Transcutaneous prosthesis
a prosthesis and transcutaneous technology, applied in the field of transcutaneous prosthesis, can solve the problems of difficult healing, pressure sores, and use of endo-prosthetic devices, and achieve the effects of facilitating the integration of components, increasing external surface area, and increasing the torqu
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
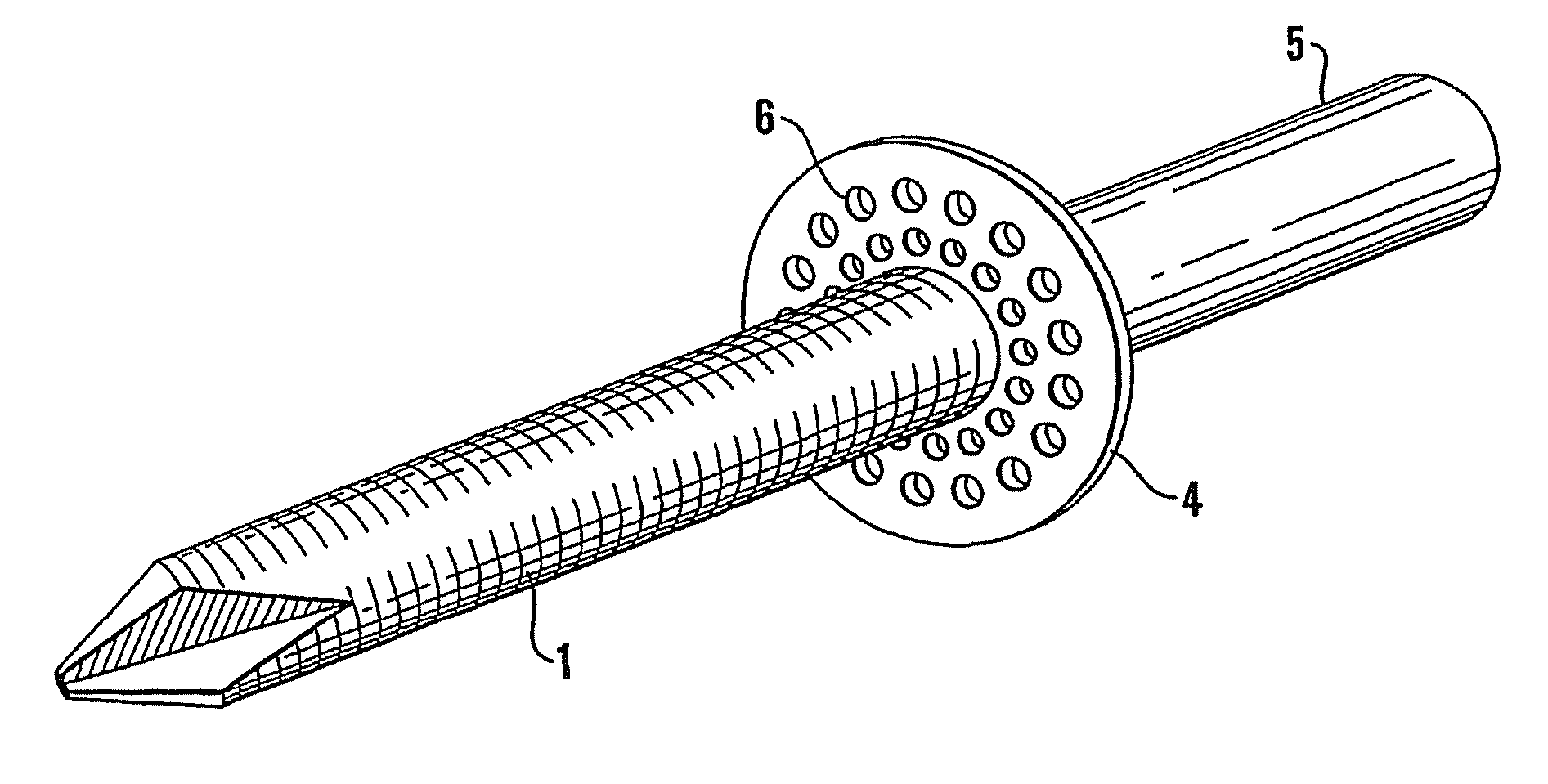
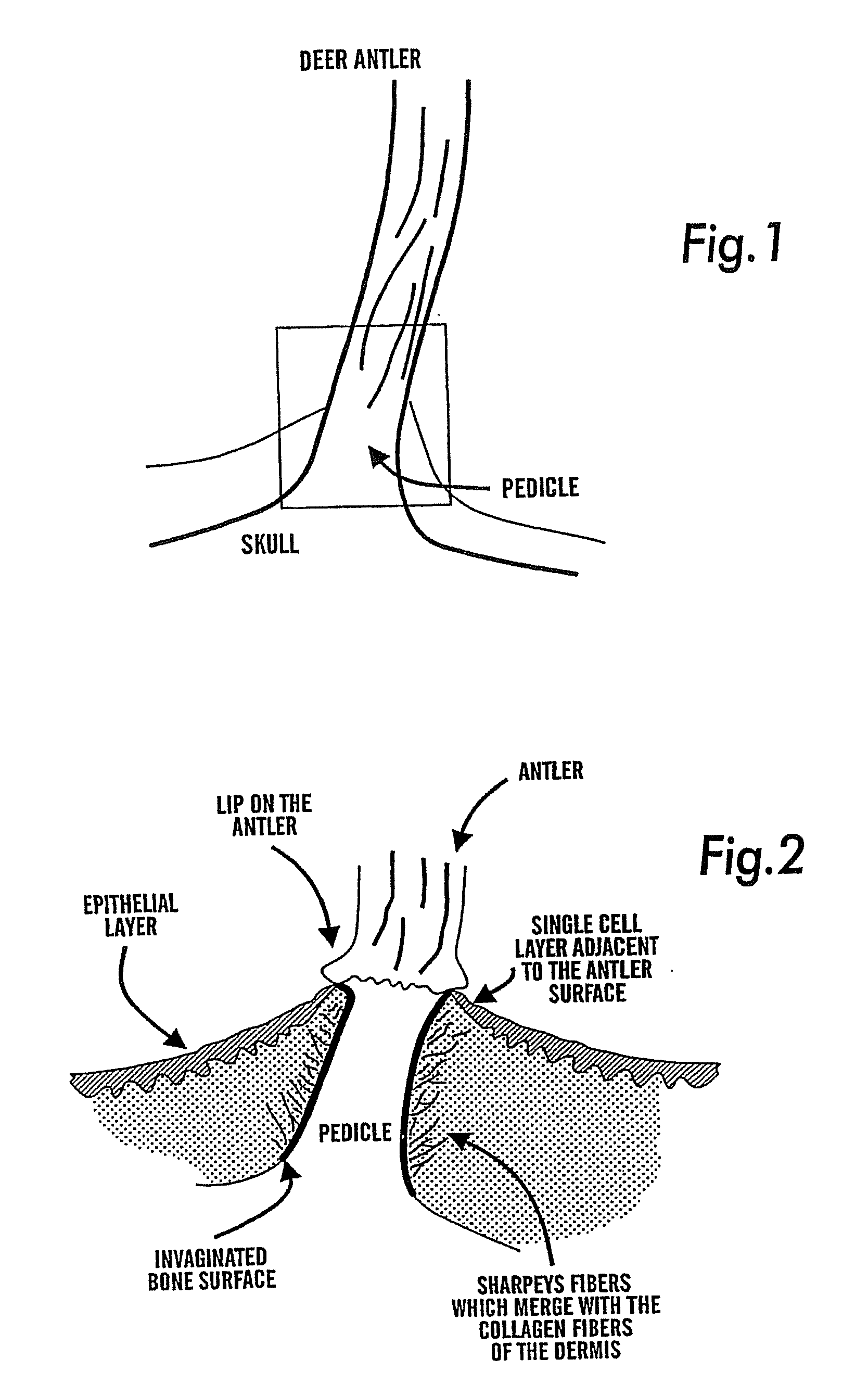
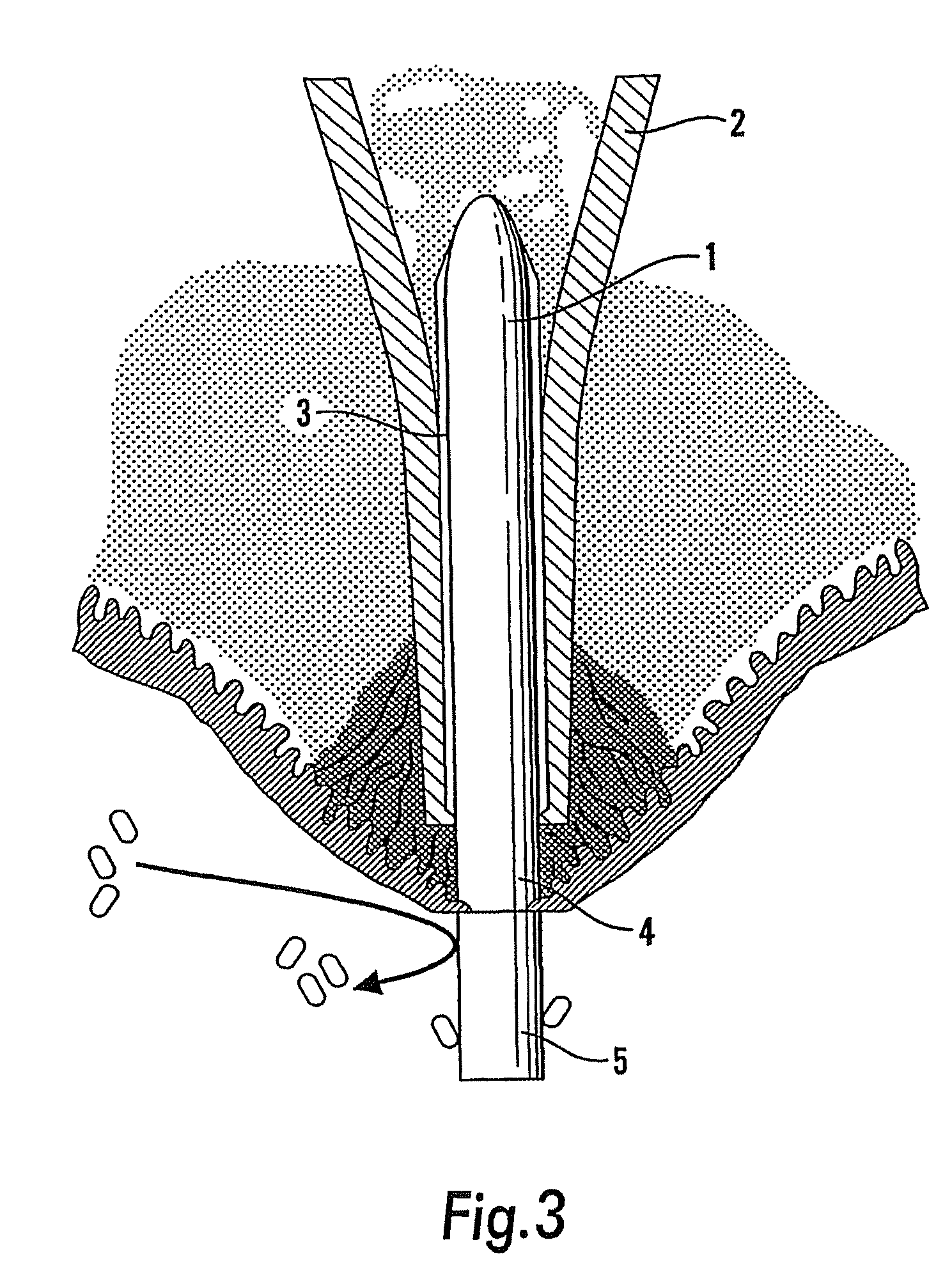
[0022]Referring to the drawings, the present invention was in part stimulated by study of the skin-bone interface around red deer antlers. This is a unique structure and may be thought of as a biological model for a transcutaneous implant. The deer antler at periods of the year is very heavily loaded during the rut. Histological examination indicates that the layer of skin epithelial cells become thinner as the epithelial layer approaches the antler, such that at the antler-skin interface an epithelial skin layer is only about one cell thick. The dermis is intimately attached to the bone (pedicle) interface. The attachment is achieved through a series of “Sharpeys fibres” which attach to the dermis and to the bone and prevent differential skin movement. Antlers do not normally become infected and the bone structure is invaginated with small pores measuring 18 to 40 microns in diameter. This helps the interface between the dermis and the bone to resist shear stresses. These features ...
PUM
| Property | Measurement | Unit |
|---|---|---|
| size | aaaaa | aaaaa |
| size | aaaaa | aaaaa |
| diameter | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com