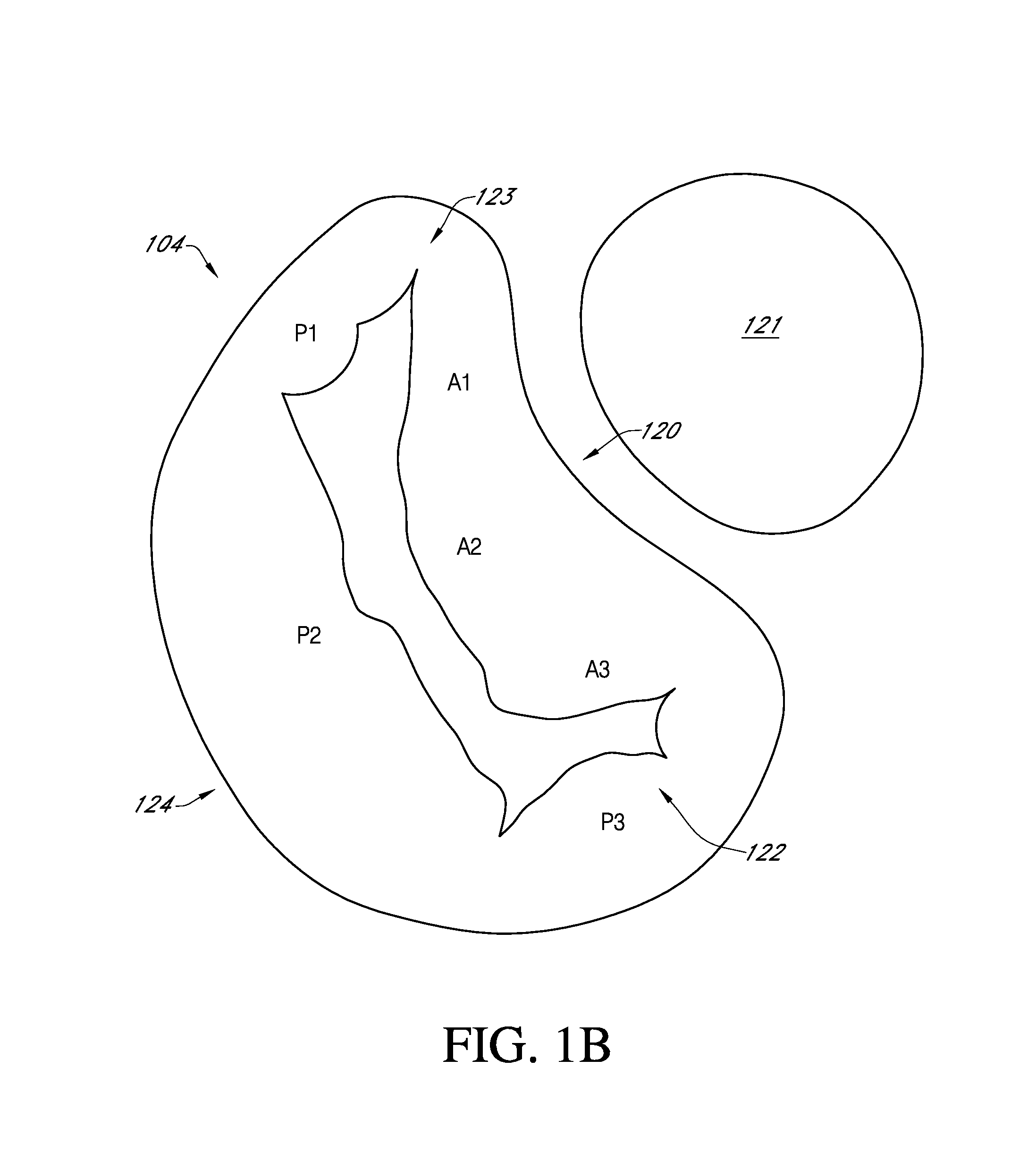
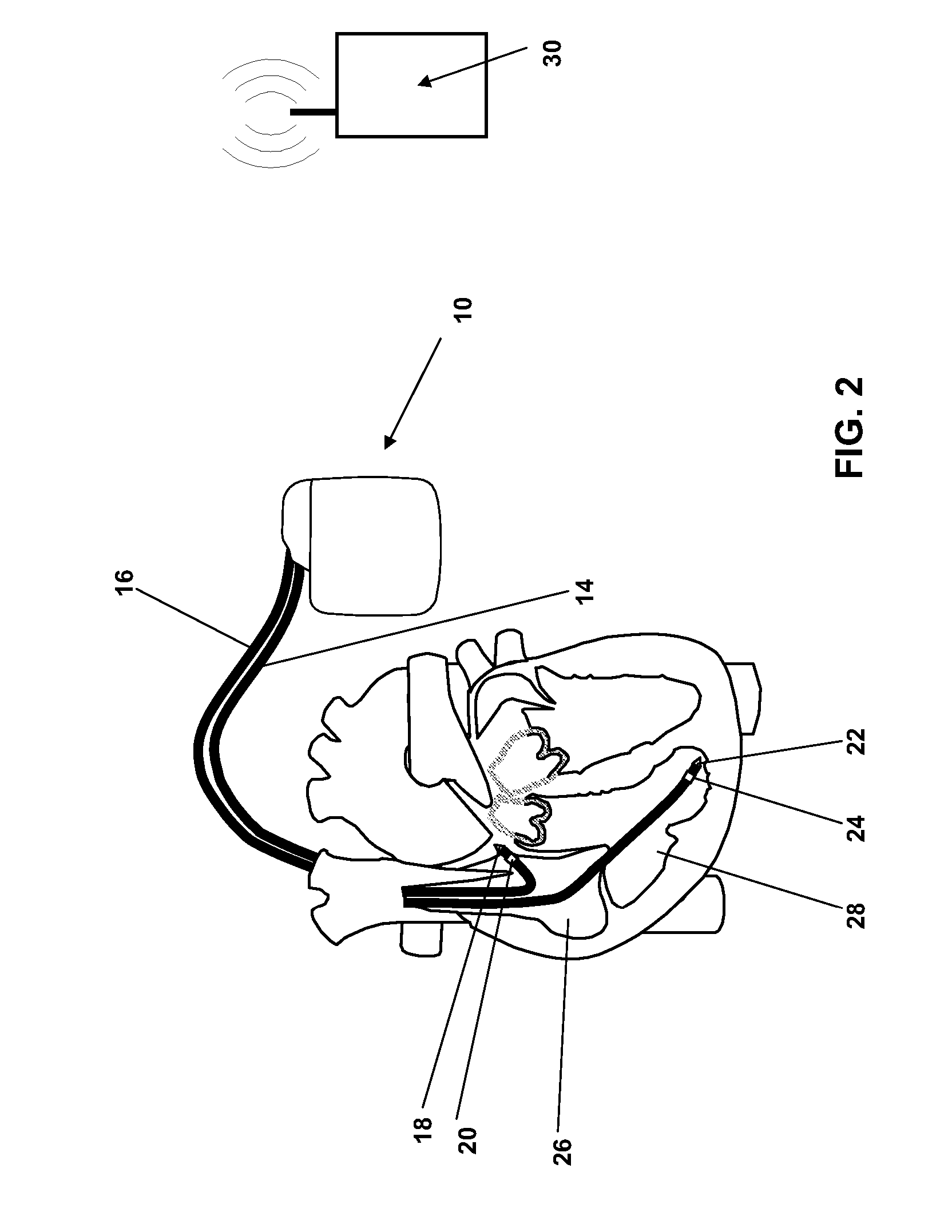
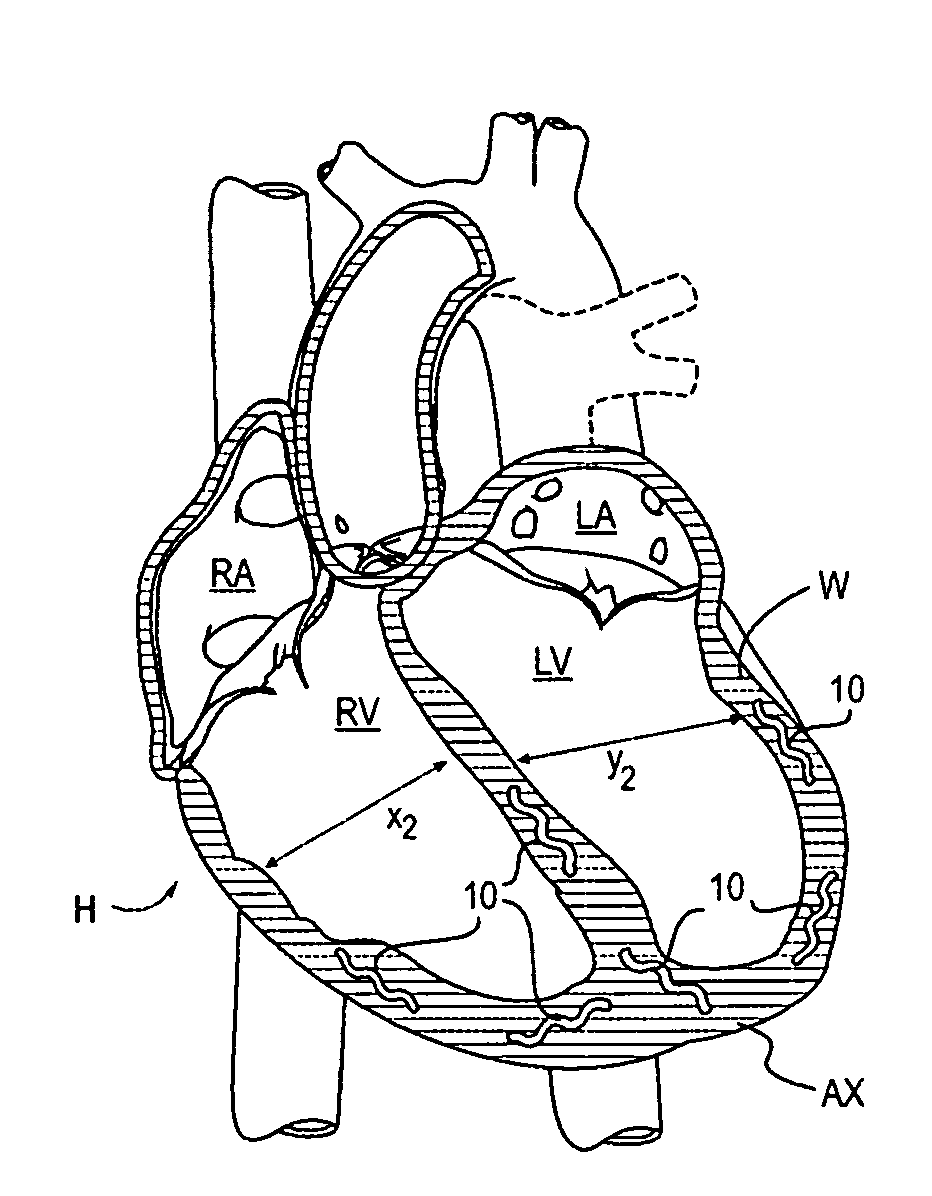
Described are devices and methods for treating degenerative, congestive heart disease and related valvular dysfunction. Percutaneous and minimally invasive surgical tensioning structures offer devices that mitigate changes in the ventricular structure (i.e., remodeling) and deterioration of global left ventricular performance related to tissue damage precipitating from ischemia, acute myocardial infarction (AMI) or other abnormalities. These tensioning structures can be implanted within various major coronary blood-carrying conduit structures (arteries, veins and branching vessels), into or through myocardium, or into engagement with other anatomic structures that impact cardiac output to provide tensile support to the heart muscle wall which resists diastolic filling pressure while simultaneously providing a compressive force to the muscle wall to limit, compensate or provide therapeutic treatment for congestive heart failure and / or to reverse the remodeling that produces an enlarged heart.
Owner:EXTENSIA MEDICAL
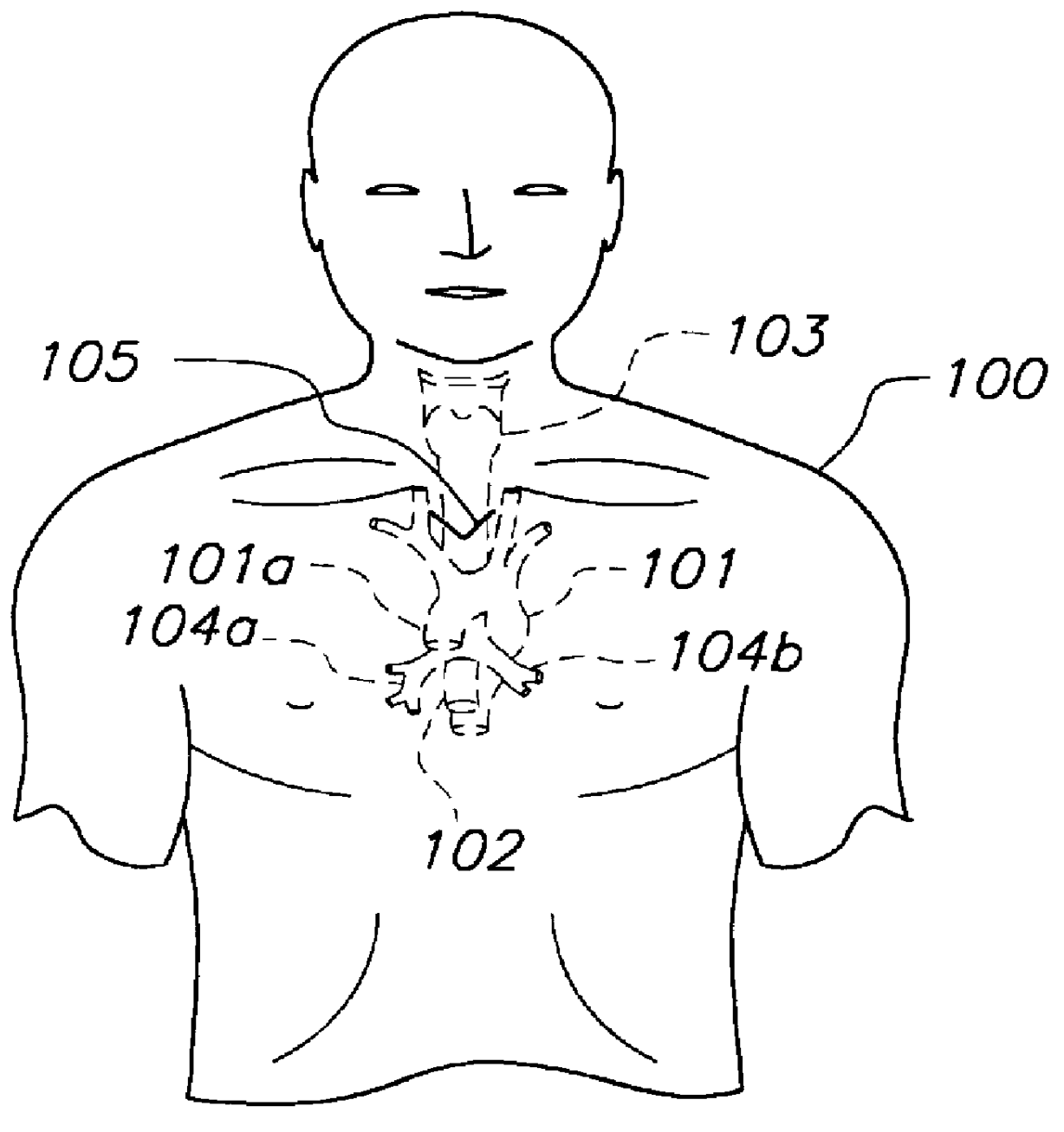
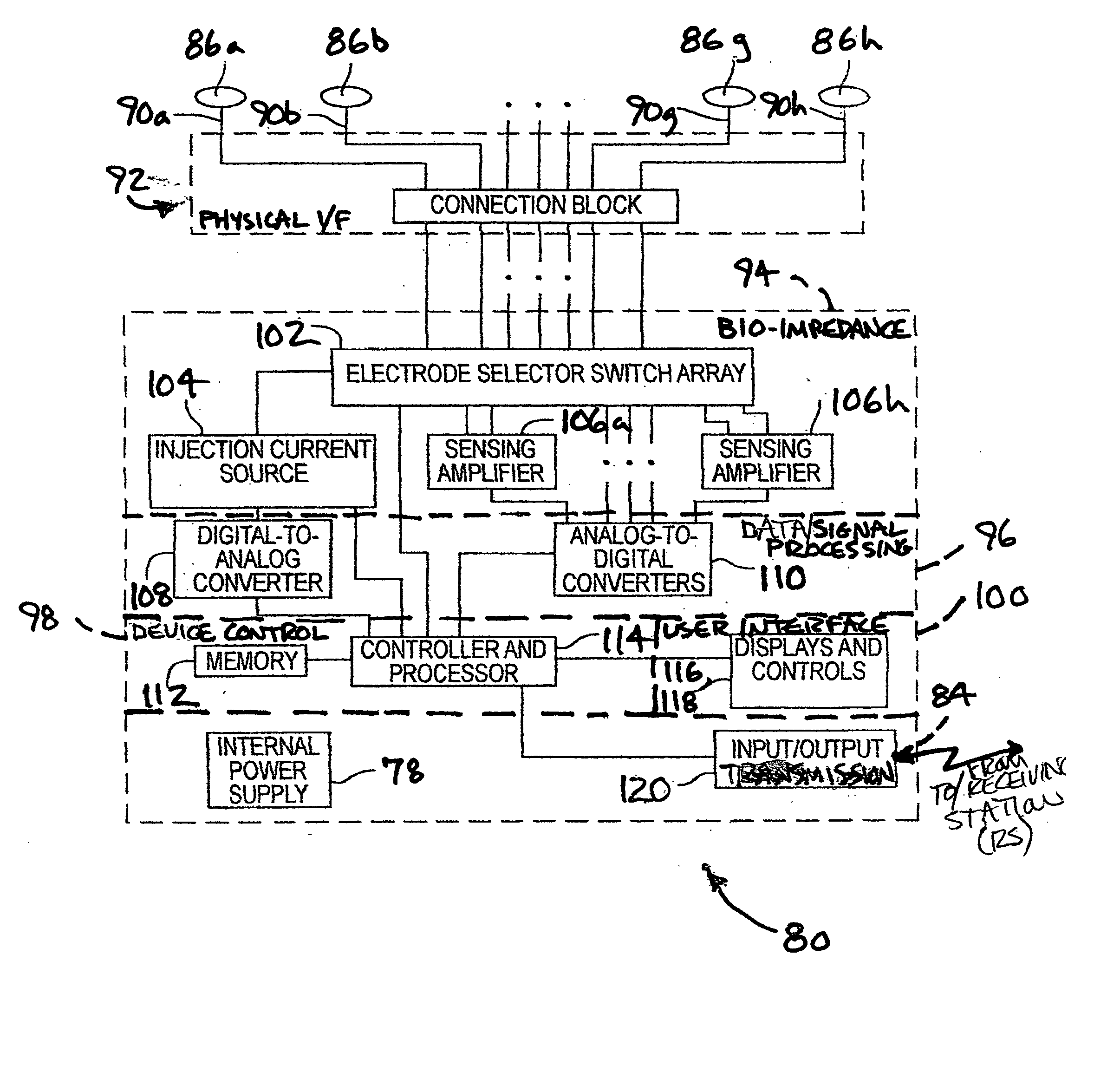
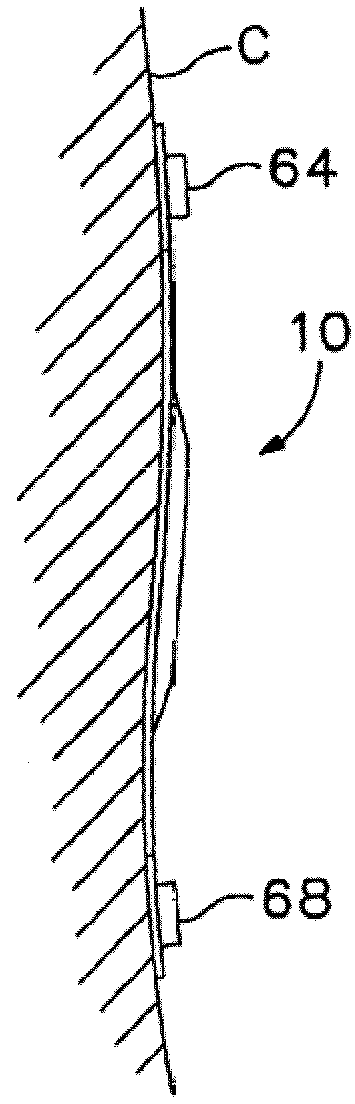
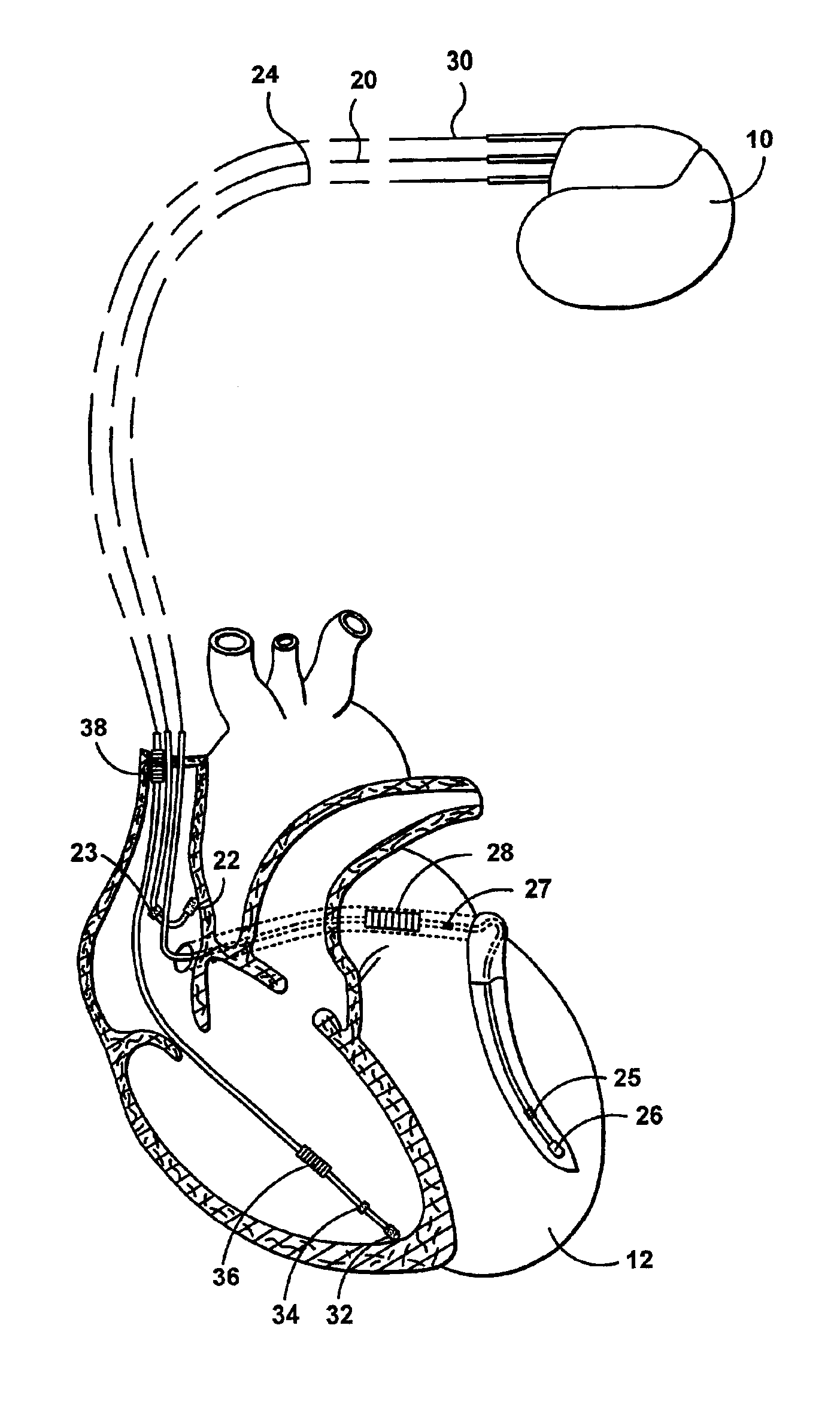
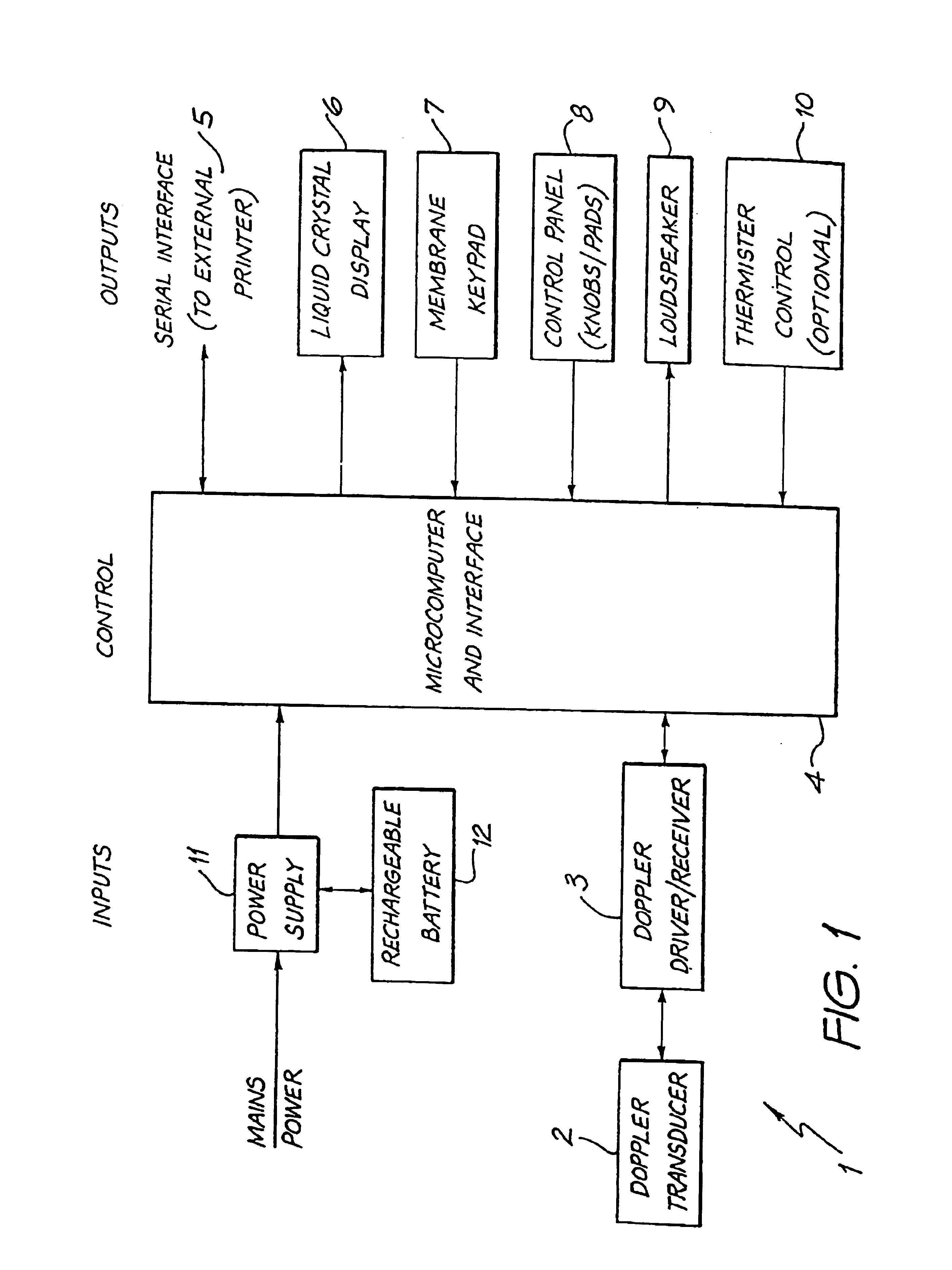
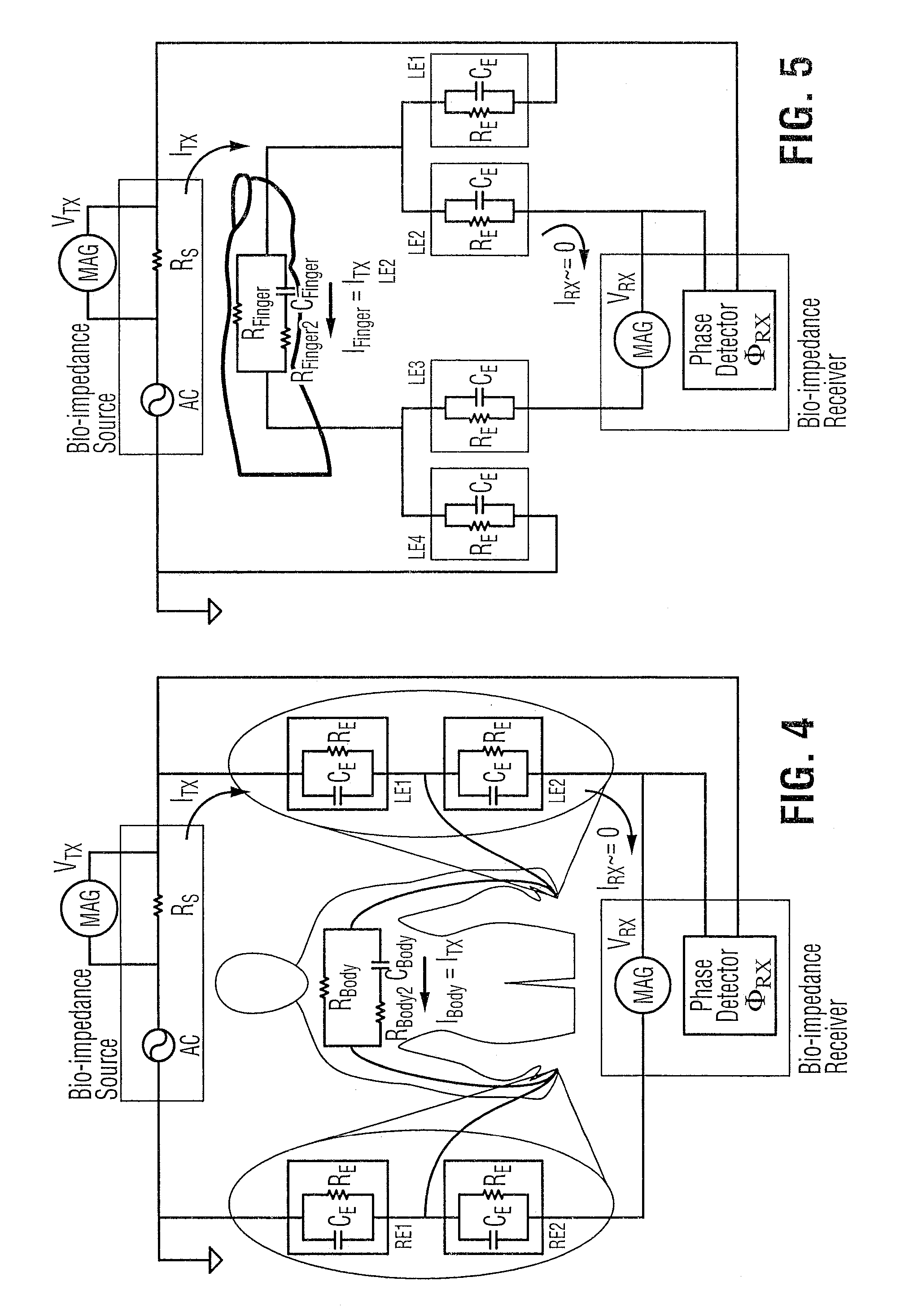
Apparatus and methods of bioelectrical impedance analysis of blood flow
InactiveUS6095987AAccurately and non-invasively and continuously measuring cardiac outputCatheterSensorsBioelectrical impedance analysisCardiac pacemaker electrode
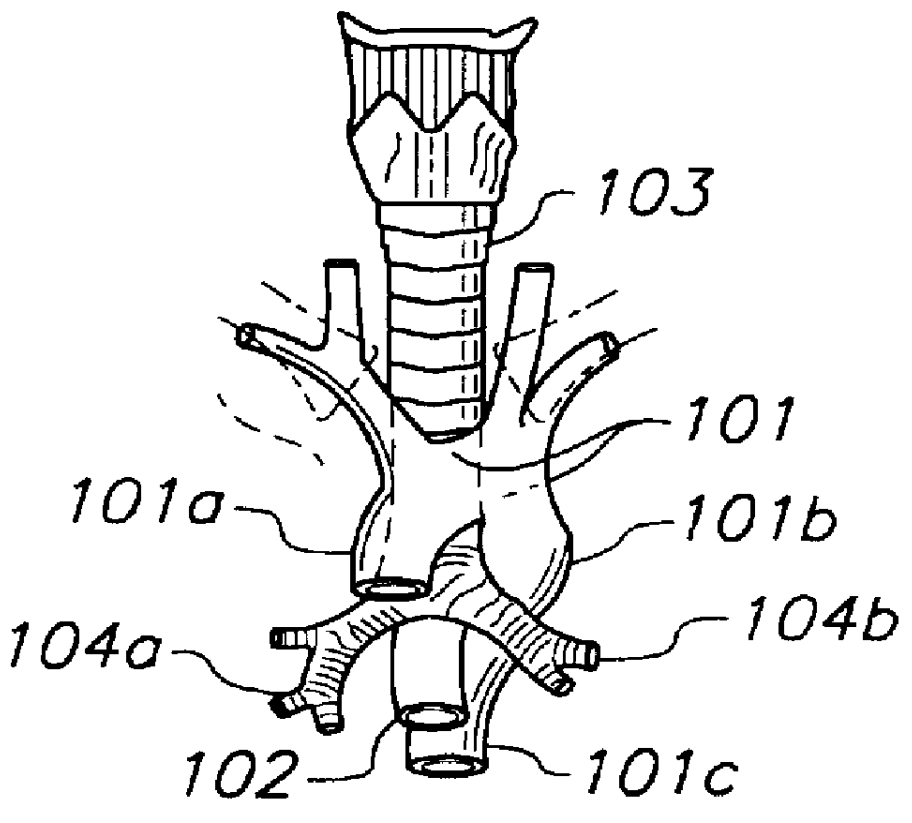
Apparatus and methods are provided for monitoring cardiac output using bioelectrical impedance techniques in which first and second electrodes are placed in the trachea and / or bronchus in the vicinity of the ascending aorta, while an excitation current is injected into the thorax via first and second current electrodes, so that bioelectrical impedance measurements based on the voltage drop sensed by the first and second electrodes reflect voltage changes induced primarily by blood flow dynamics, rather than respiratory or non-cardiac related physiological effects. Additional sense electrodes may be provided, either internally, or externally, for which bioelectrical impedance values may be obtained. Methods are provided for computing cardiac output from bioelectrical impedance values. Apparatus and methods are also provided so that the measured cardiac output may be used to control administration of intravenous fluids to an organism or to optimize a heart rate controlled by a pacemaker.
Owner:ECOM MED
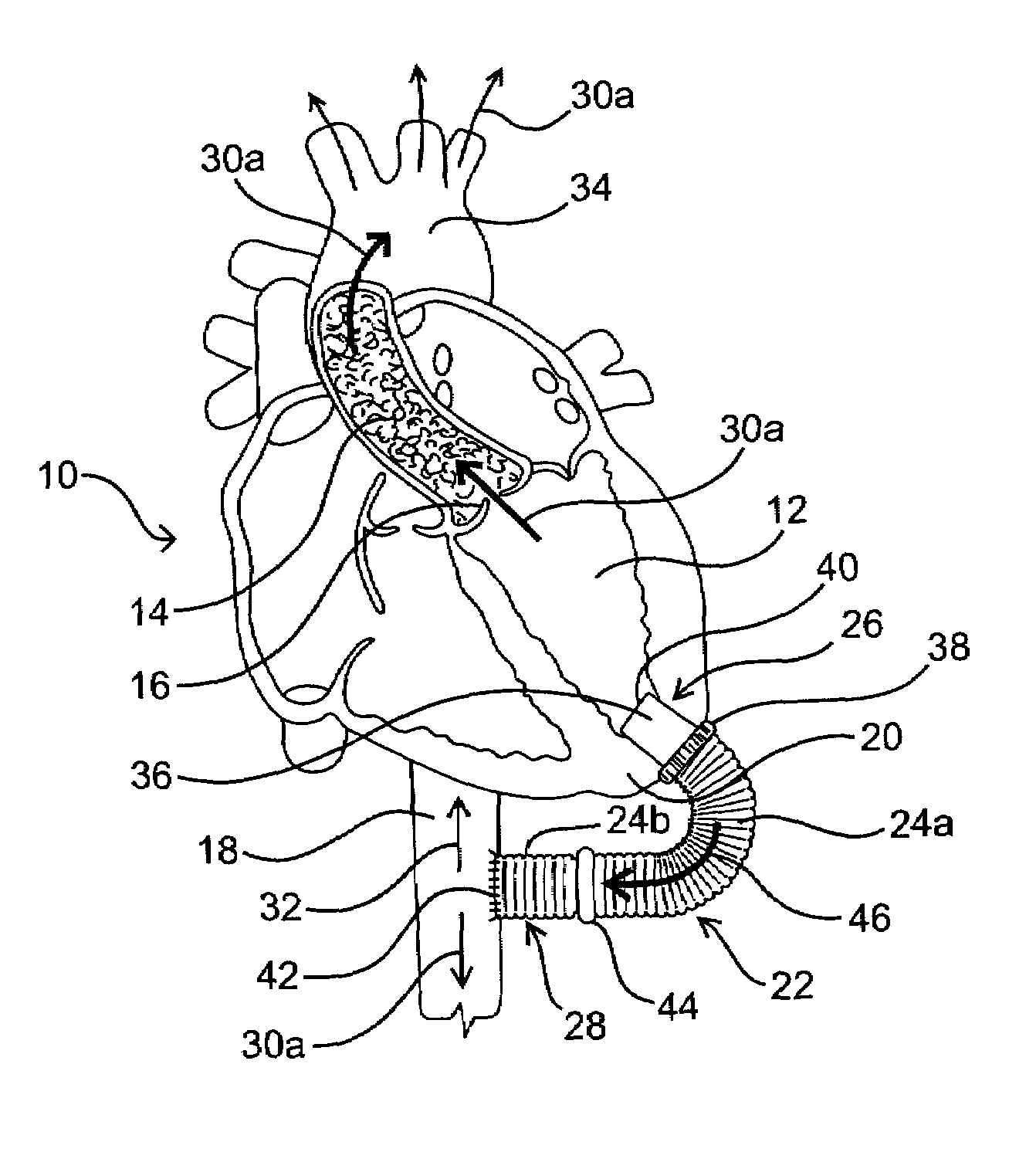
Magnetic devices and methods for reshaping heart anatomy
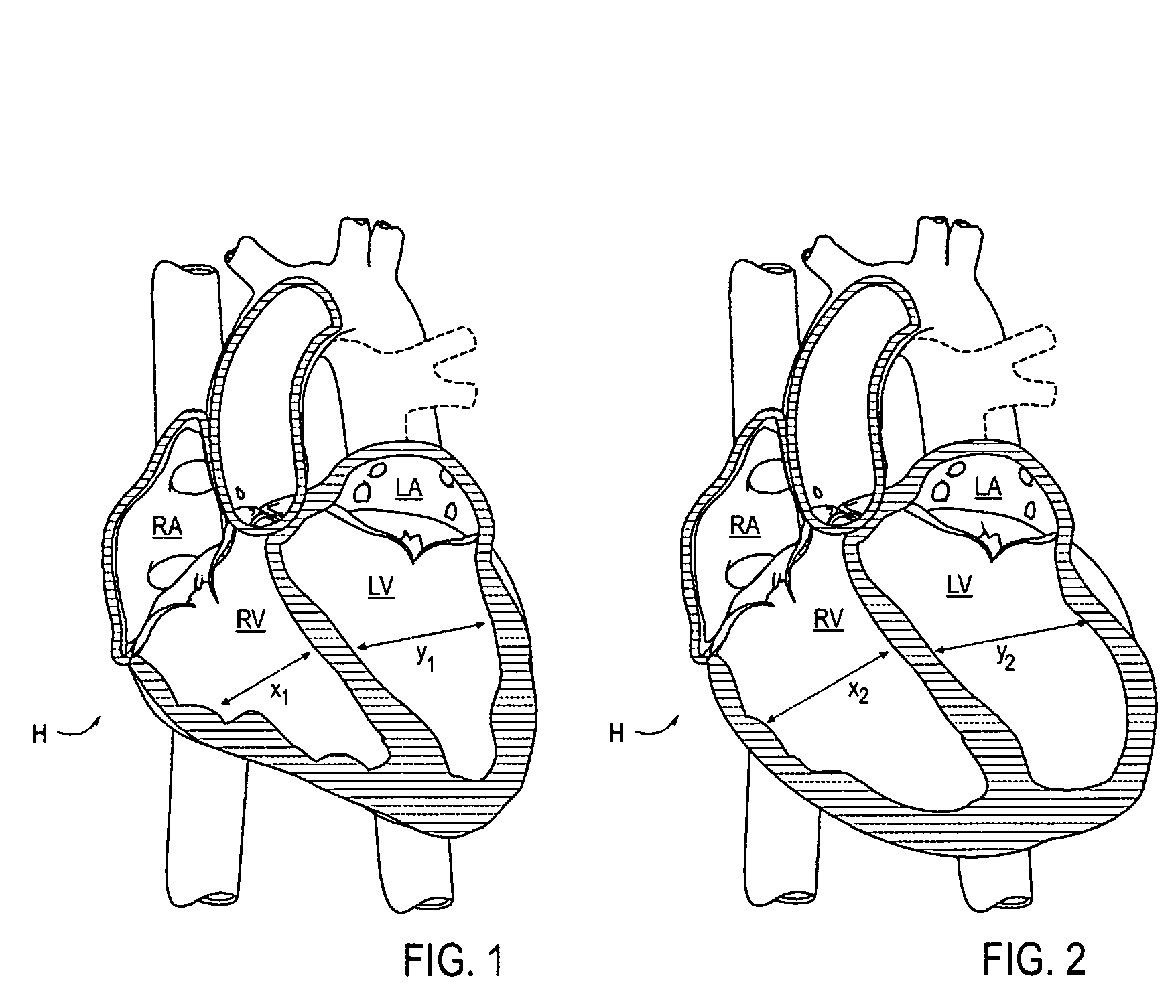
InactiveUS20060015003A1Improve shrinkageIncreased total stroke volumeElectrotherapyHeart valvesCardiac surfaceHeart Part
Systems, methods and devices are provided for treating heart failure patients suffering from various levels of heart dilation. Heart dilation treated by reshaping the heart anatomy with the use of magnetic forces. Such reshaping changes the geometry of portions of the heart, particularly the right or left ventricles, to increase contractibility of the ventricles thereby increasing the stroke volume which in turn increases the cardiac output of the heart. The magnetic forces are applied with the use of one or more magnetic elements which are implanted within the heart tissue or attached externally and / or internally to a surface of the heart. The various charges of the magnetic forces interact causing the associated heart tissue areas to readjust position, such as to decrease the width of the ventricles. Such repositioning is maintained over time by the force of the magnetic elements, allowing the damaging effects of heart dilation to slow in progression or reverse.
Owner:MICARDIA CORP
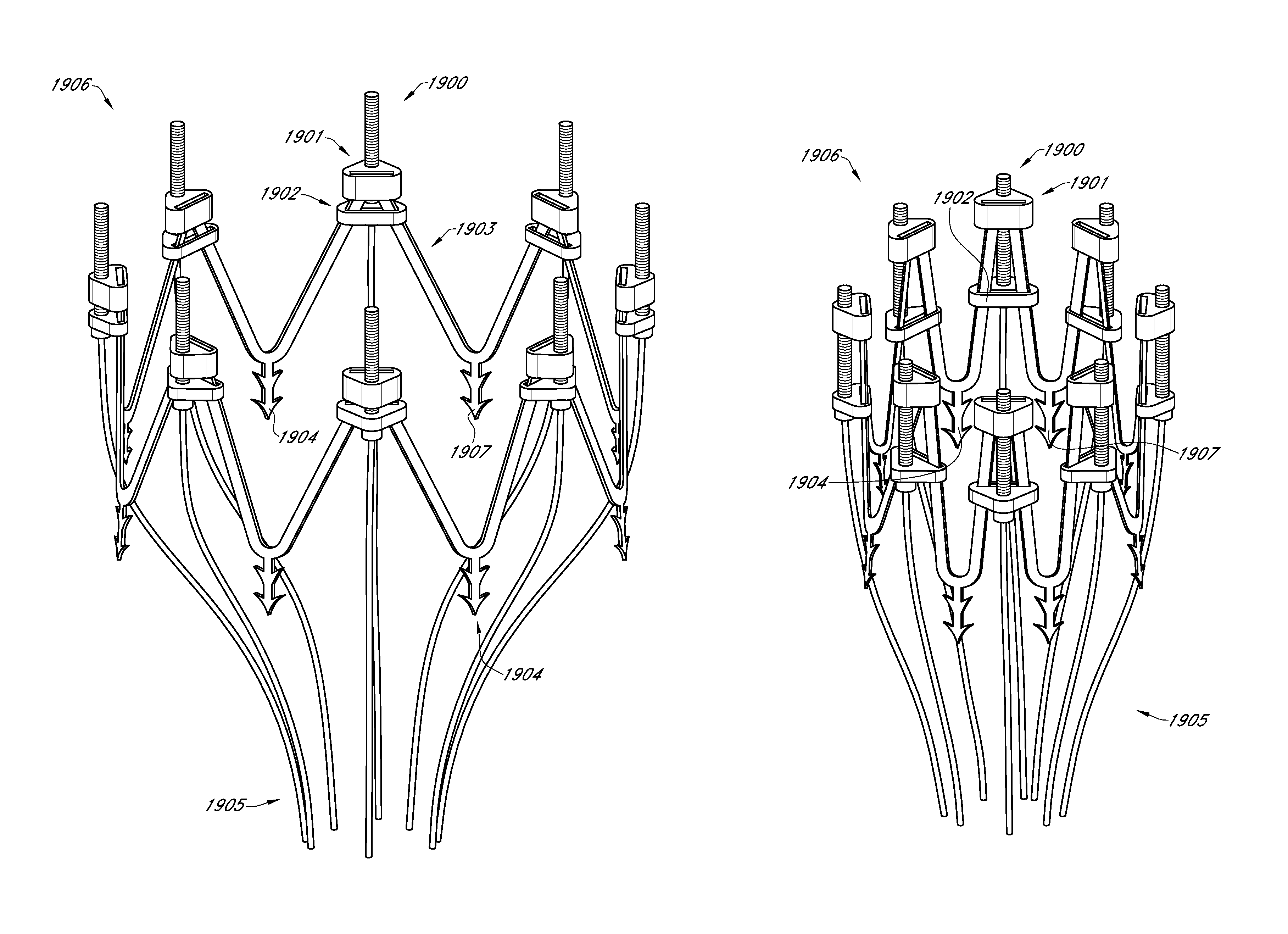
Adjustable endolumenal mitral valve ring
ActiveUS9180005B1Mitral regurgitation has been reduced and eliminatedStentsGuide needlesVentricular contractionMitral valve leaflet
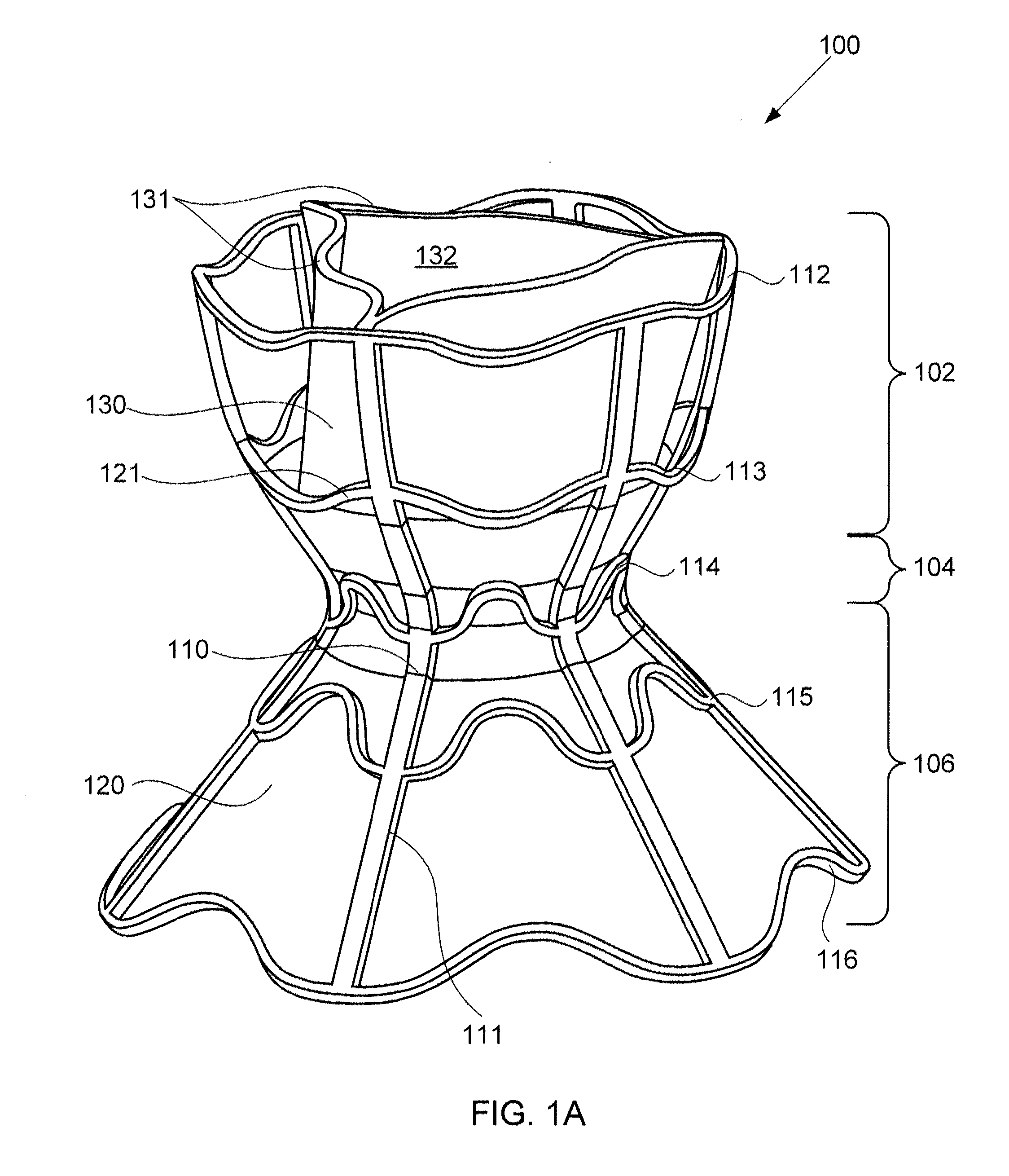
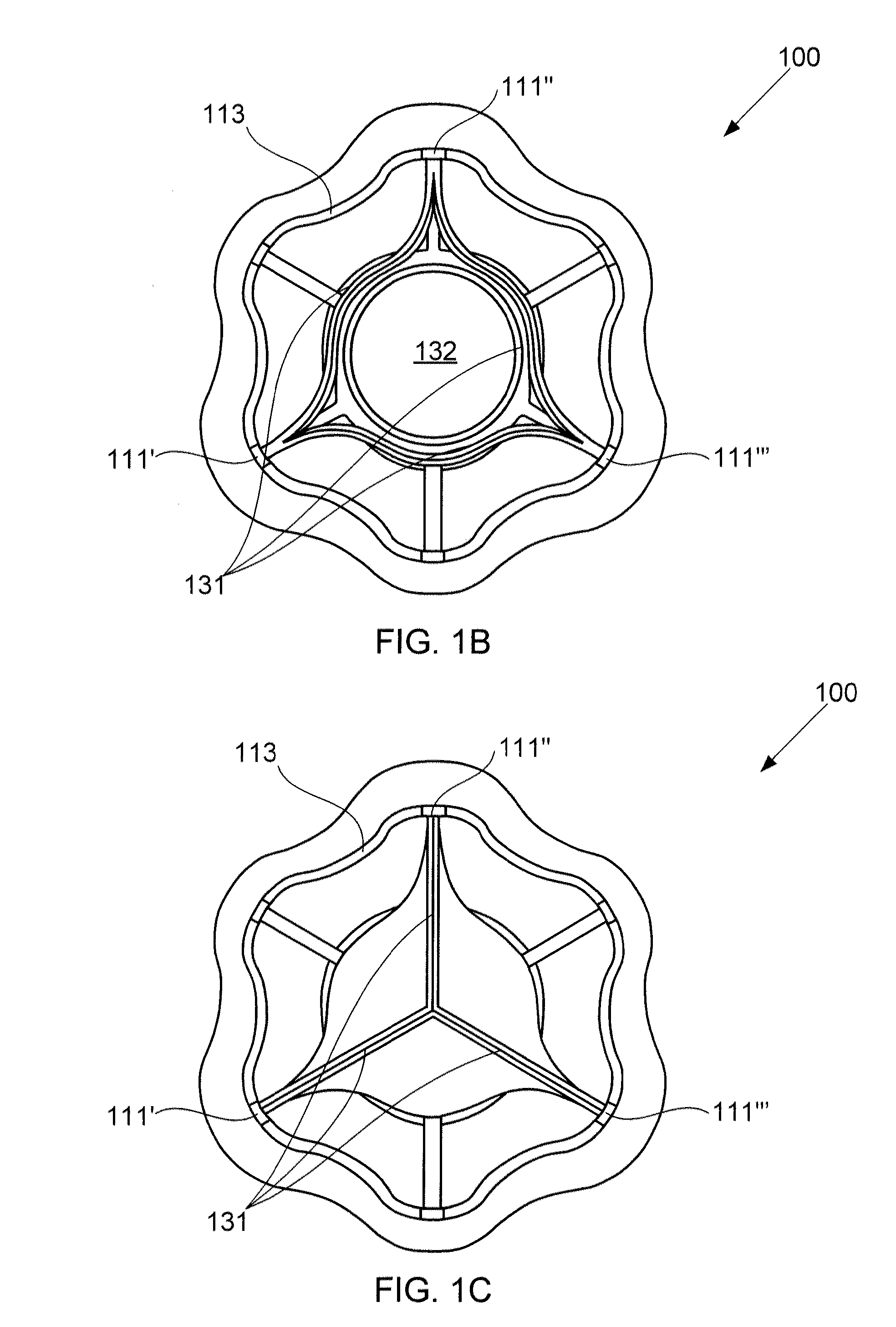
Excessive dilation of the annulus of a mitral valve may lead to regurgitation of blood during ventricular contraction. This regurgitation may lead to a reduction in cardiac output. Disclosed are systems and methods relating to an implant configured for reshaping a mitral valve. The implant comprises a plurality of struts with anchors for tissue engagement. The implant is compressible to a first, reduced diameter for transluminal navigation and delivery to the left atrium of a heart. The implant may then expand to a second, enlarged diameter to embed its anchors to the tissue surrounding and / or including the mitral valve. The implant may then contract to a third, intermediate diameter, pulling the tissue radially inwardly, thereby reducing the mitral valve and lessening any of the associated symptoms including mitral regurgitation.
Owner:BOSTON SCI SCIMED INC
Systems for heart treatment
InactiveUS7144363B2Reduce stressReduce/limit volumeSuture equipmentsHeart valvesLeft ventricular sizeTherapeutic treatment
Owner:BAY INNOVATION GROUP
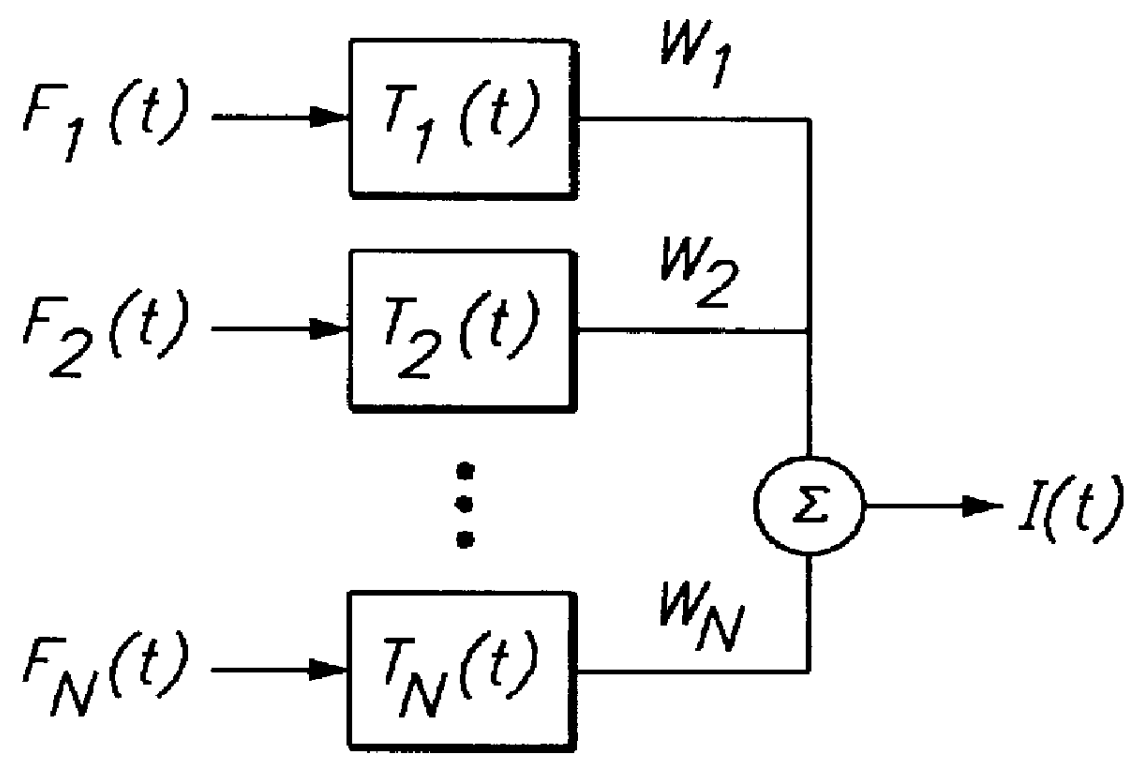
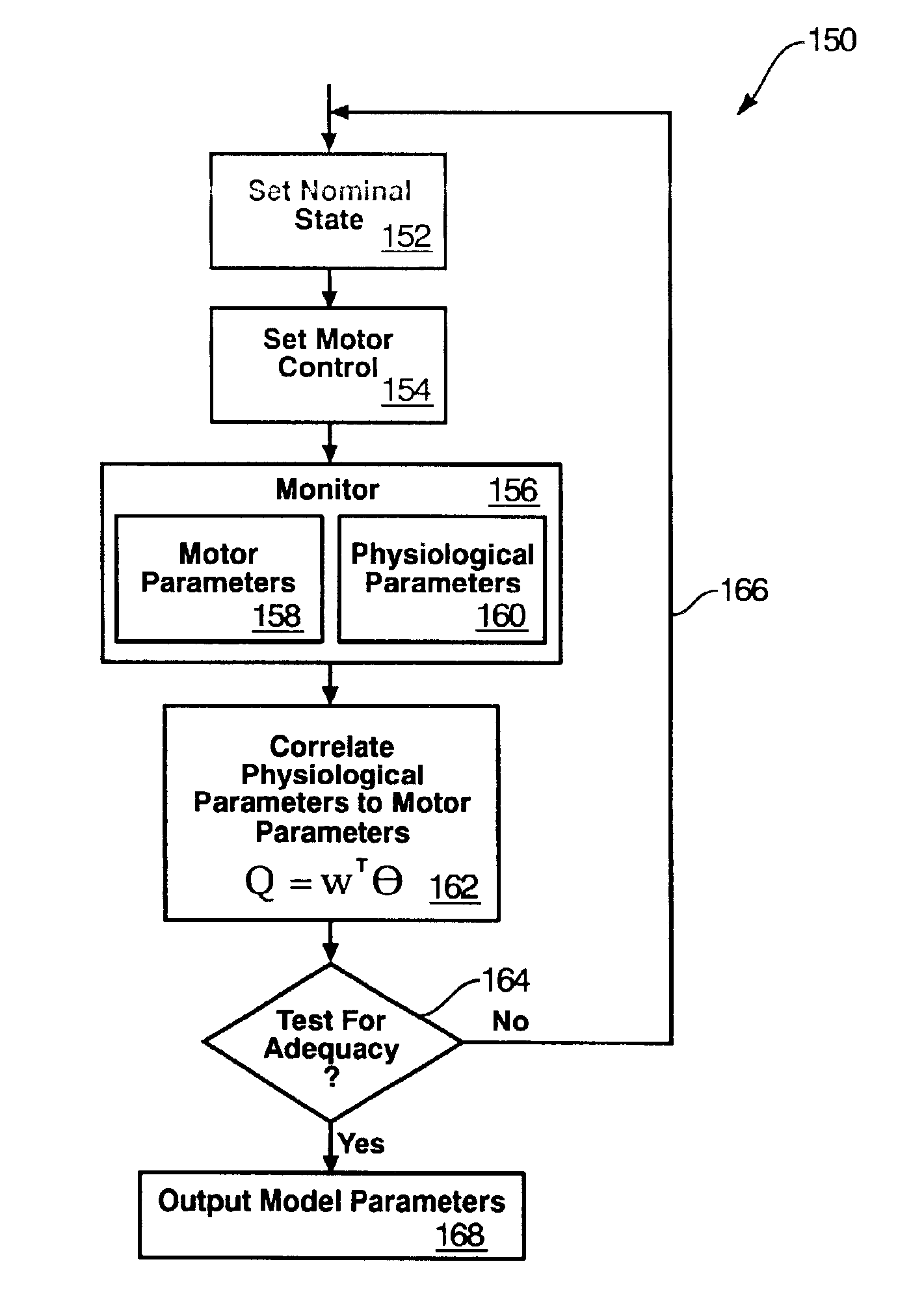
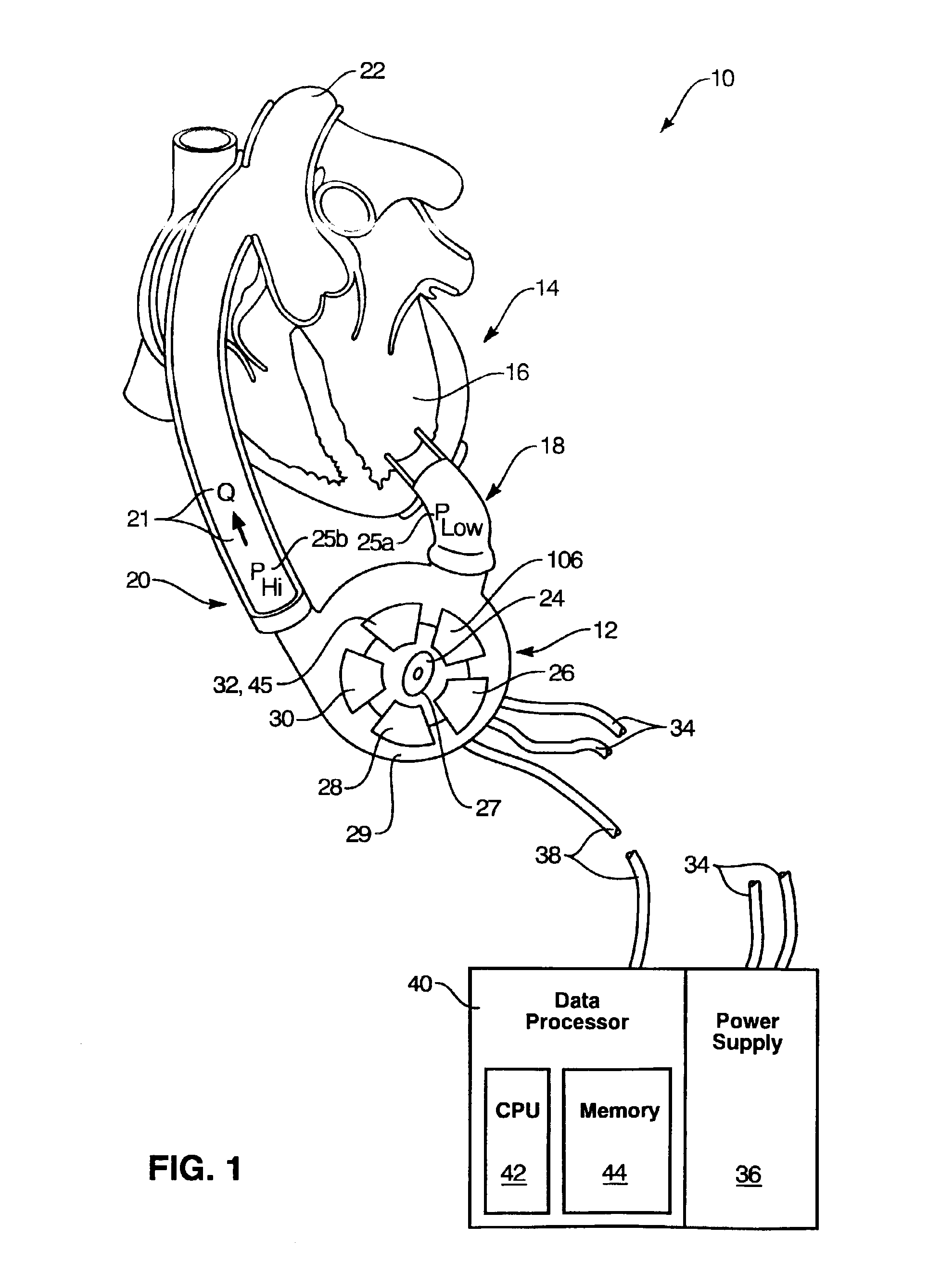
Rotary blood pump diagnostics and cardiac output controller
A method and apparatus for controlling a ventricular assist device are disclosed. The method includes the step of providing a ventricular assist device which can be defined in terms of operational parameters such as pump speed or current. Measuring at least one physiological parameter reflecting a physiological state corresponding to a patient. Correlating at least one physiological parameter measured from the patient to at least one operational parameter using an estimation method. Selecting a physiological state definable by desired values of the physiological parameters. Monitoring at least one operational parameter. Controlling input values of the operational parameter based on output from the monitoring step. The apparatus includes a pump driven by a motive drive and having an impeller. A sensor detects the value of an operational parameter of the pump. A processor provides a statistical correlation between patients physiological parameter and the operational parameter of the pump and adjusts the operational parameter to affect a predetermined optimal physiological state.
Owner:WORLD HEART
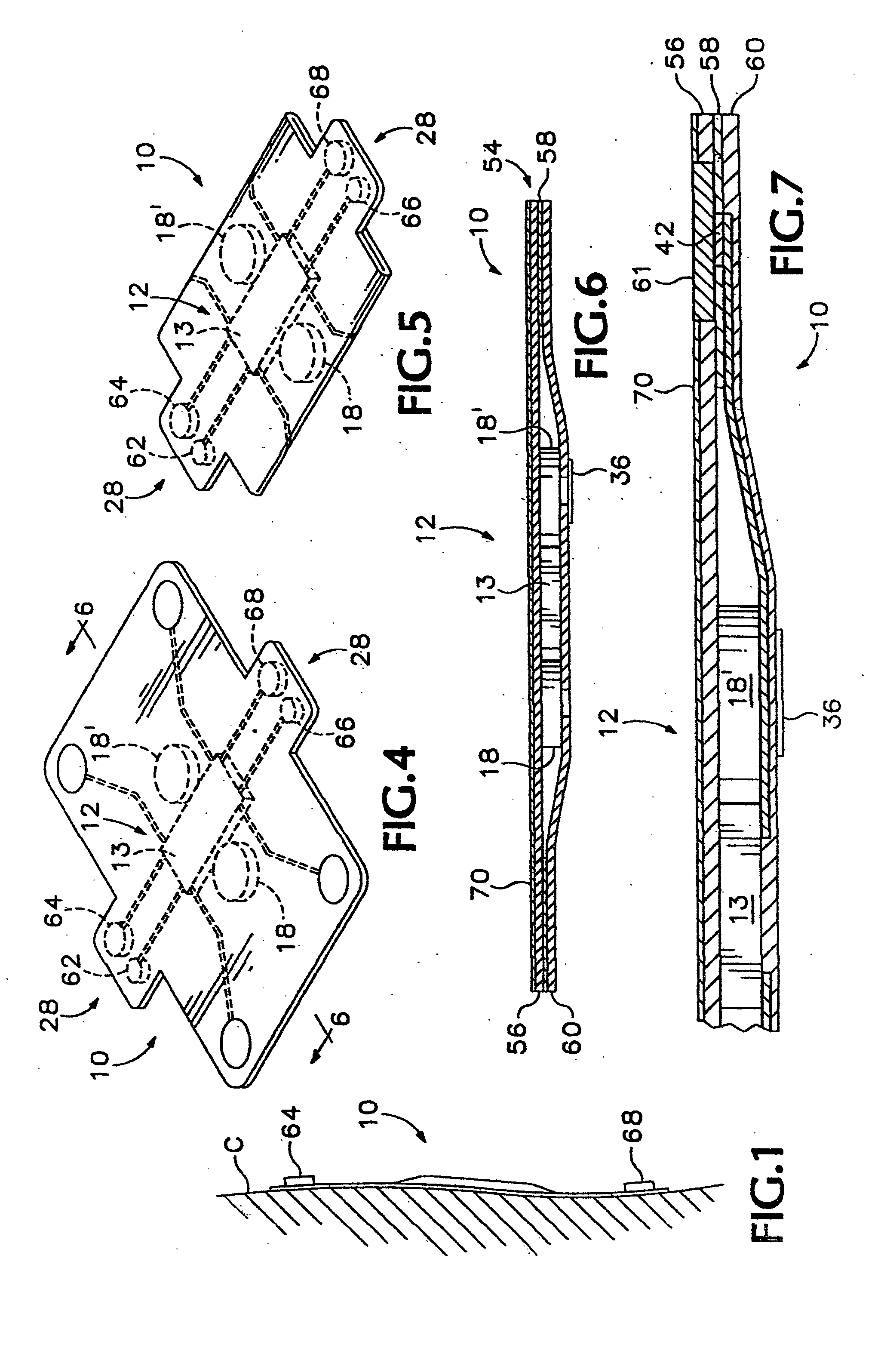
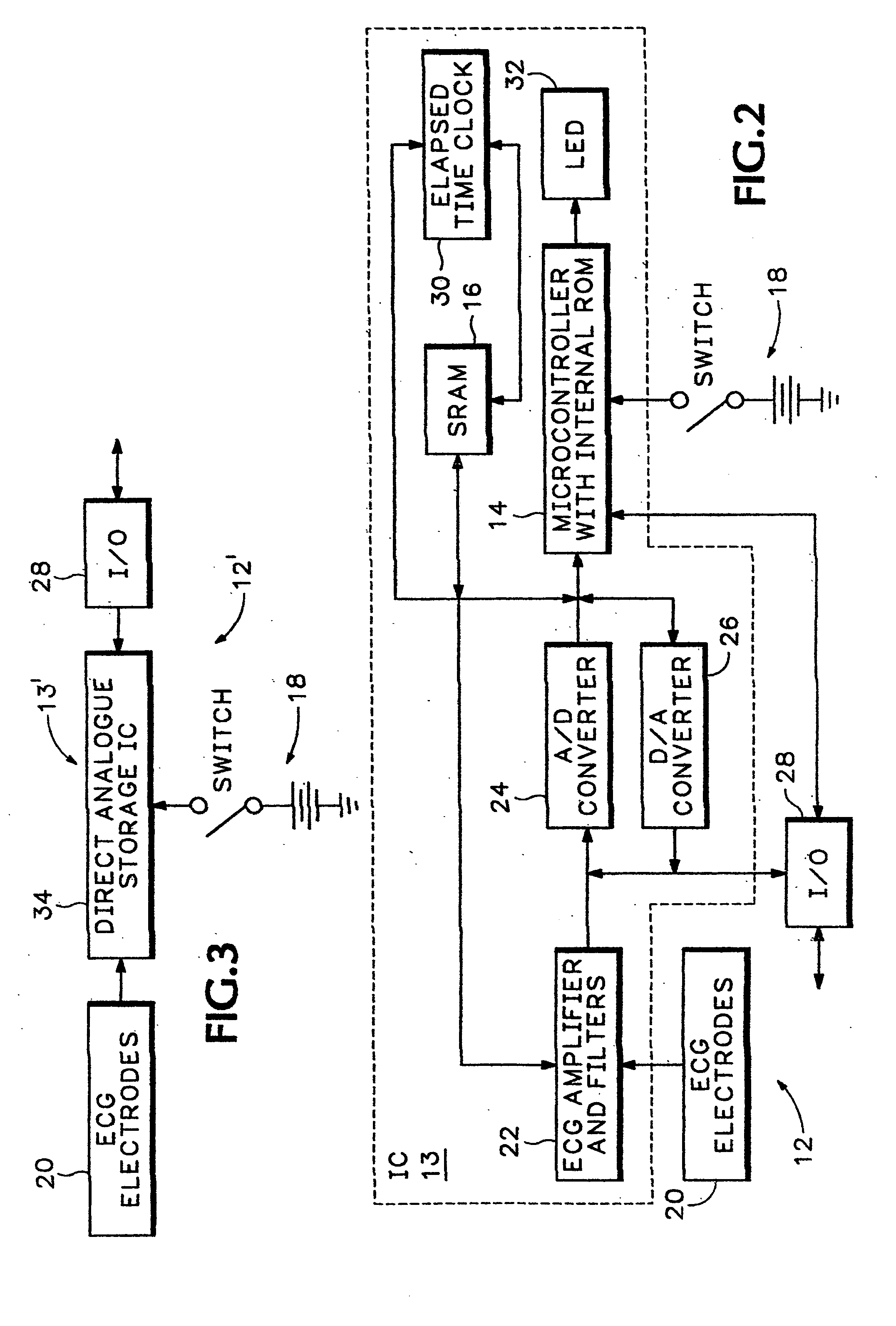
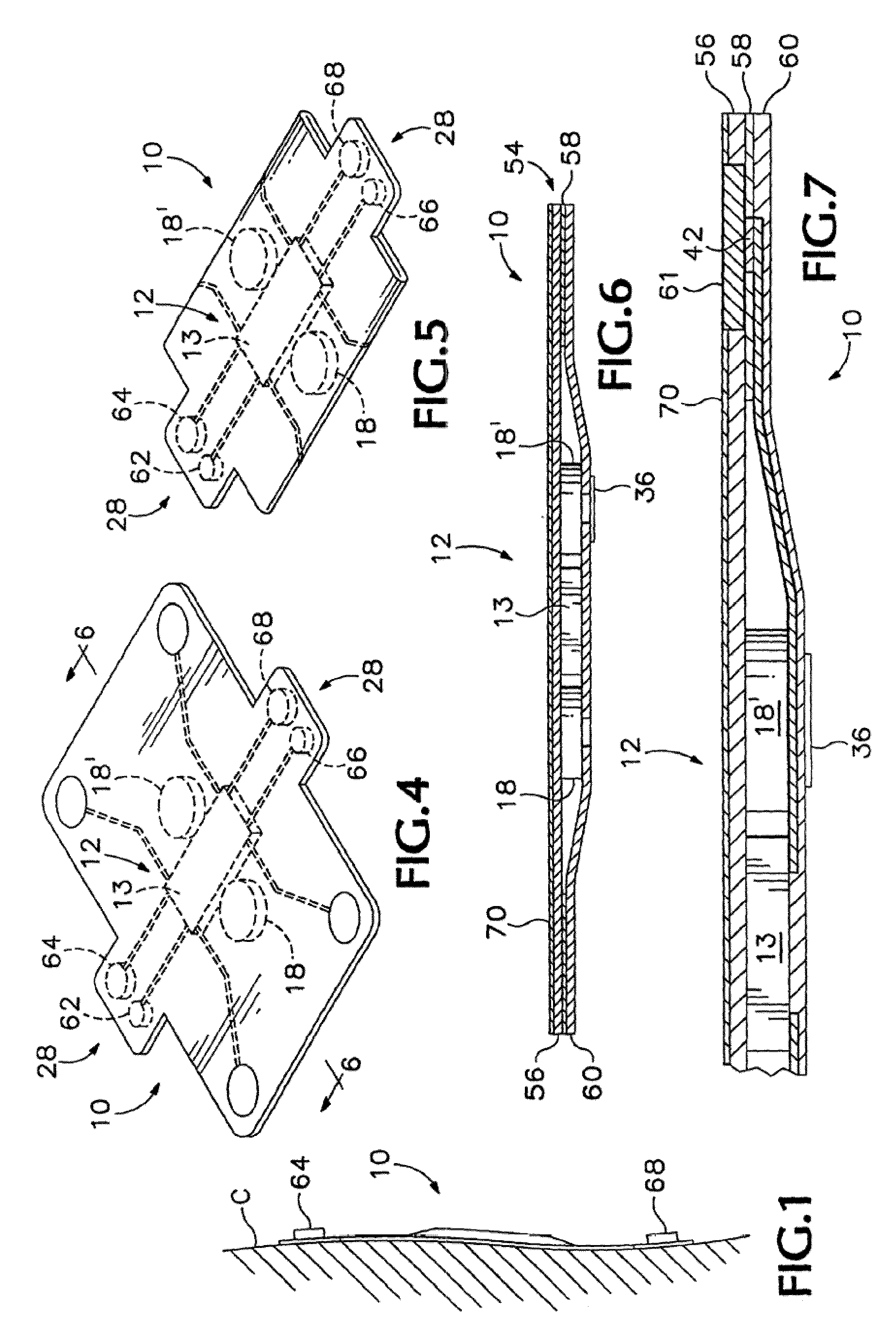
Non-invasive body composition monitor, system and method
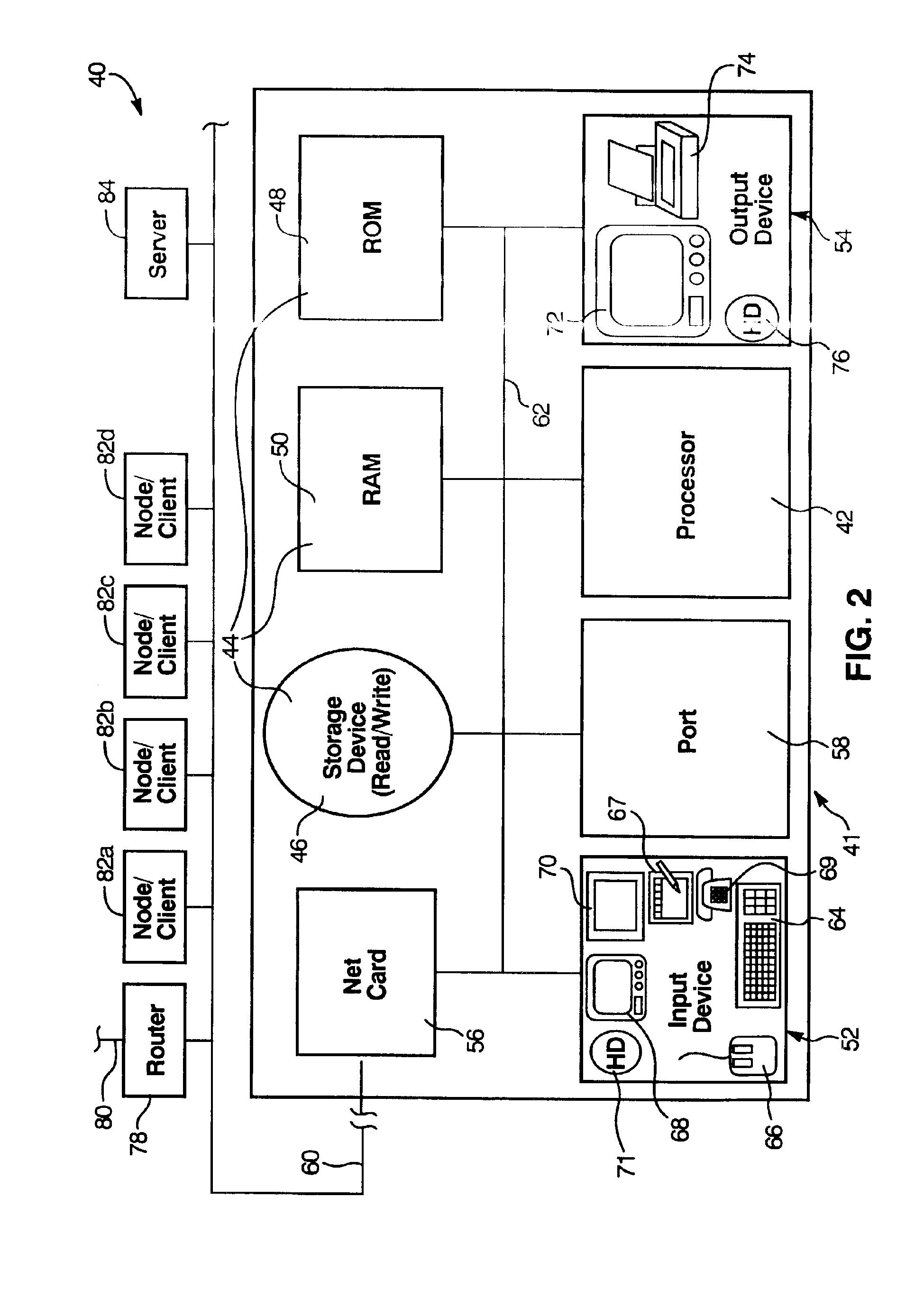
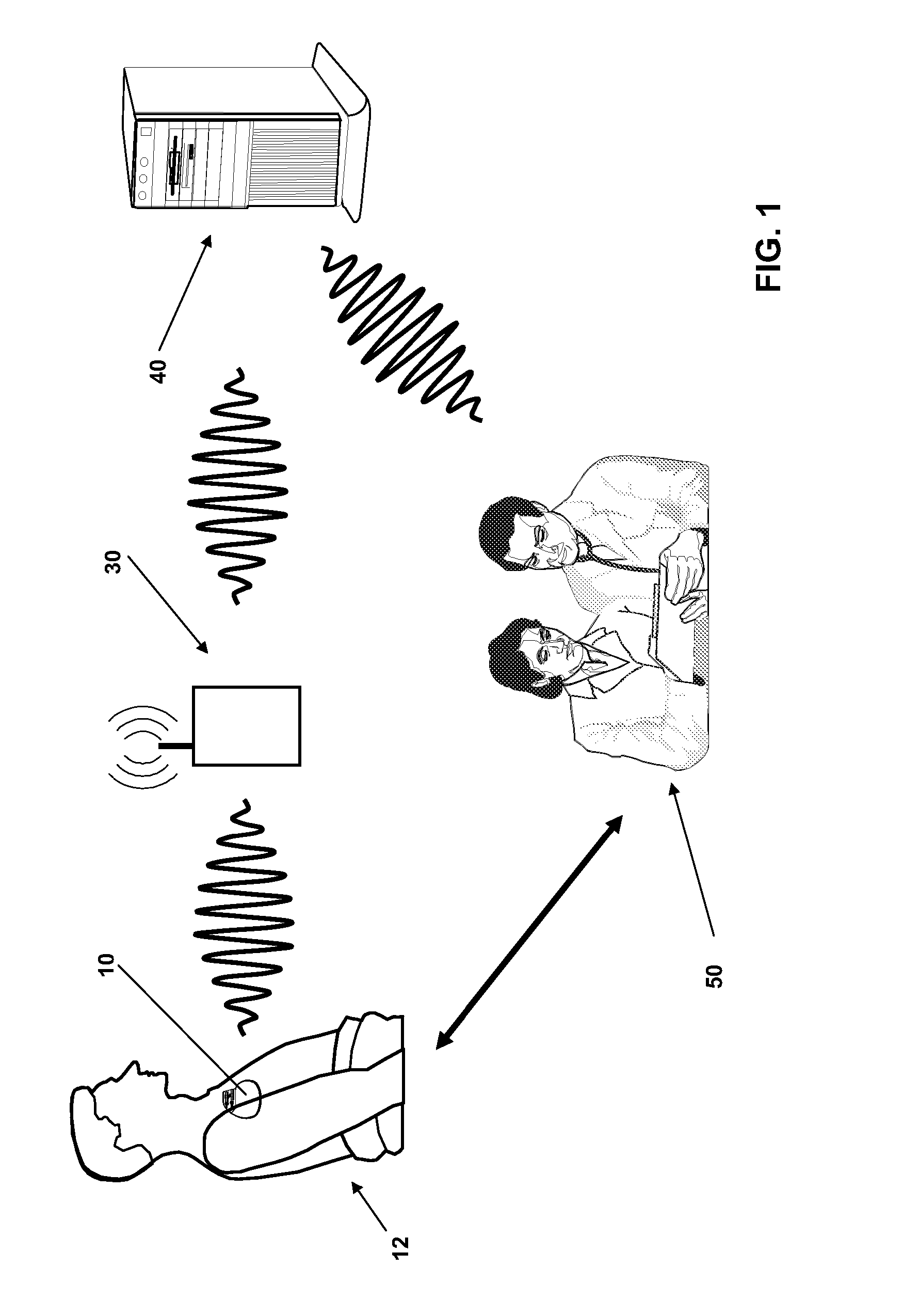
The invented non-invasive vital signs monitor is in a flexible, nominally flat planar form having integral gel electrodes, a sticky-back rear surface, an internal flex circuit capable of sensing, recording and playing out several minutes of the most recently acquired ECG waveform data and a front surface that includes an outplay port. The invented non-invasive body composition ‘risk’ monitor includes a measurement device for monitoring one or more variables including body fluid mass, dehydration, respiratory rate, blood pressure, bio-impedance, cardiography such as cardiac output, and body conformation parameters. The risk monitor may be provided in a lightweight carrying case into which the vital signs monitor plugs. Thus the two monitors may be independent or they may be integrated into one portable, non-invasive device that can convey important patient data to / from a remote patient medical data center via wireless telemetry for oversight, treatment and possible intervention by a physician.
Owner:RIGHT CORP
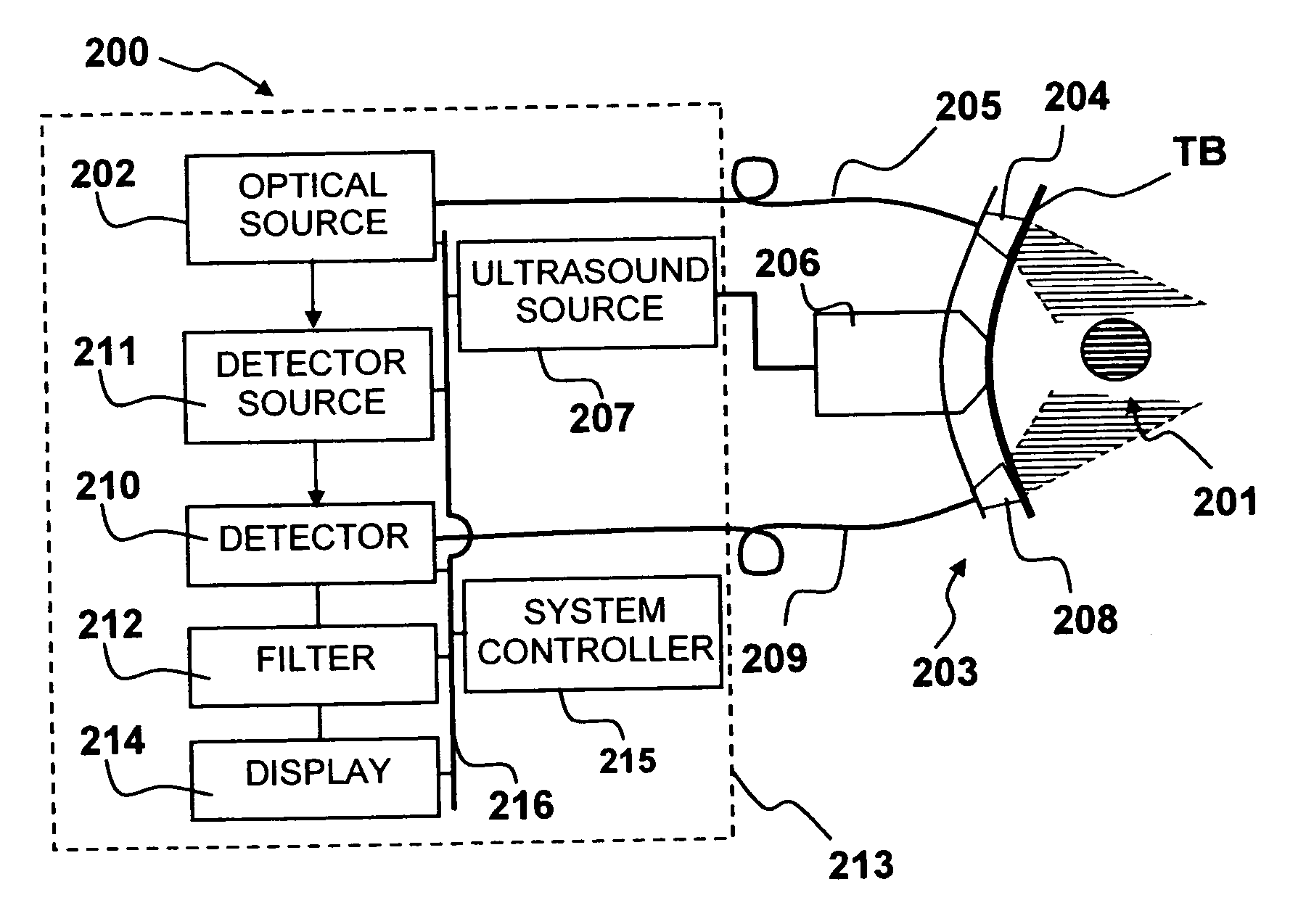
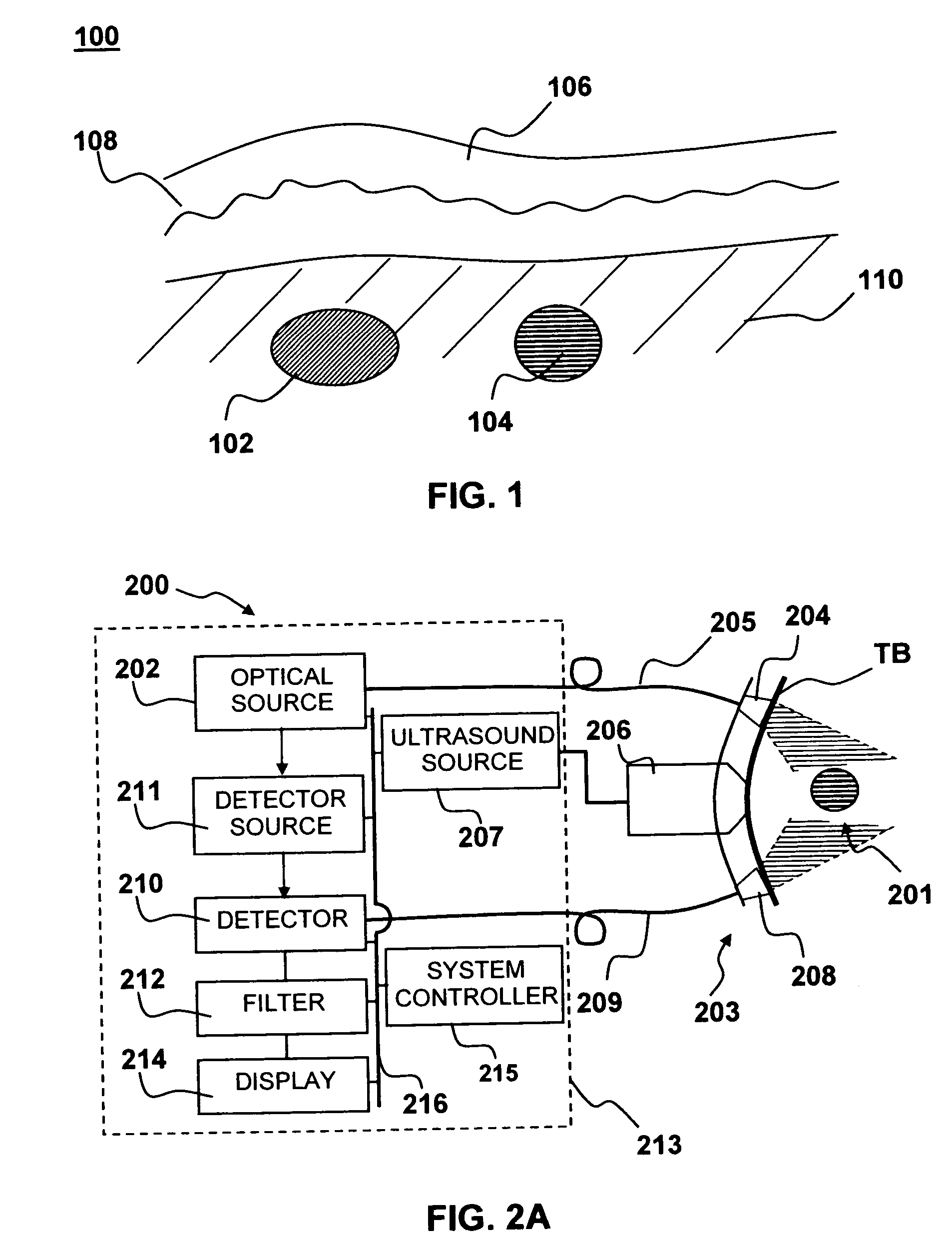
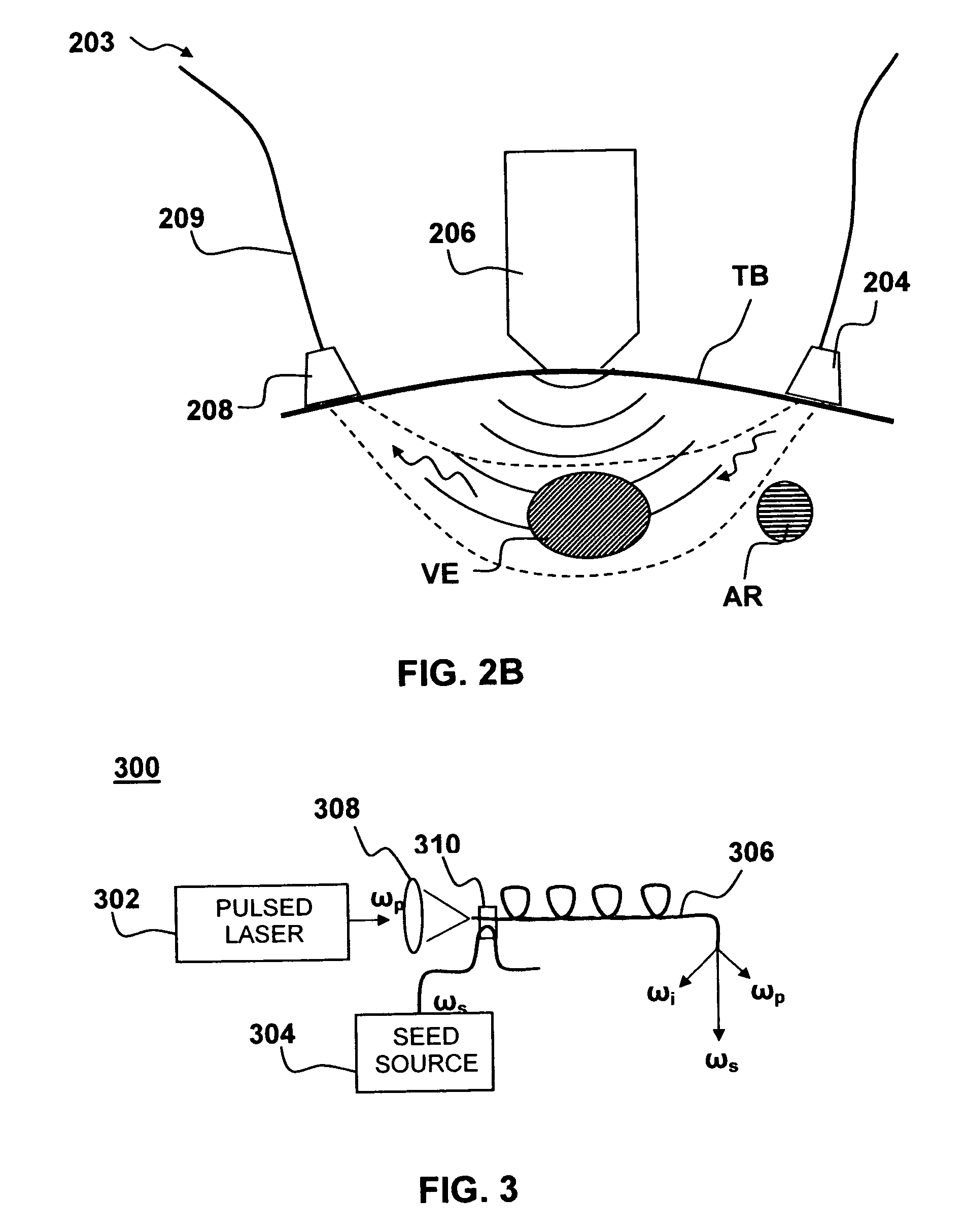
Apparatus and method for non-invasive and minimally-invasive sensing of venous oxygen saturation and pH levels
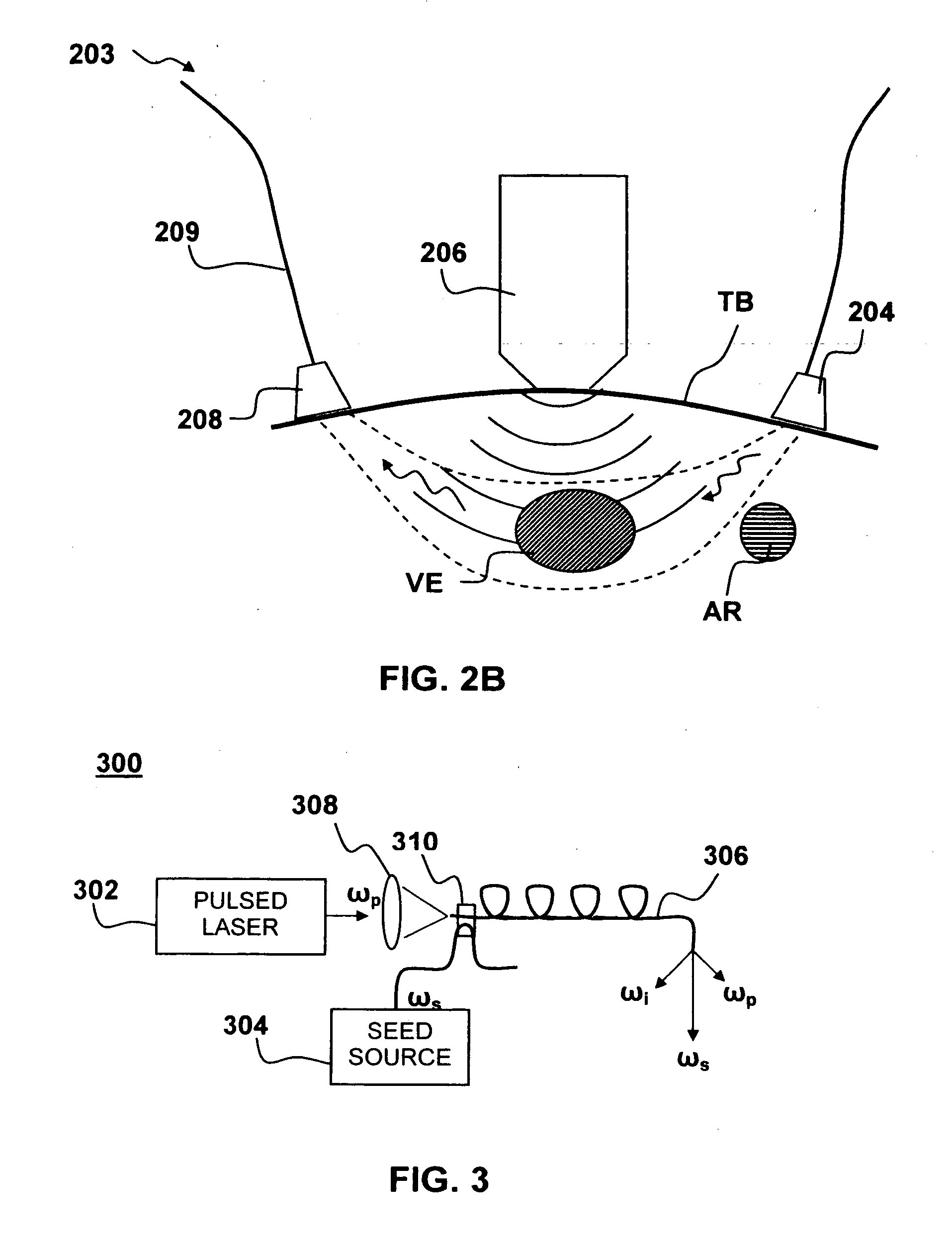
InactiveUS20060224053A1Easy to useCost effectiveOrgan movement/changes detectionSensorsSonificationScattering cross-section
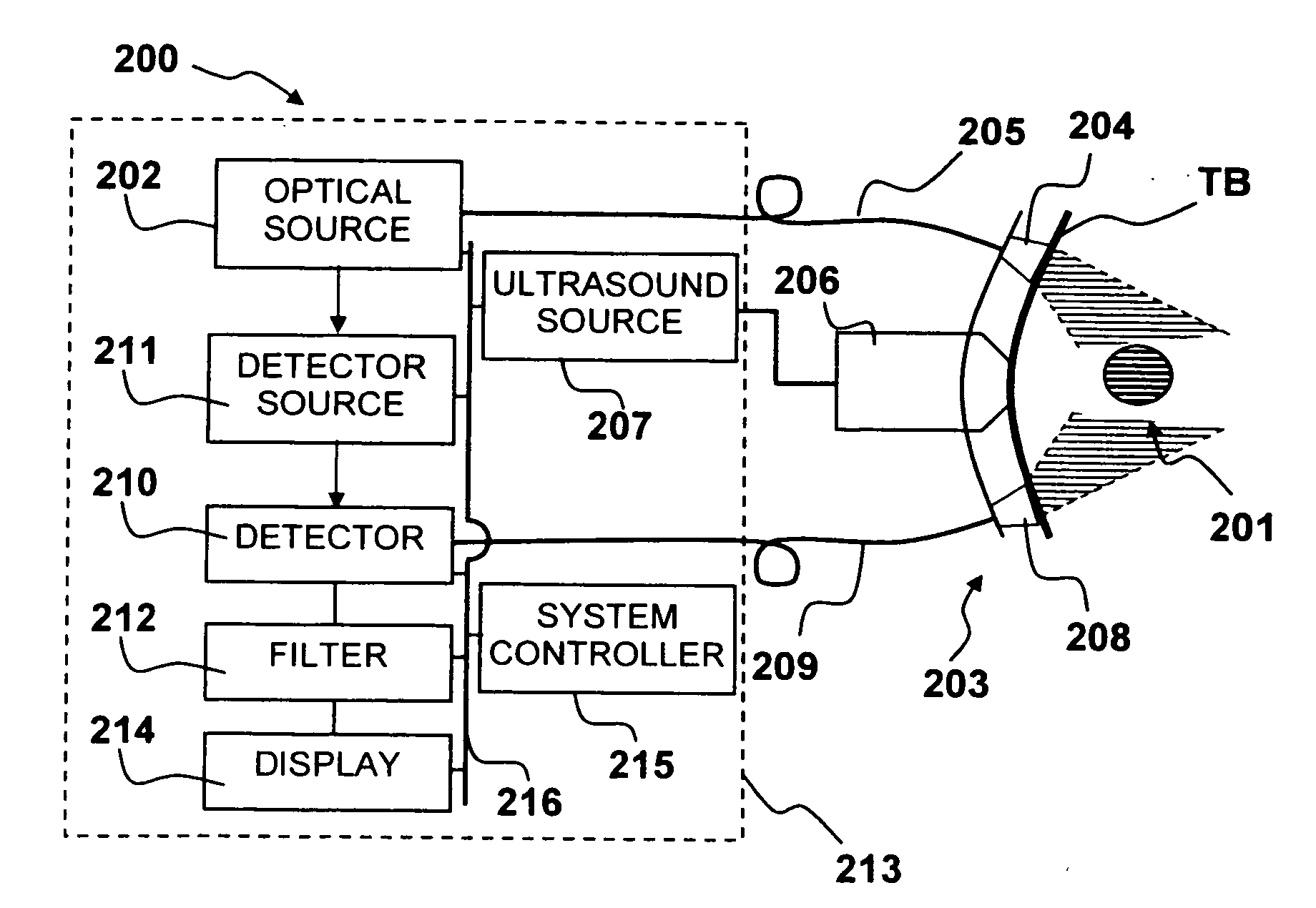
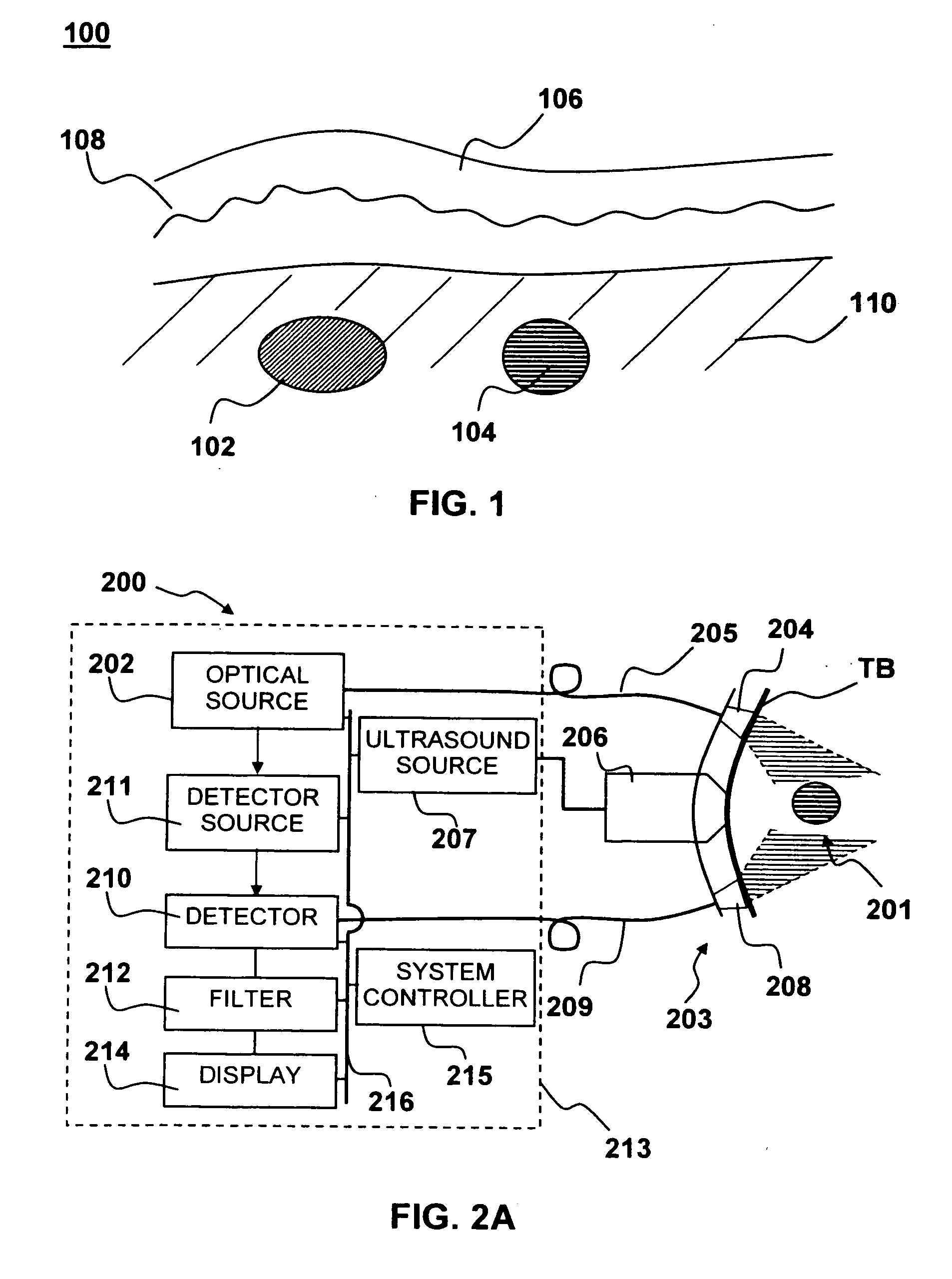
Medical diagnostic apparatus and methods are disclosed. Ultrasound radiation pressure selectively modulates a target area within a body. One or more pulses of radiation containing temporally correlated groups of photons are generated. The photons are characterized by two or more different wavelengths that are selected to have specific interaction with a target chromophore. The two or more different wavelengths are also selected to have substantially similar scattering cross-sections and anisotropy parameters in the target and its surroundings. The pulses of radiation are injected into the body proximate the target area being modulated by the radiation pressure field. Photon groups at each of the different wavelengths that are backscattered from the target area are detected in temporal coincidence. Time-gated background-free amplification of the return signal is used to exclude photons which could not by virtue of their arrival time have interacted with the radiation-pressure-modulated target. Photon groups are selected with a modulation component at the modulation frequency of the radiation pressure modulation field, or at a harmonic of the modulation frequency. From the arrival rate of the detected temporally correlated photon pairs or multiplets, chemical information about the target area, such as an oxygenation or pH level can be inferred. Cardiac output may be computed from measurements of venous and / or arterial oxygenation using this technique.
Owner:SKYLINE BIOMEDICAL
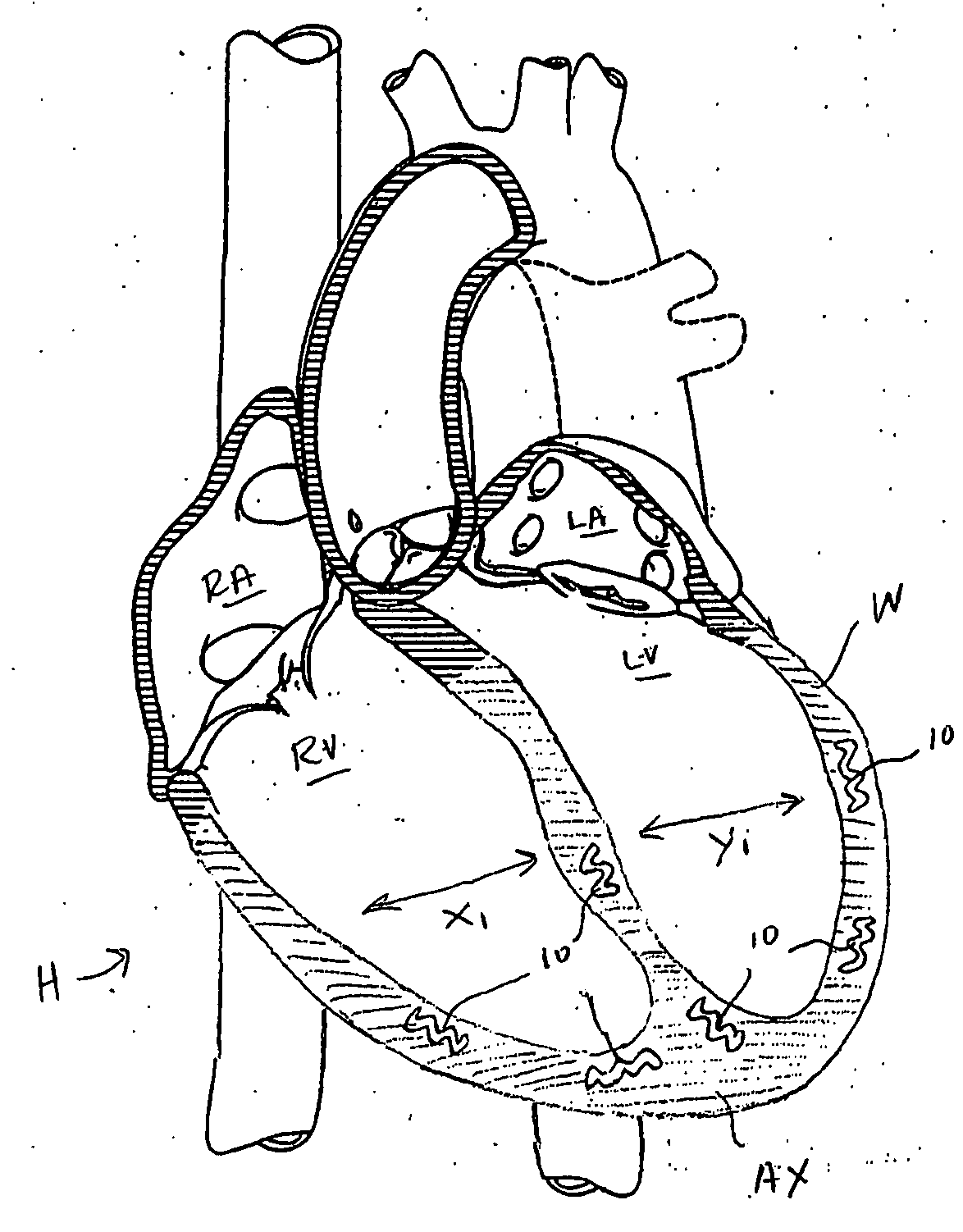
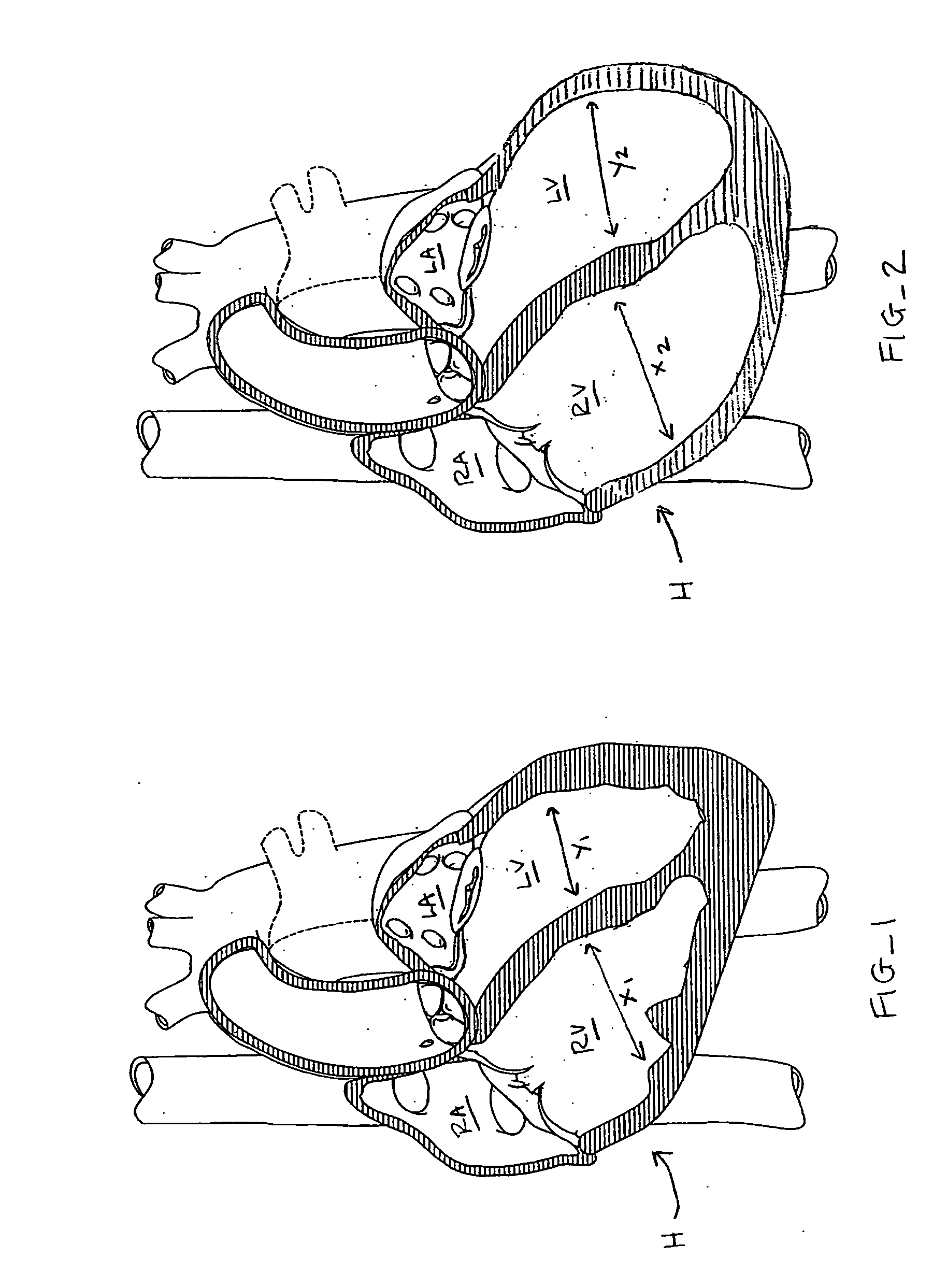
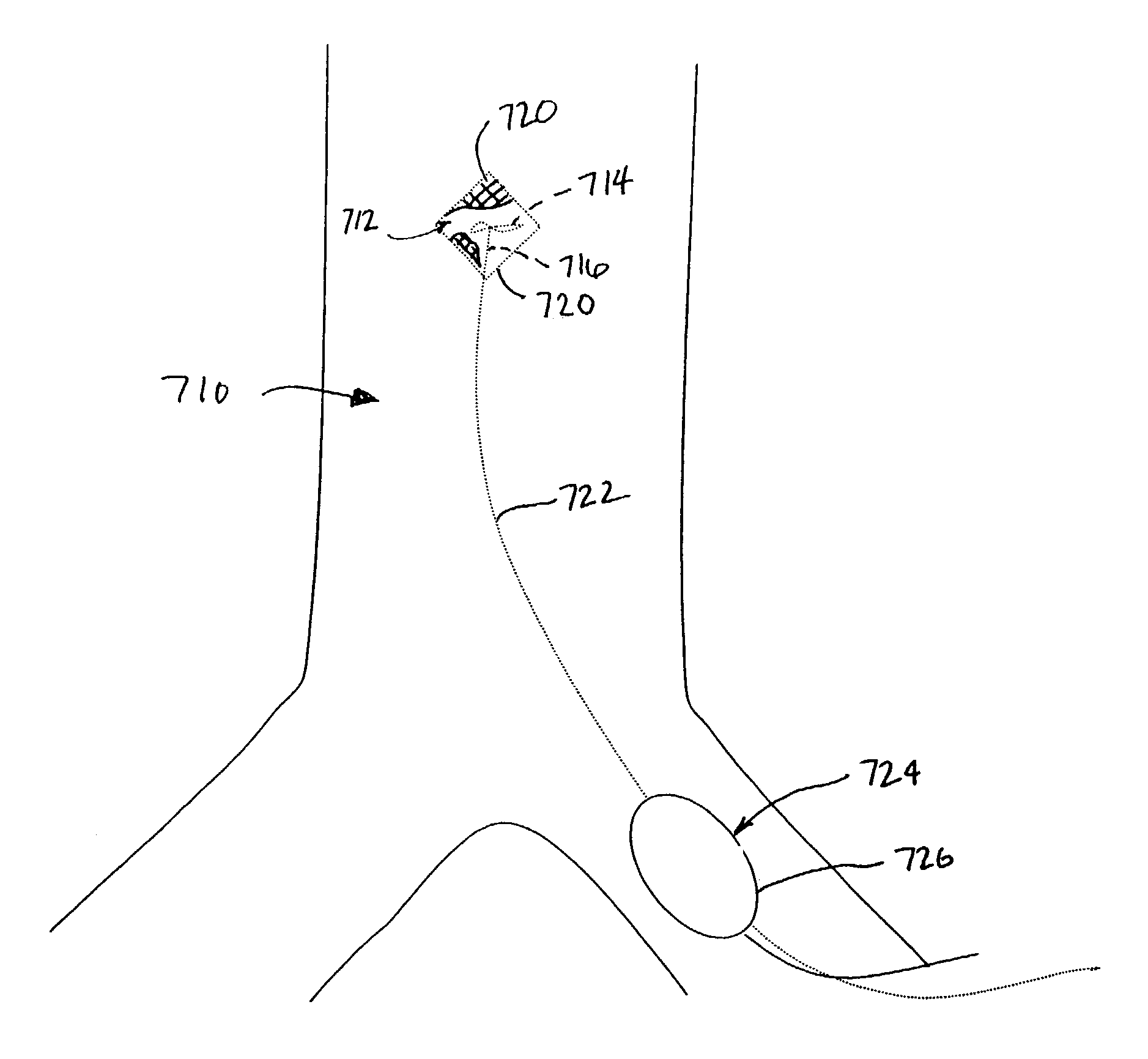
Systems for heart treatment
InactiveUS20050197692A1Decreasing wall stressReinforce wallSuture equipmentsElectrotherapyLeft ventricular sizeTherapeutic treatment
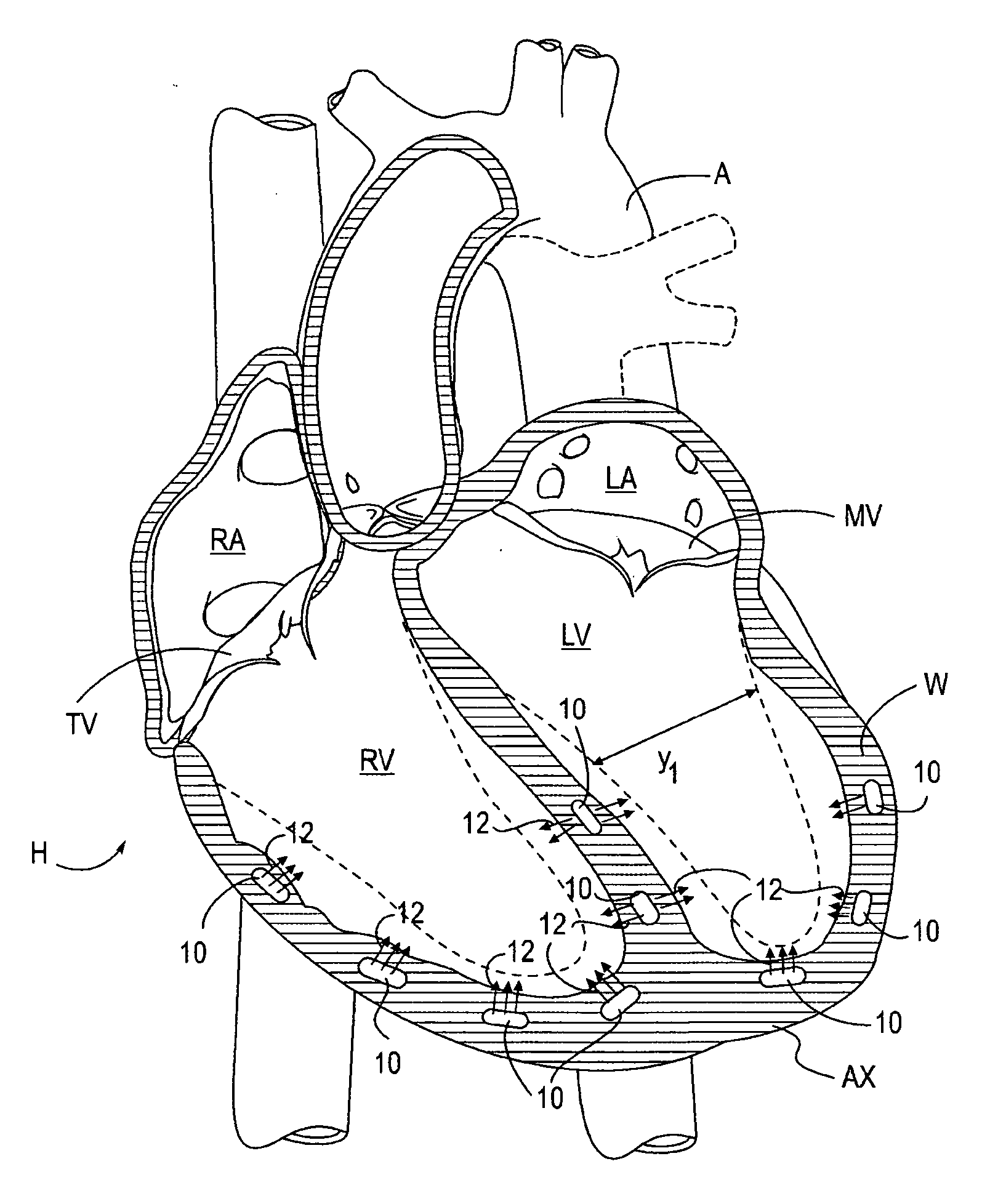
Described are devices and methods for treating degenerative, congestive heart disease and related valvular dysfunction. Percutaneous and minimally invasive surgical tensioning structures offer devices that mitigate changes in the ventricular structure (i.e., remodeling) and deterioration of global left ventricular performance related to tissue damage precipitating from ischemia, acute myocardial infarction (AMI) or other abnormalities. These tensioning structures can be implanted within various major coronary blood-carrying conduit structures (arteries, veins and branching vessels), into or through myocardium, or into engagement with other anatomic structures that impact cardiac output to provide tensile support to the heart muscle wall which resists diastolic filling pressure while simultaneously providing a compressive force to the muscle wall to limit, compensate or provide therapeutic treatment for congestive heart failure and / or to reverse the remodeling that produces an enlarged heart.
Owner:EXTENSIA MEDICAL
Body composition, circulation, and vital signs monitor and method
The invented non-invasive vital signs monitor is in a flexible, nominally flat planar form having integral gel electrodes, a sticky-back rear surface, an internal flex circuit capable of sensing, recording and playing out several minutes of the most recently acquired ECG waveform data and a front surface that includes an outplay port. The invented non-invasive body composition ‘risk’ monitor includes a measurement device for monitoring one or more variables including body fluid mass, dehydration, respiratory rate, blood pressure, bio-impedance, cardiography such as cardiac output, and body conformation parameters. The risk monitor may be provided in a lightweight carrying case into which the vital signs monitor plugs. Finally, a lightweight portable probe or transducer containing a transmissive or reflective electro-optical emitter and receptor in the infrared spectrum is fitted on a subject's finger or toe. Associated electronics energize and monitor the probe, detect cardio-rhythmic fluctuations therefrom, and process digital data over a prescribed window to produce a non-invasive, qualitative or quantitative measure of the subject's circulation. In accordance with one embodiment of the invention, a simple tri-color LED array is used to indicate the subject's circulation as being normal, reduced, or borderline. Thus the vital signs, bio-impedance, and circulation monitors may be independent or they may be integrated into one portable, non-invasive device that can concurrently monitor and locally display or remotely convey important patient data including circulation data to a local subject or physician or to / from a remote patient medical data center via wireless telemetry for oversight, treatment and possible intervention by a remote physician.
Owner:SEMLER SCI
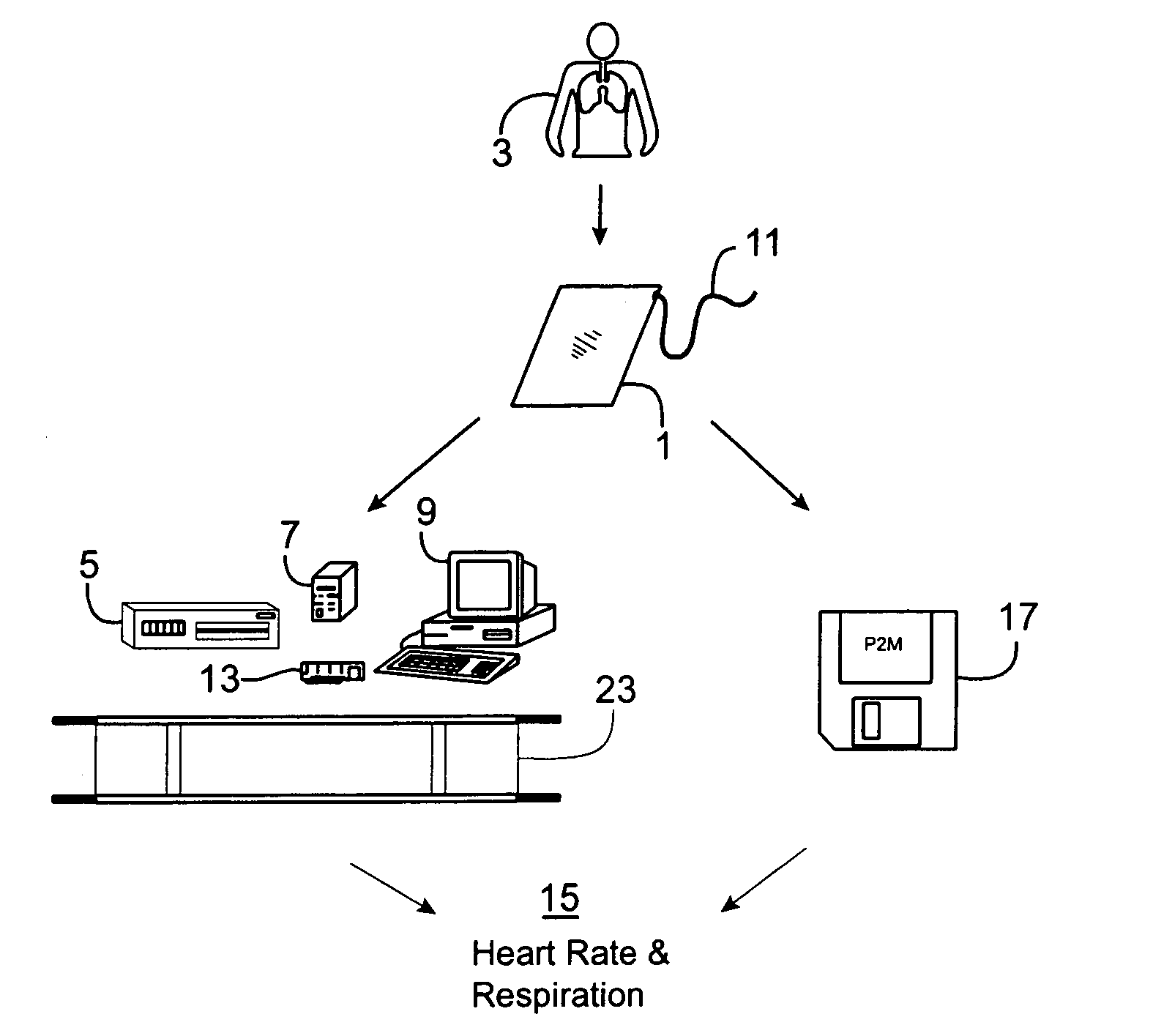
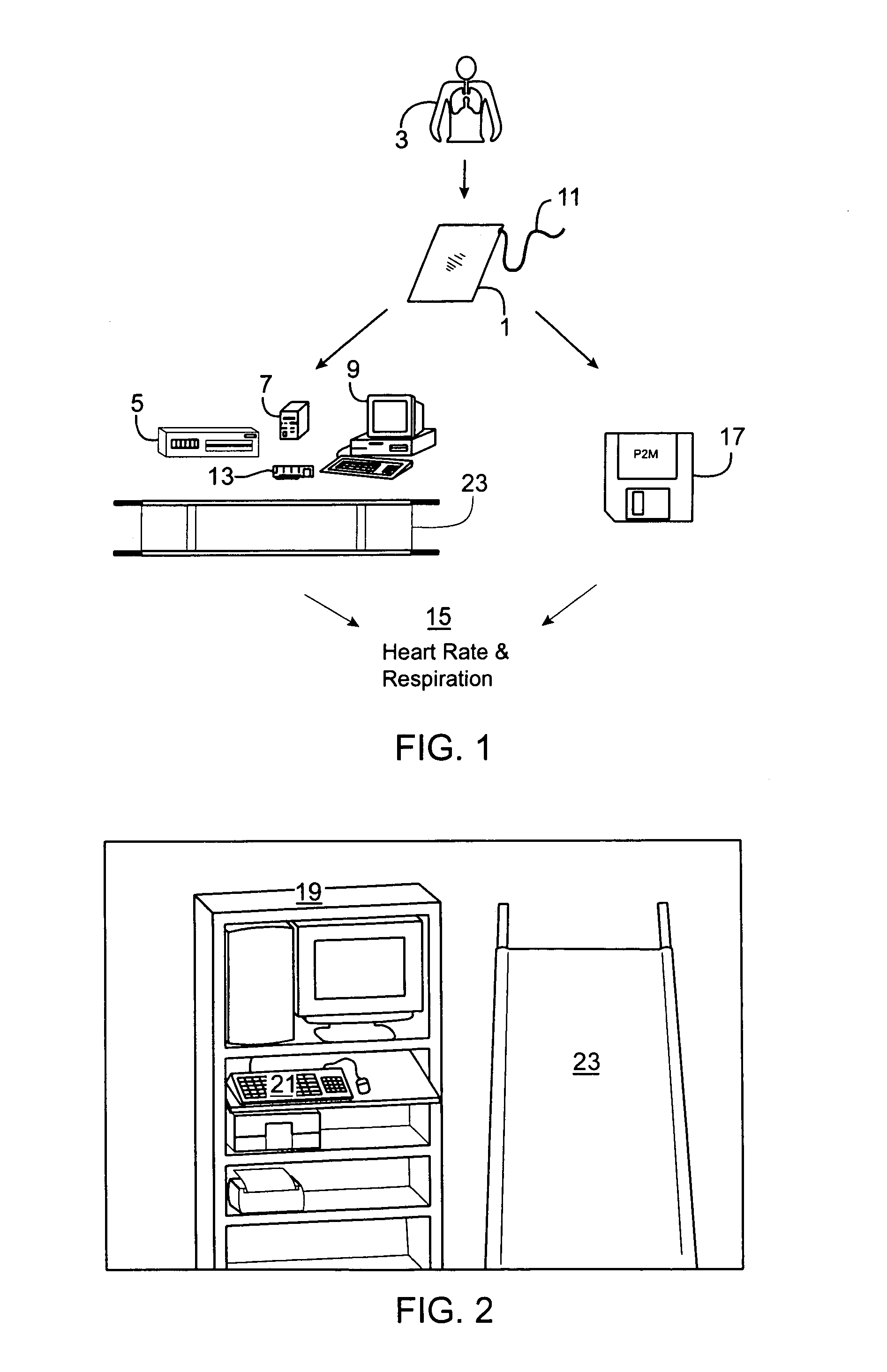
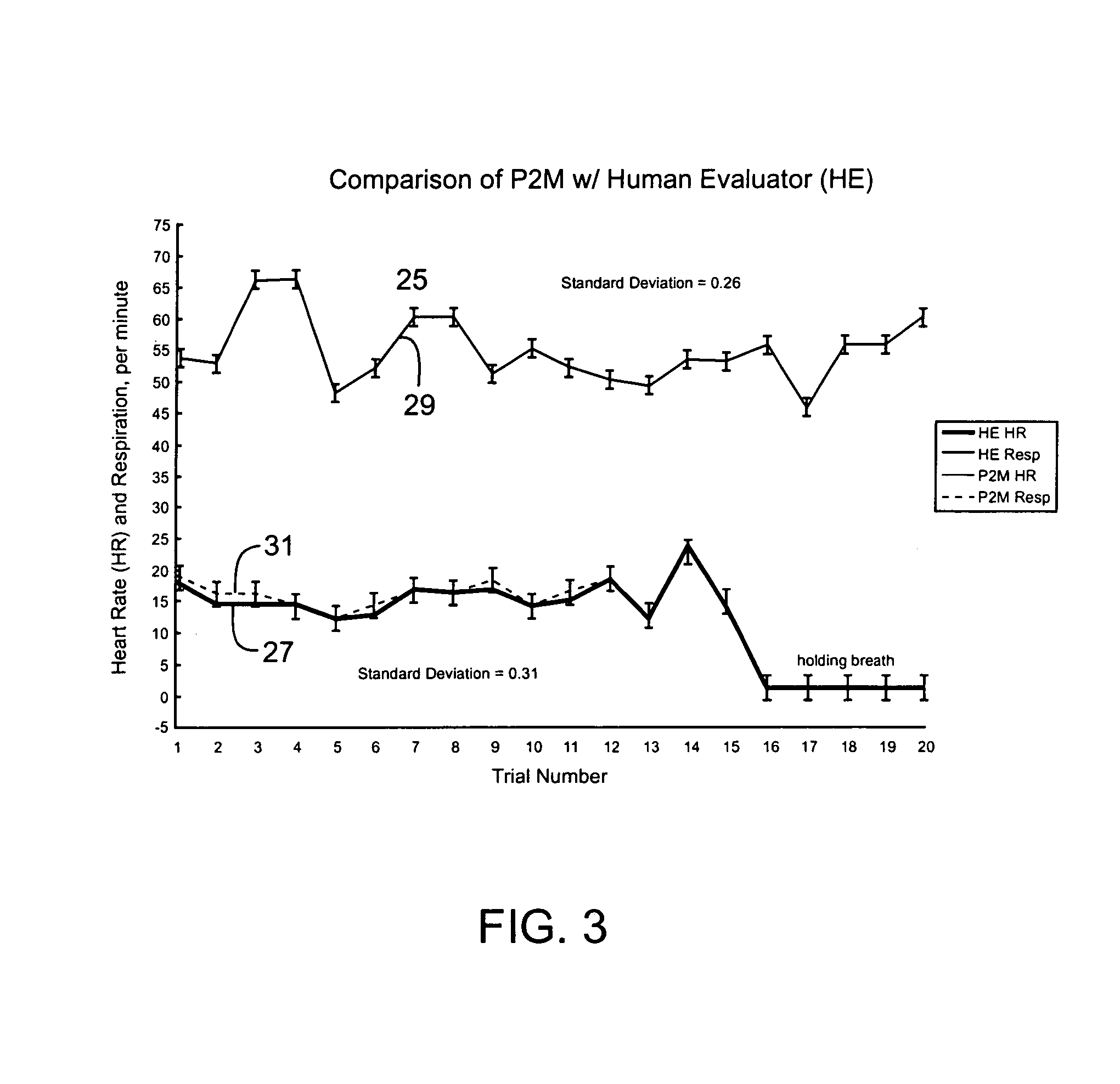
Passive physiological monitoring (P2M) system
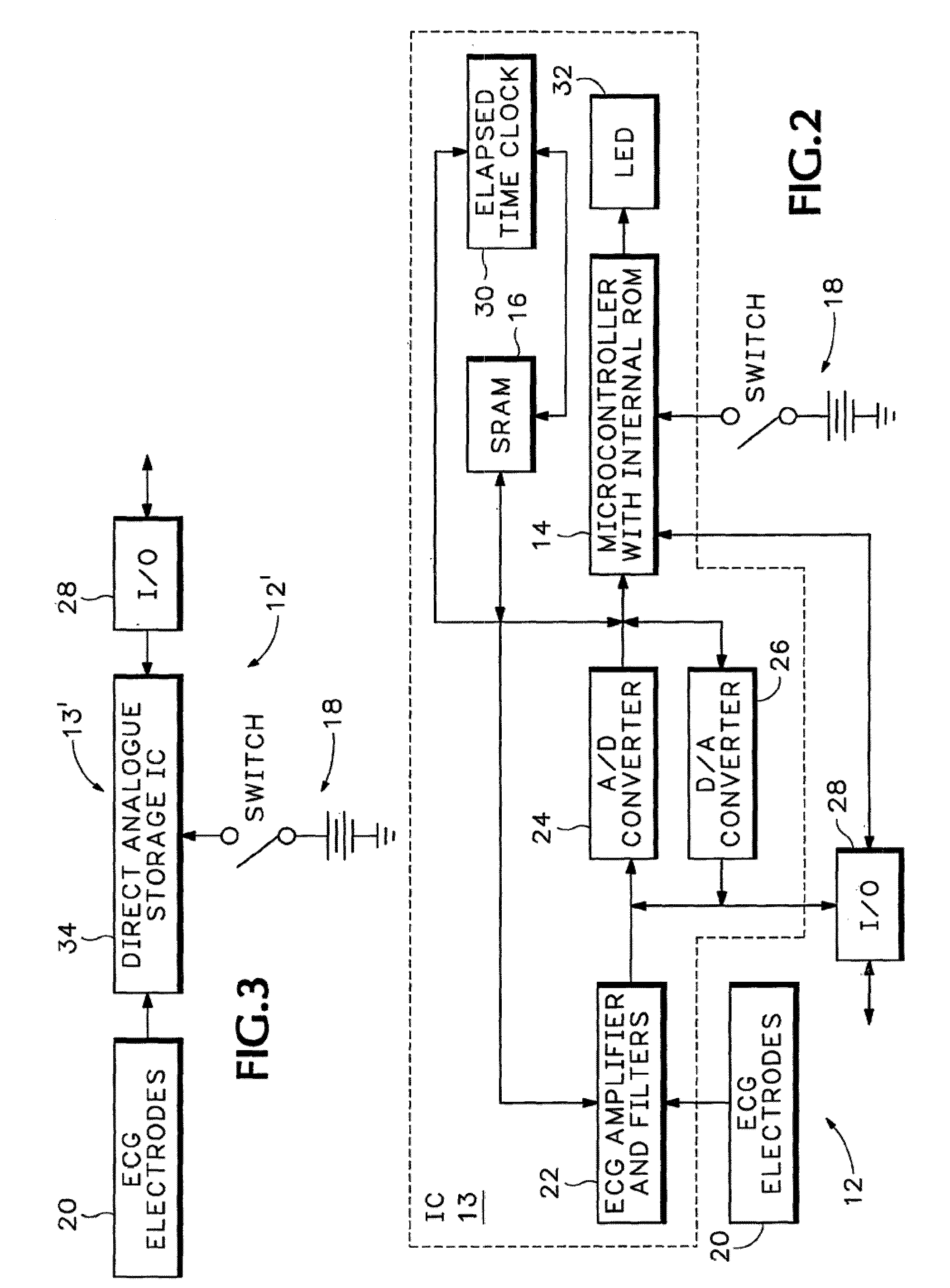
InactiveUS6984207B1Easy to deployEvaluation of blood vesselsCatheterInternal bleedingBand-pass filter
Passive Physiological monitoring apparatus and method have a sensor for sensing physiological phenomenon. A converter converts sensed data into electrical signals and a computer receives and computes the signals, and outputs computed data for real-time interactive display. The sensor is a piezoelectric film of polyvinylidene fluoride. A band-pass filter filters out noise and isolates the signals to reflect data from the body. A pre-amplifier amplifies signals. Signals detected include mechanical, thermal and acoustic signatures reflecting cardiac output, cardiac function, internal bleeding, respiratory, pulse, apnea, and temperature. A pad may incorporate the PVDF film and may be fluid-filled. The film converts mechanical energy into analog voltage signals. Analog signals are fed through the band-pass filter and the amplifier. A converter converts the analog signals to digital signals. A Fourier transform routine is used to transform into the frequency domain. A microcomputer is used for recording, analyzing and displaying data for on-line assessment and for providing realtime response. A radio-frequency filter may be connected to a cable and the film for transferring signals from the film through the cable. The sensor may be an array provided in a MEDEVAC litter or other device for measuring acoustic and hydraulic signals from the body of a patient for field monitoring, hospital monitoring, transport monitoring, home, remote monitoring.
Owner:HOANA MEDICAL
Device to permit offpump beating heart coronary bypass surgery
Owner:MAQUET CARDIOVASCULAR LLC
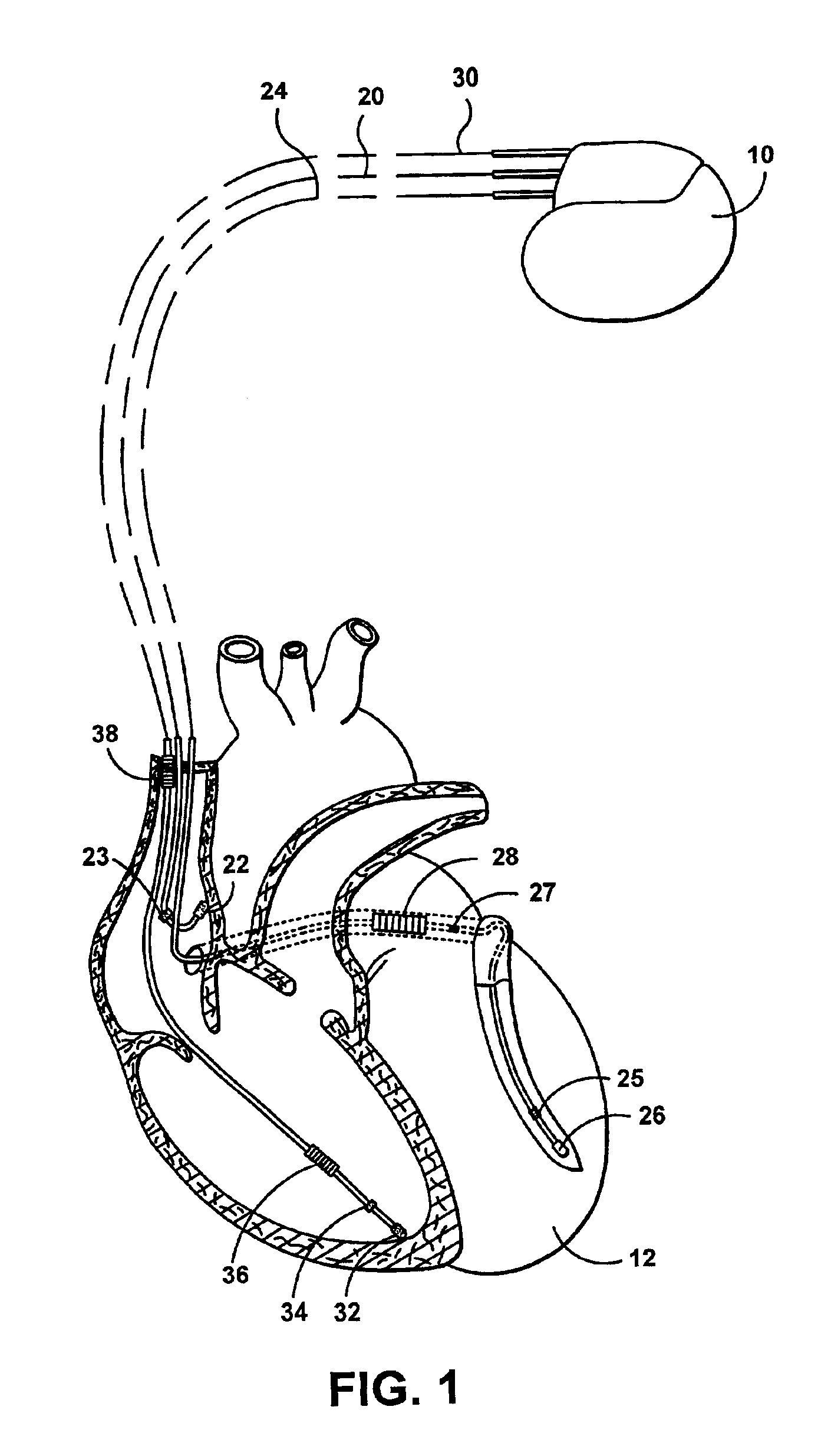
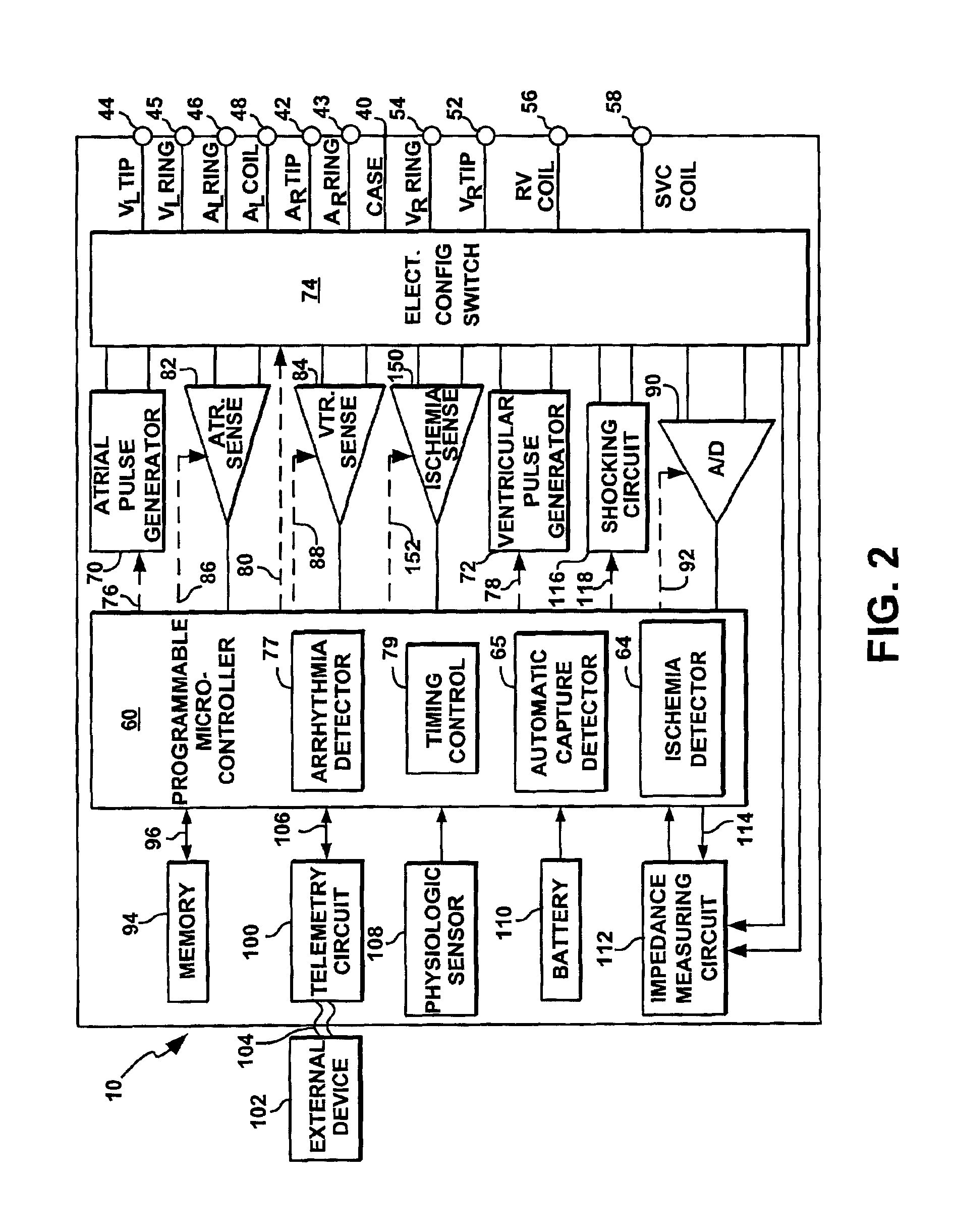
Cardiac stimulation device for optimizing cardiac output with myocardial ischemia protection
InactiveUS6865420B1Reduce demandReduce detectionHeart stimulatorsCardiac muscleIntracardiac Electrogram
A cardiac stimulation device and method detect myocardial ischemia and provide a response for alleviating the ischemia. Myocardial ischemia is detected by identifying changes in the ST-segment of the intracardiac electrogram (EGM) sensed using large sensing electrode surfaces created by electrically coupling one or more cardiac electrodes or by using larger surface area shocking coils. Myocardial ischemia monitoring is performed when stimulation parameters are adjusted for increasing cardiac output, causing an increased metabolic demand to be placed on the myocardium itself. When myocardial ischemia is detected, stimulation parameters are re-adjusted to reduce the demand placed on the myocardium and thereby alleviate the ischemia.
Owner:PACESETTER INC
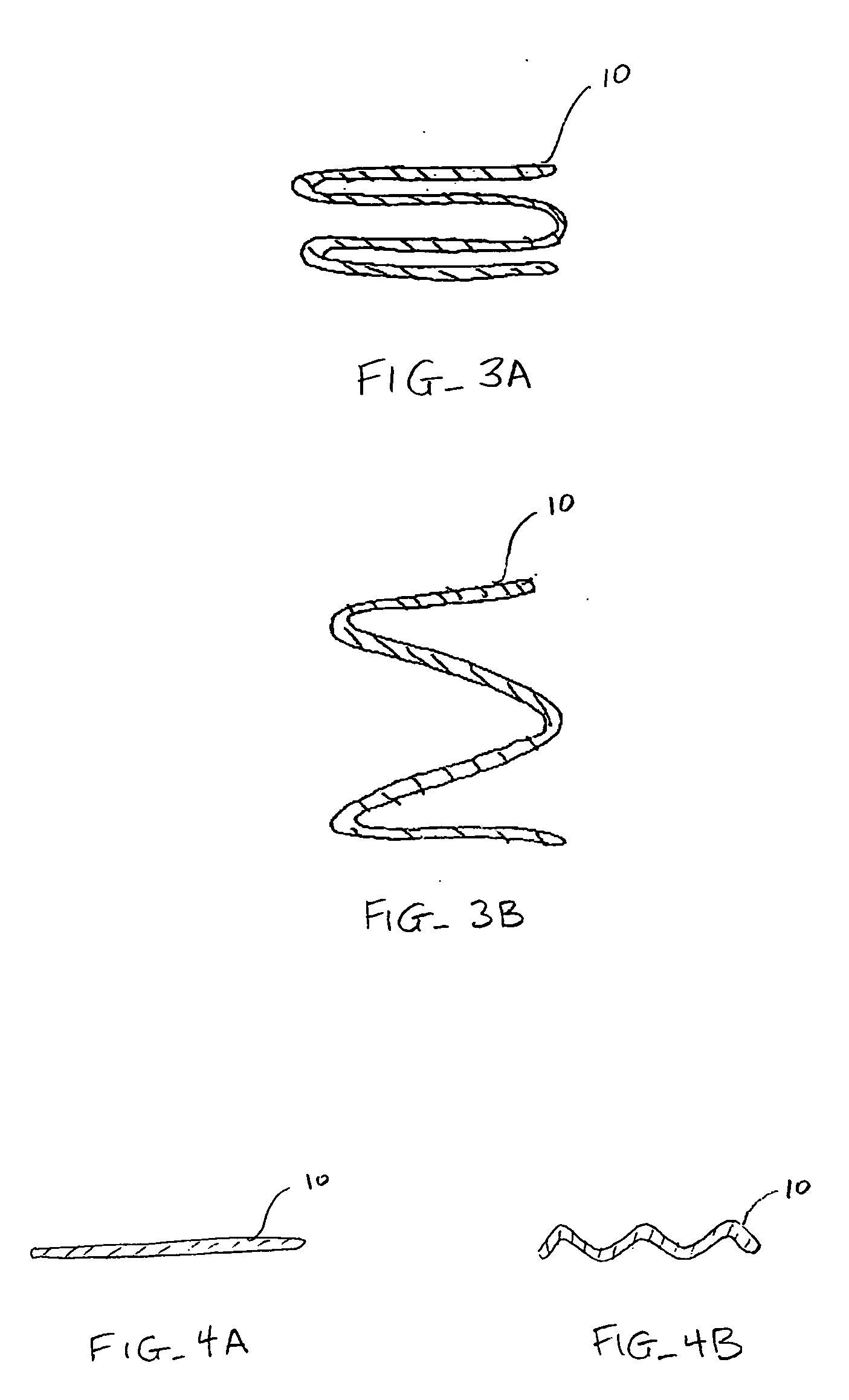
Shape memory devices and methods for reshaping heart anatomy
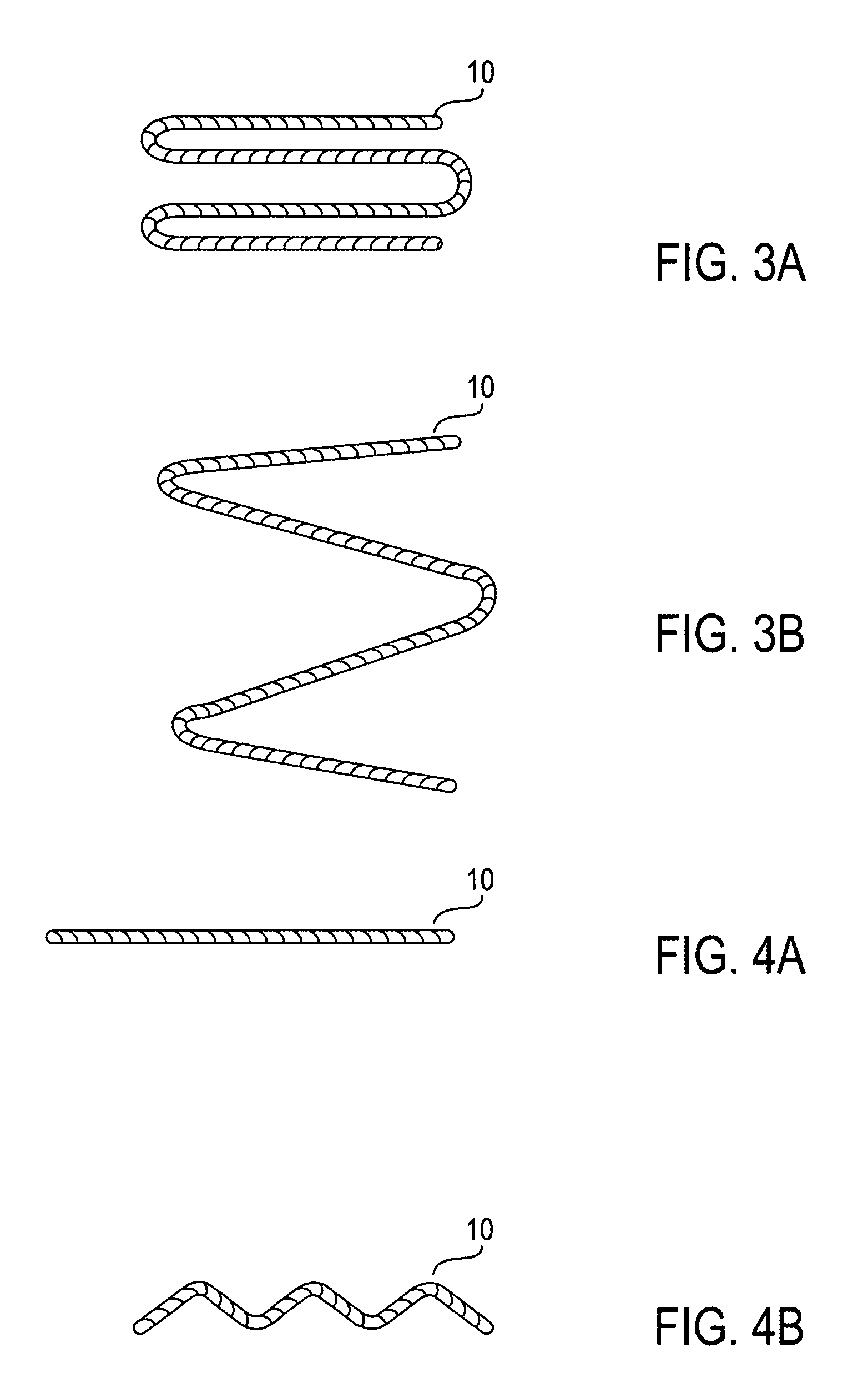
InactiveUS20060015002A1Improve shrinkageReduce widthSuture equipmentsSurgical needlesCardiac surfaceHeart anatomy
Systems, methods and devices are provided for treating heart failure patients suffering from various levels of heart dilation. Such heart dilation is treated by reshaping the heart anatomy with the use of shape memory elements. Such reshaping changes the geometry of portions of the heart, particularly the right or left ventricles, to increase contractibility of the ventricles thereby increasing the stroke volume which in turn increases the cardiac output of the heart. The shape memory elements have an original shape and at least one memory shape. The elements are implanted within the heart tissue or attached externally and / or internally to a surface of the heart when in the original shape. The elements are then activated to transition from the original shape to one of the at least one memory shapes. Transitioning of the elements cause the associated heart tissue areas to readjust position, such as to decrease the width of the ventricles. Such repositioning is maintained over time by the elements, allowing the damaging effects of heart dilation to slow in progression or reverse.
Owner:MICARDIA CORP
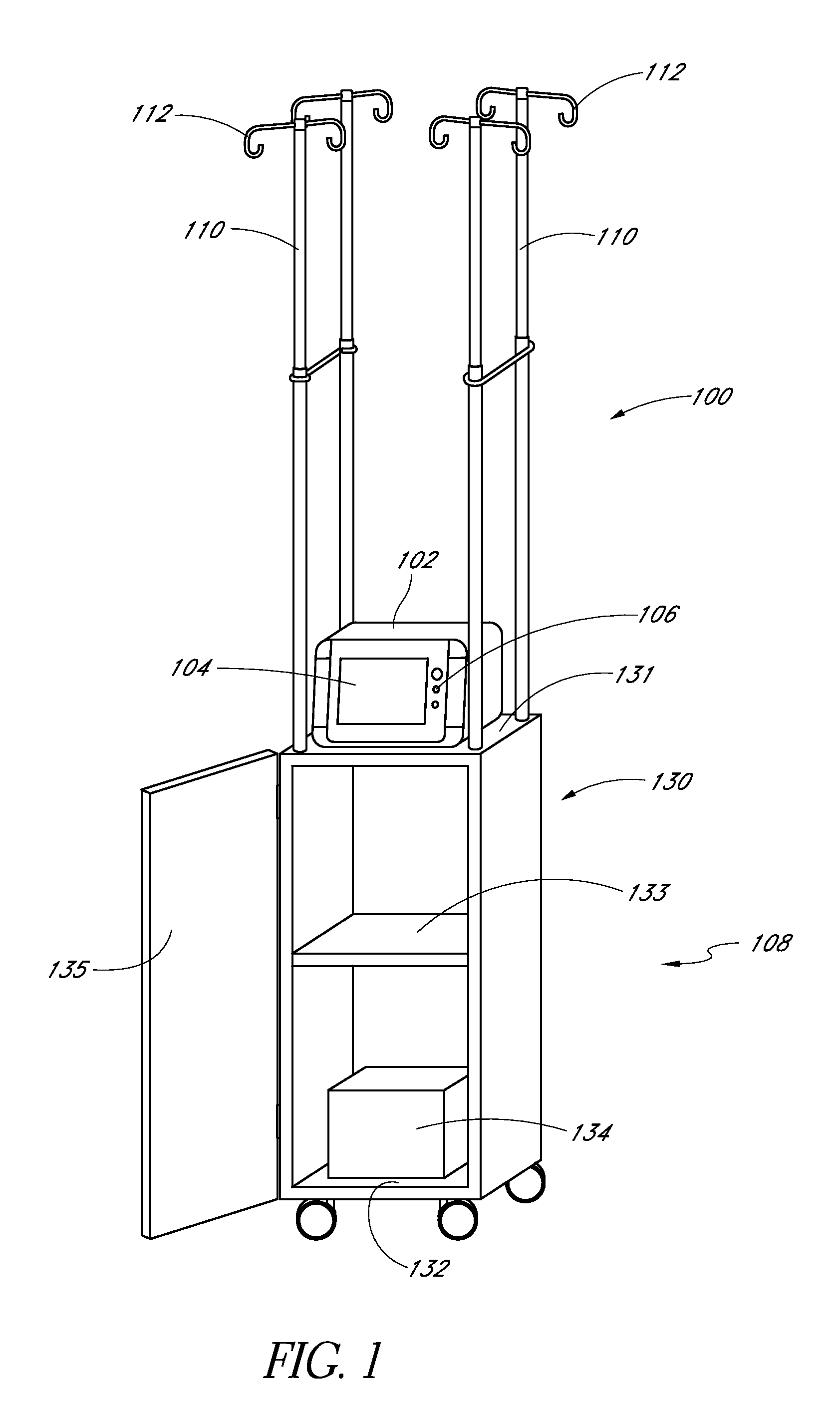
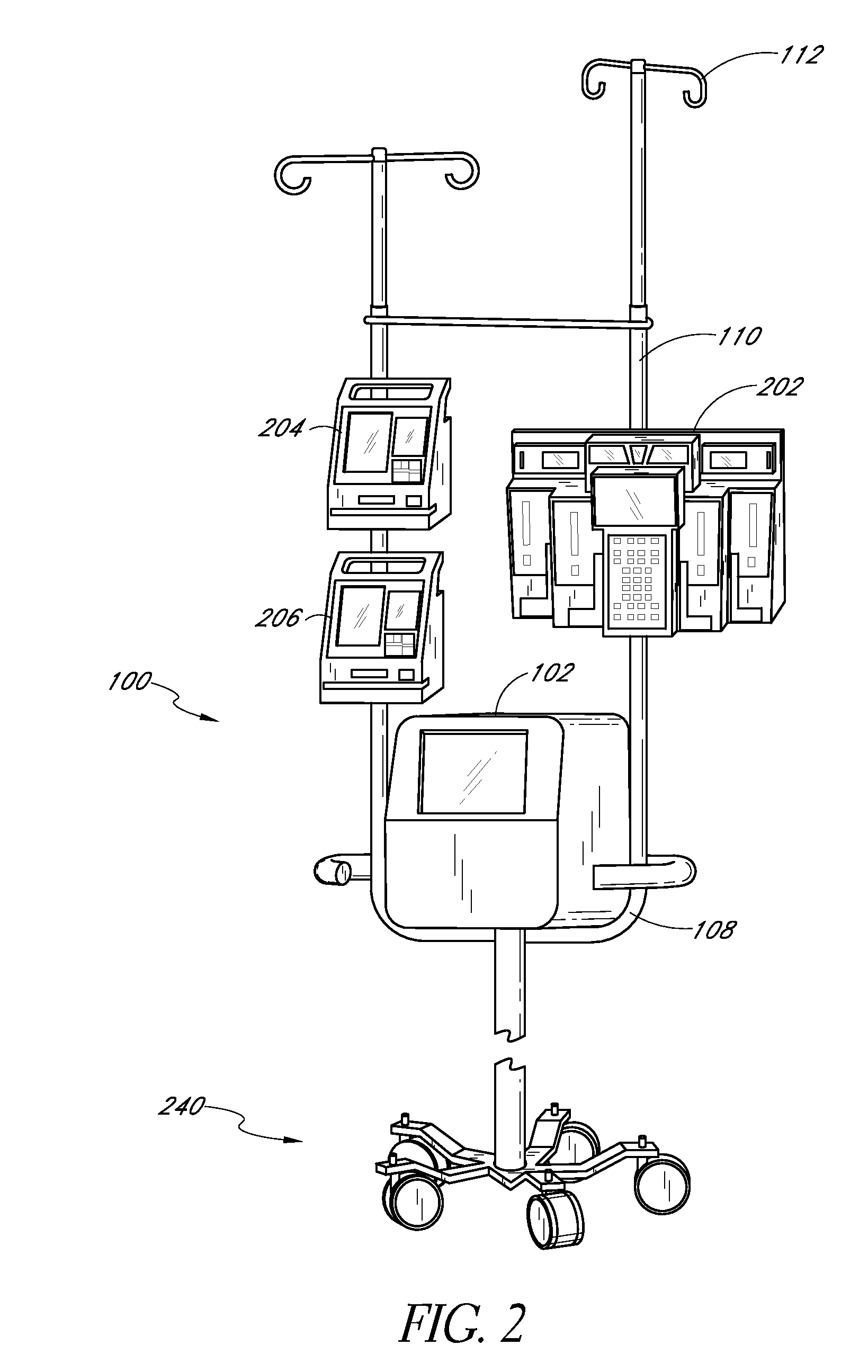
Systems And Methods For Determining Physiological Parameters Using Measured Analyte Values
Systems and methods for determining a physiological parameter in a patient are provided. In certain embodiments, a system can include an analyte detection system configured to measure first analyte data in a fluid sample received from a patient, a medical sensor configured to measure second analyte data in the patient, and a processor configured to receive the first analyte data and the second analyte data and to determine a physiological parameter based at least in part on the first analyte data and the second analyte data. In certain such embodiments, the medical sensor may be a pulse oximeter, and the physiological parameter may include a cardiovascular parameter including, for example, cardiac output.
Owner:OPTISCAN BIOMEDICAL +1
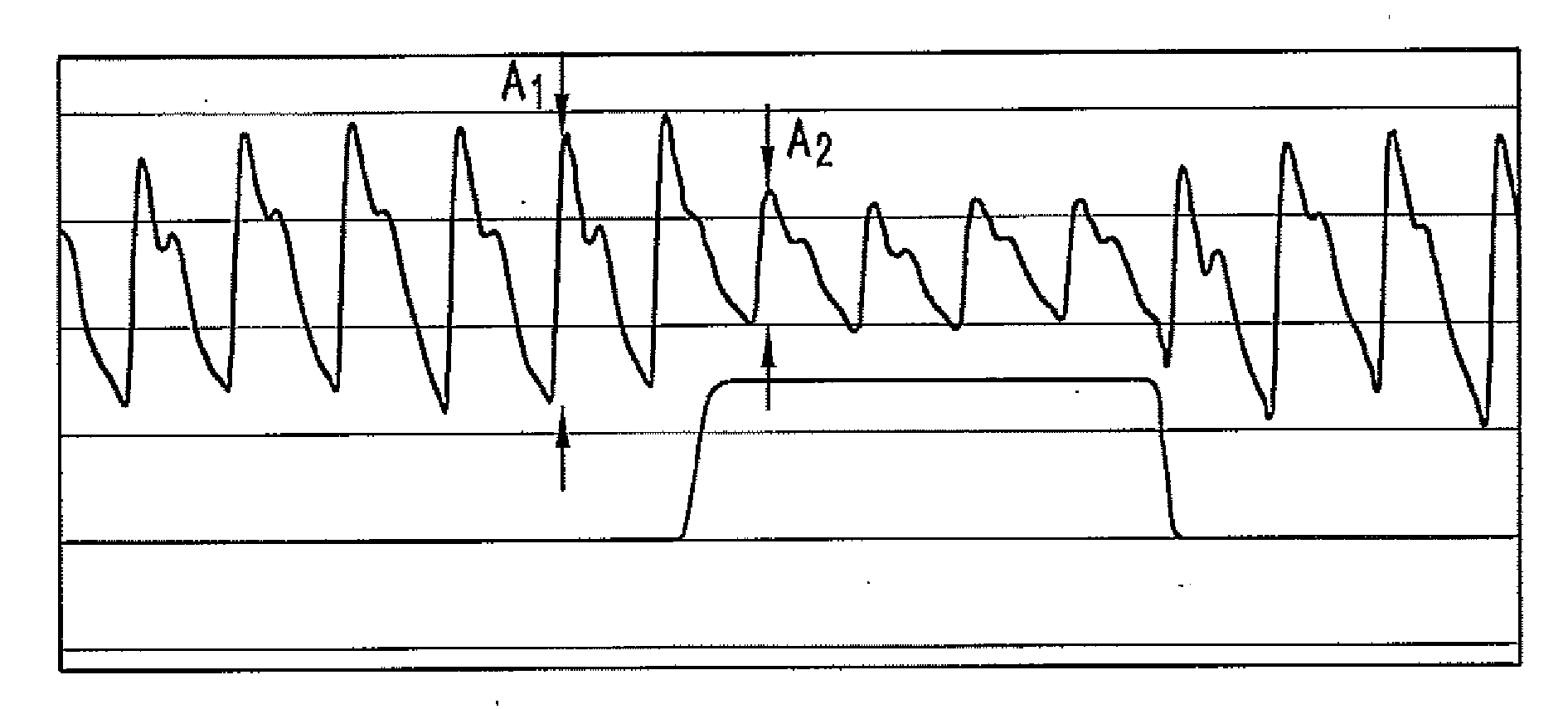
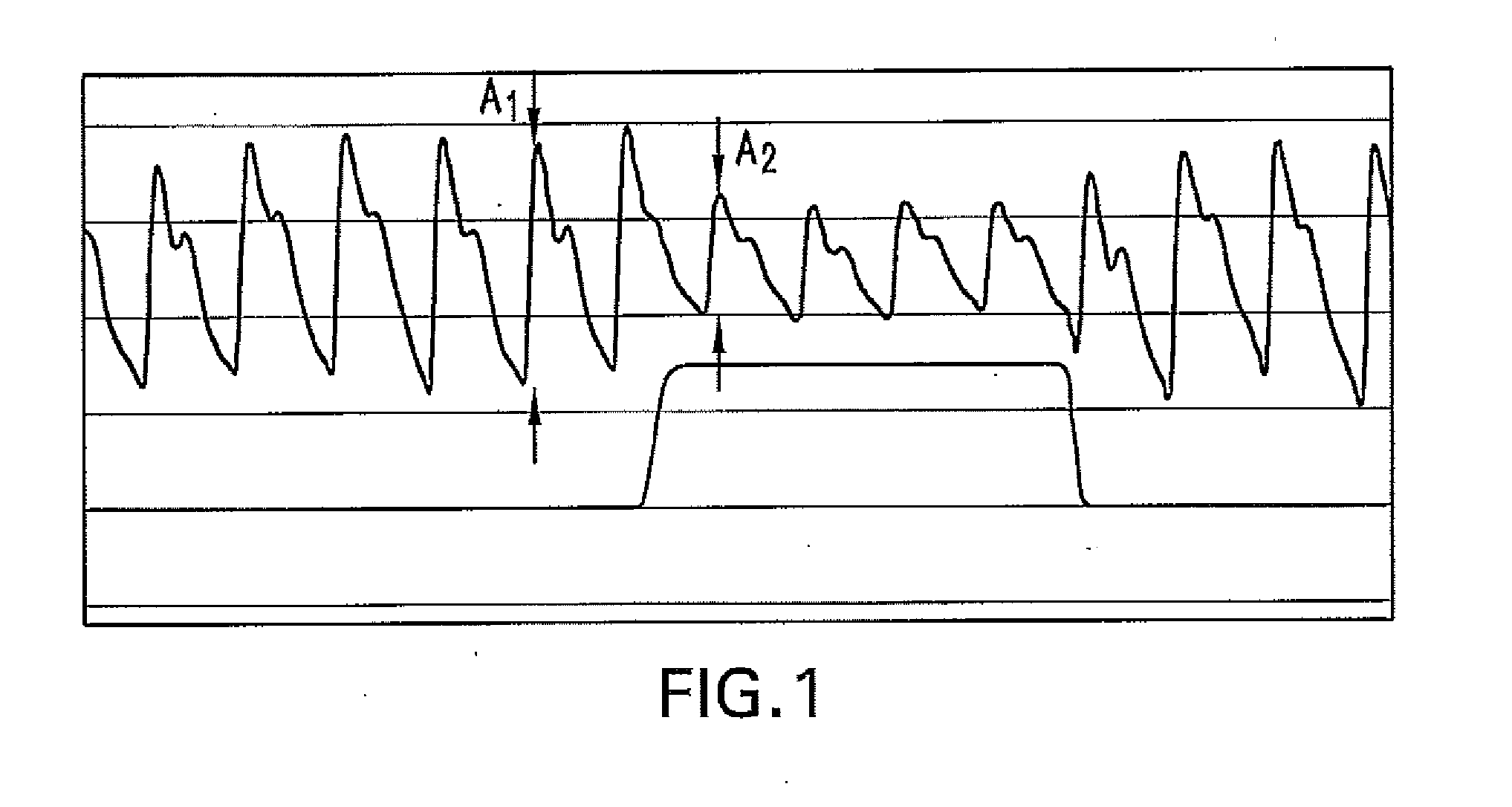
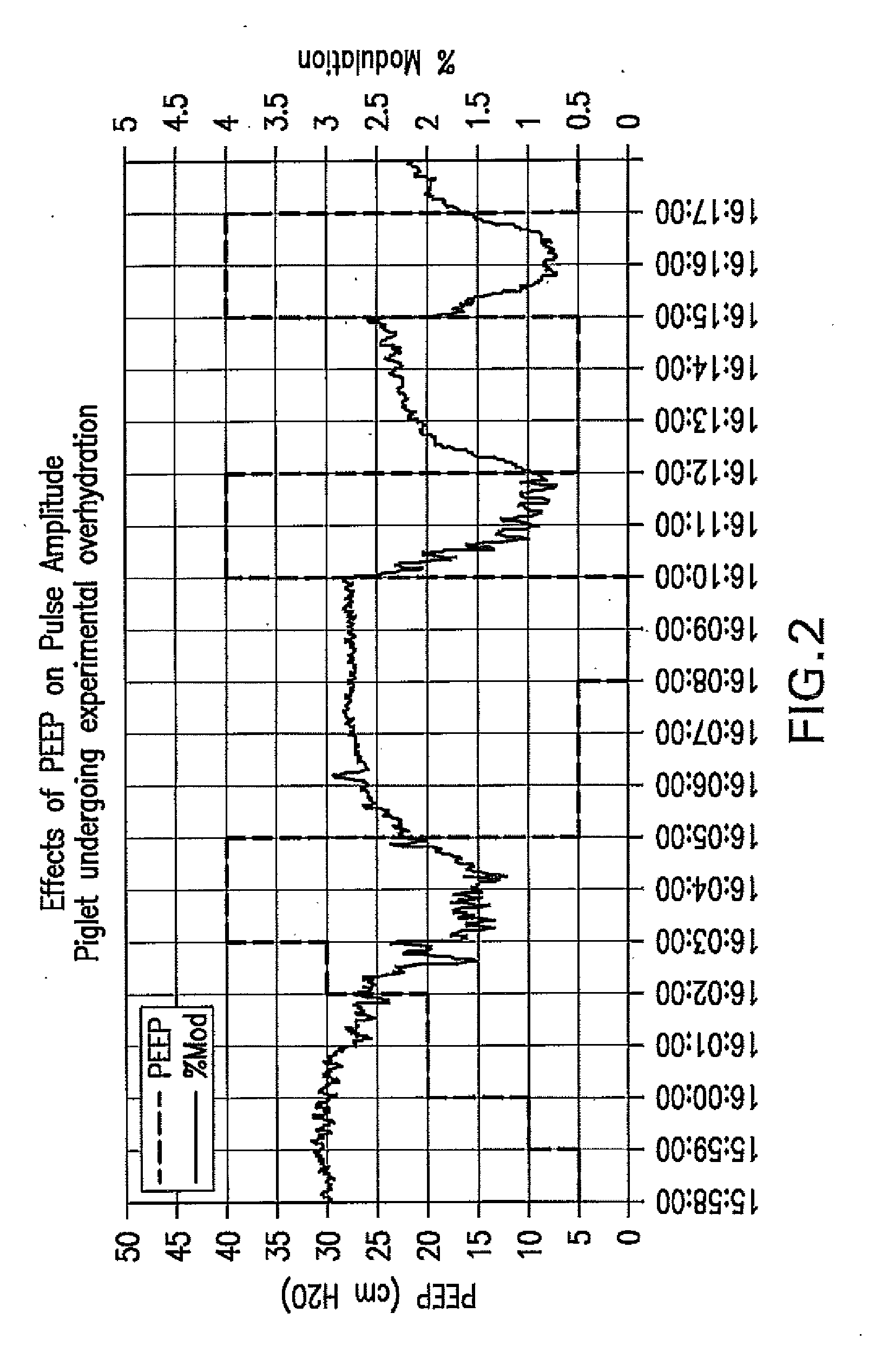
Method For Determining Hemodynamic Effects Of Positive Pressure Ventilation
The present disclosure relates, in some embodiments, to devices, systems, and / or methods for collecting, processing, and / or displaying stroke volume and / or cardiac output data. For example, a device for assessing changes in cardiac output and / or stroke volume of a subject receiving airway support may comprise a processor; an airway sensor in communication with the processor, wherein the airway sensor is configured and arranged to sense pressure in the subject's airway, lungs, and / or intrapleural space over time; a blood volume sensor in communication with the processor, wherein the blood volume sensor is configured and arranged to sense pulsatile volume of blood in a tissue of the subject over time; and a display configured and arranged to display a representative of an airway pressure, a pulsatile blood volume, a photoplethysmogram, a photoplethysmogram ratio, the determined cardiac output and / or stroke volume, or combinations thereof. A method of assessing changes in cardiac output or stroke volume of a subject receiving airway support from a breathing assistance system may comprise sensing pressure in the subject's airway as a function of time, sensing pulsatile volume of blood in a tissue of the subject as a function of time, producing a photoplethysmogram from the sensed pulsatile volume, determining the ratio of the amplitude of the photoplethysmogram during inhalation to the amplitude of the photoplethysmogram during exhalation, and determining the change in cardiac output or stroke volume of the subject using the determined ratio.
Owner:TYCO HEALTHCARE GRP LP
Wavelet based feature extraction and dimension reduction for the classification of human cardiac electrogram depolarization waveforms
ActiveUS20080109041A1Improve accuracyPrecise processElectrocardiographyMedical automated diagnosisCardiac pacemaker electrodeClassification methods
A depolarization waveform classifier based on the Modified lifting line wavelet Transform is described. Overcomes problems in existing rate-based event classifiers. A task for pacemaker / defibrillators is the accurate identification of rhythm categories so correct electrotherapy can be administered. Because some rhythms cause rapid dangerous drop in cardiac output, it's desirable to categorize depolarization waveforms on a beat-to-beat basis to accomplish rhythm classification as rapidly as possible. Although rate based methods of event categorization have served well in implanted devices, these methods suffer in sensitivity and specificity when atrial / ventricular rates are similar. Human experts differentiate rhythms by morphological features of strip chart electrocardiograms. The wavelet transform approximates human expert analysis function because it correlates distinct morphological features at multiple scales. The accuracy of implanted rhythm determination can then be improved by using human-appreciable time domain features enhanced by time scale decomposition of depolarization waveforms.
Owner:BIOTRONIK SE & CO KG
Apparatus and method for non-invasive and minimally-invasive sensing of parameters relating to blood
InactiveUS20060253007A1Reduce disadvantagesImprove accuracyDiagnostics using lightOrgan movement/changes detectionNon invasiveThree vessels
Medical diagnostic system, apparatus and methods are disclosed. Optical transmitters generate radiation-containing photons having a specific interaction with at least one target chromophore in a target structure, preferably a blood vessel such as the interior jugular vein. The optical transmitters transmit the radiation into at least a first area including a substantial portion of the target structure and into a second area not including a substantial portion of the target structure. Optical receivers detect a portion radiation scattered from at least the first area and the second area. A processor estimates oxygenation, pH or cardiac output based on the scattered radiation detected from the first area, and the scattered radiation from the second area.
Owner:SKYLINE BIOMEDICAL
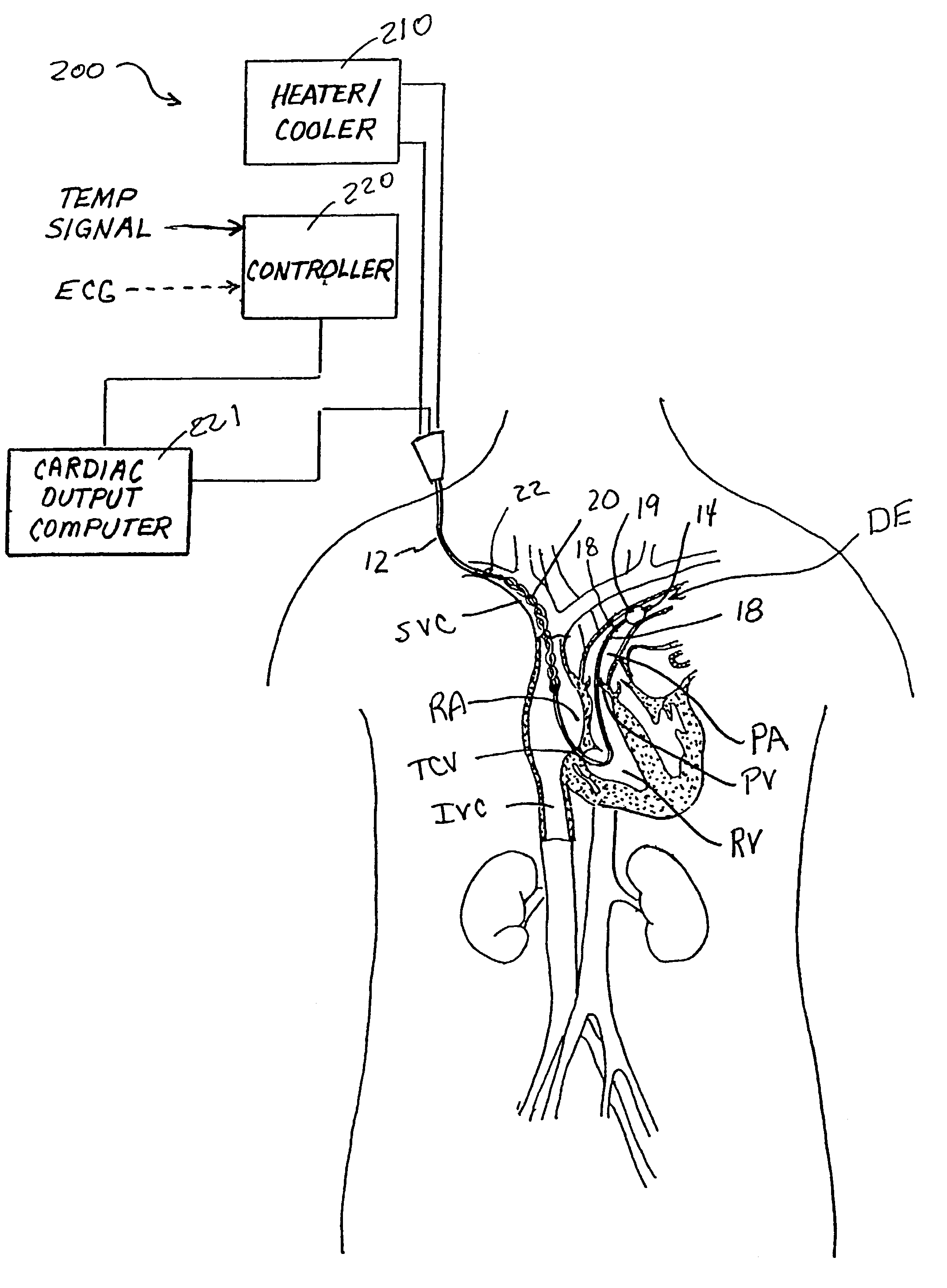
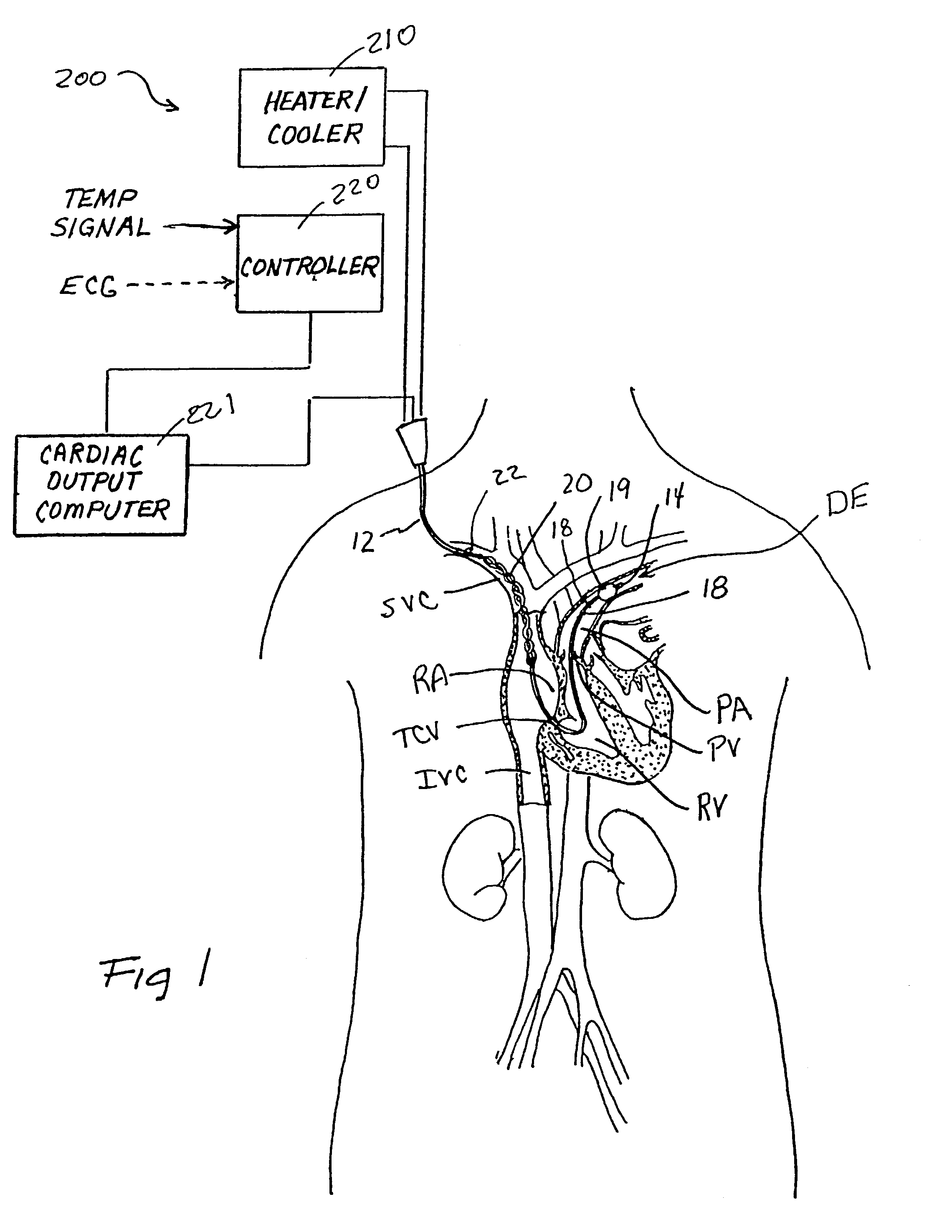
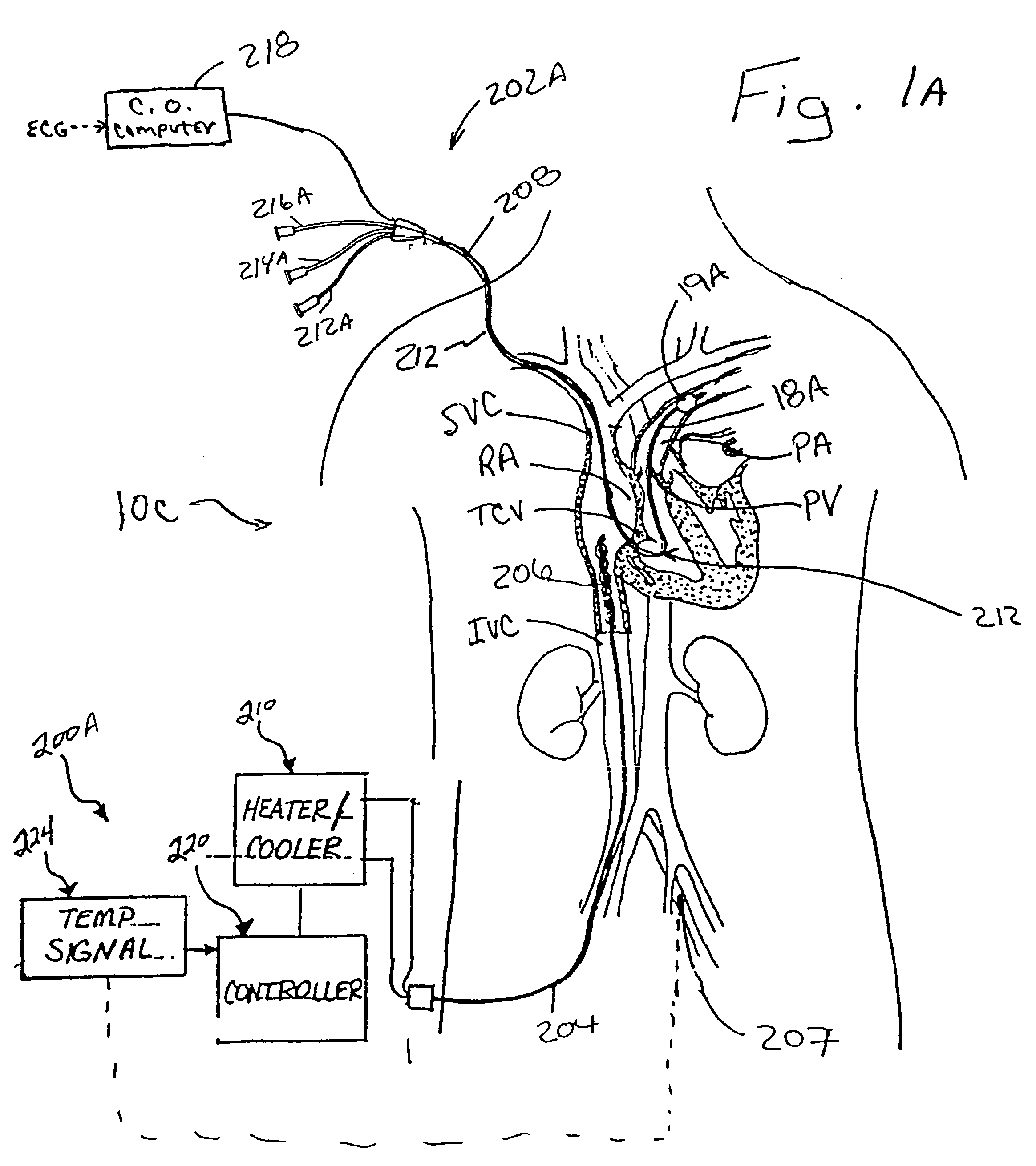
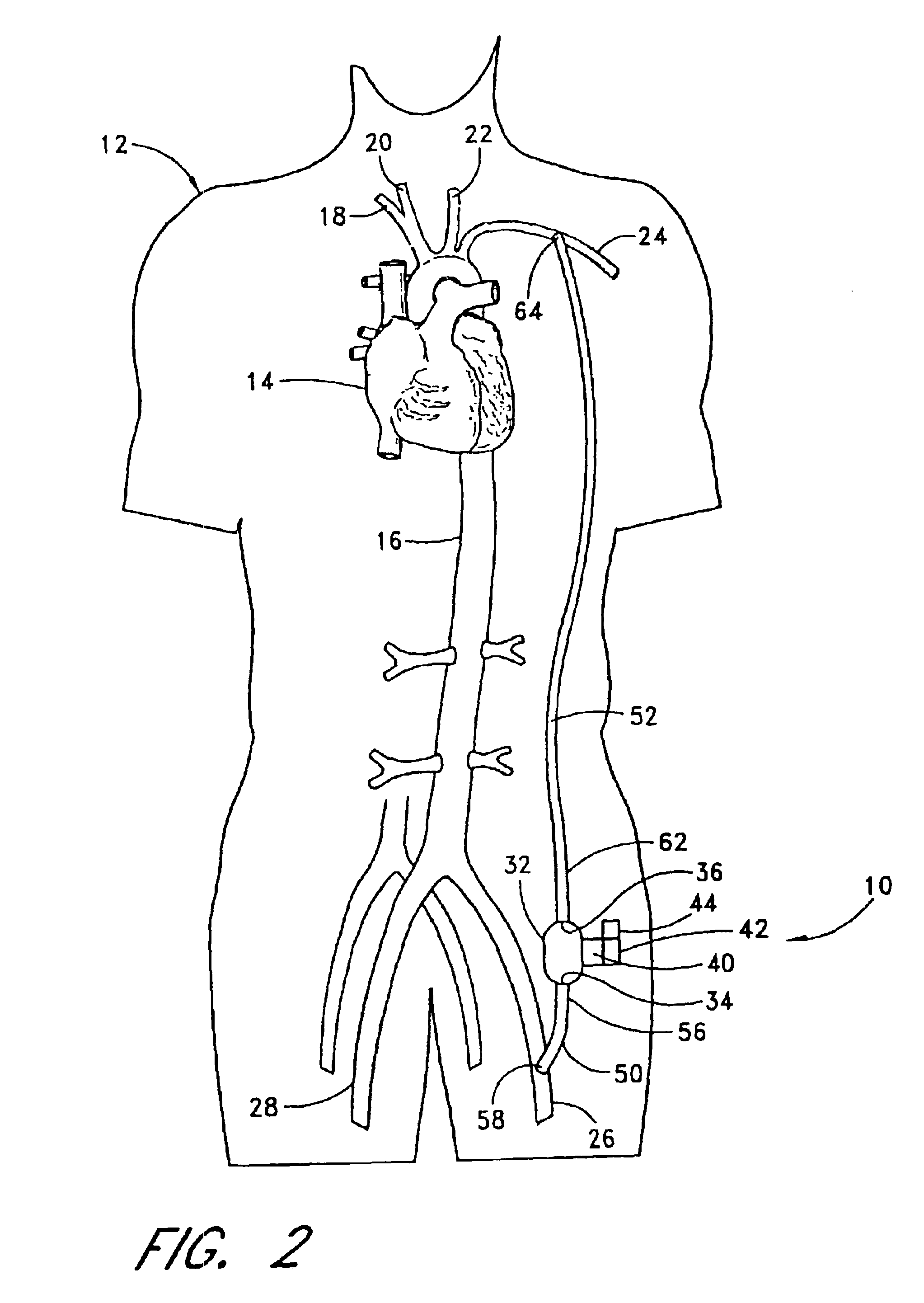
Devices and methods for measuring blood flow rate or cardiac output and for heating or cooling the body
Heat exchanger-equipped catheters and related methods that are useable for changing or maintaining at least a portion of the body of a human or veterinary patient at a desired temperature and for the measurement of cardiac output or blood flow rate within a blood vessel, without the need for introduction of saline solution or any other foreign substance into the patient's blood.
Owner:ZOLL CIRCULATION
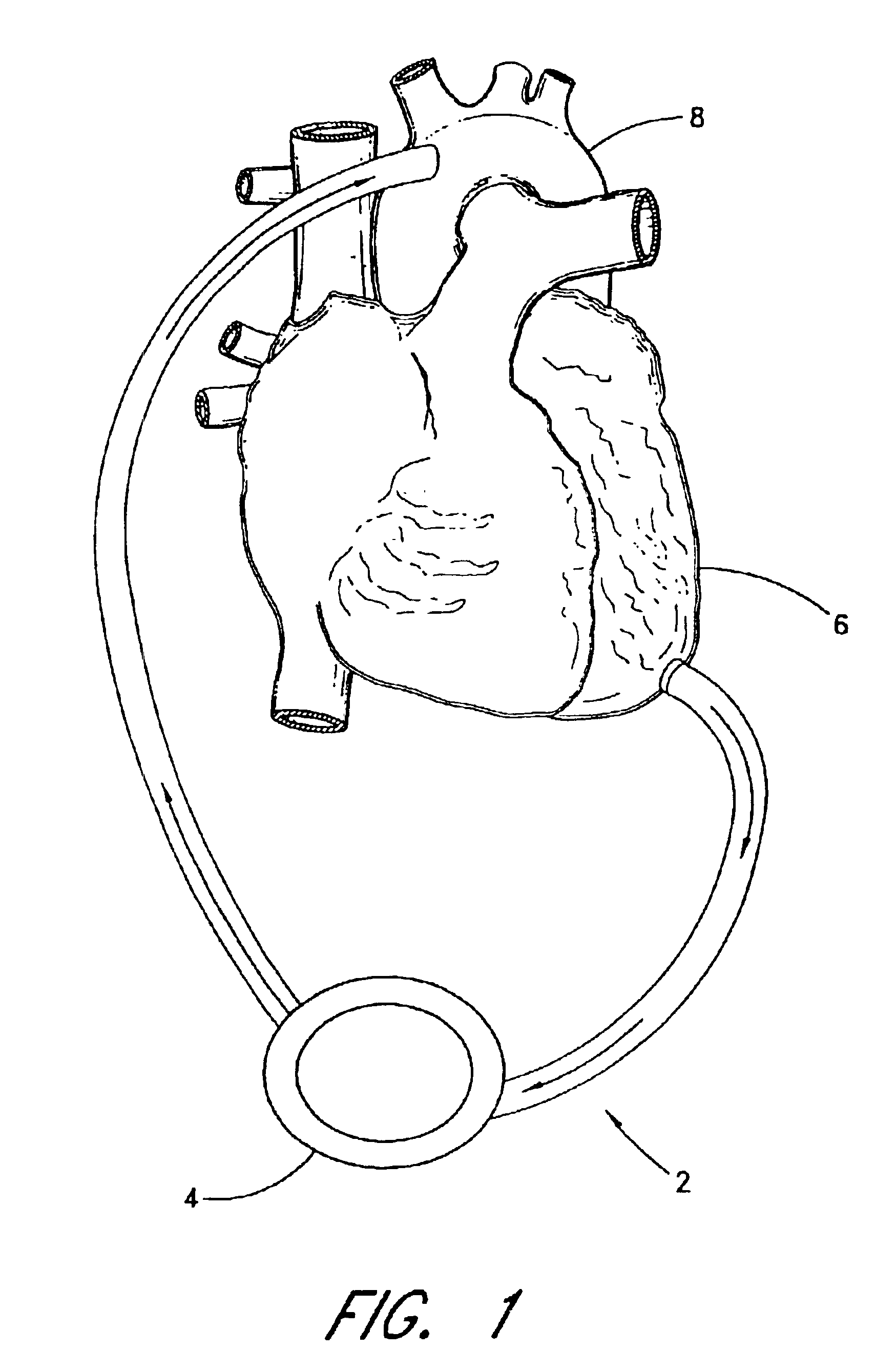
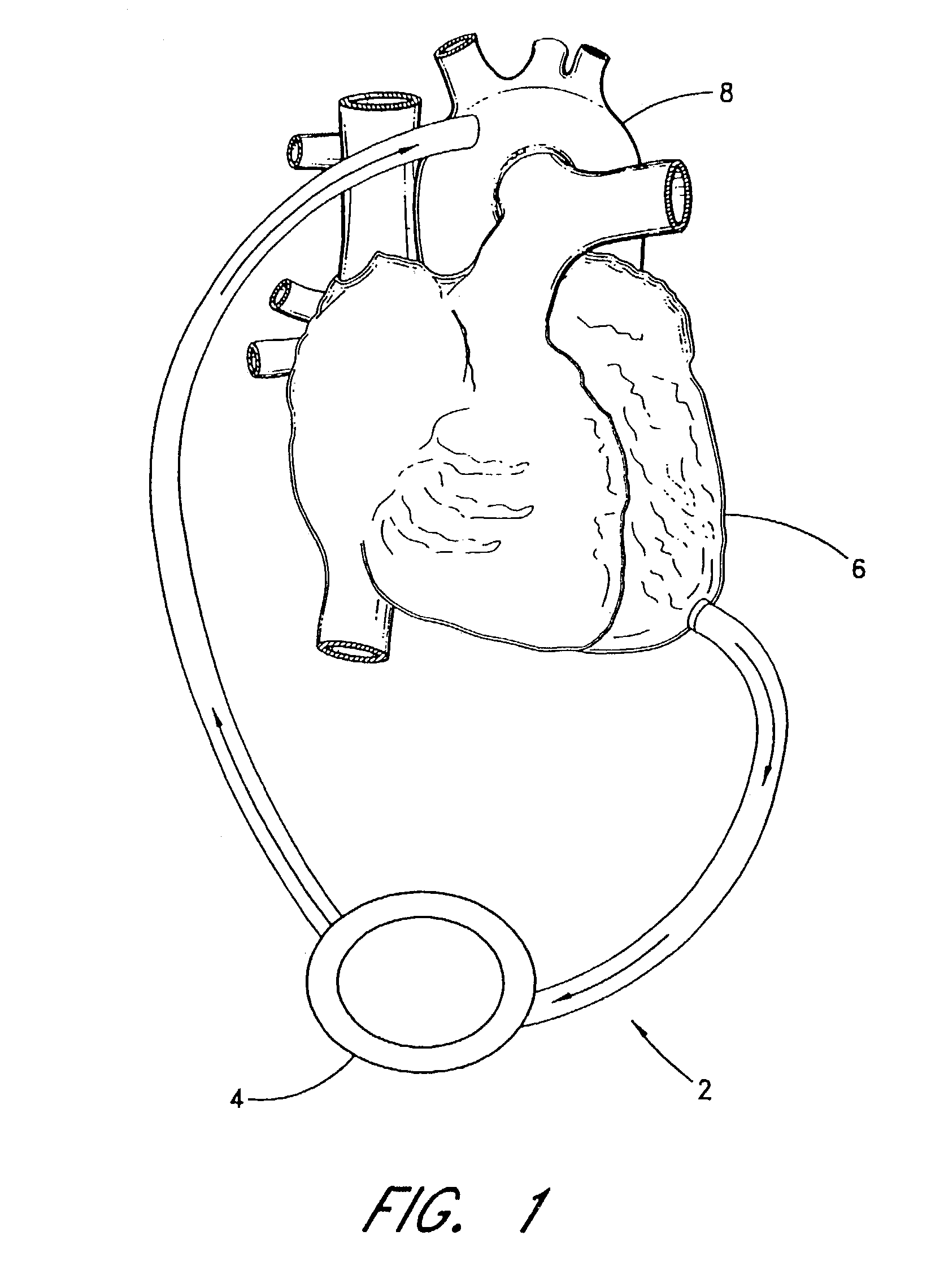
Implantable heart assist system and method of applying same
InactiveUS6889082B2RevitalizeReduce energy inputElectrotherapyElectrocardiographyMinimally invasive proceduresCatheter
An extracardiac pumping for supplementing the circulation of blood, including the cardiac output, in a patient without any component thereof being connected to the patient's heart, and methods of using same. One embodiment provides a vascular graft that has a first end that is sized and configured to couple to a non-primary blood vessel and a second end that is fluidly coupled to a pump to conduct blood between the pump and the non-primary blood vessel. An outflow conduit is also provided that has a first end sized and configured to be positioned within the same or different blood vessel, whether primary or non-primary, through the vascular graft. The outflow conduit is fluidly coupled to the pump to conduct blood between the pump and the patient. The vascular graft may be connected to the blood vessel subcutaneously to permit application of the extracardiac pumping system in a minimally-invasive procedure.
Owner:TC1 LLC +1
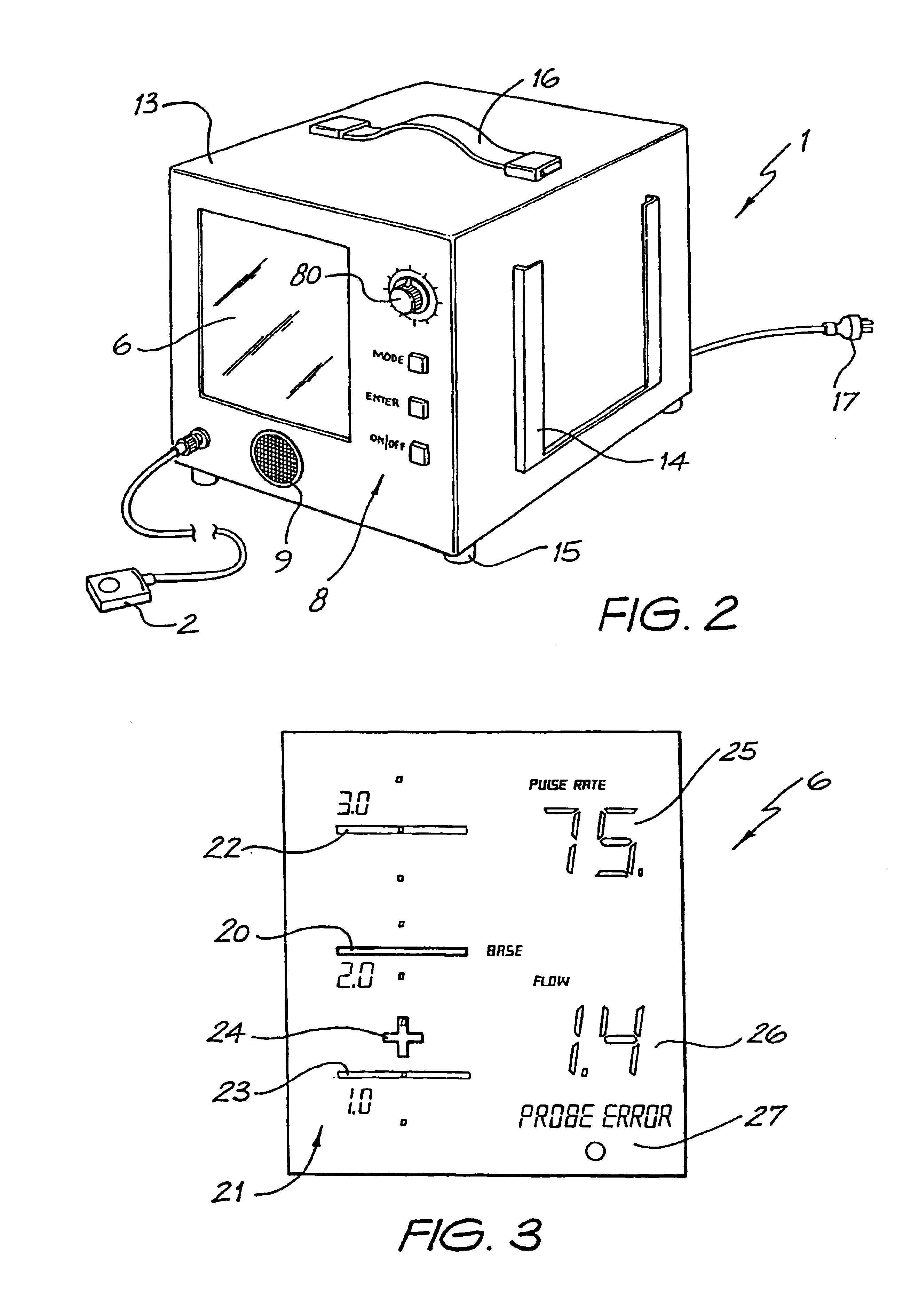
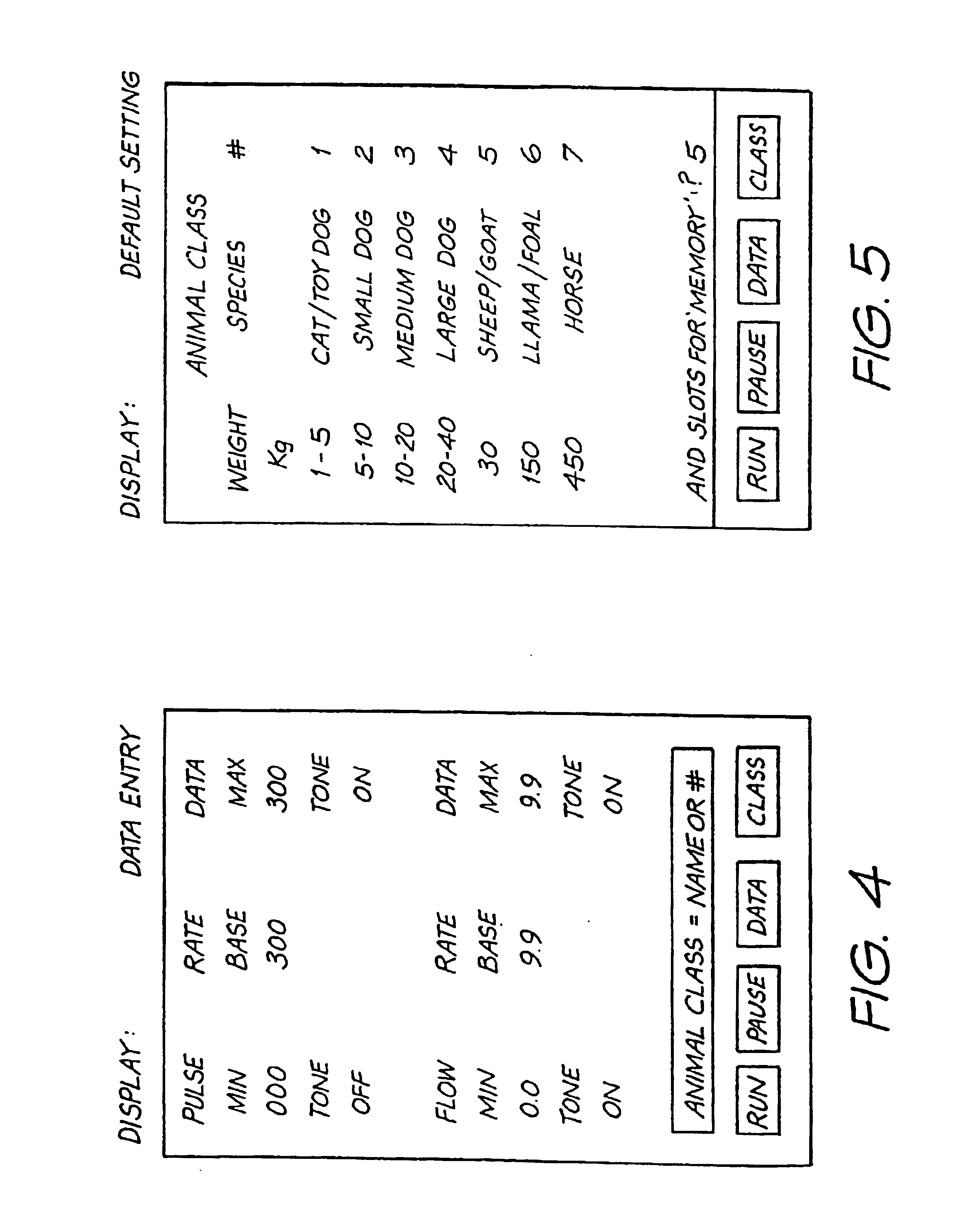
Method and apparatus for monitoring haemodynamic function
InactiveUS6939307B1Accurate indicationAccurate of oxygen deliveryBlood flow measurement devicesCatheterBlood flowBiology
The present invention relates to a method and apparatus for monitoring haemodynamic function in animals and humans during anaesthesia and surgery. During anaesthesia and surgery the subject's haemodynamic, respiratory, neuromuscular and neurological functions are monitored as indicators of the condition of the health of the subject. Commonly, variations in blood pressure are used to imply corresponding variations in cardiac output, i.e. good blood pressure equals good cardiac output. The present invention utilizes a device to monitor changes of blood flow in peripheral blood vessels of the subject as an indicator of cardiac output. This is believed to provide a much more accurate indicator.
Owner:DUNLOP COLIN
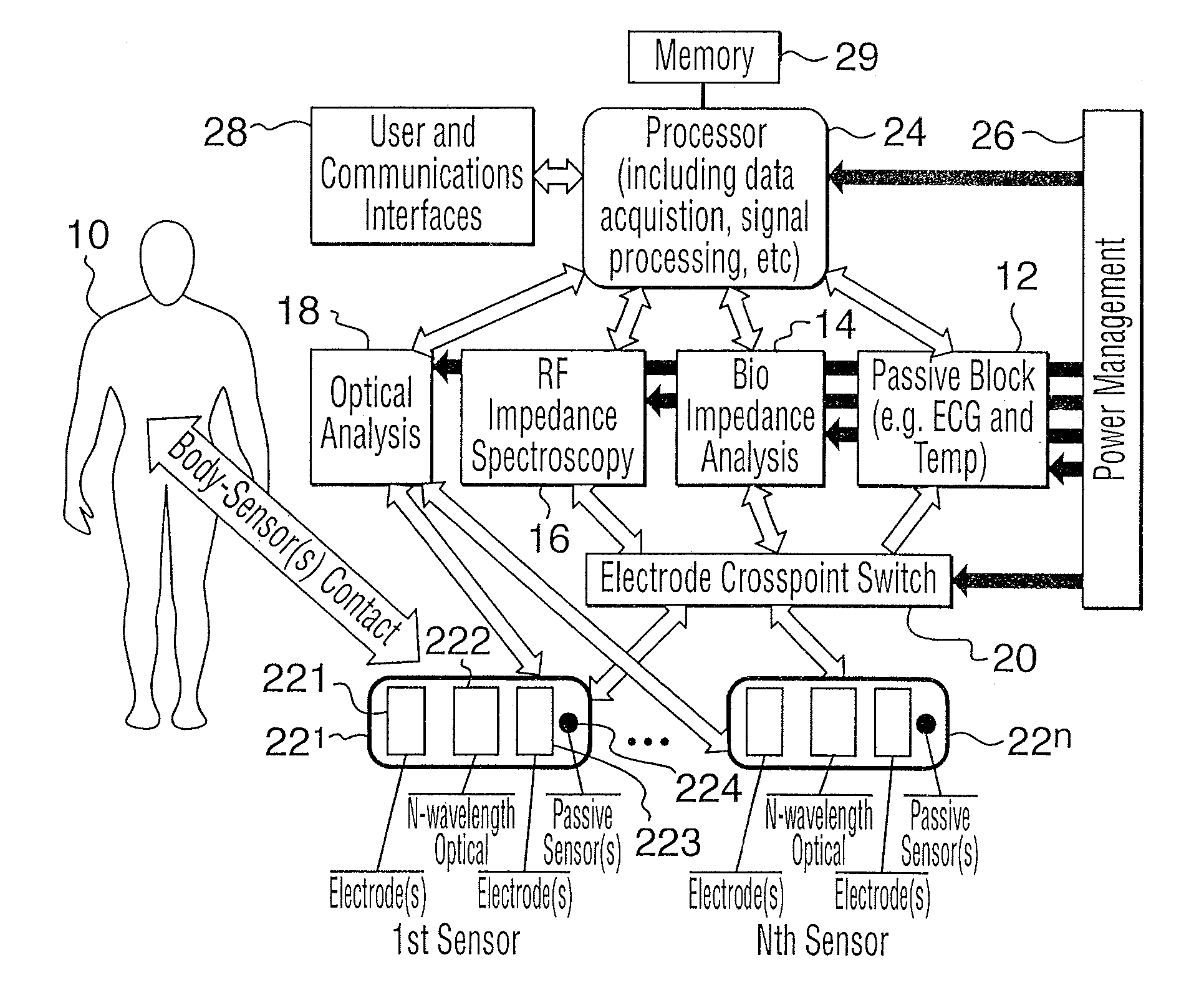
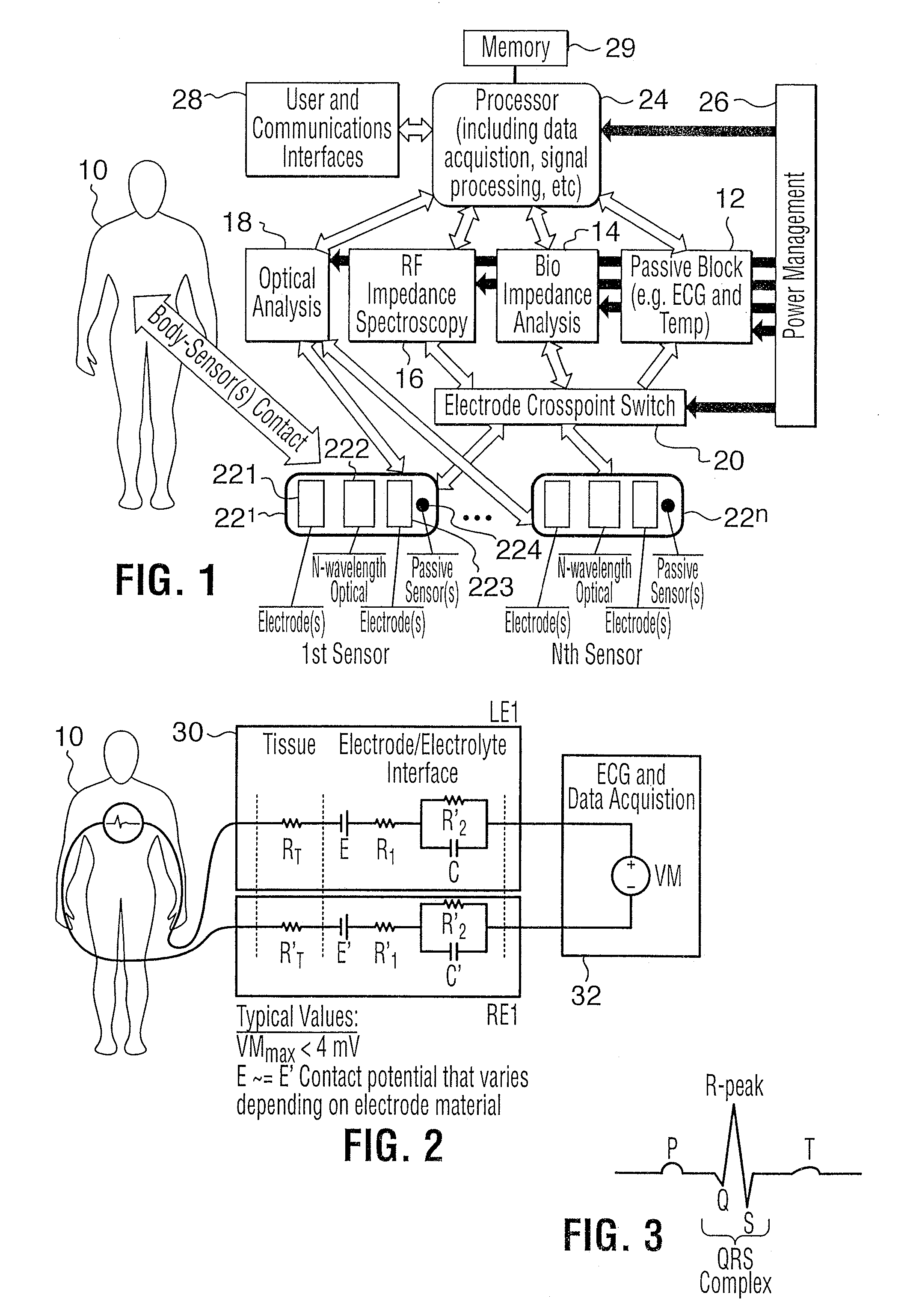
Non-invasive method and apparatus for determining a physiological parameter
InactiveUS20100004517A1Accurate measurementThe result is accurateElectrotherapyElectrocardiographyMeasurement deviceNon invasive
The present invention relates to an apparatus and method for the non-invasive analysis of physiological attributes, such as heart rate, blood pressure, cardiac output, respiratory response, body composition, and blood chemistry analytes including glucose, lactate, hemoglobin, and oxygen saturation. Using a combination of multi-functioning disparate sensors, such as optical and electrical, improvements are made over existing physiological measurement devices and techniques. The special configuration of one or more multi-functional sensors is used to non-invasively measure multi-wavelength optical plus one or more of ECG, Bio-impedance, and RF-impedance spectroscopic data. This information is used to develop self-consistent, non-linear algorithm in order to derive the physiological attributes while compensating for various forms of interfering effects including motion artifacts, sensor attachment variability, device component variability, subject physical and physiology variability, and various interfering physiological attributes.
Owner:BIOPEAK CORP
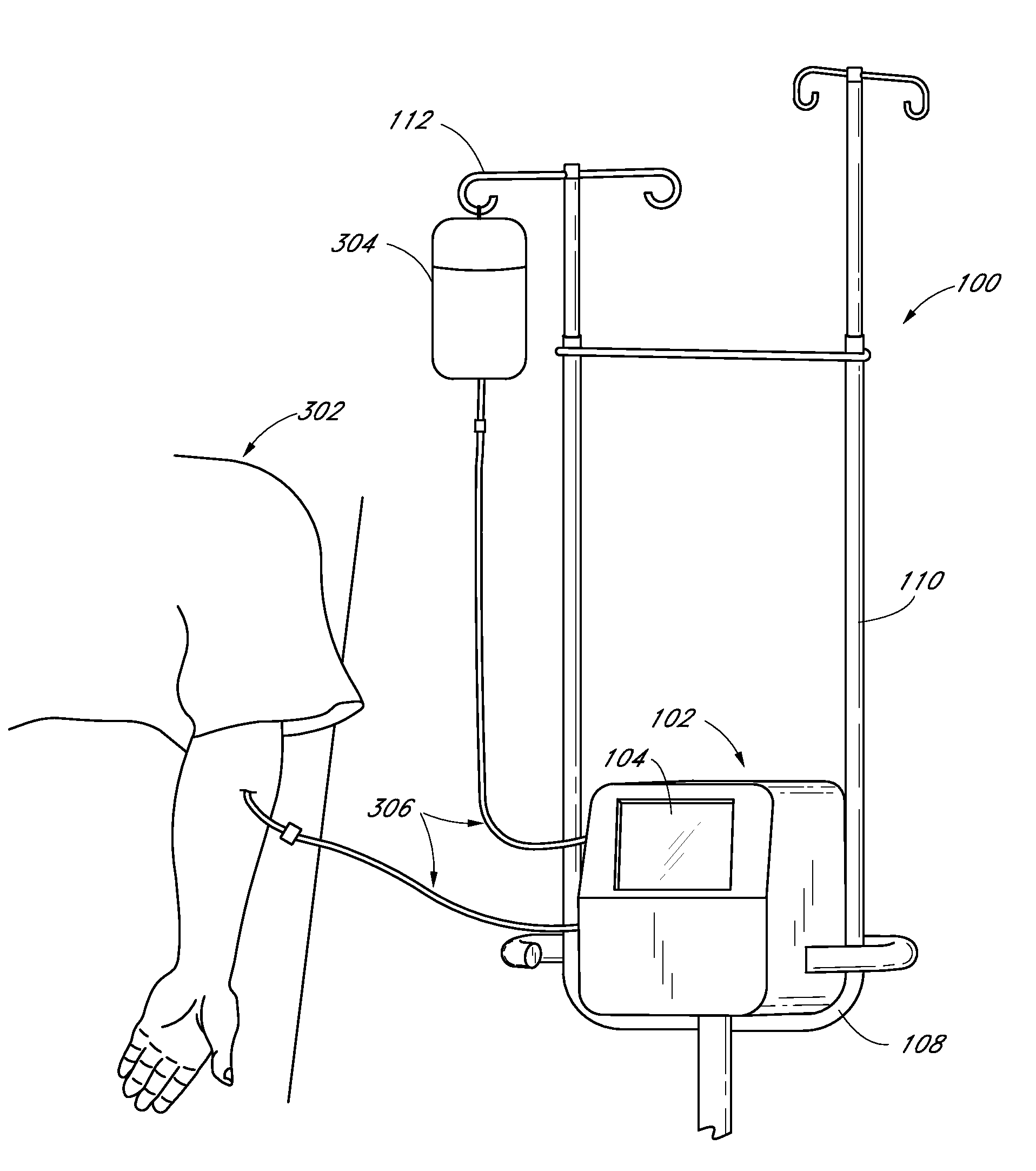
Methods and devices for improving cardiac output
InactiveUS7077801B2Facilitate cardiac output functionEliminate the problemExcision instrumentsIntravenous devicesProsthesisCatheter
Methods and devices are provided for improving cardiac output. The methods involve establishing a fluid communication pathway between the left ventricle and another natural or prosthetic structure. In one method, a conduit is implanted between the left ventricle and the descending aorta where ventricular blood flows from the left ventricle directly into the descending aorta and bypassing the aortic valve. The devices include such conduits and valves for forming the fluid communication pathways.
Owner:CORLIFE GBR
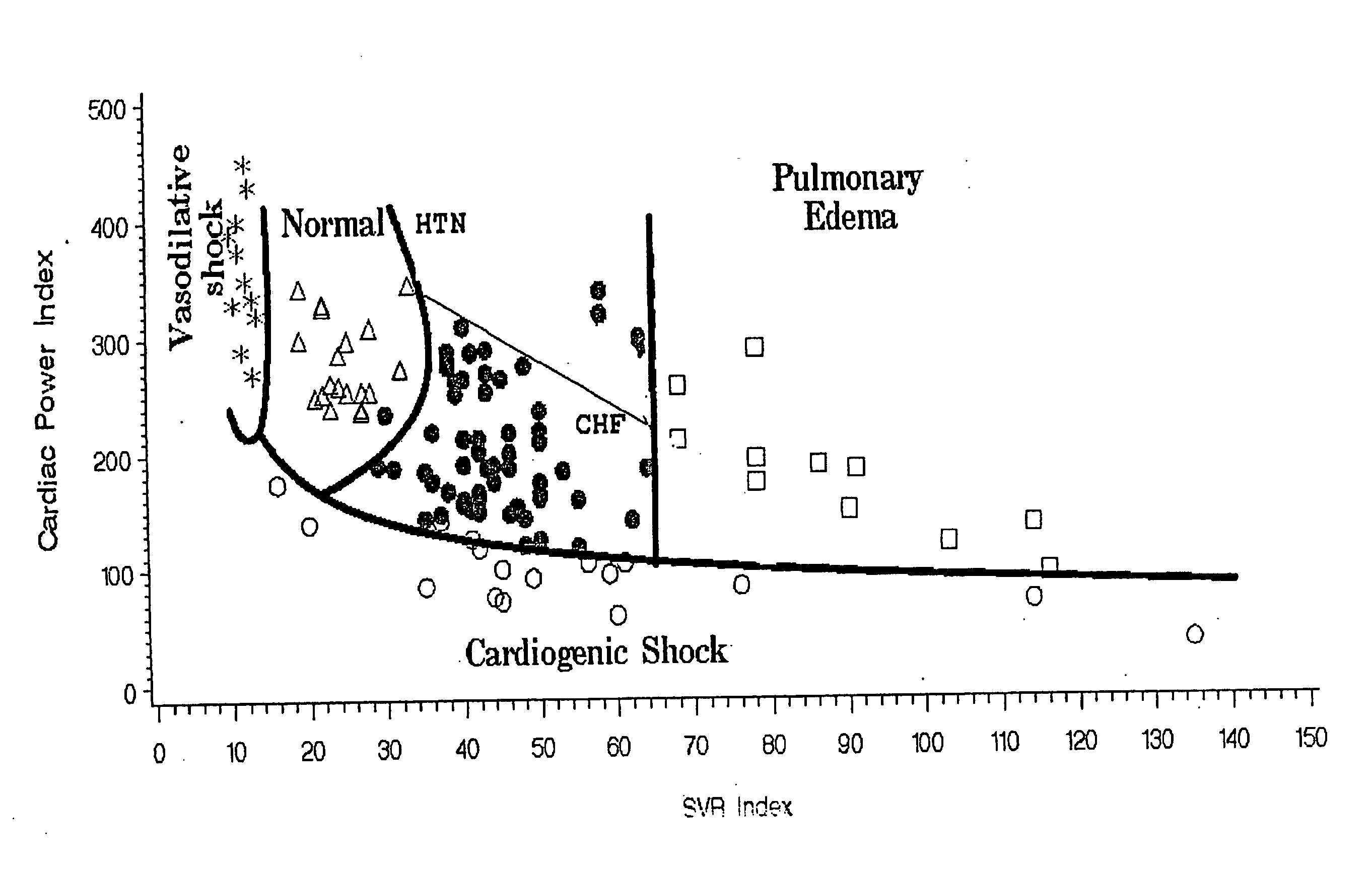
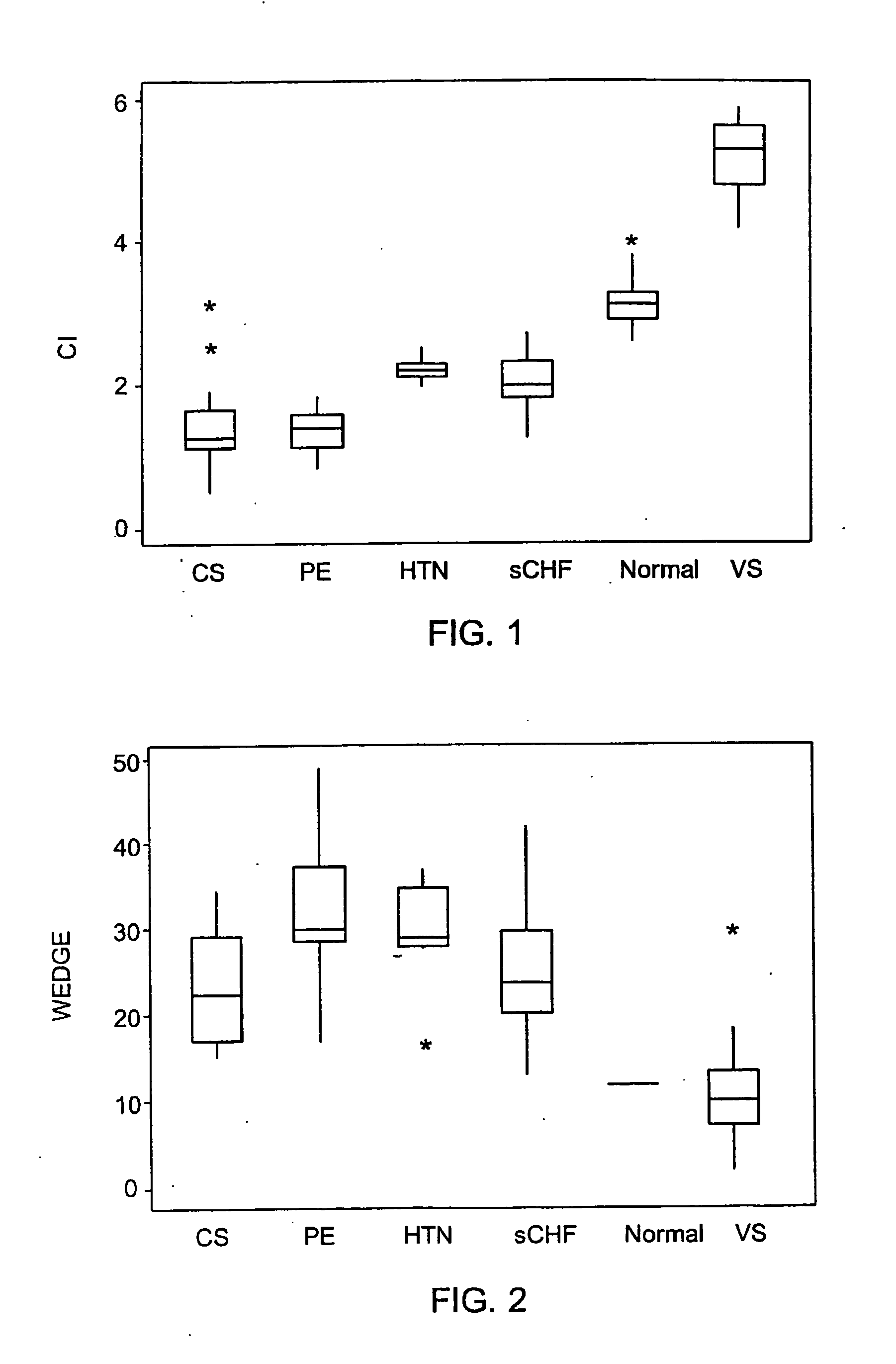
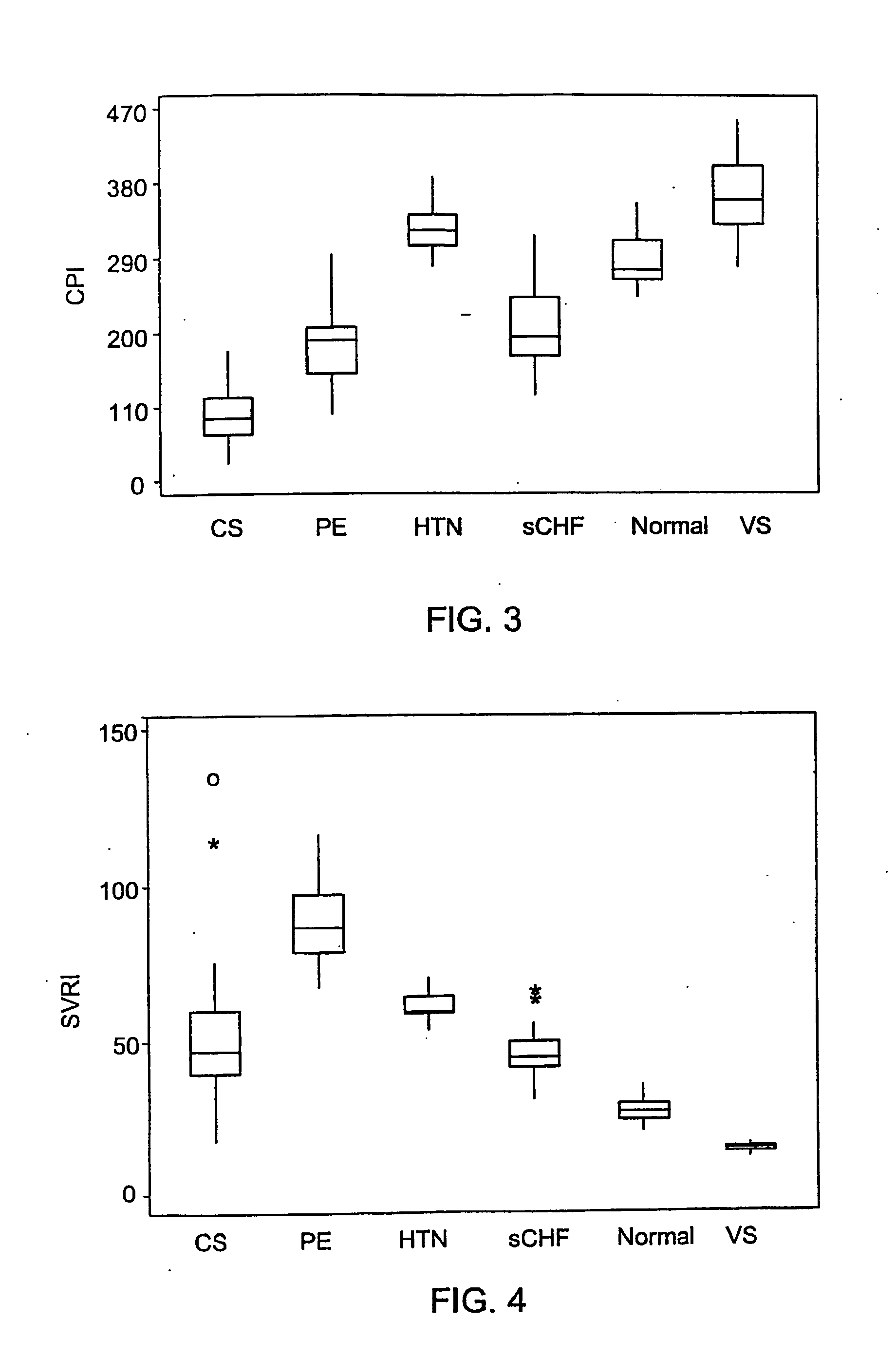
Device for determining hemodynamic state
InactiveUS20050090753A1Easy to monitorEffectivity of a treatment may be assessedCatheterSensorsElectricityWhole body
A non-invasive device for determining the hemodynamic state of a subject. The device comprises: (a) at least two electrodes (20); (b) an electrical total body integral bioimpedance measuring unit (26) coupled to the electrodes; and (c) a data processing and analyzing unit (30) coupled to the electrical integral bioimpedance measuring unit and optionally to a display means (34) for calculating the cardiac output of the subject from the active component of the-integral bioimpedance. Also disclosed are methods for determining the hemodynamic state of a subject and for diagnosing a tendency of a subject to a cardiac disease.
Owner:N I MEDICAL
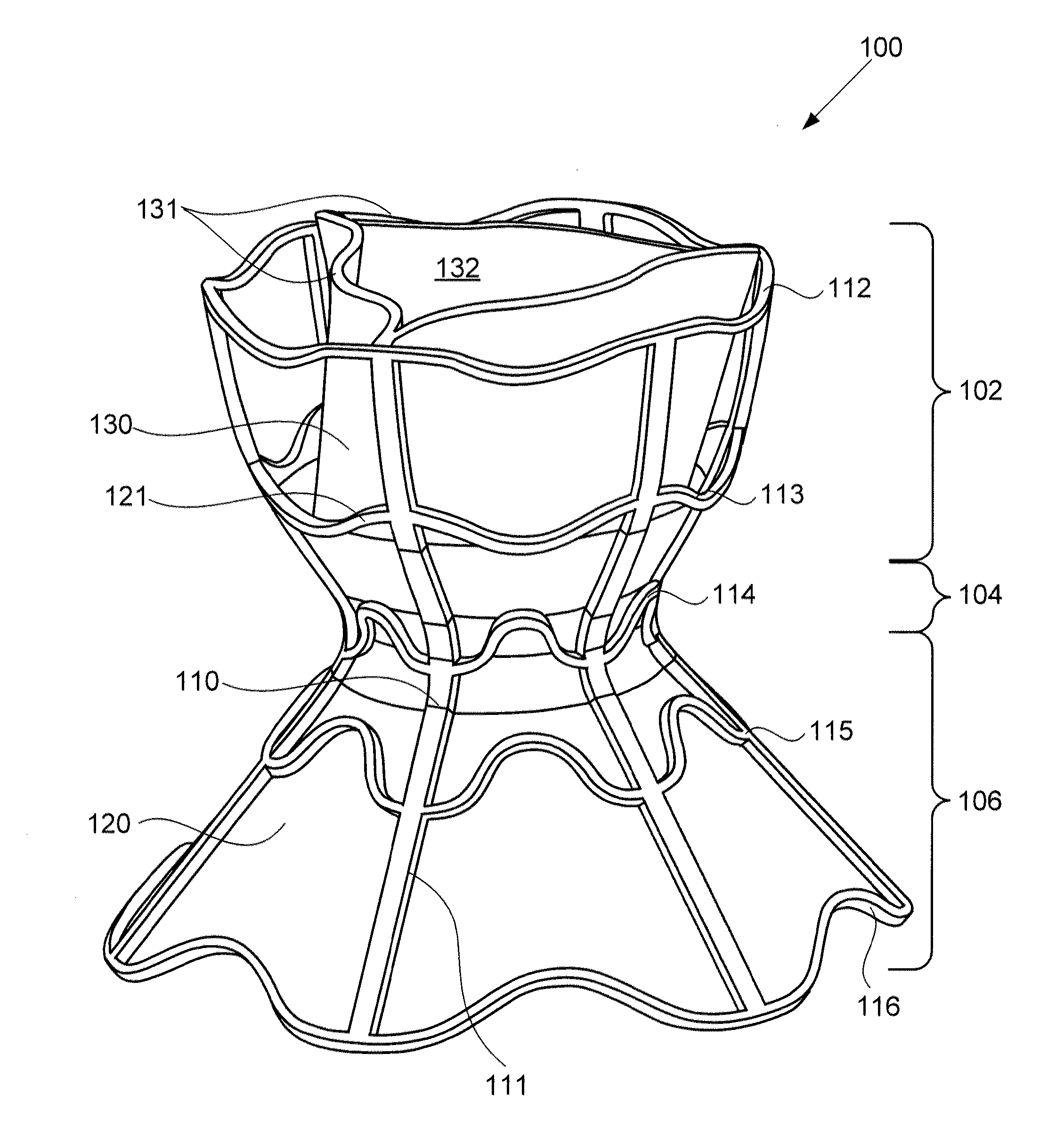
Devices for reducing left atrial pressure, and methods of making and using same
ActiveUS20120165928A1Reducing left atrial pressureIncrease cardiac outputHeart valvesSurgeryLeft ventricular sizeLeft atrial pressure
A device for regulating blood pressure between a patient's left atrium and right atrium comprises an hourglass-shaped stent comprising a neck region and first and second flared end regions, the neck region disposed between the first and second end regions and configured to engage the fossa ovalis of the patient's atrial septum; and a one-way tissue valve coupled to the first flared end region and configured to shunt blood from the left atrium to the right atrium when blood pressure in the left atrium exceeds blood pressure in the right atrium. The inventive devices may reduce left atrial pressure and left ventricular end diastolic pressure, and may increase cardiac output, increase ejection fraction, relieve pulmonary congestion, and lower pulmonary artery pressure, among other benefits. The inventive devices may be used, for example, to treat subjects having heart failure, pulmonary congestion, or myocardial infarction, among other pathologies.
Owner:WAVE LTD V
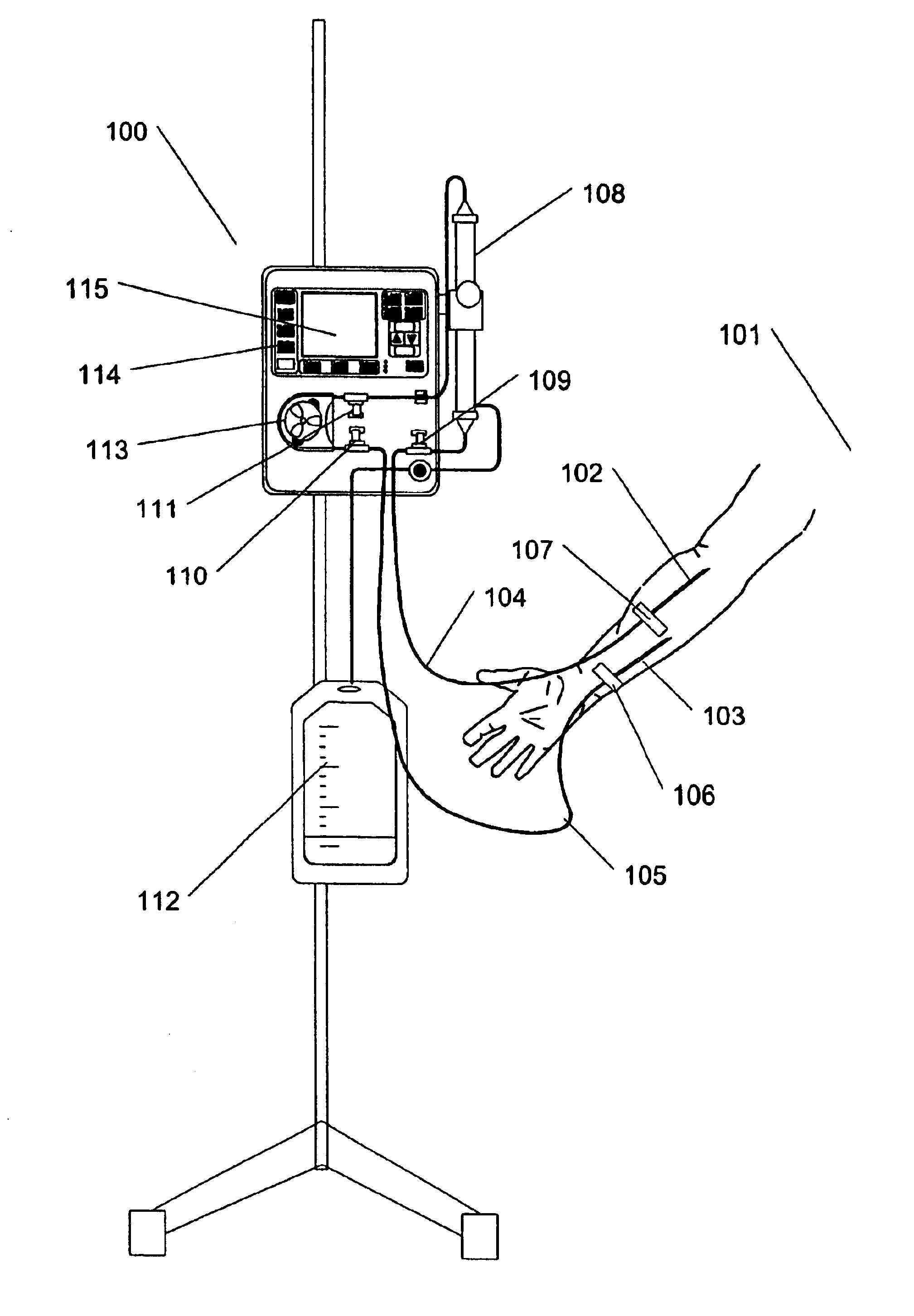
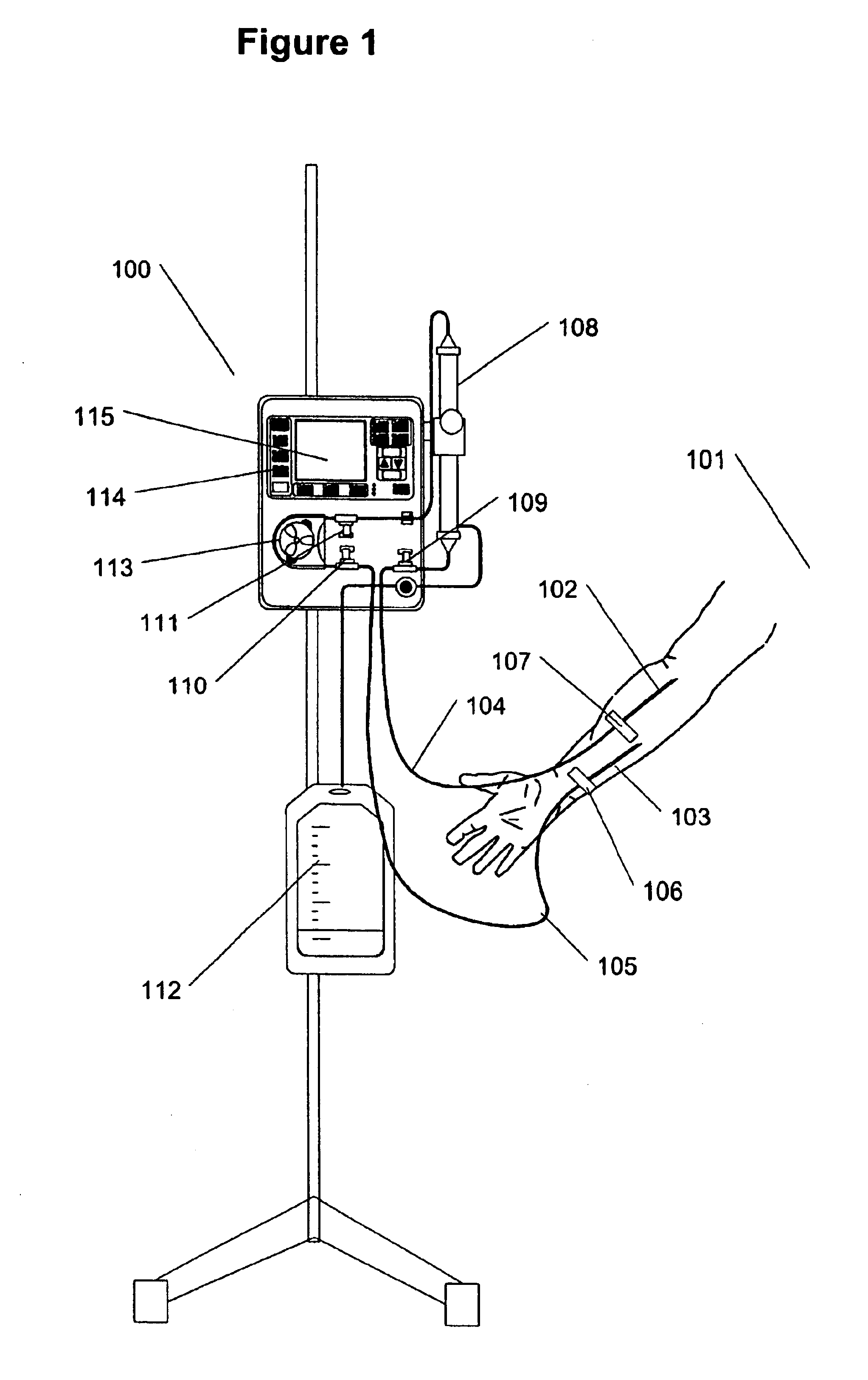
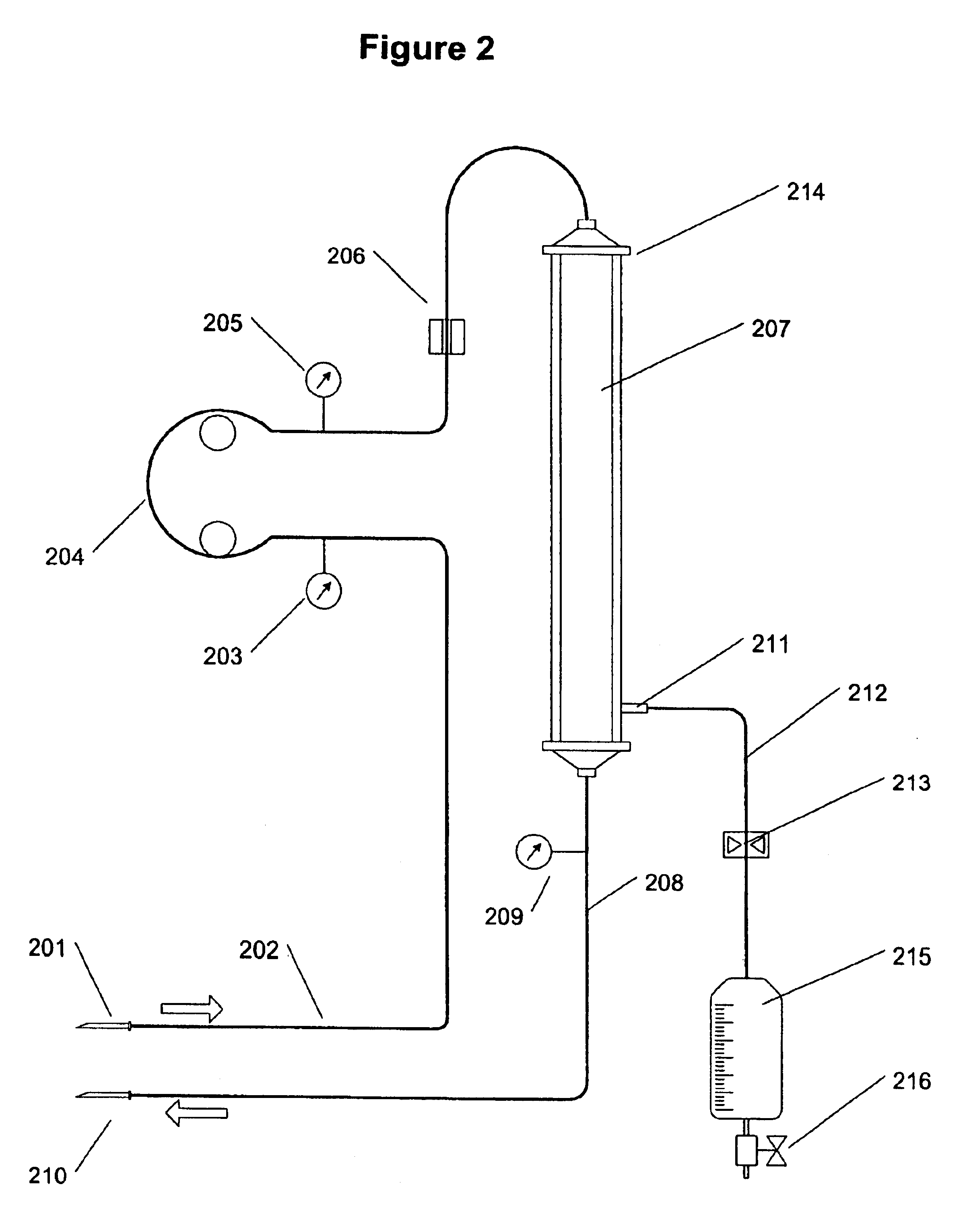
Method and apparatus for vein fluid removal in heart failure
InactiveUS6890315B1Relieve CHF symptomSimple processSemi-permeable membranesSolvent extractionVeinUltrafiltration
A method and apparatus for ultrafiltration of blood operating by removing blood from a peripheral blood vessel at a rate of less than two percent of total cardiac output of a patient, extracting fluid at a rate of 0.1 liter to 1.0 liters per hour while retaining cells and proteins in the blood, and returning the concentrated blood to a secondary blood vessel is disclosed. Blood is removed and returned using small gage needles. As a pump circulates blood from the patient, a filter removes ultrafiltrate from the blood using duty cycle or pump control, and a transparent container collects the removed fluid.
Owner:GAMBRO LUNDIA AB
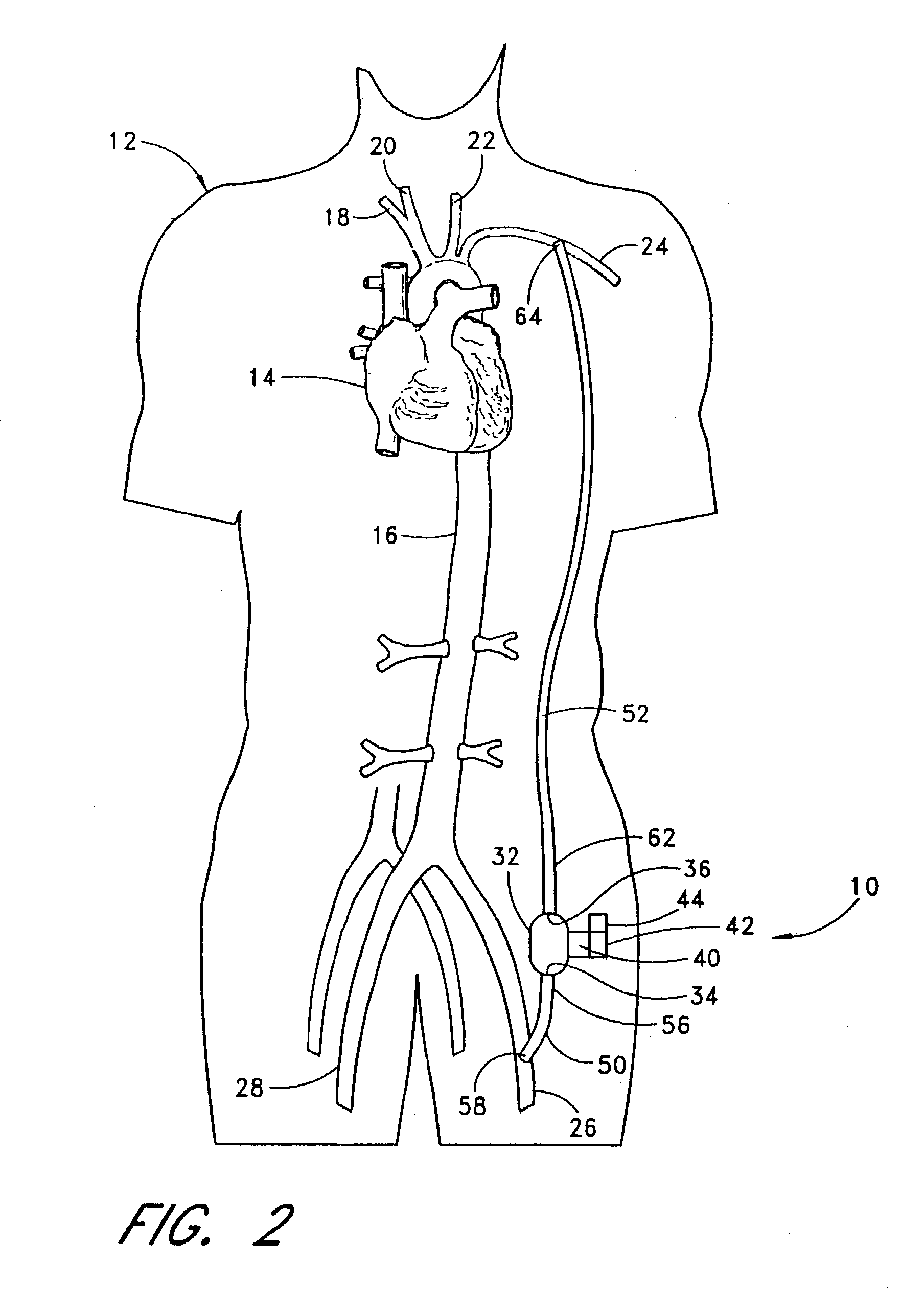
Implantable heart assist system and method of applying same
InactiveUS7125376B2RevitalizeReduce energy inputSpecific fluid pumpsOther blood circulation devicesAfterloadCatheter
An extracardiac pumping for supplementing the circulation of blood, including the cardiac output, in a patient without any component thereof being connected to the patient's heart, and methods of using same. One embodiment of the intravascular extracardiac system comprises a pump with inflow and outflow conduits that are sized and configured to be implantable intravascularly through a non-primary vessel, whereby it may positioned where desired within the patient's vasculature. The system comprises a subcardiac pump that may be driven directly or electromagnetically from within or without the patient. The pump is configured to be operated continuously or in a pulsatile fashion, synchronous with the patient's heart, thereby potentially reducing the afterload of the heart. In another embodiment, the system is positioned extracorporeally, with the inflow conduit and outflow conduit applied percutaneously to a non-primary vessel for circulating blood to and from the non-primary vessel or between the non-primary vessel and another blood vessel within the patient's vasculature.
Owner:TC1 LLC
Method of measuring cardiac related parameters non-invasively via the lung during spontaneous and controlled ventilation
InactiveUS20070062531A1RespiratorsOperating means/releasing devices for valvesAnatomical dead spaceGas concentration
An apparatus to measure cardiac output (Q) and other parameters such as alveolar ventilation (VA), minute CO2 elimination from the lung (VCO2 ), minute oxygen consumption (VO2), oxygenated mixed venous partial pressure of CO2, (PvCO2-oxy), true mixed venous partial pressure of CO2(PvCO2), PaCO2, mixed venous oxygen saturation (SvO2), pulmonary shunt, and anatomical dead space, consisting of: a) a breathing circuit with characteristics that: i. on exhalation, exhaled gas is kept substantially separate from inhaled gas; ii. oninhalation, when VE is greater than FGS flow, the subject inhales FGS first and then inhales a gas that is substantially SGS, for the balance of inhalation; b) gas sensor means for monitoring gas concentrations at the patient-circuit interface c) a first gas set (FGS), and a second gas set (SGS), said second gas set which may comprise previously exhaled gases or exogenous gases or both d) a gas flow control means for controlling the rate of FGS flow into the breathing circuit e) means to identify phase of breathing, said means may consist of pressure sensors or analysis of signal generated by gas sensors or other means known to those skilled in the art; f) machine intelligence consisting of a computer or logic circuit capable of controlling the gas flow control means, receiving the output of the gas sensor means and means to identify phased of breathing, and performing the calculations for measuring cardiac output and other parameters as outlined in the disclosure.
Owner:THORNHILL SCI INC
Shape memory devices and methods for reshaping heart anatomy
InactiveUS7285087B2Improve shrinkageReduce widthSuture equipmentsSurgical needlesCardiac surfaceHeart Part
Owner:MICARDIA CORP
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com