Compositions and methods for treatment of tumors and metastatic diseases
a tumor and metastatic disease technology, applied in the field of tumor and metastatic disease compositions and methods, can solve the problems of inability to cause disease, low and insufficient immunogenicity of tumor antigens to induce more than occasional immune responses, so as to achieve effective treatment and accelerate tumor growth
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 2
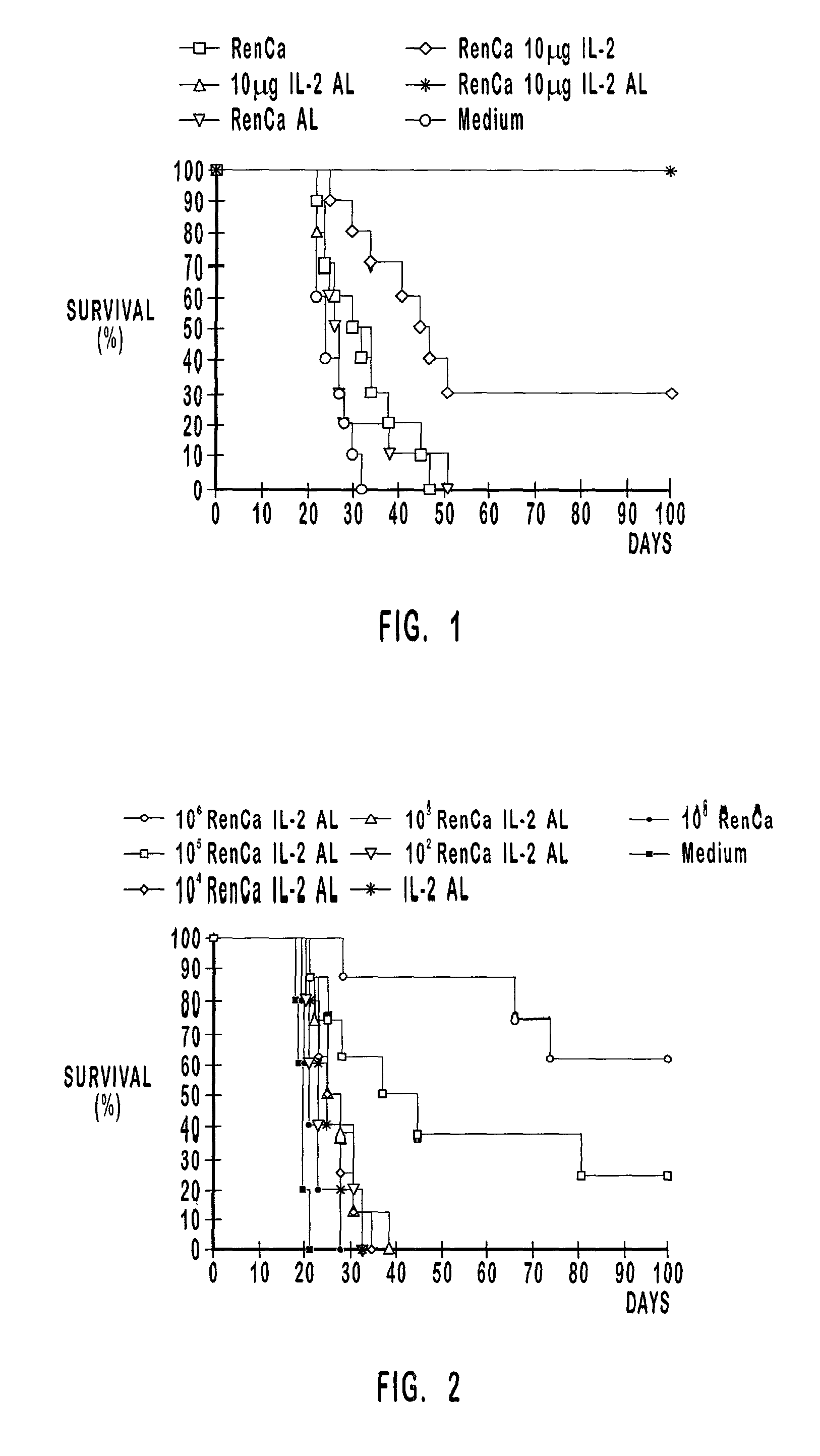
[0202] Therapeutic Vaccination Experiment
[0203] Renal carcinoma was induced into mice via intraperitoneal injection of a lethal dose of vital carcinoma cells to test the influence of tumor cell dose on survival. Four days later, the mice were vaccinated with the compositions described in the first column of Table 2.
2 TABLE 2 vaccination group n day -4 day 0 1 10.sup.6 RenCa 10 .mu.g IL-2 AL 8 i.p. tumor induction s.c. vaccination 2 10.sup.5 RenCa 10 .mu.g IL-2 AL 8 i.p. tumor induction s.c. vaccination 3 10.sup.4 RenCa 10 .mu.g IL-2 AL 8 i.p. tumor induction s.c. vaccination 4 10.sup.3 RenCa 10 .mu.g IL-2 AL 8 i.p. tumor induction s.c. vaccination 5 10.sup.2 RenCa 10 .mu.g IL-2 AL 5 i.p. tumor induction s.c. vaccination 6 10 .mu.g IL-2 AL 5 i.p. tumor induction s.c. vaccination 7 10.sup.6 RenCa 5 i.p. tumor induction s.c. vaccination 8 Medium (RPMI 1640) 5 i.p. tumor induction s.c. injection
[0204] Vaccination groups 1-4 were composed of 8 mice each and vaccination groups 5-7 compris...
example 3
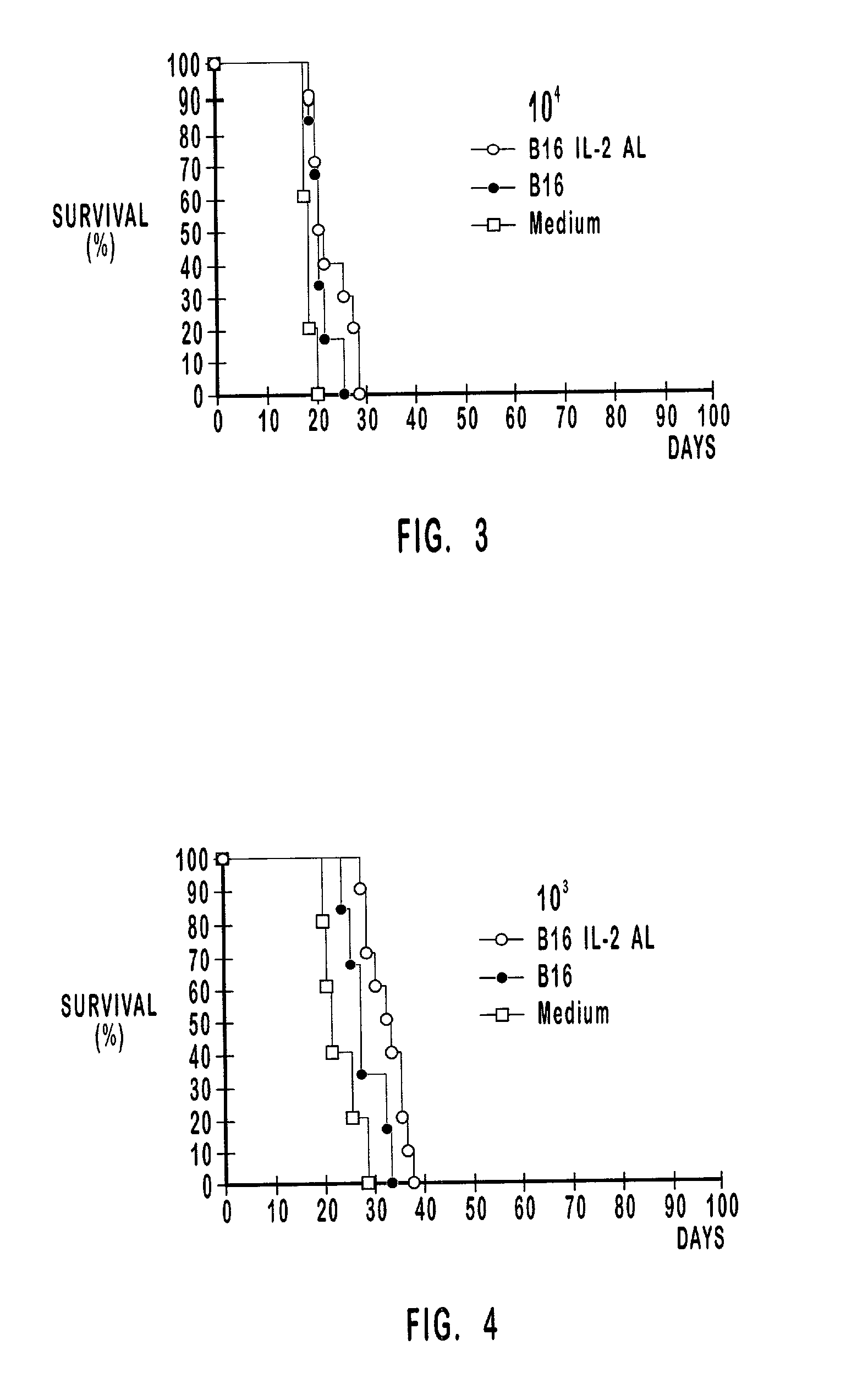
[0220] Therapeutic Vaccination Experiment
[0221] The number of tumor cells plays a role in the composition of the vaccination preparation and also in the composition of the tumor induction preparation. The tumor cells are inactive in the vaccination preparation and the effect of the number of inactivated tumor cells in therapeutic vaccination has been analyzed in Example 2. The tumor cells are active a or vital (hereinafter "vit") in the tumor induction preparations of the therapeutic vaccination study in this example. The number of tumor cells used to induce a tumor is hereinafter referred to as "tumor burden".
[0222] As shown in Table 3, the vaccination groups comprised 10 mice each. The amount of vit B16 cells used to induce tumors were about 10.sup.4, about 10.sup.3 and about 10.sup.2. Mice with tumors induced by each one of these preparations were therapeutically vaccinated with preparations that comprised about 10.sup.5 inactivated B16 cells alone or about 10.sup.5 inactivated B...
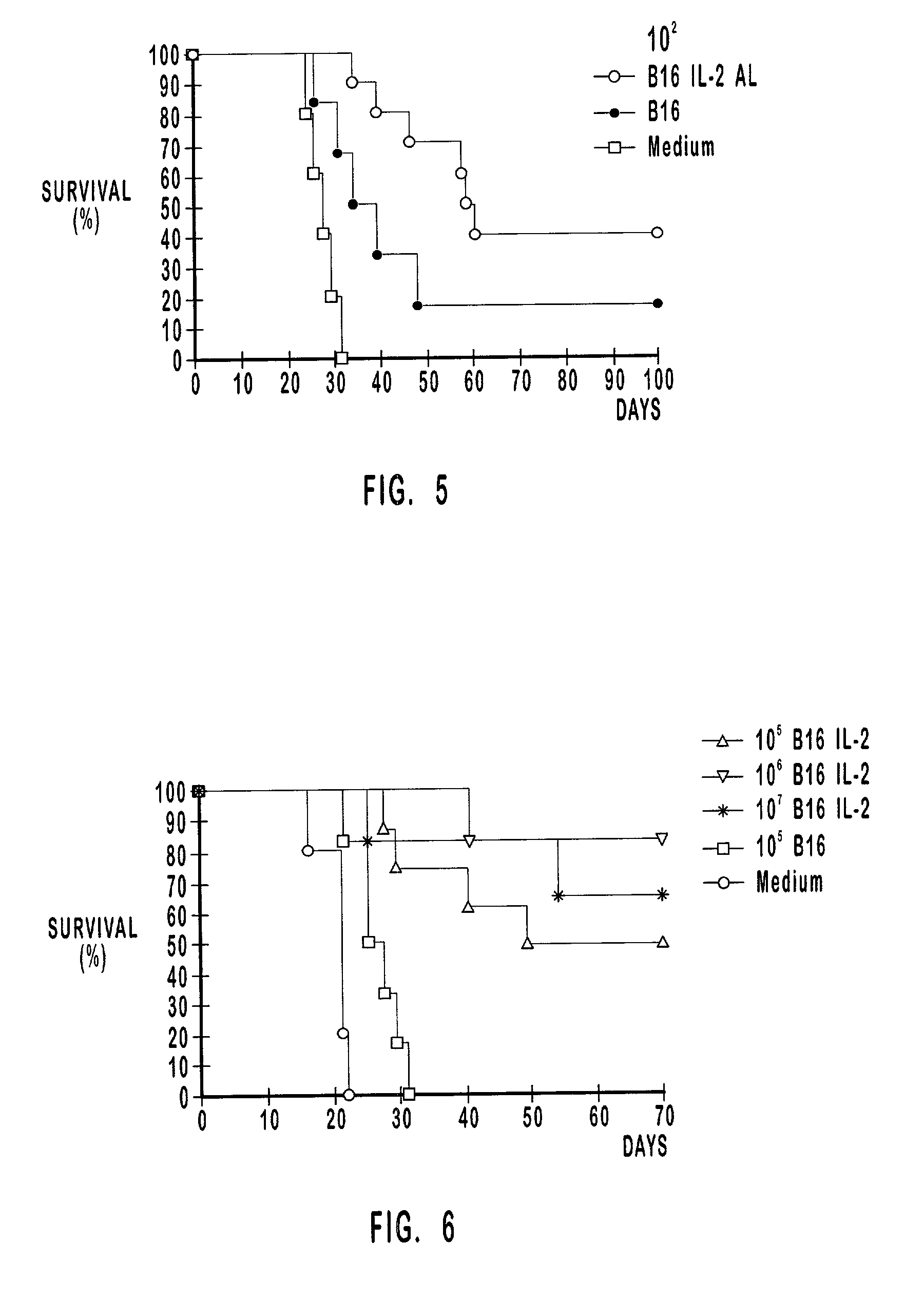
example 4
[0241] Prophylactic Vaccination Experiment
[0242] The influence of the number of inactivated tumor cells in the vaccination composition on survival is analyzed here in a B16 prophylactic study. Prophylactic vaccination was administered four times prior to day 0 (hereinafter "challenge day") when the mice were subcutaneously injected a dose of tumor inducing preparation. Specifically, the prophylactic vaccinations were administered four times (4.times.) on days 35, 28, 21, and 14 prior to the challenge day. The control group comprised 5 mice that were subcutaneously injected medium on the same vaccination days that the mice in the vaccination groups were subcutaneously injected the corresponding vaccination preparation. Vaccination group 1 comprised 8 mice, and the vaccination preparation included about 10.sup.5 inactivated B16 cells, and about 10 .mu.g IL-2 adsorbed to about 10 .mu.g of aluminum hydroxide depot. Vaccination groups 2 and 3 comprised 6 mice each. The vaccination prepar...
PUM
| Property | Measurement | Unit |
|---|---|---|
| concentration | aaaaa | aaaaa |
| time | aaaaa | aaaaa |
| volume | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com